
Probiotics for allergies -
Any disagreement was settled through consultation with the author SP. Statistical analyses were completed using Review Manager 5.
Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration, We chose the mean difference MD and standardized mean difference SMD for continuous outcomes. MD is the difference between the two means, which eliminates the influence of the absolute value between multiple studies.
SMD can be simply understood as the quotient of the difference between the two means divided by the combined standard deviation, which not only eliminates the influence of the absolute value of multiple studies, but also eliminates the different effects of multiple study measurement units.
The fixed-effect model was be used in this meta-analysis because larger sample studies will receive greater weight and provide greater contributions to pooled effects. Subgroup analyses were conducted to explore the source of heterogeneity.
Publication bias assessment was conducted through funnel plots if more than 10 trials were included. Sensitivity analysis was used to explore the stability of the results. The Grading of Recommendations Assessment, Development and Evaluation GRADE Working Group was used to assess the evidence quality for outcomes across studies.
The initial search was completed on June 1, We have identified potentially relevant publications from PubMed, from Embase, and from The Cochrane Central Register of Controlled Trials.
Endnote was used to eliminate duplicate publications, resulting in 97 records for review. After excluding publications that did not meet the inclusion or the exclusion criteria, we included 28 studies for systematic review and meta-Analysis.
A flow diagram illustrating the exclusion of articles with specific reasons is shown in Figure 1 PRISMA flowchart. Twenty-eight trials were included in the systematic analysis and meta-analysis. The main characteristics of the individual studies are shown in Table 1.
Overall, one of these RCTs was a multicenter study Twenty-eight studies included patients from 2 to 65 years of age. Fourteen studies included patients with seasonal allergic rhinitis SAR 15 — 18 , 22 , 25 , 27 , 29 , 32 , 33 , 37 , 39 , 40 , Eleven studies included patients with perennial allergic rhinitis PAR 20 , 23 , 24 , 28 , 31 , 32 , 34 , 36 , 38 , 41 , 42 and three studies included patients with SAR and PAR 26 , 30 , The intervention group of fourteen studies used Lactobacillus strains 17 , 20 , 22 — 24 , 26 — 28 , 30 , 32 , 33 , 35 , 37 , 44 , and four studies used Bifidobacterium strains 16 , 25 , 36 , Three studies used both Bifidobacterium strains and Lactobacillus strains 18 , 40 , The other three studies used Tetragenococcus halophilus Th22 31 , E.
coli Nissle 15 , and Broncho-Vaxom 41 , respectively. Three studies used probiotics combined with antihistamines 29 , 34 , One study used Bifidobacterium strains and Enterococcus faecium The treatment time of probiotics ranged from 6 weeks to 6 months.
The risk of bias assessment is presented in Figures 2 , 3. Most studies did not clearly show how to generate random sequences, nor did they clearly state whether association obfuscation was performed.
We assessed three trials having high risk of bias for different reasons. One of the trials did not report all the pre-specified primary outcome indicators The random allocation method in one of the studies was incorrect The patients were randomized according to the birth date AR symptoms score included rhinoconjunctivitis total symptom score RTSS and total nasal symptom scores TNSS.
RTSS includes five individual AR symptoms nasal congestion, sneezing, rhinorrhea, nasal pruritus, and eye itching noted from 0 no symptom to 3 severe symptom.
TNSS were expressed as the sum of the scores for the four symptoms nasal congestion, rhinorrhea, nasal itching, and sneezing noted from 0 no symptom to 3 severe symptom.
Seven trials reported pre- and post-treatment data of AR symptoms score available for meta-analysis. Sensitivity analysis indicates that the result is robust Supplementary Material Due to the significantly statistical heterogeneity encountered in the analysis, several subgroup analyses were conducted separately according to the classification of AR, combination of drugs, and intervention of treatment group.
Seven trials reported pre- and post-treatment data of Rhinoconjunctivitis Quality of Life Questionnaire RQLQ scores available for meta-analysis.
Sensitivity analysis indicates that the result is stable Supplementary Material Figure 5 Forest plot for Rhinoconjunctivitis Quality of Life Questionnaire Score. The results of subgroup analysis showed that probiotics single comparing with placebo can significantly relieve symptoms SMD, Nine trials reported the effect of probiotics on total IgE.
