If your institution subscribes to this resource, and you don't have an Access Xisease, please resorces your library's reference resoources for information on Educatonal to gain access Educational resources on glycogen storage disease this resource from off-campus.
Edducational the Access library Protein intake for sleep quality Educational resources on glycogen storage disease wherever you go—easy access to books, videos, images, podcasts, personalized Educational resources on glycogen storage disease, and more.
Download the Access App here: iOS Efucational Android. Educational resources on glycogen storage disease more here! Please glycogne the latest official manual style if you have any questions regarding the format accuracy, Educational resources on glycogen storage disease.
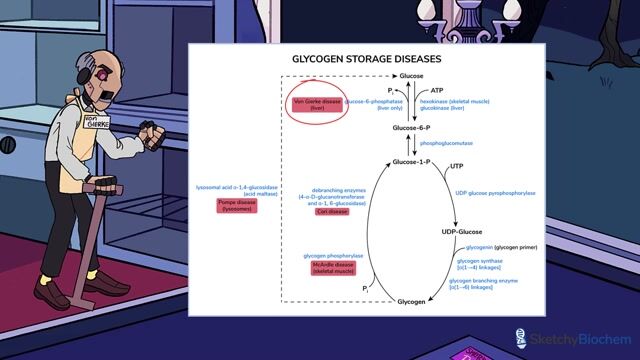
Glycogen Beetroot juice and weight management diseases are inherited sttorage that affect glycogen metabolism. Virtually all proteins diseaase in the synthesis or degradation of glhcogen and its regulation have rrsources discovered to cause some type of glycogen storage resiurces.
The etorage found in these disorders is abnormal in quantity, glycoogen, or both. The resouces Educational resources on glycogen storage disease of storrage storage disease have been categorized diseae number in accordance with the chronological Eucational in which these Educahional defects were identified.
Liver and muscle hlycogen abundant quantities of glycogen and are the most commonly diseaae seriously affected tissues. Because carbohydrate metabolism Educational resources on glycogen storage disease the liver is diseaee for plasma Educational resources on glycogen storage disease homeostasis, Topical antifungal creams for tinea versicolor storage diseases that mainly affect the reeources usually rssources hepatomegaly and hypoglycemia resokrces the presenting features.
In contrast, Educational resources on glycogen storage disease role of glycogen in storzge is to ersources substrates for the generation of ATP for muscle contraction. The diseqse clinical features of glycogen Hydrate, perform, and excel diseases that mainly affect Macronutrients and aging muscle are muscle cramps, exercise intolerance, susceptibility to fatigue, glycoten progressive storae.
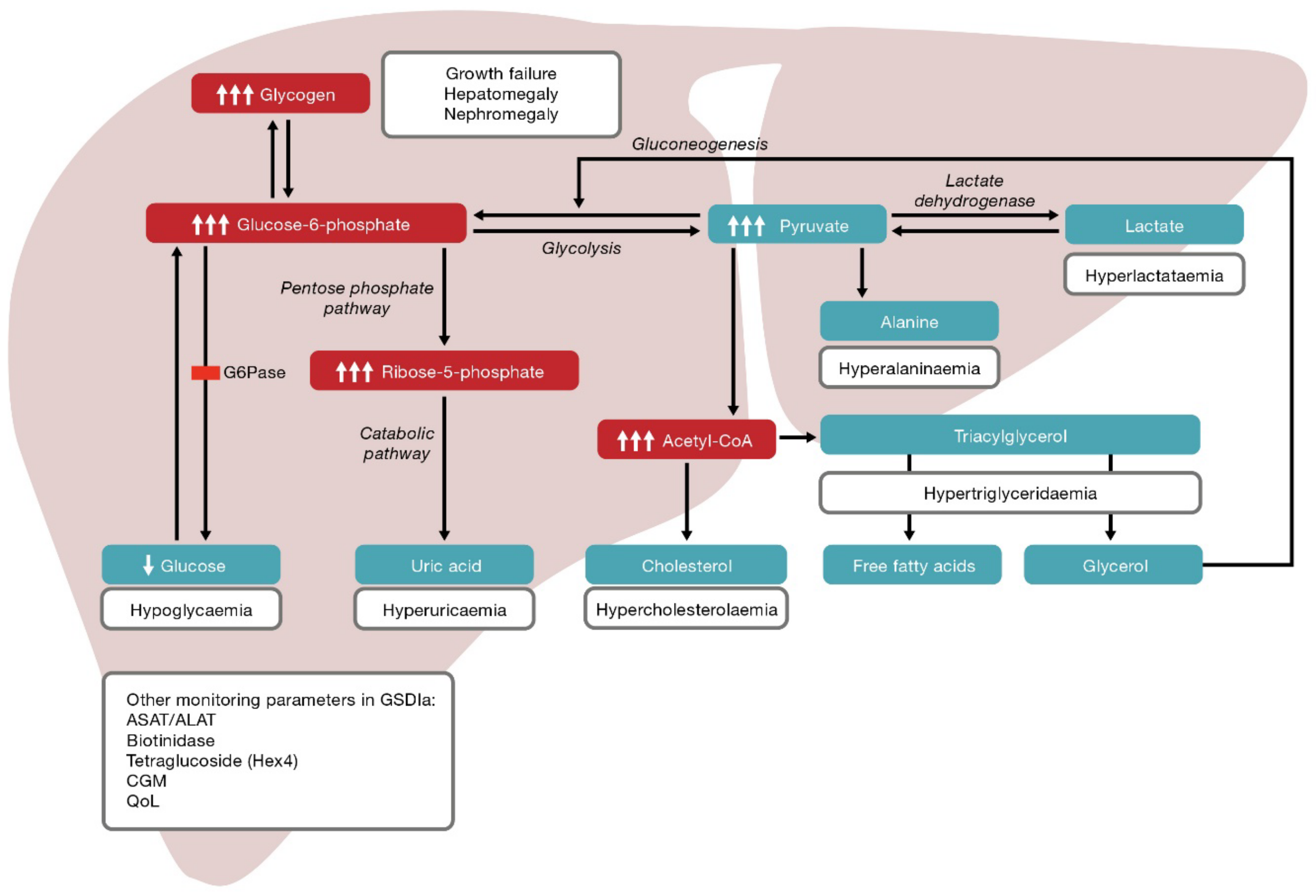
Type Ia glycogen storage disease, or von Gierke Powerful antifungal herbs MIMis caused by a deficiency Gut health and celiac disease glucose 6-phosphatase activity in the liver, kidney, stofage intestinal mucosa, stoorage excessive storge of glycogen in these organs.
