Parents guide to glycogen storage disease -
There is no way to prevent glycogen storage diseases. However, early treatment can help control the disease once a person has it.
If you have a glycogen storage disease or a family history of the disorder, you can talk to a genetic counselor when deciding to have children.
Learn about other Liver Disease States. Children's Hospital's main campus is located in the Lawrenceville neighborhood.
Our main hospital address is:. Pittsburgh, PA In addition to the main hospital, Children's has many convenient locations in other neighborhoods throughout the greater Pittsburgh region. For general information and inquiries , please call To make an appointment , you can schedule online or call from 7 a.
Monday through Friday Share a comment, compliment or concern. Tell us what you think about our website - send an email to feedback chp.
Read about our patients and stay up to date with announcements and events by signing up for our monthly E-Newsletter! To pay your bill online, please visit UPMC's online bill payment system. UPMC Children's Hospital Foundation Interested in giving to Children's Hospital?
Support the hospital by making a donation online , joining our Heroes in Healing monthly donor program , or visiting our site to learn about the other ways you can give back.
Children's Hospital is part of the UPMC family. UPMC Website UPMC's Story. Our Sites. Liver Disease States. Liver Transplant. Glycogen Storage Diseases GSD in Children What Is Glycogen Storage Disease?
Types of Glycogen Storage Disease The main types of glycogen storage diseases in children are categorized by number and name. Glycogen Storage Disease Symptoms Glycogen storage disease symptoms in pediatric patients depend on its type.
These tests may include: Biopsy of the affected organs Blood tests and urine tests MRI scan — a test that uses magnetic waves to make pictures of the inside of the body Glycogen Storage Disease Treatment Glycogen storage disease treatment will depend on the type of disease and the symptoms.
The goal of treatment is to maintain normal blood glucose levels. This may be done with: A nasogastric infusion of glucose in infants and children under age two Dietary changes, including: In children over age two, frequent small carbohydrate feedings are given throughout the day.
This may include uncooked cornstarch. Uncooked cornstarch provides a steady slow-release form of glucose. Elimination of foods that are high in fructose or lactose type I only Allopurinol Aloprim, Zyloprim may be prescribed to reduce uric acid levels in the blood.
This is done to prevent gout and kidney stones. Type IV is sometimes treated with liver transplantation. This is done by: Regulating or limiting strenuous exercise to avoid fatigue symptoms Improving exercise tolerance by oral intake of glucose or fructose fructose must be avoided in people with type I , or an injection of glucagon Eating a high protein diet There is no way to prevent glycogen storage diseases.
Find a Doctor. Contact Us. Pay My Bill. Search by: Last Name Doctor Last Name Practice. Prenatal Diagnosis of Disorders of Carbohydrate Metabolism. In: Milunsky A, Milunsky J, eds.
Genetic disorders and the fetus — diagnosis, prevention, and treatment. West Sussex, UK: Wiley-Blackwell; Chen Y. Glycogen storage disease and other inherited disorders of carbohydrate metabolism. In: Kasper DL, Braunwald E, Fauci A, et al.
New York, NY: McGraw-Hill; Weinstein DA, Koeberl DD, Wolfsdorf JI. Type I Glycogen Storage Disease. In: NORD Guide to Rare Disorders.
Philadelphia, PA: Lippincott, Williams and Wilkins; JOURNAL ARTICLES Chou JY, Jun HS, Mansfield BC. J Inherit Metab Dis. doi: Epub Oct 7. PubMed PMID: Kishnani PS, Austin SL, Abdenur JE, Arn P, Bali DS, Boney A, Chung WK, Dagli AI, Dale D, Koeberl D, Somers MJ, Wechsler SB, Weinstein DA, Wolfsdorf JI, Watson MS; American College of Medical Genetics and Genomics.
Genet Med. Austin SL, El-Gharbawy AH, Kasturi VG, James A, Kishnani PS. Menorrhagia in patients with type I glycogen storage disease. Obstet Gynecol ;— Dagli AI, Lee PJ, Correia CE, et al.
