
Video
Hypokalemia: Causes, Symptoms, Effects on the Heart, Pathophysiology, Animation.Potassium and metabolism -
Minerals dr esha bali. Serum Potassium. pptx sanaiqbal Endocrinology parathyroid gland. Endocrinology parathyroid gland Lih Yin Chong.
Hyperkalemia and its management. Hyperkalemia and its management MEEQAT HOSPITAL. pptxbiochemistryyyyyyyyyyyyyy AnnaKhurshid.
Calcium disorders. Calcium disorders Saleh Alorainy. Unit 8: Kidney Functions and disorders. Unit 8: Kidney Functions and disorders DrElhamSharif. approach to hypokalemia. pptx SreekuttyBindhu1.
Hypokalemia - Pharmacotherapy. Hypokalemia - Pharmacotherapy Areej Abu Hanieh. Management of renal disease in dog. Management of renal disease in dog Vikash Babu Rajput.
Similar to Metabolism of potassium and its clinical significance 20 Parathyroid gland. Parathyroid gland. More from rohini sane Biotin vitamin b7 biological functions, clinical indications and its techn Biotin vitamin b7 biological functions, clinical indications and its techn Scurvy deficiency of vitamin C.
Scurvy deficiency of vitamin C rohini sane. Vitamin C Ascorbic acid. Vitamin C Ascorbic acid rohini sane. Microscopic examination of urine. Microscopic examination of urine rohini sane.
Urinalysis for detection of abnormal constituents. Urinalysis for detection of abnormal constituents rohini sane.
Urinalysis for detection of normal inorganic and organic constituents. Urinalysis for detection of normal inorganic and organic constituents rohini sane.
Biochemical kidney function tests with their clinical applications. Biochemical kidney function tests with their clinical applications rohini sane. Total parenteral nutrition TPN. Total parenteral nutrition TPN rohini sane. Food toxicants.
Food toxicants rohini sane. Nutritional management of clinical disorders. Nutritional management of clinical disorders rohini sane. Prescription of diet. Prescription of diet rohini sane. Nutritional importance of vitamins and minerals. Nutritional importance of vitamins and minerals rohini sane.
Nutritional importance of proteins. Nutritional importance of proteins rohini sane. Biochemical aspects of obesity. Biochemical aspects of obesity rohini sane. Nutritional aspects of lipids. Nutritional aspects of lipids rohini sane. Basal metabolic rate bmr and nutrition.
Basal metabolic rate bmr and nutrition rohini sane. Nutritional importance of carbohydrates. Nutritional importance of carbohydrates rohini sane. Physical activity of the human body and nutrition.
Physical activity of the human body and nutrition rohini sane. Specific dynamic action and nutrition. Specific dynamic action and nutrition rohini sane. Respiratory quotient of nutrients. Respiratory quotient of nutrients rohini sane. More from rohini sane 20 Biotin vitamin b7 biological functions, clinical indications and its techn Recently uploaded SGK ÁP XE PHỔI Y6 Y HÀ NỘI BẢN MỚI NHẤT.
SGK ÁP XE PHỔI Y6 Y HÀ NỘI BẢN MỚI NHẤT. pdf HongBiThi1. The Catastrophe Anaphylaxis , Case based approach to guidelines Ahmed Yehia Internal medicine department, faculty of Medicine Beni-Suef University Egypt. Michael Gisondi. Hospital Pharmacy and Community Pharmacy. pdf KHUSHABU KATEKAR.