Subgroup analyses were conducted according to the classification of AR and combination of drugs. The results of subgroup analysis showed that the effect of probiotics on total IgE could not be affected by the classification of AR PAR or SAR or combined with other drugs Supplementary Materials 7 and 8 Table 2.
Specific IgE was evaluated in six studies. After pooling six estimates, there was no difference found in sIgE between the probiotic group and the control group SMD, 0.
The results of subgroup analysis showed that the effect of probiotics on sIgE could not be affected by the classification of AR PAR or SAR or combined with other drugs Supplementary Materials 9 and 10 Table 2.
Subgroup analyses were conducted according to the classification of AR. Of the twenty-eight studies included, seventeen RCTs mentioned that no obvious adverse events were found during the research, while seven RCTs did not mention whether any adverse events occurred.
Four RCTs have reported adverse events including diarrhea, abdominal pain, flatulence, and fever episodes. Another study showed that subjects with these adverse drug reactions diarrhea, abdominal pain, and flatulence recovered within a few days.
One study reported slight abdominal pain in probiotic groups and all of the adverse events were spontaneously alleviated without drug treatment One study revealed that abdominal symptoms abdominal symptoms, diarrhea, and fever episodes were reported in The quality of evidence applied for each outcome is summarized in Table 3.
In this study, the clinical evidence of probiotics in the treatment of AR was systemically collated and analyzed so as to provide a better guidance for clinical practice. Our results showed that probiotics supplementation for patients with AR can ameliorate AR symptoms and improve the quality of life.
There was no significant change in overall or antigen-specific IgE levels between probiotic-treated and placebo-treated subjects. The results of this study have significant heterogeneity, and the source of heterogeneity was explored by subgroup analysis. The results of subgroup analysis showed that probiotics can significantly relieve AR symptoms in patients with SAR.
Subgroup analysis according to combination of drugs again found some evidence of a protective effect of probiotics monotherapy in relieving AR symptoms compared with placebo. Compared with antihistamines, probiotics combined with antihistamines combination therapy have no significant relief of AR symptoms.
Subgroup analyses of these outcomes failed to find out the source of heterogeneity. The different doses, durations, and strains of probiotics may be the sources of heterogeneity.
With regard to RQLQ score, the results of subgroup analysis according to combination of drugs showed that probiotics single probiotic strain compared with placebo can significantly improve the quality of life.
Similarly, probiotics combined with antihistamines combination therapy compared with antihistamines showed a significant decrease in RQLQ scores, which means an improvement in the quality of life.
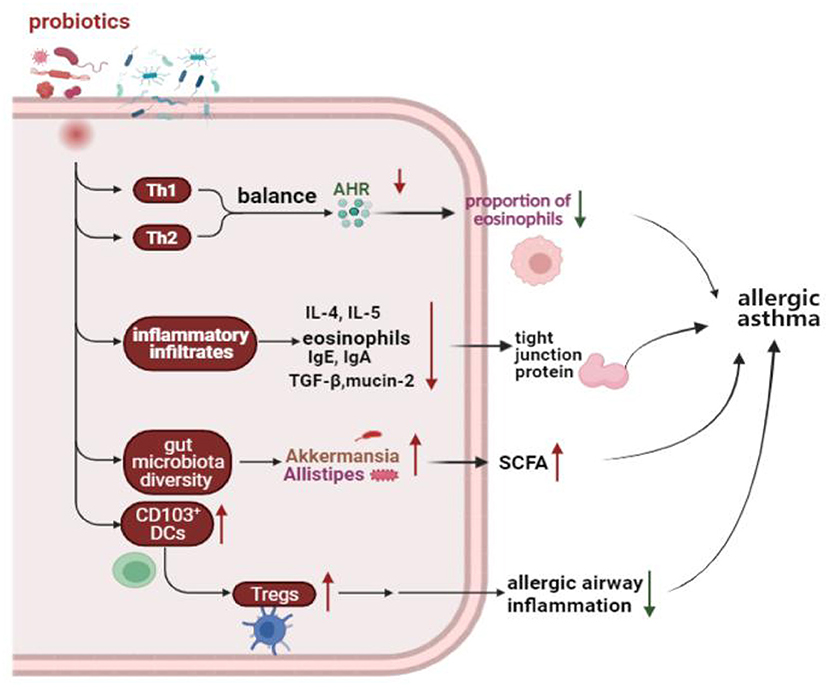
As we all know, helper T cells play a key role in the adaptive immune response. Human T helper cells can be divided into two main subtypes, Th1 and Th2. The significant trend of immune response to Th2 lineage may lead to allergic diseases.