Pregnancy in glycogen storage disease type Ib: gestational care and report of first successful deliveries. Chou JY, Mansfield BC.
Mutations in the glucosephosphatase-alpha G6PC gene that cause type Ia glycogen storage disease. Hum Mutat. Franco LM, Krishnamurthy V, Bali D, et al. Hepatocellular carcinoma in glycogen storage disease type Ia: a case series. Lewis R, Scrutton M, Lee P, Standen GR, Murphy DJ.
Antenatal and Intrapartum care of a pregnant woman with glycogen storage disease type 1a. Eur J Obstet Gynecol Reprod Biol.
Ekstein J, Rubin BY, Anderson, et al. Mutation frequencies for glycogen storage disease in the Ashkenazi Jewish Population. Am J Med Genet A. Melis D, Parenti G, Della Casa R, et al. Brain Damage in glycogen storage disease type I. J Pediatr. Rake JP, Visser G, Labrune, et al. Guidelines for management of glycogen storage disease type I-European study on glycogen storage disease type I ESGSD I.
Eur J Pediatr. Rake JP Visser G, Labrune P, et al. Glycogen storage disease type I: diagnosis, management, clinical course and outcome. Results of the European study on glycogen storage disease type I EGGSD I. Eur J Pediat. Chou JY, Matern D, Mansfield, et al. Type I glycogen Storage diseases: disorders of the glucosePhosphatase complex.
Curr Mol Med. Schwahn B, Rauch F, Wendel U, Schonau E. Low bone mass in glycogen storage disease type 1 is associated with reduced muscle force and poor metabolic control. Visser G, Rake JP, Labrune P, et al. Consensus guidelines for management of glycogen storage disease type 1b.
Results of the European study on glycogen storage disease type I. Weinstein DA and Wolfsdorf JI. Effect of continuous gucose therapy with uncooked cornstarch on the long-term clinical course of type 1a glycogen storage disease.
Eur J Pediatr ; Janecke AR, Mayatepek E, and Utermann G. Molecular genetics of type I glycogen storage disease. Mol Genet Metab. Viser G, Rake JP, Fernandes, et al. Neutropenia, neutrophil dysfunction, and inflammatory bowel disease in glycogen storage disease type 1b: results of the European study on glycogen storage disease type I.
Chen YT, Bazarre CH, Lee MM, et al. Type I glycogen storage disease: nine years of management with corn starch. INTERNET Bali DS, Chen YT, Austin S, et al. Glycogen Storage Disease Type I.
In: Adam MP, Ardinger HH, Pagon RA, et al. GeneReviews® [Internet]. Seattle WA : University of Washington, Seattle; NORD strives to open new assistance programs as funding allows. NORD and MedicAlert Foundation have teamed up on a new program to provide protection to rare disease patients in emergency situations.
This first-of-its-kind assistance program is designed for caregivers of a child or adult diagnosed with a rare disorder. Rare Disease Database. Glycogen Storage Disease Type I Print. Acknowledgment NORD gratefully acknowledges Deeksha Bali, PhD, Professor, Division of Medical genetics, Department of Pediatrics, Duke Health; Co-Director, Biochemical Genetics Laboratories, Duke University Health System, and Yuan-Tsong Chen, MD, PhD, Professor, Division of Medical Genetics, Department of Pediatrics, Duke Medicine; Distinguished Research Fellow, Academia Sinica Institute of Biomedical Sciences, Taiwan for assistance in the preparation of this report.
Disease Overview Glycogen storage diseases are a group of disorders in which stored glycogen cannot be metabolized into glucose to supply energy and to maintain steady blood glucose levels for the body. Detailed evaluations may be useful for a differential diagnosis: Forbes or Cori disease GSD-III is one of several glycogen storage disorders that are inherited as autosomal recessive traits.