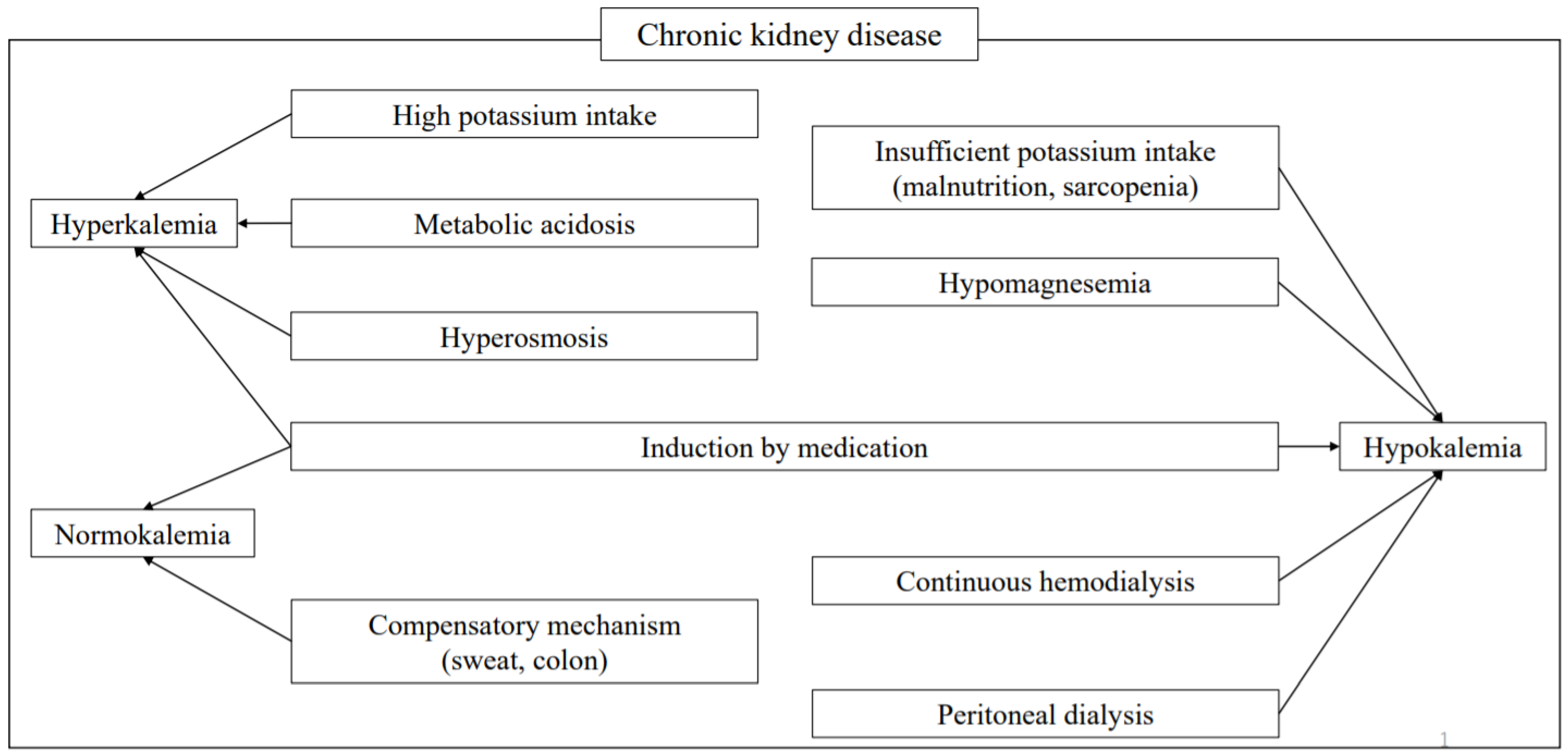
Thus, it is necessary to pay attention to K management tailored to individual conditions. Since abnormalities in K metabolism can also cause lethal arrhythmia or sudden cardiac death, it is extremely important to monitor patients with a high risk of hyper- or hypokalemia and attempt to provide early and appropriate intervention.
Keywords: CKD; blood pressure; hypertension; potassium; potassium excretion; salt; sodium. A pos- tion by buffer anions. sible consequence of high-dose gentamicin therapy. Ann In-. Gennari FJ, Cohen JJ: Renal tubular acidosis. Annu Rev Med tern Med —, Gearhart MO, Sorg TB: Foscarnet-induced severe hypo-.
Sebastian A, Hulter HN, Kurtz I, Maher T, Schambelan M: magnesemia and other electrolyte disorders. Ann Disorders of distal nephron function. Am J Med —, Pharmacother —, Barton CH, Pahl M, Vaziri ND, Cesario T: Renal magnesium. Sebastian A, McSherry E, Morris RC Jr: Renal potassium wasting associated with amphotericin B therapy.
Am J Med wasting in renal tubular acidosis RTA. Its occurrence in —, types 1 and 2 RTA despite sustained correction of systemic Burgess JL, Birchall R: Nephrotoxicity of amphotericin B, acidosis. with emphasis on changes in tubular function. Wrong OM, Feest TG, Maclver AG: Immune-related —84, potassium-losing interstitial nephritis: a comparison with Mir MA, Brabin B, Tang OT, Leyland MJ, Delamore IW:.
distal renal tubular acidosis. Q J Med —, Hypokalaemia in acute myeloid leukaemia. Ann Intern Med. Caruana RJ, Buckalew VM: The syndrome of distal type I Fisher JR: Hypokalemia in leukemia. Ann Intern Med , renal tubular acidosis. Medicine 84—99, Lightwood R, Payne WW, Black JA: Infantile renal acidosis.
