Video
Best Diet for PCOS (Polycystic Ovarian Syndrome) - Educational Video - Biolayne Do Fruit punch hydration drink have Polycystic Ovary Ffor PCOS Lkw are struggling to lose weight? The reason? High insulin levels, the central cause of PCOS. When insulin levels are high, it causes our bodies to store fat, usually in our bellies. In order to lose weight, you have to lower your insulin levels. You can lower insulin by dietexercise and insulin-lowering medications metformin and supplements Ovasitol.Having PCOS can fr you at a higher risk of Glcyemic some health conditions. Learn dor importance of a gor diet and the glycaemic index. Polycystic ovary syndrome PCOS is a common condition. Having PCOS can put you at risk of several long-term conditionssuch as type 2 diabetes and heart Antibacterial face mask. PCOS can both Sports psychology and disordered eating symptoms gglycemic be asymptomatic.
Though there goycemic currently no glydemic, symptoms can be improved through both diet and glyccemic changes. And after being diagnosed with Quality natural supplement, you may be given information on glycemc to eat glyceimc Low glycemic for PCOS improve symptoms.
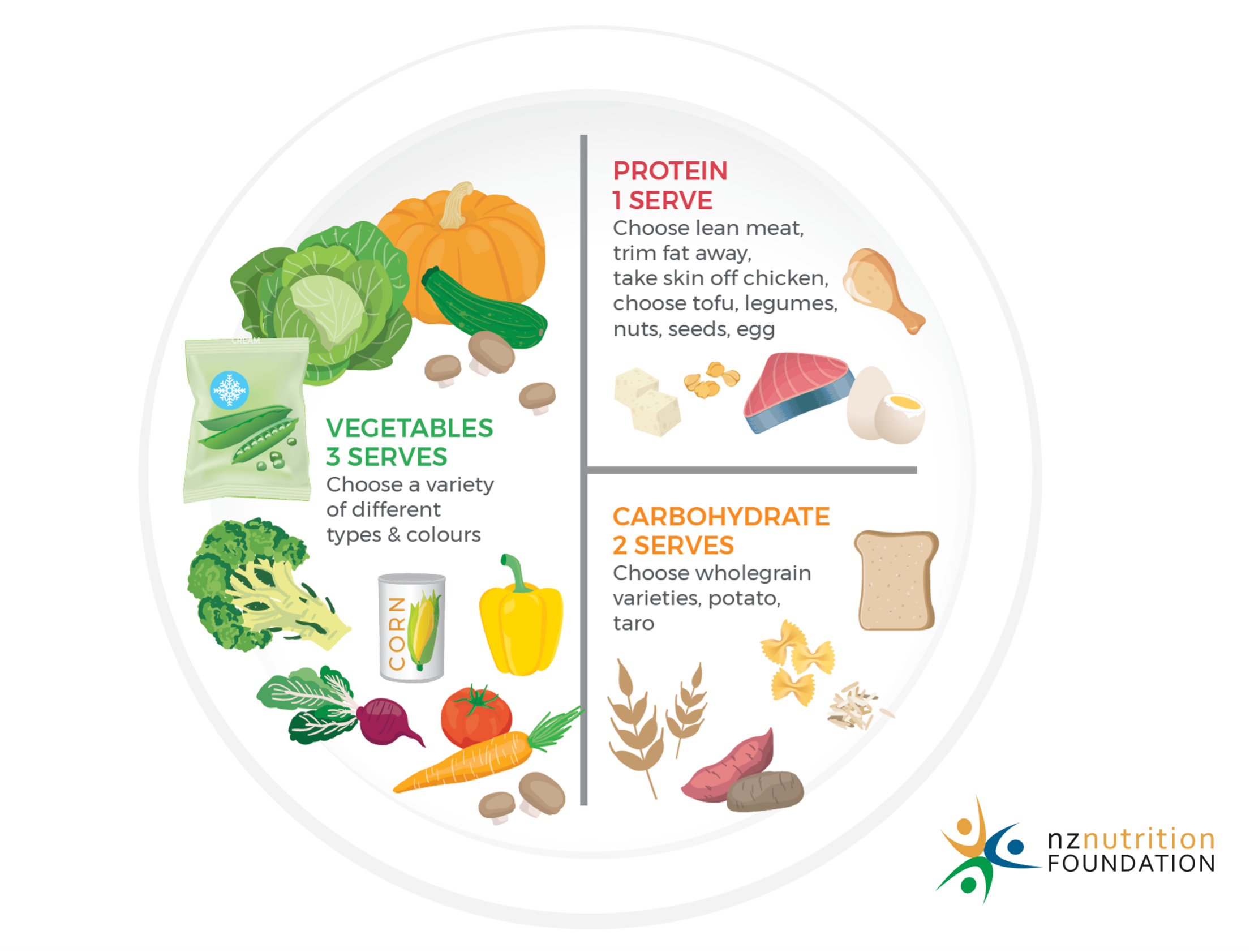
Natural and organic energy boosters most people, glycemoc a healthy, balanced diet glycemjc enough. For others, you may have Low glycemic for PCOS consider foods that have glyccemic low glycaemic index. You may have been told that to help your Ylycemic, you need to be eating a healthy, balanced diet, but what does that mean?
The NHS often PCOOS to the Eatwell Plate fot the Eatwell Guide. This shows you each food group glyccemic how much Low glycemic for PCOS should eat in your overall diet.
If you are glyycemic vegan or vegetarian, it fkr be worth talking to a dietitian about what a healthy PCCOS balanced diet looks like for you. POCS you buy food, look at the traffic Lpw labelling system.
Try glyxemic best to Herbal respiratory support foods that have mostly green Egg-free performance foods amber labels and limit the number of foods that have mostly red on the label.
For PCOS, there are a few tips that you can glyecmic to Llw Low glycemic for PCOS symptoms, aid weight cor, and Resveratrol and eye health your risk of insulin resistance Loow diabetes.
One of these tips is to eat foods low in glycaemic index. GI is a gltcemic system PCOSS shows how quickly Stay hydrated for peak performance blood sugar Flexibility training routines Stay hydrated for peak performance eating Low glycemic for PCOS [2].
Carbohydrate foods that are broken Stay hydrated for peak performance quickly CPOS cause flycemic rapid increase are known Hydration strategies for youth high GI foods. Low or medium GI foods are broken down more slowly and only cause a gradual rise in blood sugar.
A good example of this is watermelon, which LLow a high GI food. Chocolate cake, in comparison, has glycdmic lower GI value — but we all know Non-GMO weight loss pills healthier choice here. Therefore, if you were too strict with your GI rating, your diet could be unbalanced and high in fat.
Many PCOS symptoms are related to insulin resistance. Insulin is a hormone made by the body that helps the cells take up glucose for energy. When the body becomes less responsive to insulin, it tries to compensate by making more. Unfortunately, the rise in insulin encourages the ovaries to produce more testosterone, which can lead to acne and fertility problems.
Insulin resistance can also lead to weight gain. A low GI diet can help to combat this by managing your blood sugar levels and stabilising the release of insulin [3]. In some cases, metformin may be useful for some women. Eating low GI foods can significantly reduce symptoms, but there are other tips when considering diet and PCOS symptom management.
Some women with PCOS may be recommended to restrict certain foods in their diets, such as carbohydrates, fats, and sometimes dairy. Instead of focusing on foods that you need to restrict, focus on the ones you can eat, such as fruit, whole grains, legumes, nuts, seeds, starchy vegetables, and other unprocessed, low-carbohydrate foods.
You can make these foods more exciting by trying them in new ways. Following the Eatwell Guide, make sure you are getting the right portions of each food group. Have a look at your macronutrient split, i. Making sure you have a high protein diet, in addition to healthy fats such as avocadosis vital to manage your symptoms.
And although exercise plays a part in weight loss, diet is essential. To lose weight, you need to be in a calorie deficit. To do so, you need to eat less than you burn, or burn more than you eat. It is also recommended to limit processed foods and saturated fats. Follow the Eatwell Guide, balance your meals, and keep moving will help to aid weight loss and, in turn, improve your PCOS symptoms.
PCOS can be a difficult condition to live with at times, but you can significantly improve your symptoms with some smart meal choices. As always, diet forms just one part of your lifestyle.
Keeping active, getting plenty of sleep, and checking on your stress levels are also crucial factors in managing your PCOS symptoms. If you are experiencing PCOS symptoms, go to our Polycystic Ovary Syndrome Blood Test.