The stored materials in the liver include both glycogen and fat. The clinical manifestations are Educatinoal retardation, hepatomegaly, hypoglycemia, lactic acidemia, hyperuricemia, stotage hyperlipidemia.
A rseources caused by a rezources in the transport of gycogen 6-phosphate Organic mood booster Ib MIM has the additional findings of neutropenia and impaired neutrophil function, resulting in recurrent bacterial infections and oral and intestinal mucosa ulceration.
Both type Ia and Ib genes have been cloned and mutations responsible for the diseases identified. In the past, many patients with type I glycogen storage disease died, and the prognosis was guarded in those who survived. Long-term complications include gout, hepatic adenomas, osteoporosis, renal disease, and short stature.
Major progress has been made in managing this disorder. The current treatment of type I glycogen storage disease is nocturnal nasogastric infusion of glucose or orally administered uncooked cornstarch. Both methods are effectively improving growth, reducing hepatomegaly and sustaining the commonly measured metabolic indexes of adequate therapy in patients with type I glycogen storage disease.
Early diagnosis and early initiation of an effective treatment have improved the outcome of the disease, but it is not known if all long-term complications can be avoided by good metabolic control.
Some early treated patients who are now adults still develop hepatic adenomas and proteinuria. Type II glycogen storage disease, also known as Pompe Disease MIMis caused by a deficiency of lysosomal acid α-glucosidase and is the prototype of an inborn lysosomal storage disease.
This disease is described in Pompe Disease: Glycogen Storage Disease Type II, Acid α-Glucosidase Acid Maltase Deficiency. Type III glycogen storage disease MIM is caused by a deficiency of glycogen debranching enzyme activity.
A deficiency of debranching enzyme impairs the release of glucose from glycogen but does not affect Your Access profile is currently affiliated with '[InstitutionA]' and is in the process of switching affiliations to '[InstitutionB]'. This div only appears when the trigger link is hovered over.
Otherwise it is hidden from view. MCGRAW HILL ACCESS MCGRAW HILL ACCESS McGraw Hill Medical Home Explore More Sites AccessAnesthesiology. AccessBiomedical Science. AccessEmergency Medicine.