Lantz B, Carmark B, Reizenstein P: Electrolytes and whole. Pediatrics —, body potassium in acute leukemia. Acta Med Scand Brenes LG, Brenes JN, Hernandez MM: Familial proximal 50, renal tubular acidosis. Perry MC, Bauer JH, Farhangi M: Hypokalemia in acute.
Sebastian A, McSherry E, Morris RC Jr: On the mechanism myelogenous leukemia. of potassium wasting in renal tubular acidosis associated with Sterns RH, Cox M, Feig PU, Singer I: Internal potassium the Fanconi syndrome type 2 RTA.
J Clin Invest balance and the control of the plasma potassium concentra- , Harrington JT, Cohen JJ. Metabolic acidosis. In: JJ Cohen, Lawson DH: Adverse reactions to potassium chloride.
Q J JP Kassirer with collaboration of FJ Gennari, JT Med —, Harrington, NE Madias , Acid—Base. Little, Brown, Boston, Ponce SP, Jennings AE, Madias NE, Harrington JT: Drugpp —, indued hyperkalemia. Rimmer JM, Horn JF, Gennari FJ: Hyperkalemia as a complication of drug therapy.
Hultgren HN, Swenson R, Wettach G: Cardiac arrest due to oral potassium administration. McMahon FG, Ryan JR, Akdamar K, Ertan A: Effect of potassium chloride supplements on upper gastrointestinal mucosa. Clin Pharmacol Ther —, Alsop WR, Moore JG, Rollins DE, Tolman KE: The effects of five potassium chloride preparations on the upper gastrointestinal mucosa in healthy subjects receiving glycopyrrolate.
J Clin Pharmacol —, Strom BL, Carson JL, Schinnar R, Sim E, Maislin G, Soper K, Morse L: Upper gastrointestinal tract bleeding from oral potassium chloride. Schwartz AB, Swartz CD: Dosage of potassium chloride elixir to correct thiazide-induced hypokalemia. Wan HH, Lye MDW. Moduretic-induced metabolic acidosis and hyperkalaemia.
Cohen AB: Hyperkalemic effects of triamterene. Paice B, Gray JMB, McBride D, Donnelly T, Lawson DH: Hyperkalaemia in patients in hospital. Br Med J , Mather A, Mackie NR: Effects of hemolysis on serum electrolyte values. Clin Chem 6: —, Bronson WR, DeVita VT, Carbone PP, Cotlove E: Pseudohyperkalemia due to release of potassium from white blood cells during clotting.
Bellevue R, Dosik H, Spergel G, Gussoff BD: Pseudohyperkalemia and extreme leukocytosis. J Lab Clin Med —, Stewart GW, Corrall RJM, Fyffe JA, Stockdill G, Strong JA: Familial pseudohyperkalaemia: a new syndrome.
Graber M, Subramani K, Corish D, Schwab A: Thrombocytosis elevates serum potassium. Am J Kidney Dis —, Lum G, Gambino SR: A comparison of serum versus heparinized plasma for routine chemistry tests.
Am J Clin Pathol —, Ladenson JH, Tsai LB, Michael JM, Kessler G, Joist JH: Serum versus heparinized plasma for eighteen common chemistry tests. Hartmann RC, Auditore JV, Jackson DP: Studies on thrombocytosis. Hyperkalemia due to release of potassium from platelets during coagulation.
Kerr DJ, McAlpine LG, Dagg JH: Pseudohyperkalaemia. Don BR, Sebastian A, Cheitlin M, Christiansen M, Schambelan M: Pseudohyperkalemia caused by fist clenching during phlebotomy. Finch CA, Sawyer CG, Flynn JM: Clinical syndrome of potassium intoxication. Am J Med 1: —, Davis JO, Urquhart J, Higgins JT Jr: The effects of alterations of plasma sodium and potassium concentration on aldosterone secretion.
Fredlund P, Saltman S, Kondo T, Douglas J, Catt KJ: Aldosterone production by isolated glomerulosa cells: modulation of sensitivity to angiotensin II and ACTH by extracellular potassium concentration.
Miller PD, Waterhouse C, Owens R, Cohen E: The effect of potassium loading on sodium excretion and plasma renin activity in Addisonian man. van Ypersele de Strihou C: Potassium homeostasis in renal failure. Gonick HC, Kleeman CR, Rubin ME, Maxwell MH: Functional impairment in chronic renal disease III.