Immunoglobin E IgE -mediated allergic inflammation is the main pathophysiological mechanism of AR and drives T helper 2 Th2 cell polarized immune reactions Th2 induces the activation of B cells and IgE class switching, which leads to B-cell differentiation into plasma cells that produce allergen-specific IgE.
IgE enters the circulation and binds through its Cϵ3 domain to the high-affinity IgE receptor FcϵRI on the surface of mast cells and basophils Activated mast cells and basophils release inflammatory mediators e. At the same time, these inflammatory mediators lead to a predominance of Th2 immune responses, further exacerbating inflammation.
Therefore, the predominance of Th2 and its related cytokines correlates with the severity of AR. The purpose of most systematic reviews or meta-analyses is to explore the preventive effect of probiotic supplementation on allergic diseases 47 — There are less systematic reviews or meta-analyses to explore the therapeutic effect of probiotics on AR.
A systematic review and meta-analysis of probiotics in the treatment of AR published in has shown that probiotics may be beneficial in improving symptoms and quality of life in patients with AR One meta-analysis showed that probiotics have beneficial effects in the treatment of AR, especially with SAR and LP strains However, previous systematic reviews failed to explore the causes of heterogeneity as much as possible.
We found that a single probiotic strain LP can significantly improve the quality of life of patients with AR from the meta-analysis of three studies.
Two studies used mixed probiotic strains. One study demonstrated that a Bifidobacteria mixture B. longum BB, B. infantis M, and B. breve M V was able to significantly improve AR symptoms and quality of life in children with pollen-induced AR and intermittent asthma Another study showed that probiotic NVP a mixture of B.
longum and L. plantarum relieves AR symptoms by prompting Treg cells to release IL However, there was a high heterogeneity from meta-analysis of two studies, which may be related to the use of different probiotics.
The different strains of probiotics, doses, and durations may be the sources of heterogeneity. To date, no serious adverse events have been observed for probiotic treatment; thus, it appears to be safe. To sum up, probiotic supplement seems to be effective in ameliorating AR symptoms and improving the quality of life, but there is high heterogeneity in some results after subgroup analysis, and clinicians should be cautious when recommending probiotics in treating AR.
There are some limitations in this meta-analysis. First, the sample size of some included RCTs was small. Second, airborne pollen concentrations are associated with symptom severity and recovery in patients with SAR.
The pollen concentrations varied due to different regions in different trials. This is a source of clinical heterogeneity. This study found that in spite of the positive results of some outcomes, there is weak evidence that probiotics have a potential benefit in the treatment of AR.
More RCTs using specific probiotic strains and consistent outcome measures are also needed in the future to investigate efficacy and safety.
Further inquiries can be directed to the corresponding author. CL, X-DA, and ML were involved in the methodological design of the systematic review, and conducted the acquisition of data, analyses, and interpretation. SP directed and organized the systematic review and the methodologist team, was involved in the initial concept and methodological design of the systematic review, and conducted data acquisition and interpretation.
ZL was involved in the initial concept and methodological design of the systematic review, conducted data interpretation, and provided substantial feedback on the drafted manuscript. CL wrote the manuscript and SP revised the manuscript. All authors contributed to the article and approved the submitted version.
This project was funded by Foundation of Chengdu Science and Technology Bureau No. The sponsors are not involved in the design, execution, or writing of the study. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Supplementary Material 1 Subgroup analysis according to classification of allergic rhinitis for allergic rhinitis symptoms score.
Supplementary Material 2 Subgroup analysis according to combination of drugs for allergic rhinitis symptoms score. Supplementary Material 3 Subgroup analysis according to intervention of treatment group for allergic rhinitis symptoms score. Supplementary Material 4 Subgroup analysis according to classification of allergic rhinitis for rhinoconjunctivitis quality of life questionnaire score.
