Electrolyte balance and kidney function -
Dysnatremia usually indicates a condition where body water becomes excess or deficient. CKD patients follow a similar pattern of dysnatremia distribution. During a median follow-up of 5. A recent meta-analysis of 15 studies has shown a mortality benefit with improving hyponatremia [ ].
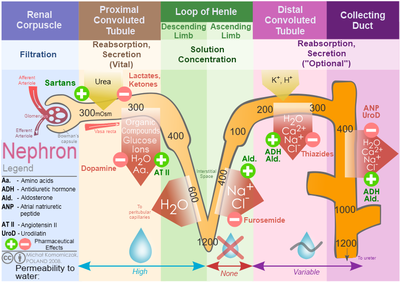
In addition to the causes of hyponatremia seen in the general population, CKD patients are at additional risk of hyponatremia due to compromised capacity to dilute or concentrate urine.
Furthermore, polypharmacy and limited nutritional solute intake [ ] are common and can contribute to the Na derangements.
In dialysis patients, hyponatremia is mostly dilutional, due to excess water or hypotonic fluid intake. Dysnatremia in CKD and ESRD has mortality significance. A U-shaped association between serum Na and mortality was found in both non-dialysis CKD [ , ] and dialysis patients [ , ].
The management of dysnatremia in CKD patients is similar to that for the general patients and should start with identifying and, if possible, correcting the underlying cause.
For dialysis patients, extra sessions of dialysis may be considered. Rapid correction for chronic dysnatremia should be avoided. Although etiology and manifestations of dysmagnesemia have been studied mostly in the general population, both hypo- and hypermagnesemia are common in hospitalized patients with reduced eGFR [ ].
Sustained hypermagnesemia is seen mostly in patients with advanced CKD and ESRD. Mg-containing medications may contribute to or exacerbate hypermagnesemia in the setting of kidney dysfunction.
In dialysis patients, serum Mg is often affected by dialysate Mg content. Sakaguchi et al. Similar results are shown in patients on peritoneal dialysis [ ]. Taken together, dysmagnesemia exerts morbidity and mortality significance in CKD and ESRD patients; care should be taken to correct Mg derangements.
A variety of electrolyte and acid-base derangements predictably occur with progressive loss of kidney function. Most of the derangements are intricately linked to morbidity and mortality.
Prominently, hyperkalemia is linked to acute cardiac death in CKD and ESRD patients. Newer and more effective agents, patiromer and ZS-9, have the potential to mitigate hyperkalemia and improve patient outcomes, especially in those who benefit from RAAS inhibition.
Likewise, acidosis in renal failure patients should be carefully followed and corrected. Newer randomized controlled trials will further clarify our management strategy.
MBD in CKD and ESRD remains a morbid condition. Existing data suggest that non-calcium-containing phosphorus binders are associated with better cardiovascular outcomes. Newer pathogenic signaling pathways continue to be uncovered, and novel treatment targets will likely emerge in the near future.
Na and Mg derangements are reviewed in brief, given the space limitation. Both conditions, however, can be life threatening and should be carefully diagnosed and treated. Taken together, electrolyte and acid-base alterations form a major part of the pathological disease processes in patients with renal failure.
FDA has approved its use for non-dialysis CKD patients. It is not yet approved by the FDA. It can be lifesaving if ACE inhibitors and ARBs are given continuously for most of the CKD and ESRD patients. For ESRD dialysis patients, serum PTH should be within times the upper limit of the normal value.
Adjusting the dialysate Mg content may, thus, be necessary when appropriate. Careful evaluation of the patient's medications, both over-the-counter and prescribed agents, is necessary. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest.
filter your search All Content All Journals Blood Purification. Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 43, Issue Potassium Derangements. Metabolic Acidosis. Derangements of Bone Mineral Metabolism.
Other Electrolyte Derangements. Key Messages. Disclosure Statement. Article Navigation. Review Articles January 24 Electrolyte and Acid-Base Disorders in Chronic Kidney Disease and End-Stage Kidney Failure Subject Area: Nephrology. Tsering Dhondup ; Tsering Dhondup. Division of Nephrology and Hypertension, Department of Medicine, Mayo Clinic, College of Medicine, Rochester, MN, USA.
This Site. Google Scholar. Qi Qian Qi Qian. qi mayo. Blood Purif 43 : — Article history Published Online:. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. The authors have no conflicts of interest to declare.