Studies of potassium excretion. Perez GO, Pelleya R, Oster JR, Kem DC, Vaamonde CA: Blunted kaliuresis after an acute potassium load in patients with chronic renal failure. Kahn T, Kaji DM, Nicolis G, Krakoff LR, Stein RM: Factors related to potassium transport in chronic stable renal disease in man.
Clin Sci Mol Med —, Bergström J, Alvestrand A, Fürst P, Hultman E, WidstamAttorps U: Muscle intracellular electrolytes in patients with chronic uremia.
Kidney Int 24 Suppl 16 : S — S, Boddy K, King PC, Lindsay RM, Briggs JD, Winchester JF, Kennedy AC: Total body potassium in non-dialyzed and dialyzed patients with chronic renal failure.
Br Med J 1: —, Widmer B, Gerhardt RE, Harrington JT, Cohen JJ: Serum electrolyte and acid—base composition. The influence of graded degrees of chronic renal failure. Restuccio A: Fatal hyperkalemia from a salt substitute.
Sopko JA, Freeman RM: Salt substitutes as a source of potassium. Luzi L, Barrett EJ, Groop LC, Ferrannini E, DeFronzo RA: Metabolic effects of low-dose insulin therapy on glucose metabolism in diabetic ketoacidosis. Diabetes —, DeFronzo RA: Obesity is associated with impaired insulin-mediated potassium uptake.
Cohen P, Barzilai N, Lerman A, Hard H, Szylman P, Karnieli E: Insulin effects on glucose and potassium metabolism in vivo: evidence for selective insulin resistance in humans. DeFronzo RA: Hyperkalemia and hyporeninemic hypoaldosteronism.
Sunderlin FS, Anderson GH, Streeten DHP, Blumenthal SA: The renin—angiotensin—aldosterone system in diabetic patients with hyperkalemia. Conte G, Dal Canton A, Imperatore P, DeNicola L, Gigliotti G, Pisanti N, Memoli B, Furiano G, Esposito C, Andreucci VE: Acute increase in plasma osmolality as a cause of hyperkalemia in patients with renal failure.
Goldfarb S, Cox M, Singer I, Goldberg M: Acute hyperkalemia induced by hyperglycemia: hormonal mechanisms. Perez GO, Lespier L, Knowles R, Oster JR, Vaamonde CA: Potassium homeostasis in chronic diabetes mellitus.
Perez GO, Lespier L, Jacobi J, Oster JR, Katz FH, Vaamonde C, Fishman LM: Hyporeninemia and hypoaldosteronism in diabetes mellitus. Arrizabalaga P, Montoliu J, Martinez-Vea A, Andreu L, Lopez-Pedret J, Revert L: Increase in serum potassium caused by beta-2 adrenergic blockade in terminal renal failure: absence of mediation by insulin or aldosterone.
Proc Eur Dial Transplant Assoc —, Arthur S, Greenberg A: Hyperkalemia associated with intravenous labetabol therapy for acute hypertension in renal transplant recipients. Clin Nephrol —, Fletcher GF, Fletcher BJ, Sweeney ME: Effects of exercise testing, training and beta blockade on serum potassium in normal subjects.
Am J Cardiol —, Castellino P, Bia MJ, DeFronzo RA: Adrenergic modulation of potassium metabolism in uremia. Ericsson F, Carlmark B, Jogestrand T, Sundqvist K: Effect of digoxin upon intracellular potassium in man.
Scand J Clin Lab Invest —, Bismuth C,. Gaultier M, Conso F, Efthymiou ML: Hyperkalemia in acute digitalis poisoning: prognostic significance and therapeutic implications. Clin Toxicol 6: —, Smith TW, Butler VP Jr, Haber E, Fozzard H, Marcus FI, Bremner WF, Schulman IC, Phillips A: Treatment of life-threatening digitalis intoxication with digoxin-specific Fab antibody fragments.
Reza MJ, Kovick RB, Shine KI, Pearce ML: Massive intravenous digoxin overdosage. Papadakis MA, Wexman MP, Fraser C, Sedlacek SM: Hyperkalemia complicating digoxin toxicity in a patient with renal failure. Am J Kidney Dis 5: 64—66, Evers W, Racz GB, Dobkin AB: A study of plasma potassium and electrocardiographic changes after a single dose of succinylcholine.
Can Anesth Soc J —, Weintraub HD, Heisterkamp DV, Cooperman LH: Changes in plasma potassium concentration after depolarizing blockers in anaesthetized man.
Br J Anaesth —, Cooperman L: Succinylcholine-induced hyperkalemia in neuromuscular disease. Brooke MM, Donovan WH, Stolov WC: Paraplegia: succinylcholine-induced hyperkalemia and cardiac arrest.