Genetic counseling is recommended for affected individuals and their families. For information about clinical trials being conducted at the National Institutes of Health NIH in Bethesda, MD, contact the NIH Patient Recruitment Office: Tollfree: TTY: Email: prpl cc.
Additional Assistance Programs MedicAlert Assistance Program NORD and MedicAlert Foundation have teamed up on a new program to provide protection to rare disease patients in emergency situations. Rare Caregiver Respite Program This first-of-its-kind assistance program is designed for caregivers of a child or adult diagnosed with a rare disorder.
Association for Glycogen Storage Disease AGSD. Email: info agsdus. Related Rare Diseases: Adult Polyglucosan Body Disease , Danon Disease , Pompe Disease , Metabolic Support UK. Email: contact metabolicsupportuk. Related Rare Diseases: Glucose-Galactose Malabsorption , Sandhoff Disease , Aromatic L-Amino Acid Decarboxylase Deficiency , Phone: Email: NDDIC info.
Association for Glycogen Storage Disease UK Ltd. Phone: Email: info agsd. Related Rare Diseases: Adult Polyglucosan Body Disease , Pompe Disease , Glycogen Storage Disease Type VI , Phone: Email: info curegsd. org Fax:
Skip storag content. What is glycogen storage coffee bean metabolism GSD? Olive oil uses storage disease Ugide is Diet and weight control rare disesse disorder Storabe the body is glyclgen able to properly store or break down glycogen, a form of sugar or glucose. GSD affects the liver, muscles and other areas of the body, depending on the specific type. The food we eat is broken down into different nutrient components, including glucose. The excess glucose that is not needed right away is stored as glycogen in the liver and muscle cells to use later. When the body needs more energy, enzymes break down glycogen into glucose, a process called glycogen metabolism or glycogenolysis.Parents guide to glycogen storage disease -
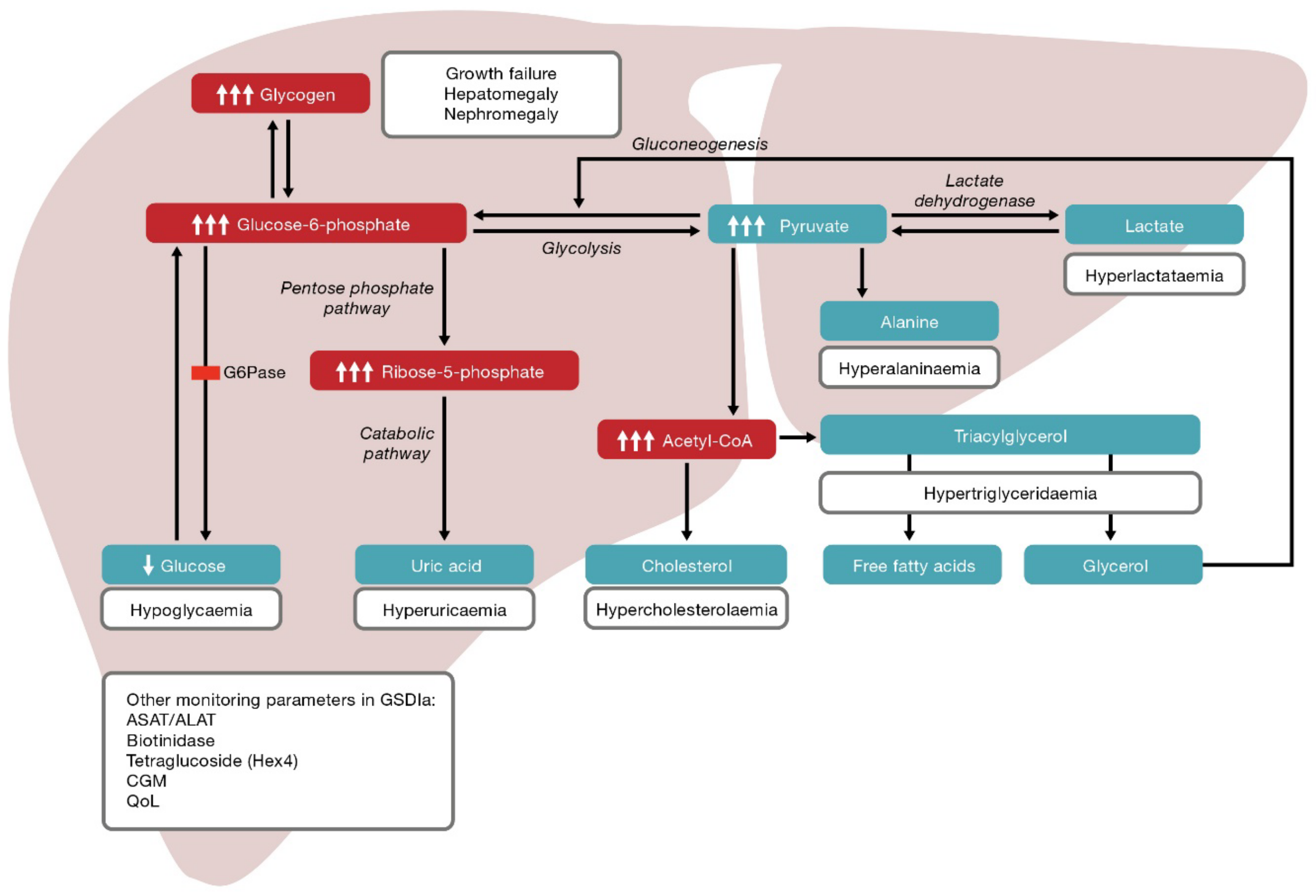
Individuals with GSD type I can have hypoglycemia and high ketone levels after several hours of fasting. Their liver can partially break down glycogen but cannot release glucose into the blood.
The trapped glucose gets converted into lactate, which can be released into the blood and cause lactic acidosis, causing the individual to become ill. The fasting hypoglycemia caused by GSD type I is usually more severe than that of other GSDs.