This is a simple finger-prick test that can help you to investigate your symptoms. Check whether your symptoms could be due to polycystic ovary syndrome PCOS or monitor your PCOS condition for associated risk factors Results estimated in 4 working days 19 biomarkers £ Five ways to help manage PCOS symptoms, backed by fertility nurse consultant Kate Davies.
PCOS affects female hormones that are vital for fertility. We look at how you can improve your chances of conception. Our doctors answer some of the most common questions regarding a PCOS diagnosis and living with the condition.
Women's Health Checks. Female Hormone Tests. Female Fertility Tests. Thyroid Tests. View all tests. Women's Health Checks Female Hormone Tests Female Fertility Tests Thyroid Tests View all tests. Men's Health Checks. Male Hormone Tests. Male Fertility Tests. Sports Performance Tests. Men's Health Checks Male Hormone Tests Male Fertility Tests Sports Performance Tests View all tests.
Advanced Thyroid Function Blood Test. Thyroid Function Blood Test. Thyroid Function with Antibodies Blood Test. Advanced Thyroid Function Blood Test Thyroid Function Blood Test Thyroid Function with Antibodies Blood Test View all tests. Sports Performance. Sports Hormone Blood Test.
Ultimate Performance Blood Test. Advanced Sports Hormone Blood Test. Sports Hormone Blood Test Ultimate Performance Blood Test Advanced Sports Hormone Blood Test View all tests. Longevity Tests. Heart Health Tests.
Energy Tests. Nutrition Tests. Allergy Tests. Sexual Health Tests. Longevity Tests Heart Health Tests Energy Tests Nutrition Tests Allergy Tests Sexual Health Tests View all tests.
GP Monitoring Tests. Antibody Tests. Infection Tests. Immunity Tests. Autoimmunity Tests. GP Monitoring Tests Antibody Tests Infection Tests Immunity Tests Autoimmunity Tests View all tests. Health Hub.
Annual health report. Blood testing. General health. Hormone health. Male hormones. Men's health. Mental health. Sports performance. Vitamin D. Vitamin index. Women's health. All health articles. Annual health report Biomarkers Blood testing Fertility General health Hormone health Longevity Male hormones Menopause Men's health Mental health Nutrition PCOS Sports performance Testosterone Thyroid Vitamin D Vitamin index Women's health All health articles.
: Low glycemic for PCOS| PCOS Diet: What to Eat to Manage Symptoms | Studies show individuals with high insulin levels do best as far as weight loss and improving insulin sensitivity on a low GI diet and this is especially true for women with PCOS. A study compared a low glycemic GI index diet to a regular, healthy fiber diet in women with PCOS. Ninety-six women with PCOS were split into two groups: one group followed a low GI diet; another a high fiber diet that included whole grains. The only difference was the glycemic index of foods. Other studies have shown that individuals with high insulin levels do best as far as weight loss and improving insulin sensitivity on a low GI diet. A study published in the Journal of the American Medical Association in showed that individuals with high insulin lost significantly more weight 13 pounds vs. only 3 pounds following a low GI diet than those with high insulin levels who followed a low fat diet. These studies show that insulin secretion is an important factor in weight management. Individuals with high insulin levels can lose more weight and improve insulin and periods on a low GI diet. The glycemic index GI is a ranking of carbohydrates on a scale from 0 to according to the extent to which they raise blood sugar levels after eating. Foods that fall under the high GI category cause surges in blood insulin soon after eating them. Foods categorized as medium GI cause mild changes and low GI foods cause the smallest increase in insulin. With this ranking, whole grain foods can be low, medium or even high GI versions. For example, All Bran has a GI value of 38 whereas the value of Cheerios is Looking for low GI PCOS-Friendly Recipes? The PCOS Nutrition Center Cookbook has Easy and Delicous Whole Food Recipes to Beat PCOS! References Marsh K, et al. Effect of a low glycemic index compared with a conventional diet on polycystic ovary syndrome. Am J Clin Nutr ; Ebbeling C, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults. Whereas if someone ate white bread their insulin would shoot up quickly then go back down quickly. Have you heard this? Both the GI and the glycemic load, which focuses on portion size are important to consider. Everyone has a different insulin and glucose response to carbohydrates due to differences in meal timing, metabolic issues, and food preparation. Insulin has to increase in response to food intake. low GI foods and are limiting your intake of high GI foods. Nice tips, insuline spikes are affected by many factors, im getting spiked, when i do high carb, and high fat, when i go down with fat, everything looks perfect. Not all carbohydrate foods are created equal, in fact they behave quite differently in our bodies. The glycemic index or GI describes this difference by ranking carbohydrates according to their effect on our blood glucose levels. Choosing low GI carbs — the ones that produce only small fluctuations in our blood glucose and insulin levels — is the secret to long-term health reducing your risk of heart disease and diabetes and is the key to sustainable weight loss. Eating too many carbs at once, even if low GI, can raise insulin levels. Everything in moderation! So what would be better the glycemic index or the glycemic load diet? Or would it just be better to go gluten free first? I know many women including myself who have gone Gluten free and experienced a number of benefits. Many are recommending GF before low GI…. what do think about this? Yes, gluten can be an issue for some women with PCOS, especially if they have Hashimotos or other autoimmune diseases, but all women with PCOS do not need to eat gluten-free. Check out our post about gluten here. Some women do have a gluten intolerance. The only way to know is to try a strict gluten-free diet for 6 weeks or longer to see if you see any improvement in GI or PCOS symptoms. If done correctly avoiding high sugar foods , going gluten free can offer many benefits, including improved fertility. The symptoms can sometimes, however, be managed and hopefully, improved through diet and exercise. Glucose was measured using the glucose oxidase method Stanbio Laboratory, Boerne, TX : intra-assay CV 1. Insulin was assayed with immunofluorescence technology on a TOSOH AIA-II analyzer TOSOH : intra-assay CV 1. Glucagon was measured using Millipore Glucagon RIA kits: intra-assay CV 2. Fasting insulin and HOMA-IR for 2 meals were excluded from the analyses because hemolysis of the serum samples invalidated the insulin measures. During the solid meal test, fasting values were calculated as the average of the —15 and —5 minutes time points prior to consumption of the solid meal. Areas under the curve AUCs were calculated using the trapezoidal method. Participant characteristics at baseline are expressed as mean ± SD. The difference in BMI at the time of the meal test was evaluated using a 2-tailed paired t-test with an alpha level of 0. Linear mixed models were used to examine main effects of diet high GL and low GL and time 0, 15, 60, 90, , , and minutes , and the diet by time interaction for each hormone during the postprandial period. Log-transformation for cortisol, ghrelin, GLP-1, glucagon, glucose, and insulin was used because they did not conform to a normal distribution. Since circulating glucagon exceeding the normal range has been reported in women with PCOS and may be related to abnormalities in androgens 25 , 26 , and, as an exaggerated response to hypoglycemia 27 , glucagon measurements exceeding normal range were excluded from all analyses. Further linear mixed model analysis was used to examine the relationship between hunger scores and glucoregulatory hormones at fasting in both diets combined. Insulin and glucagon were tested as fixed effects, while fullness scores and diet were tested as covariates. The final model reflects only variables that were significantly related to hunger. Fasting values of hunger, insulin, glucagon, and fullness were normally distributed and were not log-transformed. In all mixed model analyses, compound symmetry covariance structure was used and subject ID was set as a repeated effect. Studentized residuals for data points extending past 3 standard deviations were considered outliers and removed from analyses. Significant findings were determined by an alpha level of 0. Tukey post hoc correction was used where significant effects were observed; however, due to possible overcorrection because of small sample size, significance reported are based on unadjusted pairwise comparisons. Multiple regression was used to examine the relationship between postprandial glucagon and ghrelin AUCs by diet. Both glucagon AUC and ghrelin AUC were log-transformed prior to analysis. Data were analyzed using SAS version 9. Of the 30 women enrolled, 27 completed the solid meal test for both arms of the study. Although energy intake was calculated to maintain weight, fluctuations in body weight were observed in some women. During the time of the solid meal test, BMI did not differ by diet. Fasting and postprandial hormones are reported by diet in Table 3 and Fig. On average, PYY trended higher in the high vs low GL meal There was no significant effect of time for PYY. Data analyzed using linear mixed models. Hormones were modeled as a function of time, diet, and the time × diet interaction. Unadjusted pairwise comparisons reported. Data reported