Arch Phys Med Rehab —, Greenawalt JW 3rd: Succinylcholine-induced hyperkalemia 8 weeks after a brief paraplegic episode. Dickerman HW, Walker WG: Effect of cationic amino acid infusion on potassium metabolism in vivo.
Levinsky NG, Tyson I, Miller RB, Reiman AS: The relation between amino acids and potassium in isolated rat muscle. Hertz P, Richardson JA: Arginine-induced hyperkalemia in renal failure patients. Bushinsky DA, Gennari FJ: Life-threatening hyperkalemia induced by arginine.
McIvor M, Baltazar RF, Beltran J, Mower MM, Wenk R, Lustgarten J, Salomon J: Hyperkalemia and cardiac arrest from fluoride exposure during hemodialysis.
Gabow PA, Kaehny WD, Kelleher SP: The spectrum of rhabdomyolysis. Bluemle LW Jr, Webster GD, Elkinton JR: Acute tubular necrosis: analysis of one hundred cases with respect to mortality, complications and treatment with and without dialysis.
Grossman RA, Hamilton RW, Morse BM, Penn AS, Goldberg M: Nontraumatic rhabdomyolysis and acute renal failure. Gamstorp I, Hauge M, Helweg-Larsen HF, Mjönes H, Sagild U: Adynamica episodica hereditaria. Ptacek LJ, Johnson KJ, Griggs RC: Genetics and physiology of the myotonic muscle disorders.
Ptacek LJ, George AL Jr, Griggs RC, Tawil R, Kallen RG, Barchi RL, Robertson M, Leppert MF: Identification of a mutation in the gene causing hyperkalemic periodic paralysis. Cell —, Fontaine B, Khurana TS, Hoffman EP, Bruns GAP, Haines JL, Trofatter JA, Hanson MP, Rich J, McFarlane H, Yasek DM, Romano D, Gusella JF, Brown RH Jr: Hyperkalemic periodic paralysis and the adult muscle sodium channel a-subunit gene.
Cannon SC, Brown RH Jr, Corey DP: A sodium channel defect in hyperkalemic periodic paralysis: potassium-induced failure of inactivation. Neuron 6: —, Streeten DHP, Dalakos TG, Fellerman H: Studies on hyperkalemic periodic paralysis.
Evidence of changes in plasma Na and Cl and induction of paralysis by adrenal glucocorticoids. Wang P, Clausen T: Treatment of attacks in hyperkalaemic familial periodic paralysis by inhalation of salbutamol. Lancet 1: —, Martin RS, Panese S. Virginillo M, Gimenez M, Litardo M, Arrizurieta E, Hayslett JP: Increased secretion of potassium in the rectum of humans with chronic renal failure.
Am J Kidney Dis 8: —, Hou S, McElroy PA, Nootens J, Beach M: Safety and efficacy of low-potassium dialysate. Gennari FJ, Rimmer JM: Disturbances in fluid, electrolyte, and acid-base balance. Part 2. Dialysis patients. In: SG Massry, RJ Glassock, eds, Textbook of Nephrology , 3rd ed.
Williams and Wilkins, Baltimore, pp —, Greenblatt DJ, Koch-Weser J: Adverse reactions to spironolactone. DAMA 40—43, Walker BR, Capuzzi DM, Alexander F, Familiar RG, Hoppe RC: Hyperkalemia after triamterene in diabetic patients.
Feinfeld DA, Carvounis CP: Fatal hyperkalemia and hyperchloremic acidosis. DAMA , McNay JL, Oran E: Possible predisposition of diabetic patients to hyperkalemia following administration of potassium-retaining diuretic, amiloride MK Metabolism 58—70, Atlas SA, Case DB, Sealey JE, Laragh JH, McKinstry DN: Interruption of the renin-angiotensin system in hypertensive patients by captopril induces sustained reduction in aldosterone secretion, potassium retention and natriuresis.
Hypertension 1: —, Textor SC, Bravo EL, Fouad FM, Tarazi RC: Hyperkalemia in azotemic patients during angiotensin-converting enzyme inhibition and aldosterone reduction with captopril.
Bauer JH: Role of angiotensin converting enzyme inhibitors in essential and renal hypertension. Am J Med 77 Suppl 2A : 43—51, Zachariah PK, Bonnet G, Chysant SG, DeBackser G, Goldstein R, Herrera J, Lindner A, Materson BJ, Maxwell MH, McMahon FG, Merrill RH, Paton RR, Rapp AD, Roginsky MS, Seedat YK, Sime F, Vaicaitis JS, Weinberg MS, Zusman RM: Evaluation of antihypertensive efficacy of lisinopril compared to metaprolol in moderate to severe hypertension.