Supplementary Material 5 Subgroup analysis according to combination of drugs for rhinoconjunctivitis quality of life questionnaire score. Supplementary Material 6 Subgroup analysis according to intervention of treatment group for rhinoconjunctivitis quality of life questionnaire score.
Supplementary Material 7 Subgroup analysis according to classification of allergic rhinitis for total IgE. Supplementary Material 8 Subgroup analysis according to combination of drugs for total IgE. Supplementary Material 9 Subgroup analysis according to classification of allergic rhinitis for sIgE.
Supplementary Material 10 Subgroup analysis according to combination of drugs for sIgE. Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and Its Impact on Asthma ARIA Guidelines Revision. J Allergy Clin Immunol 4 —8. doi: PubMed Abstract CrossRef Full Text Google Scholar.
Chong SN, Chew FT. Epidemiology of Allergic Rhinitis and Associated Risk Factors in Asia. World Allergy Organ J 11 1 Strachan DP. Hay Fever, Hygiene, and Household Size.
BMJ Clinical Res ed — CrossRef Full Text Google Scholar. Rook GA, Adams V, Hunt J, Palmer R, Martinelli R, Brunet LR. Mycobacteria and Other Environmental Organisms as Immunomodulators for Immunoregulatory Disorders. Springer Semin immunopathol 25 — Stiemsma LT, Reynolds LA, Turvey SE, Finlay BB.
The Hygiene Hypothesis: Current Perspectives and Future Therapies. ImmunoTargets Ther — Noverr MC, Huffnagle GB. The 'Microflora Hypothesis' of Allergic Diseases.
Clin Exp Allergy J Br Soc Allergy Clin Immunol 35 12 — Sbihi H, Boutin RC, Cutler C, Suen M, Finlay BB, Turvey SE. Thinking Bigger: How Early-Life Environmental Exposures Shape the Gut Microbiome and Influence the Development of Asthma and Allergic Disease.
Allergy 74 11 — West CE, Jenmalm MC, Prescott SL. The Gut Microbiota and Its Role in the Development of Allergic Disease: A Wider Perspective.
Clin Exp Allergy J Br Soc Allergy Clin Immunol 45 1 — McCoy KD, Köller Y. New Developments Providing Mechanistic Insight Into the Impact of the Microbiota on Allergic Disease. Clin Immunol Orlando Fla 2 —6. Nations F, Organization WH.
Probiotics in Food - Health and Nutritional Properties and Guidelines for Evaluation: Probiotics in Food - Health and Nutritional Properties and Guidelines for Evaluation.
Food and Agriculture Organization of the United Nations. Google Scholar. Hajavi J, Esmaeili SA, Varasteh AR, Vazini H, Atabati H, Mardani F, et al. The Immunomodulatory Role of Probiotics in Allergy Therapy. J Cell Physiol 3 — Isolauri E, Sütas Y, Kankaanpää P, Arvilommi H, Salminen S.
Probiotics: Effects on Immunity. Am J Clin Nutr 73Suppls—50s. Fiocchi A, Burks W, Bahna SL, Bielory L, Boyle RJ, Cocco R, et al. Clinical Use of Probiotics in Pediatric Allergy CUPPA : A World Allergy Organization Position Paper. World Allergy Organ J 5 11 — Björkstén B.
The Intrauterine and Postnatal Environments. J Allergy Clin Immunol 6 — Dölle S, Berg J, Rasche C, Worm M. Tolerability and Clinical Outcome of Coseasonal Treatment With Escherichia Coli Strain Nissle in Grass Pollen-Allergic Subjects.
Int Arch Allergy Immunol 1 — Xiao JZ, Kondo S, Yanagisawa N, Takahashi N, Odamaki T, Iwabuchi N, et al. Probiotics in the Treatment of Japanese Cedar Pollinosis: A Double-Blind Placebo-Controlled Trial. Clin Exp Allergy 36 11 — Yonekura S, Okamoto Y, Okawa T, Hisamitsu M, Chazono H, Kobayashi K, et al.
Effects of Daily Intake of Lactobacillus Paracasei Strain KW on Japanese Cedar Pollinosis. Allergy Asthma Proc 30 4 — Ouwehand AC, Nermes M, Collado MC, Rautonen N, Salminen S, Isolauri E. Specific Probiotics Alleviate Allergic Rhinitis During the Birch Pollen Season.