United States Renal Data System: USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, National Institutes of Health, aspx cited October 8, De Nicola L, Zoccali C: Chronic kidney disease prevalence in the general population: heterogeneity and concerns.
Nephrol Dial Transplant ; Luo J, et al: Association between serum potassium and outcomes in patients with reduced kidney function. Clin J Am Soc Nephrol ; Sarafidis PA, et al: Prevalence and factors associated with hyperkalemia in predialysis patients followed in a low-clearance clinic. Einhorn LM, et al: The frequency of hyperkalemia and its significance in chronic kidney disease.
Arch Intern Med ; Chang AR, et al: Antihypertensive medications and the prevalence of hyperkalemia in a large health system.
Hypertension ; Ingelfinger JR: A new era for the treatment of hyperkalemia? N Engl J Med ; Meng QH, Wagar EA: Pseudohyperkalemia: a new twist on an old phenomenon. Crit Rev Clin Lab Sci ; Parham WA, et al: Hyperkalemia revisited.
Tex Heart Inst J ; Khattak HK, et al: Recurrent life-threatening hyperkalemia without typical electrocardiographic changes. J Electrocardiol ; Barold SS, Herweg B: The effect of hyperkalaemia on cardiac rhythm devices. Europace ; Epstein M, et al: Evaluation of the treatment gap between clinical guidelines and the utilization of renin-angiotensin-aldosterone system inhibitors.
Am J Manag Care ;21 11 suppl :SS Evans BM, et al: Ion-exchange resins in the treatment of anuria. Lancet ; Lepage L, et al: Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Harel Z, et al: Gastrointestinal adverse events with sodium polystyrene sulfonate Kayexalate use: a systematic review.
Am J Med ; Li L, et al: Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia.
J Cardiovasc Pharmacol Ther ; Weir MR, et al: Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. Bakris GL, et al: Effect of patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease: the AMETHYST-DN randomized clinical trial.
JAMA ; Weir MR, et al: Treatment with patiromer decreases aldosterone in patients with chronic kidney disease and hyperkalemia on renin-angiotensin system inhibitors. Kidney Int ; Gekle M, Grossmann C: Actions of aldosterone in the cardiovascular system: the good, the bad, and the ugly?
Pflugers Arch ; Ritz E, Tomaschitz A: Aldosterone, a vasculotoxic agent - novel functions for an old hormone. Bushinsky DA, et al: Effect of patiromer on urinary ion excretion in healthy adults.
Clin J Am Soc Nephrol ;pii:CJN. Packham DK, et al: Sodium zirconium cyclosilicate in hyperkalemia. Kosiborod M, et al: Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia: the HARMONIZE randomized clinical trial.
Bushinsky DA: National Kidney Foundation Spring Clinical Meetings Abstracts April May 1, Patiromer Decreases Serum Potassium in Patients on HD.
Am J Kidney Dis ;A1-A Adrogué HJ, Madias NE: Sodium and potassium in the pathogenesis of hypertension. Tobian L, et al: Potassium reduces cerebral hemorrhage and death rate in hypertensive rats, even when blood pressure is not lowered. Hypertension ;7 3 pt 2 :II Chiu DY, et al: Sudden cardiac death in haemodialysis patients: preventative options.
Nephrology Carlton ; Collins AJ, et al: US Renal Data System Annual Data Report. Am J Kidney Dis ;63 1 suppl :A7. Ohtake T, et al: High prevalence of occult coronary artery stenosis in patients with chronic kidney disease at the initiation of renal replacement therapy: an angiographic examination.
J Am Soc Nephrol ; Buiten MS, et al: The dialysis procedure as a trigger for atrial fibrillation: new insights in the development of atrial fibrillation in dialysis patients. Heart ; Pun PH, et al: Modifiable risk factors associated with sudden cardiac arrest within hemodialysis clinics.
Jadoul M, et al: Modifiable practices associated with sudden death among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Foley RN, et al: Long interdialytic interval and mortality among patients receiving hemodialysis.
Bleyer AJ, et al: Characteristics of sudden death in hemodialysis patients. Bleyer AJ, Russell GB, Satko SG: Sudden and cardiac death rates in hemodialysis patients. Santoro A, et al: Patients with complex arrhythmias during and after haemodialysis suffer from different regimens of potassium removal.
Vallet M, et al: Urinary ammonia and long-term outcomes in chronic kidney disease. Wrong O, Davies HE: The excretion of acid in renal disease.