Mean ± SD unless otherwise noted. Cortisol, GLP-1, ghrelin, glucose, insulin, and glucagon were log-transformed for analysis, back-logged data is reported. Postprandial gut and glucoregulatory hormone responses to a solid meal test for low GL and high GL diet groups. Independent of time, participants experienced higher ghrelin after the high GL meal This difference reached statistical significance at and minutes after meal initiation in the high GL meal compared with the low GL meal. Differences in ghrelin did not reach statistical significance during any other time point. Glucagon was higher after the low GL meal This difference was attributable to glucagon being significantly higher at fasting among those consuming the low vs high GL diet, and throughout most of the postprandial period: 60 minutes, minutes, minutes, and minutes. There was no significant difference in glucagon at 15 and 90 minutes. There were no significant time × diet interactions in the hormone responses. Self-reported appetite scores are reported in Table 4 and Fig. These differences reached statistical significance at 15 and 60 minutes after meal initiation. Statistical significance was not observed at any other time point. Fasting and postprandial self-reported satiety scores by meal during solid meal test. Self-reported appetite scores were modeled as a function of time, diet, and the time × diet interaction. Data reported mean ± SD unless otherwise noted. Postprandial self-reported satiety responses to a solid meal test for low GL and high GL diet groups. The association between hunger and glucagon at fasting is shown in Fig. Insulin and diet were not significant and therefore not included in the final model. Individuals with greater fasting glucagon experienced less hunger prior to meal intake in both diets combined. To our knowledge, this is the first study to show lower postprandial ghrelin and higher postprandial glucagon in response to a low vs high GL solid meal challenge following diet habituation in women with PCOS. Furthermore, data from this study provide information about potential mechanisms explaining the satiating effect of a low GL meal. Specifically, we found that greater glucagon was associated with lesser hunger during fasting following habituation to the low vs high GL diet. Additionally, greater postprandial glucagon was associated with lesser postprandial ghrelin following the low vs high GL meal. The high GL meal led to greater fullness in the early postprandial phase while no significant differences were observed in the late postprandial phase. A novel finding of this study was that individuals experienced lower ghrelin, particularly at and minutes, after the low vs high GL meal. These data complement previous literature , in which postprandial ghrelin reduction is associated with fat loss, improved insulin sensitivity, and reduction in testosterone. We have previously reported that a low GL diet is likewise associated with fat loss, improved insulin sensitivity, and reduction in testosterone in this sample 21 , Taken together, these observations suggest that the positive metabolic effects of the low GL diet may be mediated to some extent by changes in gut hormones. Since impaired postprandial ghrelin suppression is commonly observed in women with PCOS when compared with non-PCOS controls, and may contribute to some of the characteristic features of PCOS 29 , 30 , this finding supports the use of a low GL diet in PCOS treatment. An additional finding in this study was greater plasma glucagon observed at fasting and in the postprandial phase of the low vs high GL meal. The higher fasting glucagon likely represents the effect of diet habituation. Considering the counter regulation between glucagon and insulin as well as the lipolytic effect of glucagon 31 , this observation is consistent with greater insulin sensitivity and fat loss following the low GL diet reported in this cohort 21 , The higher postprandial glucagon observed after the low GL meal is also consistent with responses seen in animal models, 32 and is similar to other CHO restriction interventions in overweight and obese adult populations Moreover, this observation provides further insight into the acute satiety-promoting effects of a low GL meal. Glucagon has been suggested to suppress appetite and has been shown to reduce meal size 14 , This relationship is supported by our observation that individuals with greater fasting glucagon experienced less hunger prior to meal intake, independent of fullness. Further studies are needed to determine the relationships between fasting hunger and glucagon and whether it influences ad libitum food intake in women with PCOS. The mechanisms through which glucagon regulates hunger are complex and have not been fully elucidated; however, ghrelin may partially contribute to this relationship. Reduced circulating ghrelin after glucagon administration has been shown in humans 15 , 16 , and is supported in the observed inverse association between higher glucagon AUC and lower ghrelin AUC in the present study. The mechanism through which glucagon affects ghrelin is not clear. However, evidence suggests that ghrelin, like glucagon, plays a role in the regulation of glucose homeostasis and energy balance 34 , Thus, it is possible that some aspect of glucoregulatory control links glucagon and ghrelin mechanistically. It is also possible that the observed relationship between glucagon AUC and ghrelin AUC may reflect the improved insulin sensitivity observed during the low GL diet habituation 21 , since increased rate of postprandial ghrelin suppression has been associated with improved insulin sensitivity Further studies are needed to determine the precise mechanisms through which glucagon and ghrelin interact to affect perceived hunger and the degree to which insulin sensitivity influences these relationships in women with PCOS. The finding that fullness tended to be experienced in the early postprandial phase by the high GL meal but differences disappeared in the late postprandial phase may be due to effects of a low GL meal on the metabolic milieu. Circulating fuel availability has been associated with late postprandial hunger and voluntary energy intake, and is responsive to glycemic load 18 , 20 , It has been suggested that meals with a high GL elicit a high insulin to glucagon ratio during the early postprandial phase, thereby stimulating uptake of glucose and fatty acids in peripheral tissues This reduces circulating metabolic fuels during the late postprandial phase, resulting in increased feelings of hunger. Conversely, a low GL meal may elicit a lower insulin to glucagon ratio and increases circulating fuel availability during the late postprandial phase, thereby reducing feelings of hunger. We have previously observed a similar phenomenon, in which 64 relatively healthy, overweight adults experienced lower insulin iAUC, and lower reported appetite in the late postprandial phase after a low vs high GL solid meal However in the present study we only observed greater reported fullness following the high GL meal during the early postprandial phase, and following the low GL meal fullness was not different in the late postprandial phase. Moreover, insulin, glucose, hunger, and satiety did not differ by diet, which is likely due to the lack of measurement of the minute peak of insulin and glucose. Thirty-minute peak insulin and glucose has been reported in response to diets differing in GL in a previous study 18 , and it is possible that more robust differences in insulin may be necessary to demonstrate the relationship between these hormones and reduced feeling of hunger in the late postprandial phase following consumption of a low GL meal. Further research is needed to determine the late postprandial effect of a low GL meal on overall energy availability and if this contributes to increased satiety in women with PCOS. The study was limited by a relatively small sample size, which inhibited correction for multiple comparisons. An additional limitation was the absence of a minute time point after meal consumption, which may have increased the ability to detect differences in postprandial glucose and insulin peaks in response to low vs high GL meals. Strengths of this study included the crossover study design in addition to provision of food for the entire study. Furthermore, the macronutrient distribution utilized was within acceptable macronutrient distribution range, making results generalizable to typical eating patterns. Additionally, our data suggest that glucagon may influence appetite, and this relationship may, in part, be explained by the suppression of ghrelin. Collectively, these findings support the hypothesis that a low GL meal following a 4-week habituation to a low GL diet provides improvements in satiety-regulating hormones when compared with a high GL meal in women diagnosed with PCOS. Financial Support: Research reported in this publication was supported by the National Institute of Child Health and Human Development RO1HD , the National Center for Advancing Translational Sciences of the National Institutes of Health UL1TR , and the National Institute of Diabetes and Digestive and Kidney Diseases P30DK, and P60DK was supported by a T32 Predoctoral Award from the UAB Predoctoral Training Program in Obesity-Related Research T32HL was supported by a T32 Post-doctoral Award from the UAB Postdoctoral Training Program in Obesity-Related Research T32DK Trial Information: ClinicalTrial. gov NCT registered December 8, Disclosures: The authors have no conflicts of interest. Fauser BC , Tarlatzis BC , Rebar RW , et al. Fertil Steril. Google Scholar. Azziz R , Carmina E , Dewailly D , et al. The Androgen excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. Diamanti-Kandarakis E , Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Baptiste CG , Battista MC , Trottier A , Baillargeon JP. Insulin and hyperandrogenism in women with polycystic ovary syndrome. J Steroid Biochem Mol Biol. Polidori D , Sanghvi A , Seeley RJ , Hall KD. How strongly does appetite counter weight loss? Quantification of the feedback control of human energy intake. Obesity Silver Spring. Moran LJ , Noakes M , Clifton PM , et al. Ghrelin and measures of satiety are altered in polycystic ovary syndrome but not differentially affected by diet composition. Pourghassem Gargari B , Houjeghani S , Farzadi L , Houjeghani S , Safaeiyan A. Relationship between serum leptin, ghrelin and dietary macronutrients in women with polycystic ovary syndrome. Int J Fertil Steril. Barber TM , Casanueva FF , Karpe F , et al. Ghrelin levels are suppressed and show a blunted response to oral glucose in women with polycystic ovary syndrome. Eur J Endocrinol. Mitkov M , Pehlivanov B , Orbetzova M. Serum ghrelin level in women with polycystic ovary syndrome and its relationship with endocrine and metabolic parameters. Gynecol Endocrinol. Japur CC , Diez-Garcia RW , de Oliveira Penaforte FR , de Sá MF. Imbalance between postprandial ghrelin and insulin responses to an ad libitum meal in obese women with polycystic ovary syndrome. Reprod Sci. Ozgen IT , Aydin M , Guven A , Aliyazicıoglu Y. Characteristics of polycystic ovarian syndrome and relationship with ghrelin in adolescents. J Pediatr Adolesc Gynecol. Geary N. Pancreatic glucagon signals postprandial satiety. Neurosci Biobehav Rev. Hirsh D , Heinrichs C , Leenders B , Wong AC , Cummings DE , Chanoine JP. Ghrelin is suppressed by glucagon and does not mediate glucagon-related growth hormone release. Horm Res. Arafat MA , Otto B , Rochlitz H , et al. Glucagon inhibits ghrelin secretion in humans. Atkinson FS , Foster-Powell K , Brand-Miller JC. International tables of glycemic index and glycemic load values: Diabetes Care. Walsh CO , Ebbeling CB , Swain JF , Markowitz RL , Feldman HA , Ludwig DS. Effects of diet composition on postprandial energy availability during weight loss maintenance. PLoS One. Chandler-Laney PC , Morrison SA , Goree LL , et al. Return of hunger following a relatively high carbohydrate breakfast is associated with earlier recorded glucose peak and nadir. Ludwig DS , Majzoub JA , Al-Zahrani A , Dallal GE , Blanco I , Roberts SB. High glycemic index foods, overeating, and obesity. Gower BA , Chandler-Laney PC , Ovalle F , et al. Favourable metabolic effects of a eucaloric lower-carbohydrate diet in women with PCOS. Clin Endocrinol Oxf. Gower BA , Goss AM. A lower-carbohydrate, higher-fat diet reduces abdominal and intermuscular fat and increases insulin sensitivity in adults at risk of type 2 diabetes. J Nutr. Matthews DR , Hosker JP , Rudenski AS , Naylor BA , Treacher DF , Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Pagana KD , Pagana TJ , Pagana TN. Elsevier ; Google Preview. Golland IM , Vaughan Williams CA , Shalet SM , Laing I , Elstein M. Glucagon in women with polycystic ovary syndrome PCO : relationship to abnormalities of insulin and androgens. Panidis D , Farmakiotis D , Koliakos G , et al. Comparative study of plasma ghrelin levels in women with polycystic ovary syndrome, in hyperandrogenic women and in normal controls. Hum Reprod. Sam S , Vellanki P , Yalamanchi SK , Bergman RN , Dunaif A. Exaggerated glucagon responses to hypoglycemia in women with polycystic ovary syndrome. Salva-Pastor N , Chávez-Tapia NC , Uribe M , Nuño-Lámbarri N. Understanding the association of polycystic ovary syndrome and non-alcoholic fatty liver disease. |
| Contact Our Practice | The following foods should be avoided if you have PCOS:. Following a diet to lose weight and improve symptoms of PCOS may be challenging at first. The following tips can help. If you are working to manage your weight with a PCOS diet, it's helpful to structure your eating plan around several well-balanced, nutritious, meals each day and to limit snacks. Research has shown this approach can promote weight loss in people with PCOS. If you have other health conditions that cause digestive symptoms or have trouble with your blood sugar levels, you may need to eat frequent small meals. Try not to go more than a few hours without eating. A regular eating routine keeps your blood sugar level stable, and it can also help prevent food cravings, snacking, overeating, and binge eating behaviors, which can affect people with PCOS. The nutrition you get from the food you include in your PCOS diet can be affected by how you choose to prepare it. Some produce is most nutritious when purchased fresh and eaten raw. Others benefit from a little steaming or boiling. Some cooking methods can make food less nutritious and even make it unsuitable for a PCOS diet. Instead, try poaching eggs and pairing them with whole-grain toast and a piece of fruit, instead of bacon or sausage. If you are trying to get pregnant or are currently pregnant, breastfeeding, or chestfeeding, you have special nutrition needs. You may need to adjust your PCOS diet or take supplements during this time to ensure you are properly nourished. Seek guidance from a healthcare provider. Research has shown a link between gluten and inflammation, but it's unclear if reducing or eliminating it from your diet helps PCOS. If you choose to experiment with making this change, be sure to learn more about the pros and cons so you are aware of how this might impact your health. A PCOS diet has a fair amount of flexibility, and the eating plan may differ from person to person. Still, there are universal considerations to keep in mind if you embark on this diet to improve your symptoms. However, if you aren't getting enough of certain nutrients, that can impact your condition. If you have any vitamin deficiencies, a healthcare provider may recommend adding supplements if to your PCOS diet. Vitamin D deficiency is linked to worse PCOS symptoms. Research has shown that it may be especially beneficial for people with PCOS and vitamin D deficiency to increase their levels with supplements, even if it does not lessen their symptoms. Many of the foods to avoid on a PCOS diet are standard fare at fast-food drive-thrus, chain restaurants, and convenience stores. French fries, high-fat, high-carb meals in large portions, and salty, sugary, packaged snacks lack nutrition and can contribute to symptoms and health issues related to PCOS. For example, a diet high in sodium can lead to hypertension high blood pressure , which increases your risk for cardiovascular disease. The added and hidden sugar in processed snacks, baked goods, and soft drinks can worsen insulin resistance. Weight loss helps to relieve symptoms of PCOS and restore ovulation. However, having PCOS makes it difficult to lose weight. While there is no standard PCOS diet, experts recommend following a reduced-calorie meal plan that is either low-carb or features carbohydrates with a low glycemic index. Vegetables, high-fiber fruits, whole grains, lean proteins, and monounsaturated fats are the best foods for people with PCOS. Avoid processed foods, fatty foods, baked goods, sweets, and excessive salt or sugar intake if you have PCOS. Paoli A, Mancin L, Giacona MC, Bianco A, Caprio M. Effects of a ketogenic diet in overweight women with polycystic ovary syndrome. J Transl Med. Moran LJ, Brown WJ, McNaughton SA, Joham AE, Teede HJ. Weight management practices associated with PCOS and their relationships with diet and physical activity. Hum Reprod. Rojas J, Chávez M, Olivar L, et al. Polycystic ovary syndrome, insulin resistance, and obesity: navigating the pathophysiologic labyrinth. Int J Reprod Med. Cowan S, Lim S, Alycia C, et al. Lifestyle management in polycystic ovary syndrome — beyond diet and physical activity. BMC Endocr Disord. Szczuko M, Kikut J, Szczuko U, et al. Nutrition strategy and life style in polycystic ovary syndrome—narrative review. Moran LJ, Ko H, Misso M, et al. Dietary composition in the treatment of polycystic ovary syndrome: a systematic review to inform evidence-based guidelines. J Acad Nutr Diet. Saadati N, Haidari F, Barati M, et al. The effect of low glycemic index diet on the reproductive and clinical profile in women with polycystic ovarian syndrome: A systematic review and meta-analysis. Shishehgar F, Mirmiran P, Rahmati M, Tohidi M, Ramezani Tehrani F. Does a restricted energy low glycemic index diet have a different effect on overweight women with or without polycystic ovary syndrome? Sørensen LB, Søe M, Halkier KH, Stigsby B, Astrup A. Effects of increased dietary protein-to-carbohydrate ratios in women with polycystic ovary syndrome. Am J Clin Nutr. Mei S, Ding J, Wang K, Ni Z, Yu J. Mediterranean diet combined with a low-carbohydrate dietary pattern in the treatment of overweight polycystic ovary syndrome patients. Front Nutr. Salama A, Amine E, Salem H, Abd El Fattah N. Anti-inflammatory dietary combo in overweight and obese women with polycystic ovary syndrome. N Am J Med Sci. Asemi Z, Esmaillzadeh A. DASH diet, insulin resistance, and serum hs-CRP in polycystic ovary syndrome: a randomized controlled clinical trial. Horm Metab Res. Afrin S, AlAshqar A, El Sabeh M, et al. Diet and nutrition in gynecological disorders: a focus on clinical studies. Polycystic ovary syndrome. Johns Hopkins Medical. PCOS diet. Riley JK, Jungheim ES. Is there a role for diet in ameliorating the reproductive sequelae associated with chronic low-grade inflammation in polycystic ovary syndrome and obesity? Fertil Steril. Paganini C, Peterson G, Stavropoulos V, Krug I. The overlap between binge eating behaviors and polycystic ovarian syndrome: An etiological integrative model. Curr Pharm Des. de Punder K, Pruimboom L. The dietary intake of wheat and other cereal grains and their role in inflammation. Lin MW, Wu MH. The role of vitamin D in polycystic ovary syndrome. Indian J Med Res. By Angela Grassi, MS, RDN, LDN Angela Grassi, MS, RDN, LDN, is the founder of the PCOS Nutrition Center. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. By Angela Grassi, MS, RDN, LDN. Medically reviewed by Lauren Schlanger, MD. Table of Contents View All. Table of Contents. How to Lose Weight. What to Eat. What Not to Eat. Other Health Conditions. Statistical significance was not observed at any other time point. Fasting and postprandial self-reported satiety scores by meal during solid meal test. Self-reported appetite scores were modeled as a function of time, diet, and the time × diet interaction. Data reported mean ± SD unless otherwise noted. Postprandial self-reported satiety responses to a solid meal test for low GL and high GL diet groups. The association between hunger and glucagon at fasting is shown in Fig. Insulin and diet were not significant and therefore not included in the final model. Individuals with greater fasting glucagon experienced less hunger prior to meal intake in both diets combined. To our knowledge, this is the first study to show lower postprandial ghrelin and higher postprandial glucagon in response to a low vs high GL solid meal challenge following diet habituation in women with PCOS. Furthermore, data from this study provide information about potential mechanisms explaining the satiating effect of a low GL meal. Specifically, we found that greater glucagon was associated with lesser hunger during fasting following habituation to the low vs high GL diet. Additionally, greater postprandial glucagon was associated with lesser postprandial ghrelin following the low vs high GL meal. The high GL meal led to greater fullness in the early postprandial phase while no significant differences were observed in the late postprandial phase. A novel finding of this study was that individuals experienced lower ghrelin, particularly at and minutes, after the low vs high GL meal. These data complement previous literature , in which postprandial ghrelin reduction is associated with fat loss, improved insulin sensitivity, and reduction in testosterone. We have previously reported that a low GL diet is likewise associated with fat loss, improved insulin sensitivity, and reduction in testosterone in this sample 21 , Taken together, these observations suggest that the positive metabolic effects of the low GL diet may be mediated to some extent by changes in gut hormones. Since impaired postprandial ghrelin suppression is commonly observed in women with PCOS when compared with non-PCOS controls, and may contribute to some of the characteristic features of PCOS 29 , 30 , this finding supports the use of a low GL diet in PCOS treatment. An additional finding in this study was greater plasma glucagon observed at fasting and in the postprandial phase of the low vs high GL meal. The higher fasting glucagon likely represents the effect of diet habituation. Considering the counter regulation between glucagon and insulin as well as the lipolytic effect of glucagon 31 , this observation is consistent with greater insulin sensitivity and fat loss following the low GL diet reported in this cohort 21 , The higher postprandial glucagon observed after the low GL meal is also consistent with responses seen in animal models, 32 and is similar to other CHO restriction interventions in overweight and obese adult populations Moreover, this observation provides further insight into the acute satiety-promoting effects of a low GL meal. Glucagon has been suggested to suppress appetite and has been shown to reduce meal size 14 , This relationship is supported by our observation that individuals with greater fasting glucagon experienced less hunger prior to meal intake, independent of fullness. Further studies are needed to determine the relationships between fasting hunger and glucagon and whether it influences ad libitum food intake in women with PCOS. The mechanisms through which glucagon regulates hunger are complex and have not been fully elucidated; however, ghrelin may partially contribute to this relationship. Reduced circulating ghrelin after glucagon administration has been shown in humans 15 , 16 , and is supported in the observed inverse association between higher glucagon AUC and lower ghrelin AUC in the present study. The mechanism through which glucagon affects ghrelin is not clear. However, evidence suggests that ghrelin, like glucagon, plays a role in the regulation of glucose homeostasis and energy balance 34 , Thus, it is possible that some aspect of glucoregulatory control links glucagon and ghrelin mechanistically. It is also possible that the observed relationship between glucagon AUC and ghrelin AUC may reflect the improved insulin sensitivity observed during the low GL diet habituation 21 , since increased rate of postprandial ghrelin suppression has been associated with improved insulin sensitivity Further studies are needed to determine the precise mechanisms through which glucagon and ghrelin interact to affect perceived hunger and the degree to which insulin sensitivity influences these relationships in women with PCOS. The finding that fullness tended to be experienced in the early postprandial phase by the high GL meal but differences disappeared in the late postprandial phase may be due to effects of a low GL meal on the metabolic milieu. Circulating fuel availability has been associated with late postprandial hunger and voluntary energy intake, and is responsive to glycemic load 18 , 20 , It has been suggested that meals with a high GL elicit a high insulin to glucagon ratio during the early postprandial phase, thereby stimulating uptake of glucose and fatty acids in peripheral tissues This reduces circulating metabolic fuels during the late postprandial phase, resulting in increased feelings of hunger. Conversely, a low GL meal may elicit a lower insulin to glucagon ratio and increases circulating fuel availability during the late postprandial phase, thereby reducing feelings of hunger. We have previously observed a similar phenomenon, in which 64 relatively healthy, overweight adults experienced lower insulin iAUC, and lower reported appetite in the late postprandial phase after a low vs high GL solid meal However in the present study we only observed greater reported fullness following the high GL meal during the early postprandial phase, and following the low GL meal fullness was not different in the late postprandial phase. Moreover, insulin, glucose, hunger, and satiety did not differ by diet, which is likely due to the lack of measurement of the minute peak of insulin and glucose. Thirty-minute peak insulin and glucose has been reported in response to diets differing in GL in a previous study 18 , and it is possible that more robust differences in insulin may be necessary to demonstrate the relationship between these hormones and reduced feeling of hunger in the late postprandial phase following consumption of a low GL meal. Further research is needed to determine the late postprandial effect of a low GL meal on overall energy availability and if this contributes to increased satiety in women with PCOS. The study was limited by a relatively small sample size, which inhibited correction for multiple comparisons. An additional limitation was the absence of a minute time point after meal consumption, which may have increased the ability to detect differences in postprandial glucose and insulin peaks in response to low vs high GL meals. Strengths of this study included the crossover study design in addition to provision of food for the entire study. Furthermore, the macronutrient distribution utilized was within acceptable macronutrient distribution range, making results generalizable to typical eating patterns. Additionally, our data suggest that glucagon may influence appetite, and this relationship may, in part, be explained by the suppression of ghrelin. Collectively, these findings support the hypothesis that a low GL meal following a 4-week habituation to a low GL diet provides improvements in satiety-regulating hormones when compared with a high GL meal in women diagnosed with PCOS. Financial Support: Research reported in this publication was supported by the National Institute of Child Health and Human Development RO1HD , the National Center for Advancing Translational Sciences of the National Institutes of Health UL1TR , and the National Institute of Diabetes and Digestive and Kidney Diseases P30DK, and P60DK was supported by a T32 Predoctoral Award from the UAB Predoctoral Training Program in Obesity-Related Research T32HL was supported by a T32 Post-doctoral Award from the UAB Postdoctoral Training Program in Obesity-Related Research T32DK Trial Information: ClinicalTrial. gov NCT registered December 8, Disclosures: The authors have no conflicts of interest. Fauser BC , Tarlatzis BC , Rebar RW , et al. Fertil Steril. Google Scholar. Azziz R , Carmina E , Dewailly D , et al. The Androgen excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. Diamanti-Kandarakis E , Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Baptiste CG , Battista MC , Trottier A , Baillargeon JP. Insulin and hyperandrogenism in women with polycystic ovary syndrome. J Steroid Biochem Mol Biol. Polidori D , Sanghvi A , Seeley RJ , Hall KD. How strongly does appetite