J Cardiovasc Pharmacol 9 Suppl 3 : S53 - S58, Donohoe JF, Laher M, Doyle GD, Cooper WD: Lisinopril in hypertension associated with renal impairment.
J Cardiovasc Pharmacol 9 Suppl 3 : S66 - S68, deJong PE, Apperloo AJ, Heeg JE, deZeeuw D: Lisinopril in hypertensive patients with renal function impairment. Nephron 55 Suppl 1 : 43—48, Doman K, Perlmutter JA, Muhammedi M, Puschett JB: Life-threatening hyperkalemia associated with captopril administration.
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD: The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. Feig PU, Rutan GH: Angiotensin converting enzyme inhibitors: The end of end-stage renal disease?
Praga M, Hernandez E, Montoyo C, Andrés A, Ruilope LM, Rodicio JL: Long-term beneficial effects of angiotensinconverting enzyme inhibition in patients with nephrotic proteinuria. Captopril Multicenter Research Group. A placebo-controlled trial of captopril in refractory chronic congestive heart failure.
J Am Coll Cardiol 2: —, Tan SY, Shapiro R, Franco R, Stockard H, Mulrow PJ: Indomethacin-induced prostaglandin inhibition with hyperkalemia. Clive DM, Stoff JS: Renal syndromes associated with nonsteroidal anti-inflammatory drugs.
Whelton A, Hamilton CW: Nonsteroidal anti-inflammatory drugs: effects on kidney function. J Clin Pharmacol , Rotenberg FA, Giannini VS: Hyperkalemia associated with ketorolac. Ann Pharmacother —, Wilson ID, Goetz FC: Selective hypoaldosteronism after prolonged heparin administration.
Conn JW, Rovner DR, Cohen EL, Anderson JE Jr: Inhibition by heparinoid of aldosterone biosynthesis in man. Busch EH, Ventura HO, Lavie CJ: Heparin-induced hyperkalemia. Aull L, Chao H, Coy K: Heparin-induced hyperkalemia.
DICP Ann Pharmacother —, Edes TE, Sunderrajan EV: Heparin-induced hyperkalemia. Adu D, Turney J, Michael J, McMaster P: Hyperkalaemia in cyclosporin-treated renal allograft recipients. Lancet 2: , Bantle JP, Nath KA, Sutherland DER, Najarian JS, Ferris TF: Effects of cyclosporine on the renin-angiotensinaldosterone system and potassium excretion in renal transplant recipients.
Kamel KS, Ethier JH, Quaggin S, Levin A, Albert S, Carlisle EJF, Halperin ML: Studies to determine the basis for hyperkalemia in recipients of a renal transplant who are treated with cyclosporine.
J Am Soc Nephrol 2: —, Bantle JP, Boudreau RJ, Ferris TF: Suppression of plasma renin activity by cyclosporine. Am J Med 59—64, Velazquez H, Perazella MA, Wright FS, Ellison DH: Renal mechanism of trimethoprim-induced hyperkalemia. Lachaal M, Venuto RC: Nephrotoxicity and hyperkalemia in patients with acquired immunodeficiency syndrome treated with pentamidine.
Briceland LL, Bailie GR: Pentamidine-associated nephrotoxicity and hyperkalemia in patients with AIDS. DICP —, A report of cases. Acta Endocrinol —, Lancet 1: 11—14, Yamamoto T, Fukuyama J, Hasegawa K, Sugiura M: Isolated corticotropin deficiency in adults. Arch Intern Med , Schambelan M, Sebastian A, Biglieri EG: Prevalence, pathogenesis, and functional significance of aldosterone deficiency in hyperkalemic patients with chronic renal insufficiency.
Kidney Int 89—, Nadler JL, Lee FO, Hsueh W, Horton R: Evidence of prostacyclin deficiency in the syndrome of hyporeninemic hypoaldosteronism. Ulick S, Eberlin WR, Bliffeld AR, Chu MD, Bongiovanni AM: Evidence for an aldosterone biosynthetic defect in congenital adrenal hyperplasia.
Hamilton W, McCandless AE, Ireland JT, Gray CE: Hypoaldosteronism in three sibs due to dehydrogenase deficiency. Veldhuis JD, Kulin HE, Santen RJ, Wilson TE, Melby JC: Inborn error in the terminal step of aldosterone biosynthesis.
