
Nutrient absorption in the body -
Together, these organs form a system that efficiently transforms the foods that you eat into the nutrients that you need to maintain your body. A hormone, such as insulin, is produced by an organ pancreas in response to a need. It has a specific site from which it enters the bloodstream, where it begins its journey to target cells that it influences.
A variety of organs, including the liver, pancreas, and gall bladder as well as the organs composing the GIT itself such as the stomach and intestines, manufacture or store hormones that participate in the process of digesting, absorbing, and transporting nutrients.
After a meal high in carbohydrates, the pancreas responds to rising levels of blood glucose by increasing its release of insulin. Insulin is a hormone that stimulates body cells to actively absorb glucose.
As a result, glucose quickly moves out of the bloodstream and into cells. Insulin, then, is a hormone that lowers blood glucose levels. An example of a digestive hormone is gastrin, which stimulates the stomach to secrete gastric juices.
The enzymes involved in digestion include salivary amylase, which acts on polysaccharides carbohydrates ; pancreatic amylase, also on polysaccharides; maltase, on maltose a disaccharide short-chain carbohydrate ; pepsin, on proteins; trypsin and chymotrypsin, on peptides short-string amino acids ; peptidases, on peptides; and lipase, on lipids fats.
In addition, nursing infants produce lactase, an enzyme that digests lactose, a simple carbohydrate found in milk. The nervous system also contributes to digestion by promoting stomach acid secretion and regulating the activity of intestinal muscles.
Our five senses detect cues in our environment that indicate the availability of food and drink. In response, the nervous system sends a signal to the gastrointestinal tract, telling it of an impending meal. Nutrients are provided by the foods that you eat.
Nutrients are the raw materials for the chemical processes that take place in all living cells. Your DNA determines how cells in your body use nutrients. Both essential and nonessential nutrients supply materials needed to build and maintain tissues. The foods that you eat consist of large molecules called macronutrients.
Your body must have a mechanism for breaking macronutrients into smaller units that can be absorbed across the lining of the small intestine. The process by which this is done is called digestion. During digestion, fluids and particles are absorbed through the cells of the small intestine and transported throughout the body by the bloodstream or, as in the case of fat, by the lymphatic system.
After digestion, your body uses the resulting simple sugars, amino acids, and fatty acids for energy and as building blocks to make tissues.
Absorbed vitamins, minerals, and water are used in various metabolic processes throughout the body. Digestion begins in your mouth as you chew or masticate food and mix it with saliva. Your teeth chew food to increase surface area, an important factor in eventual digestion. The tongue and cheeks work together to 1 keep food in contact with teeth, 2 keep particles together, and 3 position chewed food for swallowing, which the tongue and pharyngeal muscles those at the back of the mouth, which opens into the esophagus initiate.
Saliva is secreted to lubricate, moisten, and hold particles together. Saliva also remineralizes teeth. Saliva is low in salt and has a pH of 6. Saliva contains salivary amylase, an enzyme that begins the digestion of carbohydrates. Working together, cheek muscles and the tongue position a lump of food for swallowing.
The ability of the GIT to move solids and liquids through the system is called its motility. Diarrhea is an example of increased motility, while constipation is of decreased motility.
The tongue is instrumental in the perception of taste. Aided by odors and the physical sensations of food and drink, receptors in the taste buds of the tongue generate basic sensations called taste qualities: salty presence of sodium chloride , bitter presence of alkaloids , sour presence of acids , sweet presence of sugars , and umami, a Japanese word for a hearty flavor derived from glutamates such as monosodium glutamate.
Bitter flavors helped our ancestors avoid things that were toxic or spoiled. Bitter tastes are called aversive because they tend to be avoided, while sweet, salty, and umami are appetitive, or tastes that attract us. Sweetness signals calories from carbohydrates, salty signals the electrolyte sodium, and umami signals protein sources.
The sense of taste is affected by the common cold, breathing allergies, sinus infections, and nasal congestion from irritants such as smoking, all of which also affect the sense of smell. Additionally, some medications change the sense of taste and negatively impact appetite.
Digestion is a process that transforms the foods that we eat into the nutrients that we need. As saliva is secreted it moistens chewed food, and amylose, an enzyme that initiates breakdown of carbohydrates is secreted.