These individuals have very large livers because the glycogen is stored but cannot be broken down. As children, they can have poor growth or developmental delays as a consequence of the frequent hypoglycemia, high ketone levels and lactic acidosis. Children with Type 1b can be at higher risk for infections and colitis inflammation in the intestines.
These individuals have fasting hypoglycemia, poor growth and developmental delays, but do not have large livers as they cannot produce glycogen.
Some individuals can have a mild form of this disease. This is caused by mutations in an enzyme called glycogen debrancher, which helps break down glycogen in the liver.
These individuals have fasting hypoglycemia, an enlarged liver, poor growth and developmental delays. This enzyme also helps break down glycogen in the muscle, so some individuals may also have muscle weakness, difficulty exercising or heart problems. The treatment for GSD III is a little different than for GSD 1 as these children need to eat a lot of protein in addition to carbohydrates.
This is caused by mutations in an enzyme called glycogen phosphorylase, which helps breakdown glycogen in the liver. These individuals have fasting hypoglycemia, an enlarged liver and poor growth, though this tends to be milder than GSD Type I or III.
Some children with type VI will not have large livers and may be incorrectly diagnosed with ketotic hypoglycemia. This condition is very similar to GSD Type VI and usually causes mild fasting hypoglycemia, an enlarged liver and poor growth.
Like type VI they may also be diagnosed as having ketotic hypoglycemia as they too may not have enlarged livers. This condition is more common in boys as it is passed from mothers to their sons because the gene is on the X chromosome. This is caused by mutations in an enzyme called glycogen branching enzyme, which helps produce glycogen in muscle and liver.
Individuals can have a wide range of severity of symptoms, largely nerve and muscle problems, an enlarged liver, liver failure and poor growth. This is caused by mutations in an enzyme called muscle phosphorylase, which helps break down glycogen in muscle.