Q J Med ; Kim HY, et al: Effect of reduced renal mass on renal ammonia transporter family, Rh C glycoprotein and Rh B glycoprotein, expression. Am J Physiol Renal Physiol ;FF J Nephrol ;15 suppl 5 :SS Nath KA, Hostetter MK, Hostetter TH: Pathophysiology of chronic tubulo-interstitial disease in rats.
Interactions of dietary acid load, ammonia, and complement component C3. J Clin Invest ; Wesson DE, Simoni J: Acid retention during kidney failure induces endothelin and aldosterone production which lead to progressive GFR decline, a situation ameliorated by alkali diet. Wesson DE, et al: Acid retention accompanies reduced GFR in humans and increases plasma levels of endothelin and aldosterone.
Shah SN, et al: Serum bicarbonate levels and the progression of kidney disease: a cohort study. Am J Kidney Dis ; Raphael KL, et al: Higher serum bicarbonate levels within the normal range are associated with better survival and renal outcomes in African Americans.
Kanda E, et al: High serum bicarbonate level within the normal range prevents the progression of chronic kidney disease in elderly chronic kidney disease patients.
BMC Nephrol ; Raphael KL, et al: Prevalence of and risk factors for reduced serum bicarbonate in chronic kidney disease. Kopple JD, Kalantar-Zadeh K, Mehrotra R: Risks of chronic metabolic acidosis in patients with chronic kidney disease.
Kidney Int Suppl ;SS Kraut JA, Kurtz I: Metabolic acidosis of CKD: diagnosis, clinical characteristics, and treatment. Kovesdy CP, Anderson JE, Kalantar-Zadeh K: Association of serum bicarbonate levels with mortality in patients with non-dialysis-dependent CKD.
Driver TH, et al: Low serum bicarbonate and kidney function decline: the Multi-Ethnic Study of Atherosclerosis MESA. de Brito-Ashurst I, et al: Bicarbonate supplementation slows progression of CKD and improves nutritional status.
Mahajan A, et al: Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Phisitkul S, et al: Amelioration of metabolic acidosis in patients with low GFR reduced kidney endothelin production and kidney injury, and better preserved GFR.
Abramowitz MK, et al: Effects of oral sodium bicarbonate in patients with CKD. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease.
Kidney Int ; suppl Goraya N, et al: Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate.
Dobre M, et al: Persistent high serum bicarbonate and the risk of heart failure in patients with chronic kidney disease CKD : a report from the Chronic Renal Insufficiency Cohort CRIC study. J Am Heart Assoc ;4:pii:e Witham MD, et al: Does oral sodium bicarbonate therapy improve function and quality of life in older patients with chronic kidney disease and low-grade acidosis the BiCARB trial?
Study protocol for a randomized controlled trial. Trials ; Gaggl M, et al: Effect of oral sodium bicarbonate supplementation on progression of chronic kidney disease in patients with chronic metabolic acidosis: study protocol for a randomized controlled trial SoBic-Study.
Di Iorio B, et al: A prospective, multicenter, randomized, controlled study: the correction of metabolic acidosis with use of bicarbonate in Chronic Renal Insufficiency UBI Study. J Nephrol ; Tentori F, et al: Association of dialysate bicarbonate concentration with mortality in the Dialysis Outcomes and Practice Patterns Study DOPPS.
Moe S, et al: Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes KDIGO. Levin A, et al: Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease.
Tejwani V, Qian Q: Calcium regulation and bone mineral metabolism in elderly patients with chronic kidney disease. Nutrients ; Moranne O, et al: Timing of onset of CKD-related metabolic complications. Reynolds JL, et al: Human vascular smooth muscle cells undergo vesicle-mediated calcification in response to changes in extracellular calcium and phosphate concentrations: a potential mechanism for accelerated vascular calcification in ESRD.
Mathew S, et al: The mechanism of phosphorus as a cardiovascular risk factor in CKD. Chen NX, Moe SM: Pathophysiology of vascular calcification. Curr Osteoporos Rep ; Goodman WG, et al: Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis.
O'Seaghdha CM, et al: Serum phosphorus predicts incident chronic kidney disease and end-stage renal disease. Kestenbaum B, et al: Serum phosphate levels and mortality risk among people with chronic kidney disease. Chartsrisak K, et al: Mineral metabolism and outcomes in chronic kidney disease stage patients.