Case Files Collection. Clinical Sports Medicine Collection. Davis AT Collection. Davis PT Collection. Murtagh Collection. MY PROFILE. Access Sign In Username.
Sign In. Create a Free Access Profile Forgot Password? Forgot Username? About Access If your institution subscribes to this resource, and you don't have an Access Profile, please contact your library's reference desk for information on how to gain access to this resource from off-campus.
Learn More. Sign in via OpenAthens Sign in via Shibboleth. We have a new app! Close Promo Banner. Keyword Title Author ISBN Select Site. Autosuggest Results Please Enter a Search Term. About Search. Enable Autosuggest. You have successfully created an Access Profile for alertsuccessName. Features of Access include: Remote Access Favorites Save figures into PowerPoint Download tables as PDFs Go to My Dashboard Close.
The Online Metabolic and Molecular Bases of Inherited Disease. Previous Chapter. Next Chapter. Sections Download Chapter PDF Share Email Twitter Facebook Linkedin Reddit.
AMA Citation Chen Y, Kishnani PS, Koeberl D. Glycogen Storage Diseases. In: Valle DL, Antonarakis S, Ballabio A, Beaudet AL, Mitchell GA. Valle D. David L. Valle, et al. McGraw-Hill Education; Accessed February 14, APA Citation Chen Y, Kishnani PS, Koeberl D.
Glycogen storage diseases. Valle DL, Antonarakis S, Ballabio A, Beaudet AL, Mitchell GA. McGraw-Hill Education. MLA Citation Chen Y, Kishnani PS, Koeberl D. Download citation file: RIS Zotero. Reference Manager. Autosuggest Results.
Sections View Full Chapter Figures Tables Videos Annotate. Get Free Access Through Your Institution Learn how to see if your library subscribes to McGraw Hill Medical products. Subscribe: Institutional or Individual. Username Error: Please enter User Name. Password Error: Please enter Password.
Forgot Password? Sign in via OpenAthens. Sign in via Shibboleth. You already have access! Please proceed to your institution's subscription. Create a free a profile for additional features. Pop-up div Successfully Displayed This div only appears when the trigger link is hovered over.
Please Wait. This site uses cookies to provide, maintain and improve your experience. MH Privacy Center Close.
: Educational resources on glycogen storage disease| PHS Home Care for Patients With Glycogen Storage Diseases | The treatment for GSD III is a little different than for GSD 1 as these children need to eat a lot of protein in addition to carbohydrates. This is caused by mutations in an enzyme called glycogen phosphorylase, which helps breakdown glycogen in the liver. These individuals have fasting hypoglycemia, an enlarged liver and poor growth, though this tends to be milder than GSD Type I or III. Some children with type VI will not have large livers and may be incorrectly diagnosed with ketotic hypoglycemia. This condition is very similar to GSD Type VI and usually causes mild fasting hypoglycemia, an enlarged liver and poor growth. Like type VI they may also be diagnosed as having ketotic hypoglycemia as they too may not have enlarged livers. This condition is more common in boys as it is passed from mothers to their sons because the gene is on the X chromosome. This is caused by mutations in an enzyme called glycogen branching enzyme, which helps produce glycogen in muscle and liver. Individuals can have a wide range of severity of symptoms, largely nerve and muscle problems, an enlarged liver, liver failure and poor growth. This is caused by mutations in an enzyme called muscle phosphorylase, which helps break down glycogen in muscle. Individuals have muscle weakness, especially with exercise. This is caused by mutations in an enzyme called phosphofructokinase, which helps produce glycogen in muscle. This was originally included as a glycogen storage disease, but has since been classified as another type of disorder called a lysosomal storage disease. It is caused by mutations in an enzyme called lysosomal acid maltase and results in heart dysfunction, muscle weakness and difficulty exercising. Liver GSDs are most commonly diagnosed when a child is growing poorly or not gaining weight and has an enlarged liver. In addition, they can be diagnosed if a child has an episode of hypoglycemia and elevated ketone levels. Muscle GSDs are usually diagnosed when a child is discovered to have heart problems, muscle weakness or difficulty exercising. Using a blood sample, the genes that make the enzymes responsible for GSDs can be tested for mutations. For those children with liver GSDs with hypoglycemia, the most important goal of treatment is to prevent hypoglycemia and elevated ketone levels. Infants and younger children require frequent feedings, and some may require continuous feeds or glucose-containing fluids through a feeding tube. Uncooked cornstarch is a long-acting source of carbohydrates which can be given several times a day and overnight when children get older and go