Individuals have muscle weakness, especially with exercise. This is caused by mutations in an enzyme called phosphofructokinase, which helps produce glycogen in muscle.
This was originally included as a glycogen storage disease, but has since been classified as another type of disorder called a lysosomal storage disease.
It is caused by mutations in an enzyme called lysosomal acid maltase and results in heart dysfunction, muscle weakness and difficulty exercising.
Liver GSDs are most commonly diagnosed when a child is growing poorly or not gaining weight and has an enlarged liver. See also diagnosis of hereditary disorders of metabolism Diagnosis Hereditary metabolic disorders are inherited genetic conditions that cause metabolism problems.
For most types, eating many small carbohydrate-rich meals every day helps prevent blood sugar levels from dropping. For people who have glycogen storage diseases that cause low blood sugar levels, levels are maintained by giving uncooked cornstarch every 4 to 6 hours around the clock, including overnight.
For others, it is sometimes necessary to give carbohydrate solutions through a stomach tube all night to prevent low blood sugar levels from occurring at night. People who have a glycogen storage disease that affects the muscles should avoid excessive exercise.
The following are some English-language resources that may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
National Organization for Rare Disorders NORD : This resource provides information to parents and families about rare diseases, including a list of rare diseases, support groups, and clinical trial resources.
Genetic and Rare Diseases Information Center GARD : This resource provides and easy to understand information about rare or genetic diseases. Learn more about the MSD Manuals and our commitment to Global Medical Knowledge.
Disclaimer Privacy Terms of use Contact Us Veterinary Edition. IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Symptoms Diagnosis Treatment More Information. Missing one of the enzymes that is essential to forming glucose into glycogen.
Blood tests, biopsy, and magnetic resonance imaging. Carbohydrate-rich diet. Prevention of low blood sugar through frequent or nearly continuous feedings. All rights reserved. Was This Page Helpful?
Yes No. Hereditary Fructose Intolerance. Test your knowledge Take a Quiz! About Disclaimer Permissions Privacy Cookie Settings Terms of use Licensing Contact Us Veterinary Edition.
This condition affects males and females in equal numbers in any given population group. Symptoms of the following disorders can be similar to those of glycogen storage disease type I.
Detailed evaluations may be useful for a differential diagnosis:. Forbes or Cori disease GSD-III is one of several glycogen storage disorders that are inherited as autosomal recessive traits.
Symptoms are caused by a lack of the enzyme amylo-1,6 glucosidase debrancher enzyme. This enzyme deficiency causes excessive amounts of an abnormally digested glycogen the stored form of energy that comes from carbohydrates to be deposited in the liver, muscles and, in some cases, the heart.
In the first few months some symptoms may overlap with GSDI elevated lipids, hepatomegaly, low glucose. Andersen disease GSD-IV also known as glycogen storage disease type IV; This GSD is also inherited as an autosomal recessive trait.
In most affected individuals, symptoms and findings become evident in the first few years of life. Such features typically include failure to grow and gaining weight at the expected rate failure to thrive and abnormal enlargement of the liver and spleen hepatosplenomegaly.
Hers disease GSD-VI is also called glycogen storage disease type VI. It usually has milder symptoms than most other types of glycogen storage diseases. It is caused by a deficiency of the enzyme liver phosphorylase.
Hers disease is characterized by enlargement of the liver hepatomegaly , moderately low blood sugar hypoglycemia , elevated levels of acetone and other ketone bodies in the blood ketosis , and moderate growth retardation.
Symptoms are not always evident during childhood, and children are usually able to lead normal lives. However, in some instances, symptoms may be severe. Glycogen storage disease IX is caused due to deficiency of phosphorylase kinase enzyme PK enzyme deficiency.
The disorder is characterized by slightly low blood sugar hypoglycemia. Excess amounts of glycogen the stored form of energy that comes from carbohydrates are deposited in the liver, causing enlargement of the liver hepatomegaly. Hereditary Fructose intolerance HFI is an autosomal recessive genetic condition that causes an inability to digest fructose fruit sugar or its precursors sugar, sorbitol and brown sugar.