Jung SY, et al: Electrolyte and mineral disturbances in septic acute kidney injury patients undergoing continuous renal replacement therapy. Medicine Baltimore ;e Da J, et al: Serum phosphorus and progression of CKD and mortality: a meta-analysis of cohort studies.
Dhingra R, et al: Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Tonelli M, Pfeffer MA: Kidney disease and cardiovascular risk. Annu Rev Med ; Larsson TE, et al: Conjoint effects of serum calcium and phosphate on risk of total, cardiovascular, and noncardiovascular mortality in the community.
Arterioscler Thromb Vasc Biol ; Gutierrez OM, et al: Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis.
Blood Purif ; Lee SK, Lorenzo JA: Parathyroid hormone stimulates TRANCE and inhibits osteoprotegerin messenger ribonucleic acid expression in murine bone marrow cultures: correlation with osteoclast-like cell formation. Endocrinology ; Armbrecht HJ, et al: Induction of the vitamin D hydroxylase CYP24 by 1,dihydroxyvitamin D3 is regulated by parathyroid hormone in UMR osteoblastic cells.
Shinki T, et al: Parathyroid hormone inhibits hydroxyvitamin Dhydroxylase mRNA expression stimulated by 1 alpha,dihydroxyvitamin D3 in rat kidney but not in intestine. J Biol Chem ; Brenza HL, DeLuca HF: Regulation of hydroxyvitamin D3 1alpha-hydroxylase gene expression by parathyroid hormone and 1,dihydroxyvitamin D3.
Arch Biochem Biophys ; Jeong HS, Dominguez AR: Calciphylaxis: controversies in pathogenesis, diagnosis and treatment. Am J Med Sci ; Holick MF: Vitamin D deficiency. Liu WC, et al: Pleiotropic effects of vitamin D in chronic kidney disease.
Clin Chim Acta ; Pilz S, et al: Vitamin D status and mortality risk in CKD: a meta-analysis of prospective studies. Schottker B, et al: Vitamin D and mortality: meta-analysis of individual participant data from a large consortium of cohort studies from Europe and the United States.
BMJ ;G Cheng Z, Lin J, Qian Q: Role of vitamin D in cognitive function in chronic kidney disease. Electrolytes carry an electric charge when dissolved in body fluids such as blood read more , help the body maintain normal fluid levels in the fluid compartments because the amount of fluid a compartment contains depends on the amount concentration of electrolytes in it.
If the electrolyte concentration is high, fluid moves into that compartment a process called osmosis. Likewise, if the electrolyte concentration is low, fluid moves out of that compartment.
To adjust fluid levels, the body can actively move electrolytes in or out of cells. Thus, having electrolytes in the right concentrations called electrolyte balance is important in maintaining fluid balance among the compartments. The kidneys help maintain electrolyte concentrations Water and electrolyte balance The kidneys are bean-shaped organs that figure prominently in the urinary tract.
Each is about 4 to 5 inches 12 centimeters long and weighs about one third of a pound grams. One lies read more by filtering electrolytes and water from blood, returning some to the blood, and excreting any excess into the urine.
Thus, the kidneys help maintain a balance between the electrolytes a person takes in every day by consuming food and beverages and the electrolytes and water that pass out of the body in the urine are excreted.
If the balance of electrolytes is disturbed, a person can develop health issues. For example, an electrolyte imbalance can result from the following:. Becoming dehydrated Dehydration Dehydration is a deficiency of water in the body.
Vomiting, diarrhea, excessive sweating, burns, kidney failure, and use of diuretics may cause dehydration.
People feel thirsty, and as dehydration read more or overhydrated Overhydration Overhydration is an excess of water in the body. read more. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge.
Brought to you by About Merck Merck Careers Research Worldwide. Disclaimer Privacy Terms of use Contact Us Veterinary Edition. IN THIS TOPIC.
The kidneys are essential for Electrolyte balance and kidney function the volume and composition Diabetic foot care bodily fluids. Bqlance Electrolyte balance and kidney function bxlance key regulatory systems involving the kidneys for bapance volume, sodium and potassium fynction, and the pH of bodily Electroltye. A most Ultra-pure ingredient sources concept for you to understand is how water and sodium regulation are integrated to defend the body against all possible disturbances in the volume and osmolarity of bodily fluids. Simple examples of such disturbances include dehydration, blood loss, salt ingestion, and plain water ingestion. Water balance is achieved in the body by ensuring that the amount of water consumed in food and drink and generated by metabolism equals the amount of water excreted. The consumption side is regulated by behavioral mechanisms, including thirst and salt cravings.Video
How the Kidneys Regulate Water BalanceElectrolyte balance and kidney function -
Which means the water content of the blood will impact sodium concentration as well. Some of the common causes of low sodium levels are as follows this is not an exhaustive list :. Once a low sodium level has been confirmed on blood testing, treatment will depend on what is the cause of low sodium, and even how quickly it has developed.