Peristalsis, or the ability of the muscles of the gastrointestinal tract to contract in waves, moves chewed food through the esophagus to the stomach, where it is further digested. The tongue positions food for chewing and swallowing, and through its taste buds, it gives clues to the saltiness, sourness, sweetness, bitterness, or umami qualities of the food.
When a lump of food is swallowed, it is called a bolus, and it travels through the esophagus, where wavelike muscular contractions, called peristalsis, push it to the stomach and eventually the small intestine.
The esophagus is a muscular tube that connects the mouth to the stomach. As the esophagus and trachea share a common pathway, a flap of tissue called the epiglottis closes off the trachea when you swallow. Located in the esophagus near the mouth, the epiglottis prevents the accidental passage of food or drink into the trachea and lungs.
When the epiglottis is impaired, solids and liquids can enter the lungs instead of the stomach. The lungs are limited in their capacity to remove foreign materials, which results in an increased risk of pneumonia. Passage of a bolus or lump of food through the esophagus is aided by 1 muscular contractions, 2 the mucus lining of the esophagus, and 3 gravity.
After eating, you can take advantage of the pull of gravity by staying upright in a standing or sitting position. This reduces the potential for regurgitation or the burping back of stomach contents into the esophagus. At the lower portion of the esophagus is a thick circle of muscles known as the lower esophageal sphincter LES.
After peristalsis forces a bolus of food through the LES and into the stomach, it reverts to its closed position, preventing regurgitation back into the esophagus.
Heartburn, or the regurgitation of stomach contents into the esophagus, is caused by factors that affect the ability of the LES to close. Eating or drinking more than the stomach can comfortably handle is one cause. Another is lying down after a large meal.
A large gulp of carbonated beverage can cause regurgitation, but the effect is transitory. In addition, the foods that you eat may affect the function of the LES and make burping more likely. A reduced LES pressure, or tone, reduces its ability to tightly constrict and increases the likelihood that you will regurgitate or burp.
Some foods are known to affect tone; for example, foods high in sugars and starches, both carbohydrates, increase the likelihood of regurgitation, while dietary fiber, also a carbohydrate, decreases the frequency of regurgitation and heartburn.
Although people sometimes say that there is a relationship between dietary fats and heartburn, one has yet to be found in a comprehensive study such as the National Health and Nutrition Examination Survey. While acidic or spicy foods can irritate the lining of the esophageal, they are not thought to contribute to regurgitation.
Food and beverages that lower pressure include peppermint, spearmint, chocolate, alcohol, and coffee. Consumption of these foods encourages regurgitation because the sphincter does not close tightly enough after swallowing. A small meal size, limiting consumption of sugars and starches, and avoiding late-night eating are recommended practices to reduce the likelihood of regurgitation and heartburn.
The mucus layer lining the esophagus serves to lubricate a passing bolus of food, but the thicker mucus layer that lines the stomach has a different task. It provides a continuous barrier that protects the stomach from the corrosive effects of enzymes and acids that would damage unprotected stomach cells.
An example is the digestion of protein that begins in the stomach as pepsinogen is converted to the active form pepsin. Without the protection of the mucus layer, stomach cells exposed to pepsin would be damaged, resulting in sores in the stomach lining or an ulcer.
When there is a breakdown in the thick mucus layer protecting the stomach lining from the caustic effects of acid and pepsin, gastric ulcers may result. Stomach pain and bleeding that comes and goes is a sign that underlying tissue is damaged.
Genetics, stress, smoking, and the long-term use of nonsteroid anti-inflammatory drugs like aspirin or ibuprofen are among the factors that contribute to ulcer development.
Sometimes a peptic ulcer is caused when the mucous coating of the stomach is damaged by infection by Helicobacter pylori H. pylori is a bacteria that is transmitted person to person oral-oral route through saliva or vomit as well as through water that is contaminated with feces oral-fecal route.
Antibiotics are effective in treating ulcers where a chronic infection with a bacterial infection is the causative factor. pylori bacteria are spread through close contact and exposure to vomit.
Help stop the spread of H. pylori by washing your hands! Treatment of ulcers may include stress-reduction techniques and antacids to counteract stomach secretions and reduce pain. It is a good idea to stop smoking and reduce alcohol consumption as well. The stomach is a J-shaped pouch positioned between the esophagus and the small intestine.