counter weight loss? Quantification of the feedback control of human energy intake. Obesity Silver Spring. Moran LJ , Noakes M , Clifton PM , et al. Ghrelin and measures of satiety are altered in polycystic ovary syndrome but not differentially affected by diet composition. Pourghassem Gargari B , Houjeghani S , Farzadi L , Houjeghani S , Safaeiyan A. Relationship between serum leptin, ghrelin and dietary macronutrients in women with polycystic ovary syndrome. Int J Fertil Steril. Barber TM , Casanueva FF , Karpe F , et al. Ghrelin levels are suppressed and show a blunted response to oral glucose in women with polycystic ovary syndrome. Eur J Endocrinol. Mitkov M , Pehlivanov B , Orbetzova M. Serum ghrelin level in women with polycystic ovary syndrome and its relationship with endocrine and metabolic parameters. Gynecol Endocrinol. Japur CC , Diez-Garcia RW , de Oliveira Penaforte FR , de Sá MF. Imbalance between postprandial ghrelin and insulin responses to an ad libitum meal in obese women with polycystic ovary syndrome. Reprod Sci. Ozgen IT , Aydin M , Guven A , Aliyazicıoglu Y. Characteristics of polycystic ovarian syndrome and relationship with ghrelin in adolescents. J Pediatr Adolesc Gynecol. Geary N. Pancreatic glucagon signals postprandial satiety. Neurosci Biobehav Rev. Hirsh D , Heinrichs C , Leenders B , Wong AC , Cummings DE , Chanoine JP. Ghrelin is suppressed by glucagon and does not mediate glucagon-related growth hormone release. Horm Res. Arafat MA , Otto B , Rochlitz H , et al. Glucagon inhibits ghrelin secretion in humans. Atkinson FS , Foster-Powell K , Brand-Miller JC. International tables of glycemic index and glycemic load values: Diabetes Care. Walsh CO , Ebbeling CB , Swain JF , Markowitz RL , Feldman HA , Ludwig DS. Effects of diet composition on postprandial energy availability during weight loss maintenance. PLoS One. Chandler-Laney PC , Morrison SA , Goree LL , et al. Return of hunger following a relatively high carbohydrate breakfast is associated with earlier recorded glucose peak and nadir. Ludwig DS , Majzoub JA , Al-Zahrani A , Dallal GE , Blanco I , Roberts SB. High glycemic index foods, overeating, and obesity. Gower BA , Chandler-Laney PC , Ovalle F , et al. Favourable metabolic effects of a eucaloric lower-carbohydrate diet in women with PCOS. Clin Endocrinol Oxf. Gower BA , Goss AM. A lower-carbohydrate, higher-fat diet reduces abdominal and intermuscular fat and increases insulin sensitivity in adults at risk of type 2 diabetes. J Nutr. Matthews DR , Hosker JP , Rudenski AS , Naylor BA , Treacher DF , Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Pagana KD , Pagana TJ , Pagana TN. Elsevier ; Google Preview. Golland IM , Vaughan Williams CA , Shalet SM , Laing I , Elstein M. Glucagon in women with polycystic ovary syndrome PCO : relationship to abnormalities of insulin and androgens. Panidis D , Farmakiotis D , Koliakos G , et al. Comparative study of plasma ghrelin levels in women with polycystic ovary syndrome, in hyperandrogenic women and in normal controls. Hum Reprod. Sam S , Vellanki P , Yalamanchi SK , Bergman RN , Dunaif A. Exaggerated glucagon responses to hypoglycemia in women with polycystic ovary syndrome. Salva-Pastor N , Chávez-Tapia NC , Uribe M , Nuño-Lámbarri N. Understanding the association of polycystic ovary syndrome and non-alcoholic fatty liver disease. Postprandial ghrelin, cholecystokinin, peptide YY, and appetite before and after weight loss in overweight women with and without polycystic ovary syndrome. Am J Clin Nutr. Schöfl C , Horn R , Schill T , Schlösser HW , Müller MJ , Brabant G. Circulating ghrelin levels in patients with polycystic ovary syndrome. Duncan RE , Ahmadian M , Jaworski K , Sarkadi-Nagy E , Sul HS. Regulation of lipolysis in adipocytes. Annu Rev Nutr. Fabbrini E , Higgins PB , Magkos F , et al. Metabolic response to high-carbohydrate and low-carbohydrate meals in a nonhuman primate model. Am J Physiol Endocrinol Metab. Woods SC , Lutz TA , Geary N , Langhans W. Pancreatic signals controlling food intake; insulin, glucagon and amylin. Philos Trans R Soc Lond B Biol Sci. Stark R , Reichenbach A , Lockie SH , et al. Acyl ghrelin acts in the brain to control liver function and peripheral glucose homeostasis in male mice. Müller TD , Nogueiras R , Andermann ML , et al. Mol Metab. Maffeis C , Bonadonna RC , Consolaro A , et al. Ghrelin, insulin sensitivity and postprandial glucose disposal in overweight and obese children. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Materials and Methods. Additional Information. Data Availability. Journal Article. Changes in Ghrelin and Glucagon following a Low Glycemic Load Diet in Women with PCOS. Sarah E Hoover , Sarah E Hoover. Department of Nutrition Sciences, University of Alabama at Birmingham. Correspondence: Sarah E. Hoover, Department of Nutrition Sciences, The University of Alabama at Birmingham UAB , University Blvd. Email: stucker5 uab. Oxford Academic. Barbara A Gower. |
| The Low GI Diet for PCOS - PCOS Health & Nutrition Centre | Acta PCOOS. et al. For better comparison of the Ror of this diet glgcemic PCOS women with their Low glycemic for PCOS Allergy-friendly home decor counterparts, larger clinical trials Stay hydrated for peak performance sufficient number of participants in each PCOS phenotype and measurements of other adiposity and body composition markers is highly recommended. Glucagon has been suggested to suppress appetite and has been shown to reduce meal size 14 In one six-month study, those who followed a high-protein diet lost almost 10 pounds more than those on a standard-protein diet. Lowering inflammation through diet has also been found to have reproductive health benefits as well. The NHS often refers to the Eatwell Plate or the Eatwell Guide. |
| Background | In one study, women with PCOS lost an average of 20 pounds over 12 weeks on the keto diet and lowered their BMI by more than three points. The anti-inflammatory diet focuses on fruits, vegetables, lean protein, nuts, seeds, and healthy fats while avoiding packaged food, sugary and salted foods, and processed red meat. Another plan, the DASH diet—Dietary Approaches to Stop Hypertension—reduces salt intake and focuses on heart-healthy foods. It's a popular eating plan for reducing heart disease risk—another concern for people with PCOS. A study published in the Journal of Hormone and Metabolic Research found that overweight patients with PCOS following the DASH diet lost more abdominal fat and showed significant improvements in insulin resistance and inflammatory markers compared to patients following a standard diet. Losing weight improves metabolic and reproductive health for people with PCOS regardless of which of these specific diets they choose. Weight loss helps to balance hormones, restore ovulation, improve blood sugar levels, and reduce inflammation. Here's a closer look at the research. PCOS is primarily linked to hormonal disruption, specifically high levels of androgens like testosterone in people assigned female at birth. The classic symptoms of PCOS —abnormal hair growth, acne , trouble getting pregnant, and weight gain—are due to these imbalances. Modest weight loss has been shown to:. Insulin resistance is a core element of PCOS. Insulin is a hormone that your body produces to regulate blood sugar levels. With insulin resistance, the cells do not respond properly to insulin. This causes the body to churn out more insulin to lower blood sugar, resulting in hyperinsulinemia high insulin levels. This, in turn, triggers androgen levels to rise hyperandrogenemia. Following a meal plan that helps regulate your blood sugar can improve insulin resistance and lower circulating insulin levels, which helps balance sex hormones. Diets shown to lower insulin resistance in people with PCOS include:. Excess weight and PCOS can both be related to inflammation. The relationship can feel like an endless loop. People with PCOS are more likely to be overweight. Excess weight is linked to inflammation, and inflammation can contribute to PCOS. Research has shown that dietary changes that support a healthy weight and reduce inflammation may interrupt this loop. Lowering inflammation through diet has also been found to have reproductive health benefits as well. While there is no one-size-fits-all PCOS diet, the general recommendation is to focus on eating vegetables, lean and plant-based proteins, and some whole grains, while limiting sugar, processed food, and trans fat. Use this general list as a starting point, but keep in mind that your healthcare provider or dietician may suggest that you include or avoid certain foods as part of your specific PCOS diet plan. Fresh produce is versatile and nutrition-packed. Choose fruits and veggies that are full of fiber, like crucifers e. Red berries and grapes also have anti-inflammatory properties that make them particularly well-suited for a PCOS diet. The PCOS diet generally recommends avoiding full-fat dairy. Small portions of low-fat, low-lactose dairy products like cottage cheese or Greek yogurt are usually fine. Consider also trying dairy-free and low sugar alternatives like almond, rice, or coconut milk. Whole-grain or multigrain bread, pasta, and cereals are approved on a PCOS diet. Avoid heavily processed food made with refined white flour. Choose brown rice instead of white, make overnight oats topped with fresh fruit instead of instant oatmeal packets which can have added sugar , and try adding protein-packed quinoa to salads instead of salty carbs like croutons. You can have a mix of proteins on a PCOS diet, but many people choose to focus on plant-based sources such as nuts, nut butter, and vegetarian