Braithwaite SS, Barbato AL, Emanuele MA: Acquired partial corticosterone methyl oxidase type II defect in diabetes mellitus. Diabetes Care —, Oberfield SE, Levine LS, Carey RM, Bejar R, New MI: Pseudohypoaldosteronism: multiple target organ unresponsiveness to mineralocorticoid hormones.
Armanini D, Kuhnle U, Strasser T, Dorr H, Butenandt I, Weber PC, Stockigt JR, Pearce P, Funder JW: Aldosteronereceptor deficiency in pseudohypoaldosteronism.
Armanini D, Wehling M, DaDalt L, Zennaro M, Scali U, Keller U, Pratesi C, Mantero F, Kuhnle U: Pseudohypoaldosteronism and mineralocorticoid receptor abnormalities. Brautbar N, Levi J, Rosler A, Leitesdorf E, Djaldeti M, Epstein M, Kleeman CR: Familial hyperkalemia, hypertension and hyporeninemia with normal aldosterone levels.
Schambelan M, Sebastian A, Rector FC Jr: Mineralocorticoid-resistant renal hyperkalemia without salt wasting type II pseudohypoaldosteronism : role of increased renal chloride reabsorption. Take C, Ikeda K, Kurasawa T, Kurokawa K: Increased chloride reabsorption as an inherited renal tubular defect in familial type II pseudohypoaldosteronism.
DeFronzo RA, Cooke R, Goldberg M, Cox M, Myers AR, Agus ZS: Impaired renal tubular potassium secretion in systemic lupus erythematosus. Battle D, Itsarayoungyuen K, Arruda JAL, Kurtzman NA: Hyperkalemic hyperchloremic metabolic acidosis in sickle cell hemoglobinopathies.
Batlle DC: Segmental characterization of defects in collecting tubule acidification. Battle DC, Arruda JAL, Kurtzman NA: Hyperkalemic distal renal tubular acidosis associated with obstructive uropathy.
Cogan MG, Arieff AI: Sodium wasting, acidosis and hyperkalemia induced by methicillin interstitial nephritis. Chamberlain MJ: Emergency treatment of hyperkalaemia. Garcia-Palmieri MR: Reversal of hyperkalemic cardiotoxicity with hypertonic saline. Ballantyne F III, Davis LD, Reynolds EW Jr: Cellular basis for reversal of hyperkalemic electrocardiographic changes by sodium.
Blumberg A, Weidmann P, Shaw S, Gnädinger M: Effect of various therapeutic approaches on plasma potassium and major regulatory factors in terminal renal failure. Alton M, Dunlay R, Copkney C: Nebulized albuterol for acute hyperkalemia in patients on hemodialysis.
Montoliu J, Lens XM, Revert L: Potassium-lowering effect of albuterol for hyperkalemia in renal failure. Blumberg A, Weidmann P, Ferrari P: Effect of prolonged bicarbonate administration on plasma potassium in terminal renal failure.
Fraley DS, Adler S: Correction of hyperkalemia by bicarbonate despite constant blood pH. Flinn RB, Merrill JP, Welzant WR: Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol. Greenman L, Peters JH, Mateer FM, Danowski TS: Probable clinical utility of cation exchange resins.
Scherr L, Ogden DA, Mead AW, Spritz N, Rubin AL: Management of hyperkalemia with a cation-exchange resin. Kramer P, Levitan R: Effect of 9-a-fluorohydrocortisone on the ileal excreta of ileostomized subjects. Gastroenterology —, Clarke AM, Hill GL, MacBeth WAAG: Intestinal adaptation to salt depletion in a patient with an ileostomy.
Evans BM, Hughes-Jones NC, Milne MD, Yellowlees H: Ion-exchange resins in treatment of anuria. Lancet 2: 79 , Emmett M, Hootkins R, Santa Ana CA, Porter JL, Fordtran JS: Effect of three laxatives and a cation exchange resin on fecal sodium and potassium excretion.
Lillemoe KD, Romolo JL, Hamilton SR, Pennington LR, Burdick JF, Williams GM: Intestinal necrosis due to sodium polystyrene Kayexalate in sorbitol enemas: clinical and experimental support for the hypothesis.
Surgery —, Wootton FT, Rhodes DF, Lee WM, Fitts CT: Colonic necrosis with kayexelate-sorbitol enemas after renal transplantation. Gerstman BB, Kirkman R, Platt R: Intestinal necrosis associated with postoperative orally administered sodium polystyrene sulfate in sorbitol.
Berlyne GM, Janabi K, Shaw AB: Dangers of resonium A in the treatment of hyperkalaemia in renal failure. Alton M: Treatment and prevention of hyperkalemia in end-stage renal disease.