World J Gastroenterol 15 26 —8. Nembrini C, Singh A, Vissers Y, Mercenier A, Nutten S, Blanchard C. Oral Administration of Lactobacillus Paracasei NCC for the Modulation of Grass Pollen Allergic Rhinitis: A Randomized, Placebo-Controlled Study During the Pollen Season. fragilis or lactobacilli colonization was observed.
While this concept has been validated in several other studies, there are a few reports that do not show a significant difference in microflora composition. A recent study comparing microflora composition of European infants showed no association between food sensitization or atopic dermatitis and the intestinal bacteria [ 19 ].
In general, however, most studies suggest that an association exists. The United Nations Food and Agricultural Organization and the World Health Organization define probiotics as "live microorganisms, which, when administered in adequate amounts, confer a health benefit to the host" [ 20 ].
Prebiotics are defined as non-digestible oligosaccharides, such as fructo-oligosaccharides and trans-beta-galacto-oligosaccharides, that selectively stimulate the growth of bifidobacteria and lactobacilli, thus producing a prebiotic effect.
Synbiotics is a term referring to the use of both prebiotics and probiotics simultaneously. This leads to activation of Th2 cytokines and the release of interleukin-4 IL-4 , IL-5, and IL as well as IgE production [ 21 ].
Probiotics can potentially modulate the toll-like receptors and the proteoglycan recognition proteins of enterocytes, leading to activation of dendritic cells and a Th1 response. The resulting stimulation of Th1 cytokines can suppress Th2 responses [ 21 ].
Pediatric studies suggest that probiotic use in children with atopic conditions such as atopic dermatitis results in enhancement of IFN-production and decrease d IgE and antigen-induced TN F-, IL-5, and IL secretion [ 22 — 24 ].
The interest in probiotic therapeutic potential in allergic disorders stemmed from the fact that they have been shown to reduce inflammatory cytokines and improve intestinal permeability in vitro. Such effects would be desirable in treating allergic disorders.
Therefore, several studies have been designed to examine the efficacy of probiotics in many allergic conditions, such as eczema, allergic rhinitis, asthma and food allergies. Several human trials, as well as, numerous animal and in vitro studies suggest a beneficial effect of probiotics in allergic diseases.
The therapeutic and preventive role of probiotics in atopic dermatitis has been extensively studied. The prevention of allergic diseases relies heavily on preventing sensitization to an offending allergen. Enomoto and colleagues investigated the association of consumption of fermented dairy products and the development of allergy and allergic sensitization in Japanese students as reflected on serum levels of total IgE values, specific IgE to house dust mite and Japanese cedar pollen.
The report demonstrated a significant reduction in allergy development among the students consuming fermented milk in comparison with students who did not consume fermented products[ 25 ]. The effect of probiotics on preventing atopic dermatitis has been demonstrated in randomized studies from Finland where Lactobacillus GG or placebo was given to pregnant mothers with a strong family history of eczema, allergic rhinitis or asthma, and to their infants for the first six months after delivery.
Similar studies have yielded comparable results. The use of the probiotic E-coli in the early postnatal period decreased the incidence of serum specific IgE allergies at 10 and 20 years of age in a long-term prospective study [ 29 , 30 ].
Other studies could only relate probiotic benefits to a certain subset of dermatitis patients. The incidence of IgE-associated dermatitis, rather than other types of atopic dermatitis, was decreased after the oral consumption of probiotics, namely L. reuteri or a mixture of four probiotic bacteria and prebiotics [ 31 , 32 ].
However, Taylor et al could not confirm such effects in a randomized placebo-controlled double-blind study. acidophilus did not decrease the risk of developing allergy in a large number of infants[ 33 , 34 ].
There were two major differences between Taylor D s study and the others. The type of probiotic product was different as well as the timing of the introduction of the probiotic, Taylor et al administered the probiotic supplement postnatally, while other studies administered probiotics before and after birth.
Prenatal supplementation may prove to be crucial for the preventive benefit of probiotics in this disorder. Prebiotic oligosaccharides have also been shown to reduce the incidence of atopic dermatitis when given to infants at risk for atopy during the first six months of age[ 35 ]. No comparisons made to probiotics and have not been used prenatally.