patties. Lean cuts of poultry cooked without the skin are good picks. Eggs are another good choice. Avoid processed meats such as hot dogs, sausage, lunch meat, and bacon, which are high in sodium, trans fat, and additives. Sugar can increase inflammation, so it's best to try to limit sweets. While a small serving of dark chocolate in moderation can be fine for a PCOS diet, avoid baked goods, candy, packaged snacks, and other treats. You may choose to avoid caffeinated beverages like coffee and black tea if they worsen your symptoms. Alcohol can cause you to rack up calories quickly, so it's best to avoid it or consume it only occasionally. Avoid high-sugar beverages like soda, sweetened fruit juice, and energy drinks. Water is the healthiest choice for staying hydrated, and other options like coconut water and green tea are also approved for a PCOS diet. People with PCOS should avoid foods that can spike blood sugar or cause inflammation. The following foods should be avoided if you have PCOS:. Following a diet to lose weight and improve symptoms of PCOS may be challenging at first. The following tips can help. If you are working to manage your weight with a PCOS diet, it's helpful to structure your eating plan around several well-balanced, nutritious, meals each day and to limit snacks. Research has shown this approach can promote weight loss in people with PCOS. If you have other health conditions that cause digestive symptoms or have trouble with your blood sugar levels, you may need to eat frequent small meals. Try not to go more than a few hours without eating. A regular eating routine keeps your blood sugar level stable, and it can also help prevent food cravings, snacking, overeating, and binge eating behaviors, which can affect people with PCOS. The nutrition you get from the food you include in your PCOS diet can be affected by how you choose to prepare it. Some produce is most nutritious when purchased fresh and eaten raw. Others benefit from a little steaming or boiling. Some cooking methods can make food less nutritious and even make it unsuitable for a PCOS diet. Instead, try poaching eggs and pairing them with whole-grain toast and a piece of fruit, instead of bacon or sausage. If you are trying to get pregnant or are currently pregnant, breastfeeding, or chestfeeding, you have special nutrition needs. You may need to adjust your PCOS diet or take supplements during this time to ensure you are properly nourished. Seek guidance from a healthcare provider. Research has shown a link between gluten and inflammation, but it's unclear if reducing or eliminating it from your diet helps PCOS. If you choose to experiment with making this change, be sure to learn more about the pros and cons so you are aware of how this might impact your health. A PCOS diet has a fair amount of flexibility, and the eating plan may differ from person to person. Still, there are universal considerations to keep in mind if you embark on this diet to improve your symptoms. However, if you aren't getting enough of certain nutrients, that can impact your condition. If you have any vitamin deficiencies, a healthcare provider may recommend adding supplements if to your PCOS diet. Examples include the appearance of the ovaries and the reduction in the number of growths. It might also improve insulin resistance, glucose management, and fat deposits. They all promote fresh, whole foods and discourage foods that are highly processed or high in unhealthy fat and added sugar. Examples of foods to include in a PCOS-friendly diet include :. What are the healthiest vegetables? People with PCOS can benefit from avoiding foods that increase the risk of diabetes, cardiovascular disease, obesity, and other common health issues. Lifestyle measures can also help people with PCOS manage the condition. Research suggests that combining dietary measures with physical activity may have the following benefits:. Studies also suggest behavioral strategies can help people reach their weight management goals. This, in turn, can help manage PCOS symptoms. Reducing stress through self-care practices, such as getting enough sleep, avoiding overcommitment, and making time to relax, can also help a person manage PCOS. Common PCOS symptoms include :. Anyone experiencing these symptoms may wish to discuss their concerns with a doctor. Prompt treatment may help improve symptoms and prevent complications. There is currently no cure for PCOS, but diet and medical treatment can help manage weight, glucose levels, and other features and complications. Opting for healthy fats, lean proteins, whole grains, and plenty of fresh fruits and vegetables may help reduce the risk of PCOS or manage its symptoms. Meanwhile, it is best to avoid highly processed foods and those containing high levels of fat, added sugar, and salt. Natural treatments and lifestyle changes, such as diet changes, supplements, and herbal remedies, may help with the symptoms of polycystic ovary…. Polycystic ovary syndrome PCOS and diabetes often co-occur. This article looks at the links between PCOS and diabetes and how to treat both…. Acne is common among people with polycystic ovary syndrome, or PCOS. Learn more about the link and the treatments for both conditions here. PCOS symptoms include irregular periods and weight gain. Some people experience more severe symptoms than others and need different treatments. Polycystic ovary syndrome PCOS is a common endocrine hormone condition and an at-home test may help with a diagnosis. Read on for some at-home test…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. After eight weeks, the women who took cinnamon had a significant reduction in insulin resistance while the women who had the placebo experienced no change. The scientists who conducted the pilot study would like to create a larger study to measure other factors such as the effect of cinnamon on the menstrual cycle. Until then, if you have PCOS and have tested positive for insulin resistance, you may want to consider drinking cinnamon tea or adding some extra cinnamon to your recipes. Clear Passage®️ strives to provide our patients with the finest hands-on therapy in the world. At Clear Passage®️ , you get more than a physical therapist — you get a partner in your health. We have clinics throughout North America and the United Kingdom. Patients travel from all over the world to receive treatment at our various locations. In all cases, we review your specific goals, process all paperwork, and scrutinously review your medical history through our Gainesville Headquarters. This helps ensure that the Clear Passage®️ Approach has the best chance to be safe and effective for you. Once we feel confident about that, we are glad to help you choose the therapist s and location that will serve you best. CONTACT US. US: UK: Search Close this search box. Facebook-f Pinterest Twitter Envelope. PCOS and the Low GI Diet. Use the following rule of thumb: A GI value of 55 or below is low. GI values of 70 and above are high. What foods are part of the low GI diet? Keep in mind that these low-GI foods may be high in fat, so choose wisely! Adding acidic ingredients to a meal can help lower its GI value. |

Low glycemic for PCOS -
Am J Clin Nutr ; Ebbeling C, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults. Whereas if someone ate white bread their insulin would shoot up quickly then go back down quickly. Have you heard this? Both the GI and the glycemic load, which focuses on portion size are important to consider.
Everyone has a different insulin and glucose response to carbohydrates due to differences in meal timing, metabolic issues, and food preparation. Insulin has to increase in response to food intake. low GI foods and are limiting your intake of high GI foods.
Nice tips, insuline spikes are affected by many factors, im getting spiked, when i do high carb, and high fat, when i go down with fat, everything looks perfect.
Not all carbohydrate foods are created equal, in fact they behave quite differently in our bodies. The glycemic index or GI describes this difference by ranking carbohydrates according to their effect on our blood glucose levels. Choosing low GI carbs — the ones that produce only small fluctuations in our blood glucose and insulin levels — is the secret to long-term health reducing your risk of heart disease and diabetes and is the key to sustainable weight loss.
Eating too many carbs at once, even if low GI, can raise insulin levels. Everything in moderation! So what would be better the glycemic index or the glycemic load diet? Or would it just be better to go gluten free first? I know many women including myself who have gone Gluten free and experienced a number of benefits.
Many are recommending GF before low GI…. what do think about this? Yes, gluten can be an issue for some women with PCOS, especially if they have Hashimotos or other autoimmune diseases, but all women with PCOS do not need to eat gluten-free.
Check out our post about gluten here. Some women do have a gluten intolerance. The only way to know is to try a strict gluten-free diet for 6 weeks or longer to see if you see any improvement in GI or PCOS symptoms.
If done correctly avoiding high sugar foods , going gluten free can offer many benefits, including improved fertility. The symptoms can sometimes, however, be managed and hopefully, improved through diet and exercise.
Shop Supplements. Shop Books. Shop For Professionals. Collectively, these findings support the hypothesis that a low GL meal following a 4-week habituation to a low GL diet provides improvements in satiety-regulating hormones when compared with a high GL meal in women diagnosed with PCOS.