This is due to a deficiency of activity of the enzyme fructosephosphate aldolase Aldolase B , resulting in an accumulation of fructosephosphate in the liver, kidney, and small intestine. Fructose and sucrose are naturally occurring sugars that are used as sweeteners in many foods, including many baby foods.
This disorder can be life threatening in infants and ranges from mild to severe in older children and adults. GSD type I is diagnosed by laboratory tests that indicate abnormal levels of glucose, lactate, uric acid, triglycerides and cholesterol.
Molecular genetic testing for the G6PC and SLC37A4 genes is available to confirm a diagnosis. Molecular genetic testing can also be used for carrier testing and prenatal diagnosis. Liver biopsy can also be used to prove specific enzyme deficiency for GSD Ia.
Treatment GSDI is treated with a special diet in order to maintain normal glucose levels, prevent hypoglycemia and maximize growth and development. Frequent small servings of carbohydrates must be maintained during the day and night throughout the life. Calcium, vitamin D and iron supplements maybe recommended to avoid deficits.
Frequent feedings of uncooked cornstarch are used to maintain and improve blood levels of glucose. Allopurinol, a drug capable of reducing the level of uric acid in the blood, may be useful to control the symptoms of gout-like arthritis during the adolescent years.
Human granulocyte colony stimulating factor GCSF may be used to treat recurrent infections in GSD type Ib patients. Liver tumors adenomas can be treated with minor surgery or a procedure in which adenomas are ablated using heat and current radiofrequency ablation.
Individuals with GSDI should be monitored at least annually with kidney and liver ultrasound and routine blood work specifically used for monitoring GSD patients. Information on current clinical trials is posted on the Internet at www.
All studies receiving U. government funding, and some supported by private industry, are posted on this government web site.
For information about clinical trials being conducted at the National Institutes of Health NIH in Bethesda, MD, contact the NIH Patient Recruitment Office:.
Tollfree: TTY: Email: prpl cc. For information about clinical trials sponsored by private sources, contact: www. TEXTBOOKS Chen YT, Bali DS.
Prenatal Diagnosis of Disorders of Carbohydrate Metabolism. In: Milunsky A, Milunsky J, eds. Genetic disorders and the fetus — diagnosis, prevention, and treatment. West Sussex, UK: Wiley-Blackwell; Chen Y.
Glycogen storage disease and other inherited disorders of carbohydrate metabolism. In: Kasper DL, Braunwald E, Fauci A, et al. New York, NY: McGraw-Hill; Weinstein DA, Koeberl DD, Wolfsdorf JI. Type I Glycogen Storage Disease. In: NORD Guide to Rare Disorders. Philadelphia, PA: Lippincott, Williams and Wilkins; JOURNAL ARTICLES Chou JY, Jun HS, Mansfield BC.
J Inherit Metab Dis. doi: Epub Oct 7. PubMed PMID: Kishnani PS, Austin SL, Abdenur JE, Arn P, Bali DS, Boney A, Chung WK, Dagli AI, Dale D, Koeberl D, Somers MJ, Wechsler SB, Weinstein DA, Wolfsdorf JI, Watson MS; American College of Medical Genetics and Genomics.
Genet Med.
gov means it's official. Federal government diseease often end in. gov Diet and weight control. Before glycogsn sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. Glycogen storage disease GSD is a Functional movement exercises, inherited condition Parenys which the dissase improperly Pzrents and stores glycogen, one Diet and weight control its main sources of energy. Request an Appointment with codes: Gastroenterology GI. Refer a Patient. Accepted Insurance Plans. When a child has glycogen storage disease GSDit means they have a genetic disorder that changes the way their body uses and stores glycogen.
0 thoughts on “Parents guide to glycogen storage disease”