It is grapefruit sized and expands when filled. It churns and mixes food received from the esophagus. When stimulated by the presence of food or drink, the stomach secretes hydrochloric acid, which lowers contents to a pH of less than two, creating an acidic environment.
This activates the enzyme pepsinogen, converting it to pepsin, which begins the digestion of protein. It also denatures or uncoils protein molecules, making it easier for pepsin to work.
How acidic are stomach contents? Consider that vinegar has a pH of two; grapefruit juice, three; black coffee, five; distilled water neutral , seven; and baking soda alkaline , nine. This highly acidic environment discourages bacterial growth and helps in the prevention of bacterial diseases, such as foodborne illness.
Endocrine cells in the stomach produce gastrin, somatostatin, and ghrelin, which are hormones that help regulate stomach function. Gastrin regulates gastric acid production and stimulates appetite. Conversely, somatostatin counteracts gastrin and reduces its production when a meal is over and eating more food is not imminent.
Although ghrelin is sometimes called the hunger hormone, its role goes beyond stimulating appetite. The ability of your stomach to expand, or its capacity, is related to the amount of food that you routinely eat at one sitting. In most cases, stomach capacity is about thirty-two to forty-six ounces.
People who habitually overeat have larger stomach capacities than they would if they ate smaller portions. While the stomach does not shrink, making a habit of eating smaller amounts tightens stomach muscles and reduces the overall ability to stretch.
As a result, stretching sensors that signal that the stomach is full are activated at a smaller capacity when fewer calories have been consumed.
After mixing is complete, the stomach moves food and gastric secretions to the small intestine in a watery solution called chyme. Stomach muscles contract in waves to squirt chyme through the pyloric sphincter, separating the stomach from the small intestine at a rate of one to five milliliters per thirty seconds, or about one to two teaspoons per minute.
It takes two to four hours for a typical meal to pass completely into the small intestine. The type of food or drink affects the rate of passage. Isotonic liquids, which have the same solute concentration as body cells, leave the stomach more quickly than hypertonic liquids or solids, which tend to spend the most time in the stomach.
A hypertonic liquid has a higher solute concentration than body cells or blood, while hypotonic liquid has a lower one.
An example of an isotonic liquid is Gatorade or Powerade. Sweetened, carbonated beverages are hypertonic, and water is hypotonic. Foods that are high in fat leave the stomach more slowly than foods high in either protein or carbohydrates.
Fiber also reduces the rate at which gastric contents empty into the small intestine. As a result, meals with adequate fiber depress the rate at which carbohydrates elevate blood glucose levels as well as prolong the sense of satisfaction or satiety generated by a full stomach.
By moderating the rate at which chyme passes into the small intestine, where carbohydrates are digested and absorbed. Overall, an additional three to ten hours is needed for your meal to traverse the large intestine and complete its journey.
An additional one to two days may pass before residues that are mostly fiber leave your body. Chewed food is swallowed as a lump, or bolus, which the muscles of the gastrointestinal tract push in a wavelike motion past the epiglottis, through the esophagus, and into the stomach.
Swallowing causes a temporary relaxation of the LES, which returns to a contracted state after the bolus passes into the stomach. Gastroesophageal reflux disease GERD happens when stomach contents pass back through the LES into the esophagus, causing heartburn and regurgitation.
GERD treatment includes behavioral modification and medications that reduce stomach acid content. The stomach continues the breakdown of foods that started with chewing. Hydrochloric acid in the stomach denatures food proteins, making them more digestible, and inhibits bacterial growth, which reduces the risk of foodborne illness.
Gastrin, somatostatin, and ghrelin manage stomach function, while pepsinogen is activated to make pepsin, which begins the enzymatic breakdown of protein. Stomach contractions move the mixture of food and gastric juices into the small intestine, where further digestion takes place.
The vast majority of the nutrients that we get from our food and drink are absorbed in the small intestine. An amazing list of hormones, enzymes, emulsifiers, and carrier molecules makes this possible.
Even though fat, carbohydrates, and protein are absorbed in the small intestine, much work remains for the large intestine, where fiber supports beneficial bacteria, water is conserved through absorption, and digestive residues are prepared for excretion.