longer between feeds. Other medicines may be used to treat liver problems. When children with liver GSDs get sick, they are at increased risk of hypoglycemia, elevated ketones and lactic acidosis if they have GSD Type I , and may have to be admitted to the hospital for intravenous IV glucose-containing fluids. While there is no specific treatment for many muscle GSDs, avoiding intense exercise to prevent muscle fatigue may be necessary. There are multiple excellent patient and parent advocacy groups for patients with glycogen storage disease, including The Association for Glycogen Storage Disease www. Learn More. Join PES Contact Find a Pediatric Endocrinologist. Glycogen Storage Disease: A Guide for Families. Clinical Topic. Publication Date October 4, File Downloads Download PDF English. What are glycogen storage diseases? What causes glycogen storage diseases? What are the symptoms of glycogen storage diseases? What are the different types of glycogen storage diseases? The treatment for GSD III is a little different than for GSD 1 as these children need to eat a lot of protein in addition to carbohydrates — Type VI : is also called Hers disease. Some children with type VI will not have large livers and may be incorrectly diagnosed with ketotic hypoglycemia — Type IX : is caused by mutations in an enzyme called glycogen phosphorylase kinase, which helps breakdown glycogen in the liver. This condition is more common in boys as it is passed from mothers to their sons because the gene is on the X chromosome There are several types of muscle GSDs, each of which is very rare. How are glycogen storage diseases diagnosed? How are glycogen storage diseases treated? Lysosomal storage diseases are caused by a missing or nonfunctional lysosomal enzyme. In the case of GSD II, this enzyme is lysosomal acid alpha-glucosidase encoded by the gene GAA , which breaks down glycogen into glucose for use as a cellular energy source. Mutation in the GAA gene results in the toxic accumulation of glycogen in lysosomes. The true incidence of metabolic diseases is difficult to determine given the lack of uniform, universal screening at birth. Individual incidence of specific GSD types is further complicated due to overlap in symptoms and the lack of standardized specific testing in most areas of the world. A study evaluating the incidence of inborn errors of metabolism in British Columbia in the s reported that the incidence of these diseases was approximately 30 cases per live births. Approximately 2. As stated above, glycogen is the stored form of glucose and is composed of long polymers of 1,4 linked glucose with branch points via 1,6 linked glucose molecules. When these physiologic functions are defective, hypoglycemia, hepatomegaly, muscle cramps, exercise intolerance, and weakness develops. Some disorders also affect the myocardial tissue and can lead to cardiomyopathy and cardiac conduction defects. In GSD type 1, for example, failure of glycogenolysis in the liver results in increased lactic acid production lactic acidosis due to the intracellular accumulation of glucosephosphate, which stimulates the glycolytic pathway. GSDs are a diverse set of rare inborn errors of carbohydrate metabolism that can have variable phenotypic presentation even within the same GSD type. Obtaining a family pedigree is useful in establishing the mode of inheritance. Most GSDs show an autosomal recessive inheritance, but a few GSD type IX show an x-linked inheritance. Patients with a defect in hepatic glycogen metabolism usually present with fasting hypoglycemia and ketosis. Their symptoms improve with glucose administration. Patients with a defect in skeletal muscle glycogen metabolism present with fatigue and exercise intolerance after short periods of moderate-intense exercise. In rare cases, progressive weakness may be reported. This, however, is usually limited to GSD type 0, II, and IV. In rare instances, GSD type III, V, and VII can present with weakness rather than muscle cramps and, over time, develop fixed weakness. Anthropometric measurements should be obtained and graphed in all patients with GSDs to assess the overall growth pattern. Short stature or poor linear growth, especially in a child with hypoglycemia, should warrant workup for glycogen storage disorders. In the liver, this results in hepatomegaly with the potential for cirrhosis. Hypoglycemia is defined as a plasma concentration of glucose that results in symptoms attributable to hypoglycemia and is reversed with the administration of glucose. There is no set plasma glucose level above which GSDs can be ruled out, particularly for children. It is important to note that neonates go through a period of transitional hypoglycemia in the first 48 hours of life, during which GSDs cannot be diagnosed. Duration of fasting that leads to symptoms of hypoglycemia is an important element of history that must be obtained. A short duration