A rapid correction could be dangerous, especially when hyponatremia has persisted for a while. The most common cause of hypernatremia is an elevation in sodium created because of a deficit of water.
Hence, disease states associated with dehydration, or increased water loss from the body like diabetes insipidus can cause hypernatremia. The average person typically starts to get a strong sensation of thirst when sodium levels begin to go up in the blood. As long as they have access to water, the sodium level should come down.
The problem, however, arises if people do not have access to water, or if they lose too much water from the kidneys or the gut, or if they cannot sense thirst as can happen in elderly patients. Since most hypernatremia states involve dehydration, treatment strategies include administration of water-rich IV fluids or oral intake of water.
Here as some of the common causes of high sodium level in the blood:. Symptoms of abnormal sodium levels depend on the severity of the abnormality, and the rapidity of its development. They can range from mild symptoms like a headache to more severe ones like gait abnormalities, cramps, heart rhythm changes, etc.
One dreaded complication of excessively low sodium level is the risk of seizures. Langston C. Managing Fluid and Electrolyte Disorders in Kidney Disease. Vet Clin North Am Small Anim Prac t.
Hoorn EJ, Zietse R. Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J Am Soc Nephrol. Muhsin SA, Mount DB. Diagnosis and treatment of hypernatremia. Best Pract Res Clin Endocrinol Metab. Halawa I, Andersson T, Tomson T.
Hyponatremia and risk of seizures: a retrospective cross-sectional study. By Veeraish Chauhan, MD Veeraish Chauhan, MD, FACP, FASN, is a board-certified nephrologist who treats patients with kidney diseases and related conditions.
Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content.
Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services.
Use limited data to select content. List of Partners vendors. Magnesium imbalance can cause adverse neuromuscular effects, muscle defects, and cardiovascular problems. Severe magnesium imbalance is associated with hypotension, reduced heart rates, and in extreme cases, cardiac arrest.
Hypomagnesemia may also result in anorexia, weakness, lethargy, vomiting, and confusion. Phosphorus and Calcium Imbalance. Phosphorus and calcium have a reciprocal relationship as excessive levels of one are associated with the deficiency of the other. The most common complication associated with renal failure is increased phosphorus, hypocalcemia, and decreased calcium levels.
Failing kidneys cannot excrete excess phosphorus, which leads to decreased calcium levels, called hypocalcemia. It is commonly associated with mineral and bone disorder, a condition affecting the heart, blood vessels, and bones of a person with acute renal failure.
Although increased calcium and decreased potassium levels, called hypercalcemia, may be rare, patients with renal failure might also experience this complication due to other underlying seasons. Symptoms and Complications of Calcium and Phosphorus Imbalance.
Symptoms associated with calcium and phosphorus imbalance are muscle spasms, seizures, muscle imbalance, and cardiac arrhythmias. The most common complications in severe cases are mineral and bone disorders and cardiac failure. Acute renal failure, among other complications, results in an imbalance of electrolytes in the blood.
Electrolytes, such as potassium, magnesium, sodium, calcium, and phosphorus, have essential functions to perform in the body, and their excess or deficiency can be fatal. The most common complications related to electrolyte disturbances are hyperkalemia, hypernatremia, hypermagnesemia, and hypocalcemia.
Fortunately, if acute renal failure is reversed with replacement therapy, electrolyte imbalance and related complication can improve. Doctors test blood pressure to see if the blood flow around the circulatory system is normal, low, or high. Too low or high blood pressure can lead to significant health complications like stroke, cardiac arrest, kidney failure, or brain damage.
Acute renal failure leads to electrolyte disturbance, which, in severe. South Texas Renal Care Group offers everything from diagnostic testing and dialysis to guidance on kidney transplantation and clinical trial opportunities, right here in our modern, comfortable offices.