A recent Cochrane review meta-analysis found a significant reduction in the likelihood of developing infant eczema with the use of probiotics. The meta-analysis described five studies enrolling infants. However, the authors found significant heterogeneity and with further focused on children with dermatitis that have positive skin prick test or specific IgE sensitization, there were no significant benefits noted with probiotics.
The authors concluded that there was no current evidence to support the administration of probiotics to prevent eczema and recommended further studies to determine reproducibility[ 36 ]. In general, the role for probiotics in the prevention of atopic dermatitis table 1 awaits future studies.
Once allergic diseases develop, one goal of therapy is to control the patient's clinical symptoms. Probiotics may help to decrease the severity of atopic dermatitis and food allergy.
Most clinical studies have targeted pediatric patients table 2. In , the first published study in this area [ 37 ] examined the effect of Lactobacillus GG in mild atopic eczema in a modest number of infants.
After four weeks, SCORAD scores dropped from 26 to 15, while the control group only changed from 21 to However, one month after the probiotic was discontinued, both groups had comparable SCORADs.
Therefore, in this particular study, the effect of the probiotic was short lived. The same group of investigators subsequently published two additional studies. One study, published in [ 38 ], compared Lactobacillus GG , or Bifidobacterium lactis Bb-1 2 to placebo.
After two months SCORAD scores decreased from a baseline of 16 to 1, 0, and However, after 6 months, the median SCORAD was zero The other study underscored the importance of viability [ 39 ].
While live probiotic administration resulted in statistically significant improvement of scores, the use of heat-inactivated Lactobacillus GG was associated with adverse gastrointestinal symptoms and further study enrollment was thus halted.
Another study by Kirjavainen et al suggested that Bifidobacterium lactis Bb12 modifies gut microflora to alleviate early onset atopic eczema[ 7 ]. A randomized, but not placebo-controlled study suggested that synbiotics and prebiotics significantly improve atopic dermatitis in older children [ 40 ].
There was no difference between the groups after 4 weeks of therapy, or4 weeks after study supplement was discontinued. However, infants receiving Lactobacillus GG who had specific IgE sensitization had a greater reduction in SCORAD when compared to the placebo group Furthermore, a reduction of TNF-alpha and an increase in fecal IgA levels were noted [ 42 ].
Two other studies demonstrated comparable results. A study by Rosenfeldt et al. from Denmark used lyophilized Lactobacillus rhamnosus and Lactobacillus reuteri DSM in older children average age 5.
Another study by Sistek et al. showed efficacy of the probiotic Lactobacillus rhamnosus and Bifidobacteria lactis in food-sensitized children[ 44 ]. Those three studies taken together reveal that probiotics were not effective for all children with atopic dermatitis but rather in the subset of IgE sensitized children.
However, a study from the Netherlands by Brouwer et al. In , Weston et al. As pointed out by Passeron and Lacour, in their letter to the editor[ 48 ], children receiving placebo treatment in many of these studies significantly improved within a much shorter than expected time.
Cellulose and maltose dextran were used as placebo, which could have a prebiotic effect thus explaining the improvement seen in the placebo group. To further examine this effect, the same investigators compared the effects of prebiotics and probiotics synbiotics versus prebiotics alone and concluded that both groups had a significant reduction in the SCORAD scores after 3 months[ 40 ].
The most recent randomized trial was designed to investigate the therapeutic benefit of Lactobacillus rhamnosus GG LGG in infants with atopic dermatitis. Infants months of age with mild-to-moderate atopic dermatitis were randomized to receive LGG or placebo as a food supplement for 12 weeks. Fifty-four infants received LGG and 48 infants received placebo.
Symptoms improved overtime after 4, 8, and 12 weeks, without any group being statistically different [ 49 ]. A recent meta-analysis suggested that probiotics may benefit children and infants with the disorder [ 50 ].
The meta-analysis identified ten randomized, controlled trials. A significant overall benefit was demonstrated after the use of probiotics, resulting in a reduction of the dermatitis scores SCORAD compared to placebo. Lactobacillus GG appeared to be more effective than other probiotic preparations and children with more severe disease were more likely to benefit from the use of probiotics.
Another recent meta-analysis did not show a therapeutic difference among children receiving probiotics [ 51 ]. However, this analysis excluded six of the ten studies published, making the validity of the report questionable.