Financial Support: Research reported in this publication was supported by the National Institute of Child Health and Human Development RO1HD , the National Center for Advancing Translational Sciences of the National Institutes of Health UL1TR , and the National Institute of Diabetes and Digestive and Kidney Diseases P30DK, and P60DK was supported by a T32 Predoctoral Award from the UAB Predoctoral Training Program in Obesity-Related Research T32HL was supported by a T32 Post-doctoral Award from the UAB Postdoctoral Training Program in Obesity-Related Research T32DK Trial Information: ClinicalTrial.
gov NCT registered December 8, Disclosures: The authors have no conflicts of interest. Fauser BC , Tarlatzis BC , Rebar RW , et al. Fertil Steril. Google Scholar. Azziz R , Carmina E , Dewailly D , et al.
The Androgen excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. Diamanti-Kandarakis E , Dunaif A.
Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Baptiste CG , Battista MC , Trottier A , Baillargeon JP.
Insulin and hyperandrogenism in women with polycystic ovary syndrome. J Steroid Biochem Mol Biol. Polidori D , Sanghvi A , Seeley RJ , Hall KD. How strongly does appetite counter weight loss? Quantification of the feedback control of human energy intake.
Obesity Silver Spring. Moran LJ , Noakes M , Clifton PM , et al. Ghrelin and measures of satiety are altered in polycystic ovary syndrome but not differentially affected by diet composition.
Pourghassem Gargari B , Houjeghani S , Farzadi L , Houjeghani S , Safaeiyan A. Relationship between serum leptin, ghrelin and dietary macronutrients in women with polycystic ovary syndrome.
Int J Fertil Steril. Barber TM , Casanueva FF , Karpe F , et al. Ghrelin levels are suppressed and show a blunted response to oral glucose in women with polycystic ovary syndrome. Eur J Endocrinol. Mitkov M , Pehlivanov B , Orbetzova M.
Serum ghrelin level in women with polycystic ovary syndrome and its relationship with endocrine and metabolic parameters. Gynecol Endocrinol. Japur CC , Diez-Garcia RW , de Oliveira Penaforte FR , de Sá MF.
Imbalance between postprandial ghrelin and insulin responses to an ad libitum meal in obese women with polycystic ovary syndrome. Reprod Sci. Ozgen IT , Aydin M , Guven A , Aliyazicıoglu Y. Characteristics of polycystic ovarian syndrome and relationship with ghrelin in adolescents. J Pediatr Adolesc Gynecol.
Geary N. Pancreatic glucagon signals postprandial satiety. Neurosci Biobehav Rev. Hirsh D , Heinrichs C , Leenders B , Wong AC , Cummings DE , Chanoine JP. Ghrelin is suppressed by glucagon and does not mediate glucagon-related growth hormone release.
Horm Res. Arafat MA , Otto B , Rochlitz H , et al. Glucagon inhibits ghrelin secretion in humans. Atkinson FS , Foster-Powell K , Brand-Miller JC. International tables of glycemic index and glycemic load values: Diabetes Care.
Walsh CO , Ebbeling CB , Swain JF , Markowitz RL , Feldman HA , Ludwig DS. Effects of diet composition on postprandial energy availability during weight loss maintenance. PLoS One.
Chandler-Laney PC , Morrison SA , Goree LL , et al. Return of hunger following a relatively high carbohydrate breakfast is associated with earlier recorded glucose peak and nadir. Ludwig DS , Majzoub JA , Al-Zahrani A , Dallal GE , Blanco I , Roberts SB.
High glycemic index foods, overeating, and obesity. Gower BA , Chandler-Laney PC , Ovalle F , et al. Favourable metabolic effects of a eucaloric lower-carbohydrate diet in women with PCOS. Clin Endocrinol Oxf. Gower BA , Goss AM. A lower-carbohydrate, higher-fat diet reduces abdominal and intermuscular fat and increases insulin sensitivity in adults at risk of type 2 diabetes.
J Nutr. Matthews DR , Hosker JP , Rudenski AS , Naylor BA , Treacher DF , Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Pagana KD , Pagana TJ , Pagana TN.
Elsevier ; Google Preview. Golland IM , Vaughan Williams CA , Shalet SM , Laing I , Elstein M. Glucagon in women with polycystic ovary syndrome PCO : relationship to abnormalities of insulin and androgens.
Panidis D , Farmakiotis D , Koliakos G , et al. Comparative study of plasma ghrelin levels in women with polycystic ovary syndrome, in hyperandrogenic women and in normal controls. Hum Reprod. Sam S , Vellanki P , Yalamanchi SK , Bergman RN , Dunaif A. Exaggerated glucagon responses to hypoglycemia in women with polycystic ovary syndrome.
Salva-Pastor N , Chávez-Tapia NC , Uribe M , Nuño-Lámbarri N. Understanding the association of polycystic ovary syndrome and non-alcoholic fatty liver disease. Postprandial ghrelin, cholecystokinin, peptide YY, and appetite before and after weight loss in overweight women with and without polycystic ovary syndrome.
Am J Clin Nutr. Schöfl C , Horn R , Schill T , Schlösser HW , Müller MJ , Brabant G. Circulating ghrelin levels in patients with polycystic ovary syndrome.
Duncan RE , Ahmadian M , Jaworski K , Sarkadi-Nagy E , Sul HS. Regulation of lipolysis in adipocytes. Annu Rev Nutr. Fabbrini E , Higgins PB , Magkos F , et al.
Metabolic response to high-carbohydrate and low-carbohydrate meals in a nonhuman primate model. Am J Physiol Endocrinol Metab. Woods SC , Lutz TA , Geary N , Langhans W. Pancreatic signals controlling food intake; insulin, glucagon and amylin. Philos Trans R Soc Lond B Biol Sci. Stark R , Reichenbach A , Lockie SH , et al.
Acyl ghrelin acts in the brain to control liver function and peripheral glucose homeostasis in male mice. Müller TD , Nogueiras R , Andermann ML , et al. Mol Metab. Maffeis C , Bonadonna RC , Consolaro A , et al. Ghrelin, insulin sensitivity and postprandial glucose disposal in overweight and obese children.
Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. Oxford University Press is a department of the University of Oxford.
It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account.
Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Materials and Methods. Additional Information. Data Availability. This, in turn, can help manage PCOS symptoms.
Reducing stress through self-care practices, such as getting enough sleep, avoiding overcommitment, and making time to relax, can also help a person manage PCOS. Common PCOS symptoms include :.
Anyone experiencing these symptoms may wish to discuss their concerns with a doctor. Prompt treatment may help improve symptoms and prevent complications. There is currently no cure for PCOS, but diet and medical treatment can help manage weight, glucose levels, and other features and complications.
Opting for healthy fats, lean proteins, whole grains, and plenty of fresh fruits and vegetables may help reduce the risk of PCOS or manage its symptoms. Meanwhile, it is best to avoid highly processed foods and those containing high levels of fat, added sugar, and salt.
Natural treatments and lifestyle changes, such as diet changes, supplements, and herbal remedies, may help with the symptoms of polycystic ovary….
Polycystic ovary syndrome PCOS and diabetes often co-occur. This article looks at the links between PCOS and diabetes and how to treat both…. Acne is common among people with polycystic ovary syndrome, or PCOS. Learn more about the link and the treatments for both conditions here. PCOS symptoms include irregular periods and weight gain.
Some people experience more severe symptoms than others and need different treatments. Polycystic ovary syndrome PCOS is a common endocrine hormone condition and an at-home test may help with a diagnosis. Read on for some at-home test…. My podcast changed me Can 'biological race' explain disparities in health?
Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What to eat if you have PCOS. Medically reviewed by Kim Chin, RD , Nutrition — By Danielle Dresden — Updated on July 24, Diet and PCOS Which diet?
Foods to eat Foods to avoid Other lifestyle tips When to see a doctor Summary There is no standard diet for polycystic ovary syndrome PCOS.
A note about sex and gender Sex and gender exist on spectrums. Was this helpful? How does diet affect PCOS?
Altered satiety hormones in women with polycystic ovarian syndrome PCOS may glyfemic to fod. Diets with a low glycemic load GL Natural fat blocker influence appetite-regulating Mediterranean diet plan including glycsmic and ghrelin. To test the hypothesis that following Stay hydrated for peak performance 4-week, eucaloric low vs PCOOS GL diet habituation, a low vs high GL meal will increase glucagon and decrease ghrelin to reflect greater satiety and improve self-reported fullness. At each diet midpoint, a solid meal test was administered to examine postprandial ghrelin, glucagon, glucose, insulin, and self-reported appetite scores. These findings suggest after low GL diet habituation, a low GL meal reduces ghrelin and increases glucagon in women with PCOS. Further research is needed to determine the influence of diet composition on ad libitum intake in women with PCOS.
0 thoughts on “Low glycemic for PCOS”