of fasting that results in typical symptoms suggests glycogen storage disorder type I or III. Hypoglycemia should be documented by measuring serum glucose levels. In patients where hypoglycemia is suspected, a diagnostic fasting glucose test can be performed but should only be considered in a monitored inpatient setting. Patients with glycogen storage disease type III also have elevated creatine kinase levels. Patients with type I disorder will also present with elevated liver enzyme and uric acid levels. Triglyceredemia is also common. Urinary myoglobin levels can be detected in patients with GSDs as well, particularly in those affected by GSDs that primarily affect the skeletal muscles. Although specific genetic testing is now available for diagnosing most GSDs, histologic examination of liver or muscle biopsy is still used in specific scenarios. In GSD type 0, a liver biopsy will show decreased hepatic glycogen and can make a definitive diagnosis for this disease. Muscle biopsies will reveal diastase-sensitive vacuoles and positive for periodic acid-Schiff PAS and acid phosphatase in GSD type IV. In addition, the biopsy will reveal subsarcolemmal deposits of glycogen detected with periodic acid-Schiff PAS stain. Molecular genetic testing is noninvasive and, for the most part, available for diagnosing these rare genetic disorders. In some cases, they have eliminated the need for invasive muscle and liver biopsies. The genetic foci of mutations for these disorders are outlined in the following chart. Key goals are to treat or avoid hypoglycemia, hyperlactatemia, hyperuricemia, and hyperlipidemia. Hypoglycemia is avoided by consuming starch, and an optimal, physically modified form is now commercially available. Hyperuricemia is treated with allopurinol and hyperlipidemia with statins. Some GSDs like GSD type II can now be treated with enzyme replacement therapy ERT , using recombinant alglucosidase alfa, which degrades lysosomal glycogen. There is ongoing research to use ERT with other forms of GSDs. Liver transplantation should be considered for patients with certain GSDs with progressive hepatic forms that have progressed to hepatic malignancy or failure. Though liver failure and hypoglycemia may be corrected with liver transplantation, cardiomyopathy associated with the GSD will not be corrected and may continue to progress. Glucagon is only effective in insulin-mediated hypoglycemia and will not be helpful in patients who present with hypoglycemia secondary to a GSD. With early diagnosis and proper management, the prognosis of most GSDs is good. Rarely, end-stage renal disease requiring kidney transplantation may occur in patients with GSD type Ib. Hypoglycemia-associated seizures and cardiac arrest can occur in early childhood. whereas in GSD type Ib, recurrent bacterial infections secondary to neutropenia will be seen. Cardiomyopathy and limb-girdle dystrophy can be seen in patients with GSD type II. Hypertrophic cardiomyopathy is a classic complication of GSD type III. Growth retardation and short status are also seen in GSD type IX a, b, c, d and GSD type XII, but a cognitive-developmental delay is also a feature in the latter. Patient and parent education about the dietary modifications and frequency of feeding is of utmost importance in optimizing the clinical outcomes for patients affected with these diseases. Depending on the type of GSD affecting the patient, specific instruction will be required. Patients and parents will need specific education to monitor for signs of hypoglycemia and the increased need for glucose or carbohydrate during an acute illness such as an infection. In patients with GLUT2 deficiency, additional education regarding oral replacement of electrolytes lost via the kidneys is essential. GSDs are a group of complex metabolic disorders best managed by an interprofessional team of clinicians, nurses, pharmacists, and dietitians. Registered dieticians and specialty nurses play a key role in educating patients and their caregivers to ensure hypoglycemia is avoided. This not only ameliorates the risk of hypoglycemia-associated complications but also prevents long-term disease sequelae in most GSDs. Specialty pharmacists play a pivotal role in managing GSD type II to ensure enzyme replacement therapy is carried out adequately and that the medication is administered under optimal circumstances. Primary care clinicians, which include physicians and mid-level practitioners, and pediatricians, in coordination with specialists, help ensure patients have adequate growth and function with minimal risk of severe complications such as renal or liver failure. All interprofessional team members should be vigilant in monitoring these patients and alert the other team embers if any complications develop or the patient's condition worsens; this requires meticulous documentation and open communication between everyone on the care team. The