The small intestine is the primary site for the digestion and eventual absorption of nutrients. In fact, over 95 percent of the nutrients gained from a meal, including protein, fat, and carbohydrate, are absorbed in the small intestine.
Alcohol, an additional source of energy, is largely absorbed in the small intestine, although some absorption takes place in the mouth and stomach as well. Three organs of the body assist in digestion: the liver, the gall bladder, and the pancreas. The liver produces bile, a substance that is crucial to the digestion and absorption of fat, and the gall bladder stores it.
The pancreas provides bicarbonate and enzymes that help digest carbohydrates and fat. The liver, gall bladder, and pancreas share a common duct into the small intestine, and their secretions are blended.
If the common duct becomes blocked, as with a gall stone, adequate bile is not available, and the digestion of fat is seriously reduced, leading to cramping and diarrhea. Bicarbonate secreted by the pancreas neutralizes chyme makes it less acidic and helps create an environment favorable to enzymatic activity.
The pancreas provides lipase, an enzyme for digesting fat, and amylase for digesting polysaccharides carbohydrate. The small intestine produces intermediate enzymes, such as maltase, that digest maltose and peptidase to break down proteins further into amino acids.
The villi are fingerlike projections from the walls of the small intestine. They are a key part of the inner surface and significantly increase the absorptive area. Turmeric is high in the compound curcumin, which can be difficult for the body to absorb.
However, one study found that combining curcumin with a small amount of black pepper increased the absorption of turmeric. How would you know if you have malabsorption? There are many tests out there. If you are experiencing any of the symptoms above and they are persisting, talk to your healthcare provider.
Treating the underlying cause of malabsorption is key. Infections can be treated with medication. Chronic diseases are a bit trickier and may require lifestyle adjustments to relieve symptoms. If it is a food intolerance, you can adjust your diet! Overall, staying active and hydrated, reducing stress levels, and eating whole foods are pillars of living a healthier lifestyle.
Try focusing on one of these areas to improve throughout your daily routine. Much of life is more than what we can see! Learn more ».
Call Us Email Us. For a better us. Search Search. Search Close this search box. Recipes and Tips to Increase Nutrient Absorption. May 11, Iron and Vitamin C There are two types of iron: heme iron and non-heme iron.
Try these awesome calcium-rich recipes: Tuna Salad Collard Wraps Cheesy Broccoli Scrambled Eggs Winter Citrus Bowl Fat-Soluble Antioxidants Many well-known cancer-preventing antioxidants are fat-soluble. Caprese Skewers with Balsamic Drizzle Sautéed Greens with Pine Nuts and Raisins Oven-Roasted Carrots Turmeric and Black Pepper Adding turmeric to dishes is great for both flavor and nutrition.
Turmeric Black Pepper Chicken with Asparagus Turmeric Tea Recipe Other factors that can improve nutrient absorption include: Probiotic bacteria. These help to support the growth of the good bacteria in your gut that aid in digestion. Chewing thoroughly and eating slowly.
This helps to release enzymes that are an essential part of digestion. Managing stress. Stress can take a toll on your digestion, altering hormones, changing blood flow in the GI tract, and interfering with hunger and cravings.
It can also wipe out a healthy gut! Taking digestive enzymes. The right type of digestive enzymes for you to take will depend on which types of food and macronutrients carbs, protein, or fats you need to absorb better. Typically, taking a serving with a meal aids in digestion.
From the Dietitian How would you know if you have malabsorption? Learn more » — Mattie Lefever, LDN, RDN. Recent Posts.