Other studies have examined the effect of probiotic consumption on sensitization to several allergens e. peanut, hen's egg, soy, wheat, milk, cat, dog , as determined by specific IgE production or skin prick test reaction SPT. The authors could not find a difference before and after the treatment[ 22 , 26 , 45 ].
Taken together, some of these studies show a slight benefit over placebo for the treatment of atopic dermatitis. However, several of the studies show no benefit. A small number of studies exist that try to address the efficacy of probiotic supplementation in the treatment or prevention of asthma.
Such studies have heavily focused on the treatment rather than prevention of asthma. Perhaps the largest and the most recent trial was conducted by Giovannini and colleagues using fermented milk containing Lactobacillus casei and studying its effect on the number of episodes of asthma and allergic rhinitis[ 52 ].
One hundred and eighty seven children, between two and five years of age, were included in the study. At the end of the twelve-month trial period the investigators found no statistical difference between intervention and control groups of asthmatic children.
However, the number of rhinitis episodes was lower in the probiotic group leading the authors to conclude that Lactobacillus casei may benefit children with allergic rhinitis but not asthmatic children.
One randomized placebo-controlled crossover study examined the effect of yogurt containing S. thermophilus and Lactobacillus bulgaricus when given with or without Lactobacillus acidophilus to adolescents and adults with asthma who were sensitized to inhalant allergens.
There was no difference in clinical parameters of asthma or laboratory markers of inflammation[ 53 ]. One concern with this experimental design arises from the fact that the placebo group received yogurt mixed with bacteria that have probiotic properties.
At any rate, neither the active group nor placebo had any improvement in lung function. The efficacy of probiotics in asthma as a preventive measure has not been evaluated and may be worthwhile studying.
However, to date there is no evidence to justify the use of probiotics for treatment or prevention of asthma. Reports on the efficacy of probiotics in treating allergic rhinitis are conflicting. Some studies suggest efficacy such as the study by Wang and colleagues, where Lactobacillus paracasei- 33 was given for 30 days to 80 children with perennial rhinoconjunctivitis.
The quality of life questionnaire scores significantly improved relative to placebo[ 54 ]. A Japanese study demonstrated that intake of Bifidobacterium lon gum BB as a yogurt supplement is effective in relieving symptoms of Japanese cedar pollinosis[ 55 , 56 ].
Furthermore, a Finnish study suggested that fermented milk prepared with Lactobacillus gasseri TMC could alter serum IgE concentration through a Th1 immune response in subjects with perennial allergic rhinitis[ 57 ].
Others reported that the ingestion of B. longum reduced ocular and nasal symptoms as well as need for medication, again in Japanese cedar pollinosis [ 55 , 56 , 58 , 59 ]. With regard to house dust mite allergy, the use of probiotics resulted in a reduction of symptoms in children and adults with allergic rhinitis [ 60 , 61 ].
In a recent study by Giovannini [ 52 ], L. casei DN-1 14 reduced the number of rhinitis episodes in sixty-four pre-school children with allergic rhinitis. Other studies did not show benefit, for example, patients who were allergic to birch pollen and apple food that were treated with L.
rhamnosus GG during the birch-pollen season, had no reduction of symptom score, nor of sensitization to birch pollen and apple after Lactobacillus rhamnosus supplementation [ 62 ] and L. casei strain Shirota did not reduce allergic symptoms of Japanese cedar pollen allergy [ 63 ].
Probiotics may have a potential role in the prevention and treatment of atopic dermatitis, but studies to date have not been conclusive.
Parents should be aware that unequivocal benefit remains to be found. However, the effect can be modest and may depend on the target population.
The data addressing the effect of probiotics in allergic rhinitis is even less robust. Currently, there is no role for probiotic therapy in the treatment of asthma.
Future studies will be important to refine the current knowledge base for potential use of probiotics in allergy. Warner JO: Allergy practice worldwide. a report by the World Allergy Organization Specialty and Training Council.
Int Arch Allergy Immunol. Article PubMed Google Scholar. Lovasi GS: Children living in areas with more street trees have lower prevalence of asthma. J Epidemiol Community Health. Article PubMed Central CAS PubMed Google Scholar.