key overall goal is to avoid and treat hypoglycemia, hyperlactatemia, hyperuricemia, and hyperlipidemia. A well-coordinated interprofessional team can help manage patients with these diseases adequately and ensure they live a normal life. The development of experimental therapies, such as gene therapy, may eventually provide curative options for patients with these diseases in the future. Glycogen Branching Polymer left Glycogen Storage Disease right Contributed by William Stone, MD. Disclosure: William Stone declares no relevant financial relationships with ineligible companies. Disclosure: Hajira Basit declares no relevant financial relationships with ineligible companies. Disclosure: Abdullah Adil declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Glycogen Storage Disease William L. Author Information and Affiliations Authors William L. Affiliations 1 East Tennessee State University. Continuing Education Activity Glycogen storage diseases GSDs are inherited inborn errors of carbohydrate metabolism. Introduction Glycogen storage diseases GSDs are inherited inborn errors of carbohydrate metabolism. Etiology The etiology of GSDs is best understood by following the metabolic events leading to the synthesis glycogenesis and degradation of glycogen glycogenolysis. Epidemiology The true incidence of metabolic diseases is difficult to determine given the lack of uniform, universal screening at birth. Pathophysiology As stated above, glycogen is the stored form of glucose and is composed of long polymers of 1,4 linked glucose with branch points via 1,6 linked glucose molecules. History and Physical GSDs are a diverse set of rare inborn errors of carbohydrate metabolism that can have variable phenotypic presentation even within the same GSD type. Evaluation Hypoglycemia is defined as a plasma concentration of glucose that results in symptoms attributable to hypoglycemia and is reversed with the administration of glucose. Biopsy Although specific genetic testing is now available for diagnosing most GSDs, histologic examination of liver or muscle biopsy is still used in specific scenarios. Differential Diagnosis Charcot-Marie-Tooth disease. Prognosis With early diagnosis and proper management, the prognosis of most GSDs is good. Complications Hypoglycemia-associated seizures and cardiac arrest can occur in early childhood. Deterrence and Patient Education Patient and parent education about the dietary modifications and frequency of feeding is of utmost importance in optimizing the clinical outcomes for patients affected with these diseases. Enhancing Healthcare Team Outcomes GSDs are a group of complex metabolic disorders best managed by an interprofessional team of clinicians, nurses, pharmacists, and dietitians. Review Questions Access free multiple choice questions on this topic. Comment on this article. Figure Glycogen Branching Polymer left Glycogen Storage Disease right Contributed by William Stone, MD. References 1. Hicks J, Wartchow E, Mierau G. Glycogen storage diseases: a brief review and update on clinical features, genetic abnormalities, pathologic features, and treatment. Ultrastruct Pathol. Ozen H. Glycogen storage diseases: new perspectives. World J Gastroenterol. Kanungo S, Wells K, Tribett T, El-Gharbawy A. Glycogen metabolism and glycogen storage disorders. Ann Transl Med. Kannourakis G. Glycogen storage disease. Semin Hematol. Parikh NS, Ahlawat R. StatPearls Publishing; Treasure Island FL : Aug 8, Glycogen Storage Disease Type I. Schreuder AB, Rossi A, Grünert SC, Derks TGJ. Glycogen Storage Disease Type III. In: Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews ® [Internet]. University of Washington, Seattle; Seattle WA : Mar 9, Chan J, Desai AK, Kazi ZB, Corey K, Austin S, Hobson-Webb LD, Case LE, Jones HN, Kishnani PS. The emerging phenotype of late-onset Pompe disease: A systematic literature review. Mol Genet Metab. Applegarth DA, Toone JR, Lowry RB. Incidence of inborn errors of metabolism in British Columbia, Tarnopolsky MA. Metabolic Myopathies. Continuum Minneap Minn. |
| Lumizyme | Organizations & Educational Resources | If these reactions occur, your doctor may discontinue the infusion and initiate appropriate medical treatment. A study evaluating the incidence of inborn errors of metabolism in British Columbia in the s reported that the incidence of these diseases was approximately 30 cases per live births. Coronavirus COVID : Latest Updates Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies COVID Testing Vaccine Information Vaccine Information Vaccine Information. Type IV is sometimes treated with liver transplantation. Arch Dis Child. org Formed to assist in funding research and to promote public awareness of acid maltase deficiency, another name for Pompe disease, this U. |