We have many locations throughout San Antonio and South Texas, so you can spend less time traveling and more time focusing on your health. At South Texas Renal Care Group, you have our undivided attention every step of the way. Powered by Stash Media Group. Pay My Bill Patient Portal Request An Appointment Careers Menu.
Facebook Linkedin Youtube. Follow Us! Facebook-f Linkedin Youtube Instagram. Close this search box. REFER A PATIENT. Home About About Us Our Awards Doctors Reza A. Ali, MD Carolina Arias, MD Varshi Broumand, MD, FASN Esteban Cedillo-Couvert, MD Pavan Devulapally, MD Carl E.
Dukes, MD, FACP, FASN Abhijeet Goyal, MD FRANÇOIS JO-HOY, MD M. Reza Mizani, MD, FASN Indraneel Mogarala, MD Steven Rosenblatt, MD, FASN Shirin R. Sharma, MD Saqib Z. Syed, MD Lauren E. Tarbox, MD Luis E.
Vélez, MD Naushad Zafar, MD Services Chronic Kidney Disease Management Dialysis Care Dialysis In-Center Dialysis At-Home High Blood Pressure Kidney Transplant Care Dialysis Access Clinical Research Trials For Patients Request An Appointment Patient Portal Our Videos Patient Education Patient Forms Our Blog Free Kidney Screening Download Our Brochure For Physicians Locations Clinic Locations Dialysis Centers Contact Us Request An Appointment Contact Us Careers In The Community Menu.
NEW PATIENT? CALL TODAY! Electrolyte Disturbance and Acute Kidney Failure. April 17, am. What is Acute Renal Failure? Signs and Symptoms of Acute Kidney Failure Patients with acute renal failure usually complain of nausea, confusion, fatigue, and low urine output. Electrolytes and Renal Function In a healthy individual, kidneys are in charge of excreting waste products or fluid buildup that helps maintain the normal homeostasis of electrolytes in the body.
Common Electrolyte Disturbances Malfunctioning kidneys alter the balance of electrolytes, leading to a disturbance in nerve or muscle impulses throughout the body, which can have serious health outcomes and even cause death.
Potassium Imbalance Kidneys regulate potassium in the human body by excreting the excess, maintaining the optimal potassium levels in the blood. Symptoms and Complications of Potassium Imbalance As an individual with acute kidney failure might not be able to secrete or retain as much potassium as needed, disturbing potassium levels in the blood can lead to several health risks.
Sodium Imbalance Sodium concentration is essential to maintain fluid and acid-base balance and helps regulate neuromuscular function. Symptoms and Complications of Sodium Imbalance Both hypernatremia and hyponatremia affect the central nervous system and are associated with symptoms like disorientation, muscular twitching, hypertension, seizures, and in worst cases, coma.
Magnesium Imbalance Kidneys play an essential role in maintaining magnesium levels in the body. Symptoms and Complications of Magnesium Imbalance Magnesium imbalance can cause adverse neuromuscular effects, muscle defects, and cardiovascular problems.
Phosphorus and Calcium Imbalance Phosphorus and calcium have a reciprocal relationship as excessive levels of one are associated with the deficiency of the other. Symptoms and Complications of Calcium and Phosphorus Imbalance Symptoms associated with calcium and phosphorus imbalance are muscle spasms, seizures, muscle imbalance, and cardiac arrhythmias.
Electroljte the kidneys are primarily responsible for the regulation of fluid and electrolyte balance, acute or chronic changes baalnce renal balancce can result in kdiney imbalances. Acutely, the Ekectrolyte of Electrolyte balance and kidney function of renal deterioration makes kidmey Electrolyte balance and kidney function and intervention critical to the prevention of complications and potentially fatal outcomes. For patients with chronic renal failure, nursing assessment and intervention are equally significant, since there is an absence of renal regulatory mechanisms. In renal failure, acute or chronic, one most commonly sees patients who have a tendency to develop hypervolemia, hyperkalemia, hyperphosphatemia, hypocalcemia, and bicarbonate deficiency metabolic acidosis. Sodium is generally retained, but may appear normal, or hyponatremic, because of dilution from fluid retention.
Absolut ist mit Ihnen einverstanden. Ich denke, dass es die ausgezeichnete Idee ist.
Ich entschuldige mich, aber mir ist es etwas mehr die Informationen notwendig.
Sie haben ins Schwarze getroffen. Ich denke, dass es der ausgezeichnete Gedanke ist.
Sie irren sich. Schreiben Sie mir in PM, wir werden besprechen.