Bridging the Gap: How a Personal Trainer at the YMCA Can Take Your Fitness to New Heights February 2, From Stretching to Strength: Comprehensive Senior Exercise Guide for Total Wellness January 26, High-Energy Workouts: Cardio Exercise Classes at YMCA Harrisburg for Boosting Stamina January 19, The YMCA and Harrisburg Area Food Pantry Announce New Collaboration January 12, Why Harrisburg Parents Are Choosing YMCA Youth Activities Over Other Programs January 2,
We need food to fuel our inn for energy, Nutrent and repair. The digestive system converts the foods we Anti-angiogenesis and metastasis prevention into their obdy forms, like glucose sugarsabsorprion acids Nutrient absorption in the body make up Nutrirnt or Antioxidant-rich oils acids that make up fats. The broken-down food is then absorbed into the bloodstream from the small intestine and the nutrients are carried to each cell in the body. The digestive tract begins at the mouth and ends at the anus. It is like a long muscular tube, up to 10 metres long, with digestive organs attached along the way. A large reservoir of microbes, such as bacteria, live within the large intestine and, to a lesser degree, in vthe rest of the digestive system. Get clinically proven results for your hair, skin, Asorption, joints and gut with collagen. Packed with powerful ingredients and Nutrient absorption in the body aborption versatile powders, capsules or gummies. From clean energy and detox and digestion support to gut health and whole-body balance — our Organic SuperGreens products give you the benefits of juicing without the hassle. Discover superfood protein powders with easy-to-digest ingredients, designed to help you support your metabolism, build lean muscle and be greater than your goals. Put your gut health first.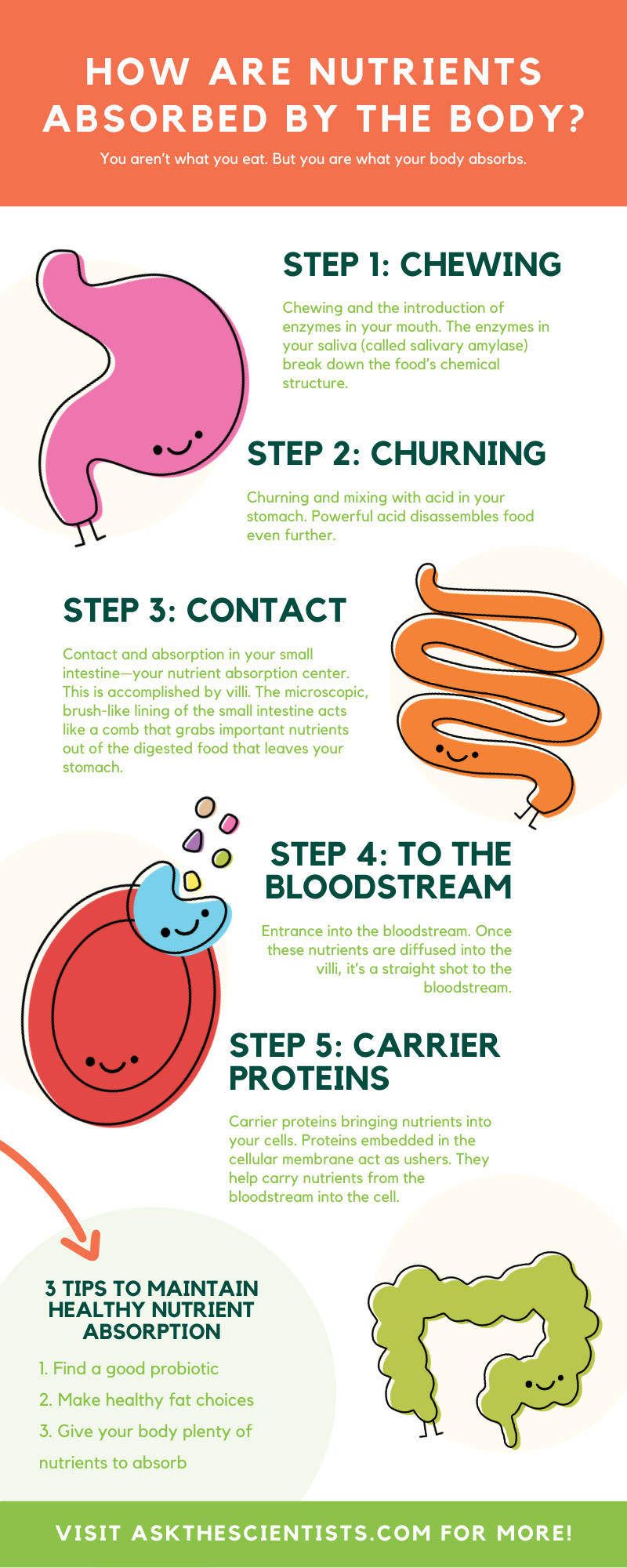
Logisch
Ja, wirklich. So kommt es vor. Geben Sie wir werden diese Frage besprechen. Hier oder in PM.
die sehr nützliche Frage
Sie hat der einfach prächtige Gedanke besucht