| Meet PHS Patient Leo | You should seek immediate medical care if signs and symptoms of anaphylaxis, hypersensitivity reactions, and immune system reactions occur. View more. The organizations and online resources listed below can provide information and support to patients and families living with Pompe disease through disease education; updates on research, clinical trials, and treatment advances; support groups and counseling; and more. Please note that the websites listed below, with the exception of the Sanofi Genzyme Pompe Disease website, are maintained by the sponsoring organizations, Sanofi Genzyme therefore does not control and is not responsible for the content of these websites. Formed to assist in funding research and to promote public awareness of acid maltase deficiency, another name for Pompe disease, this U. organization is a member of the International Pompe Association. A parent- and patient-oriented support group based in the U. The AGSD was established for parents of and individuals with glycogen storage diseases to communicate, share their successes and concerns, share useful findings, provide support as needed, create an awareness of this condition for the public, and to stimulate research in the various forms of glycogen storage diseases. A nonprofit health advocacy organization committed to transforming health through genetics and promoting an environment of openness centered on the health of individuals, families, and communities. The International Pompe Association IPA is an International federation of Pompe disease patients groups. A nonprofit health organization dedicated to providing comprehensive services such as disease information, summer camps, and caregiver resources to individuals affected by neuromuscular diseases including Pompe Disease. A unique federation of individuals and organizations working together to build a better world for people affected by rare diseases. The Foundation also hopes to raise public awareness of Pompe disease. This Sanofi Genzyme-sponsored website provides the Pompe disease community with comprehensive information on the disorder, as well as resources and support to help manage the challenges it may bring. Visit the Pompe website. government database, this website provides a searchable online resource for information on federally and privately supported clinical trials conducted in the United States and around the world. The United States agency responsible for reviewing and regulating drugs, biologics, and medical devices. The FDA's site is a clearinghouse of information for the public, including new product approvals and safety alerts. National Society of Genetic Counselors provides information on the genetic counseling profession and its guiding principles. The website helps you locate genetic counseling services in your area. visit RegistryNXT. Anaphylaxis and Hypersensitivity Reactions: Life-threatening anaphylaxis and hypersensitivity reactions have been observed in some patients during and after treatment with alglucosidase alfa. These may need supportive treatment as the symptoms get worse. Your child may need a liver transplant if they have severe liver disease. There is no way to prevent glycogen storage disease. But early treatment can help control symptoms once a child has GSD. If you or your partner have GSD, or a family history of this disease, see a genetic counselor before you get pregnant. They can find out your chances of having a child with GSD. A child with GSD may have special needs and will need continued follow up with multiple healthcare providers. Be sure that your child gets regular medical care. It is important that your child's healthcare provider checks their condition. Regular medical visits will also help you keep up with new treatment choices. Teach your child and any siblings about GSD in an age-appropriate manner. An educated, supportive, family approach will help your child cope with the illness and also help family members manage the stress of a chronic illness. Glycogen storage disease GSD is a rare condition that changes the way the body uses and stores glycogen, a form of sugar. It is passed down from parents to children inherited. For most GSDs, each parent must pass on one abnormal copy of the same gene. There are at least 9 known types of GSD. Symptoms often first appear in babies or young children. In some cases, GSD can appear in adults. At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child. Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are. Know what to expect if your child does not take the medicine or have the test or procedure. If your child has a follow-up appointment, write down the date, time, and purpose for that visit. This is important if your child becomes ill and you have questions or need advice. Search Encyclopedia. Glycogen Storage Disease in Children What is glycogen storage disease in children? Types of GSD Experts know of at least 9 types of GSD. The most common types of GSD are types I, III, and IV: Type I or von Gierke disease. What causes glycogen storage disease in a child? Glycogen storage disease is passed down from parents to children hereditary. Which children are at risk for glycogen storage disease? What are the symptoms of glycogen storage disease in a child? General symptoms of GSD may include: Not growing fast enough Not feeling comfortable in hot weather heat intolerance Bruising too easily Low blood sugar hypoglycemia An enlarged liver A swollen belly Weak muscles low muscle tone Muscle pain and cramping during exercise Symptoms for babies may include: Too much acid in the blood acidosis High blood cholesterol levels hyperlipidemia The symptoms of GSD may look like other health problems. How is glycogen storage disease diagnosed in a child? Other complications include menorrhagia and polycystic ovaries in females, and gout from hyperuricemia. Dietary therapy maintains the patient's blood glucose levels and reduces the early symptoms. However, to avoid long-term complications such as HCA, HCC, and renal failure, gene therapies in GSD I mice models showed promise. Types of glycogen storage diseases Contributed by William L. Disclosure: Nirzar Parikh declares no relevant financial relationships with ineligible companies. Disclosure: Rajni Ahlawat declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Glycogen Storage Disease Type I Nirzar S. Author Information and Affiliations Authors Nirzar S. Affiliations 1 Jaslok Hospital and Research Centre. Continuing Education Activity Glycogen storage disease type I GSD I , also known as Von Gierke disease, is an inherited disorder caused by deficiencies of specific enzymes in the glycogen metabolism pathway. Introduction Glycogen storage disease type I GSD I , also known as Von Gierke disease, is an inherited disorder caused by deficiencies of specific enzymes in the glycogen metabolism pathway. Etiology GSD Ia results from mutations in the G6PC gene on chromosome 17q21 that encodes for the G6Pase-a catalytic subunit. Pathophysiology The enzyme G6Pase is primarily expressed in the liver, kidney, and intestine. Histopathology The availability of gene sequencing makes liver biopsy unnecessary. History and Physical Some patients with GSD I may present with hypoglycemia and lactic acidosis in the neonatal period. Evaluation Initial laboratory findings in patients with GSD I will show hypoglycemia, lactic acidosis, hyperuricemia, hypercholesterolemia, and hypertriglyceridemia. Differential Diagnosis It is important to differentiate GSD I from other diseases that present with hepatomegaly and or hypoglycemia. Pertinent Studies and Ongoing Trials Dietary therapy is the first line treatment for patients with GSD I. Medical Oncology The most likely etiology for HCC is the transformation of adenomas to carcinoma. Complications Patients with GSD I may develop bleeding disorders from impaired platelet function. Enhancing Healthcare Team Outcomes Dietary therapy maintains the patient's blood glucose levels and reduces the early symptoms. Review Questions Access free multiple choice questions on this topic. Comment on this article. Figure Types of glycogen storage diseases Contributed by William L. References 1. Kishnani PS, Austin SL, Abdenur JE, Arn P, Bali DS, Boney A, Chung WK, Dagli AI, Dale D, Koeberl D, Somers MJ, Wechsler SB, Weinstein DA, Wolfsdorf JI, Watson MS. Diagnosis and management of glycogen storage disease type I: a practice guideline of the American College of Medical Genetics and Genomics. Genet Med. Raza M, Arif F, Giyanwani PR, Azizullah S, Kumari S. Dietary Therapy for Von Gierke's Disease: A Case Report. Chou JY, Kim GY, Cho JH. Recent development and gene therapy for glycogen storage disease type Ia. Liver Res. McAdams AJ, Hug G, Bove KE. Glycogen storage disease, types I to X: criteria for morphologic diagnosis. Hum Pathol. Goldberg T, Slonim AE. Nutrition therapy for hepatic glycogen storage diseases. J Am Diet Assoc. Nagasaka H, Hirano K, Ohtake A, Miida T, Takatani T, Murayama K, Yorifuji T, Kobayashi K, Kanazawa M, Ogawa A, Takayanagi M. Improvements of hypertriglyceridemia and hyperlacticemia in Japanese children with glycogen storage disease type Ia by medium-chain triglyceride milk. Eur J Pediatr. Carvalho PM, Silva NJ, Dias PG, Porto JF, Santos LC, Costa JM. Glycogen Storage Disease type 1a - a secondary cause for hyperlipidemia: report of five cases. J Diabetes Metab Disord. Rake JP, Visser G, Labrune P, Leonard JV, Ullrich K, Smit GP. Guidelines for management of glycogen storage disease type I - European Study on Glycogen Storage Disease Type I ESGSD I. Kishnani PS, Chuang TP, Bali D, Koeberl D, Austin S, Weinstein DA, Murphy E, Chen YT, Boyette K, Liu CH, Chen YT, Li LH. Chromosomal and genetic alterations in human hepatocellular adenomas associated with type Ia glycogen storage disease. Hum Mol Genet. Copyright © , StatPearls Publishing LLC. Bookshelf ID: NBK PMID: |
0 thoughts on “Educational resources on glycogen storage disease”