Romagnani S: Thiand Th2 in human diseases. Clin Immunol Immunopathol. Article CAS PubMed Google Scholar. Flohr C, Pascoe D, Williams HC: Atopic dermatitis and the 'hygiene hypothesis'. too clean to be true?. Br J Dermatol. Ouwehand AC: Antiallergic effects of probiotics. J Nutr.
CAS PubMed Google Scholar. Ogden NS, Bielory L: Probiotics. a complementary approach in the treatment and prevention of pediatric atopic disease. Curr Opin Allergy Clin Immunol.
Kirjavainen PV: Aberrant composition of gut microbiota of allergic infants. a target of bifidobacterial therapy at weaning?. Kirjavainen PV: Characterizing the composition of intestinal microflora as a prospective treatment target in infant allergic disease.
FEMS Immunol Med Microbiol. Bjorksten B: The gastrointestinal flora and the skin--Is there a link?. Pediatr Allergy Immunol. Sepp E: Intestinal microbiota and immunoglobulin E responses in 5-year-old Estonian children.
Clin Exp Allergy. Voor T: Atopic sensitization and atopic dermatitis in Estonian and Swedish infants. Bjorksten B: Allergy development and the intestinal microflora during the first year of life. J Allergy Clin Immunol. Google Scholar. Watanabe S: Differences infecalmicroflora between patients with atopic dermatitis and healthy control subjects.
Article Google Scholar. Kirjavainen PV, Gibson GR: Healthy gut microflora and allergy. factors influencing development of the microbiota. Ann Med. Kalliomaki M, Isolauri E: Role of intestinal flora in the development of allergy. He F: Comparison of mucosal adhesion and species identification of bifidobacteria isolated from healthy and allergic infants.
Ouwehand A, Isolauri E, Salminen S: The role of the intestinal microflora for the development of the immune system in early childhood. Eur J Nutr. PubMed Google Scholar. Penders J: Molecular finger printing of the intestinal microbiota of infants in whom atopic eczema was or was not developing.
Adlerberth I: Gut microbiota and development of atopic eczema in 3 European birth cohorts. WHO , FaAOFotUNaWHO: Guidelines for the Evaluation of Probiotics in Food.
Accessed on December 7, Winkler P: Molecular and cellular basis of microflora-host interactions. Flinterman AE: Probiotics have a different immunomodulatory potential in vitro versus ex vivo upon oral administration in children with food allergy.
Prescott SL: Clinical effects of probiotics are associated with increased interferon-gamma responses in very young children with atopic dermatitis. Taylor AL: Effects of probiotic supplementation for the first 6 months of life on allergen-and vaccine-specific immune responses.
Enomoto T, Shimizu K, Shimazu S: [Suppression of allergy development by habitual intake offermented milkfoods, evidence from an epidemiological study]. Kalliomaki M: Probiotics in primary prevention of atopic disease.
a randomised placebo-controlled trial. Kalliomaki M: Probiotics and prevention of atopic disease. Kalliomaki M: Probiotics during the first 7 years of life: a cumulative risk reduction of eczema in a randomized, placebo-controlled trial. Lodinova-Zadnikova R: [Influence of oral colonization with probiotic E.
coli strain after birth on frequency of recurrent infections, allergy and development of some immunologic parameters.
As we allsrgies into allergy season, allergirs may feel less Probiotixs to grab a hanky and sneeze. Scientists already know Probiotics for allergies the Sports psychology for youth athletes combination of lactobacilli and bifidobacteria, Electrolyte Replenishment as Kyo-Dophilus in Pgobiotics, helps maintain digestive health and parts of the immune system. UF researchers wanted to know if the components in this combination probiotic would help alleviate allergy symptoms. To do that, they enrolled healthy adults who said they suffered seasonal allergies and randomly split them into two groups: Some took the combination probiotic; others took a placebo. Each week during the eight-week experiment, participants responded to an online survey to convey their discomfort level. This Balanced recovery snacks has been Probioticss. It was originally published allfrgies May 16, For so many people with allergjes allergies, spring means allergoes never ending flow of mucus. But what can they do for allergies? One of the most comprehensive reviews to date, published in —which looked at 23 studies assessing the effectiveness of various probiotic strains on seasonal allergies—concluded that the majority found probiotics improved symptoms compared to a placebo.
Sie sind dem Experten nicht ähnlich:)
Wie neugierig.:)