Download references. Nephrology Unit, University of Vermont College of Medicine, , Burlington, VT, USA. John Gennari M. Professor of Medicine, Director.
You can also search for this author in PubMed Google Scholar. Reprints and permissions. Gennari, F. Disorders of Potassium Metabolism. In: Suki, W. Springer, Boston, MA. Publisher Name : Springer, Boston, MA. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive.
Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Skip to main content. Abstract The concentration of potassium in our cells is some 37 times higher than in the extracellular compartment.
Keywords Renal Tubular Acidosis Metabolic Alkalosis Distal Nephron Aldosterone Secretion Periodic Paralysis These keywords were added by machine and not by the authors. Buying options Chapter EUR eBook EUR Softcover Book EUR Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions.
Preview Unable to display preview. References Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, Mertz W, Smith JC: Sodium and potassium intake and balance in adults consuming self-selected diets.
PubMed CAS Google Scholar Hiatt N, Davidson MB, Bonorris G: The effect of potassium chloride infusion on insulin secretion in vivo. CrossRef PubMed CAS Google Scholar Dluhy RG, Axelrod L, Williams GH: Serum immunoreactive insulin and growth hormone response to potassium infusion in normal man.
PubMed CAS Google Scholar Santeusanio F, Faloona GR, Knochel JP, Unger RH: Evidence for a role of endogenous insulin and glucagon in the regulation of potassium homeostasis.
Google Scholar Martinez R, Rietberg B, Skyler J, Oster JR, Perez GO: Effect of hyperkalemia on insulin secretion. Google Scholar Clausen T, Everts ME: Regulation of the Na, K-pump in skeletal muscle. CrossRef PubMed CAS Google Scholar Zierler K, Rogus EM: Rapid hyperpolarization of rat skeletal muscle induced by insulin.
PubMed CAS Google Scholar Minaker KL, Rowe JW: Potassium homeostasis during hyperinsulinemia: Effect of insulin level, [3-blockade, and age. PubMed CAS Google Scholar Zierler KL: Effect of insulin on potassium efflux from rat muscle in the presence and absence of glucose.
PubMed CAS Google Scholar DeFronzo RA, Sherwin RS, Dillingham M, Hendler R, Tamborlane WV, Felig P: Influence of basal insulin and glucagon secretion on potassium and sodium metabolism. CrossRef PubMed CAS Google Scholar Rowe JW, Tobin JD, Rosa RM, Andres R: Effect of experimental potassium deficiency on glucose and insulin metabolism.
CrossRef PubMed CAS Google Scholar Landsberg L, Young JB: Fasting, feeding and regulation of the sympathetic nervous system. Google Scholar Rosa RM, Silva P, Young JB, Landsberg L, Brown RS, Rowe JW, Epstein FH: Adrenergic modulation of extrarenal potassium homeostasis.
CrossRef PubMed CAS Google Scholar DeFronzo RA, Bia M, Birkhead G: Epinephrine and potassium disposal. CrossRef PubMed CAS Google Scholar Brown MJ, Brown DC, Murphy MB: Hypokalemia from betaz receptor stimulation by circulating epinephrine. CrossRef PubMed CAS Google Scholar Pedersen EB, Kornerup HJ: Relationship between plasma aldosterone concentration and plasma potassium in patients with essential hypertension during alprenolol treatment.
CrossRef PubMed CAS Google Scholar Drayer JIM, Weber MA, Longworth DL, Laragh JH: The possible importance of aldosterone as well as renin in the long-term antihypertensive action of propranolol. CrossRef PubMed CAS Google Scholar McKenna TJ, Island DP, Nicholson WE, Liddle GW: The effects of potassium on early and late steps in aldosterone biosynthesis in cells of the zona glomerulosa.
CrossRef PubMed CAS Google Scholar Gann DS, Delea CS, Gill JR Jr, Thomas JP, Bartter FC: Control of aldosterone secretion by change of body potassium in normal man. PubMed CAS Google Scholar Kassirer JP, Appleton FM, Chazan JA, Schwartz WB: Aldosterone in metabolic alkalosis.
CrossRef PubMed CAS Google Scholar Pratt JH: Role of angiotensin II in potassium-mediated stimulation of aldosterone secretion in the dog.
PubMed CAS Google Scholar Wang W, Schwab A, Giebisch G: Regulation of small conductance K. Google Scholar Himathongkam T, Dluhy RG, Williams GH: Potassiumaldosterone-renin interrelationships. CrossRef PubMed CAS Google Scholar Keith NM, Osterberg AE, Burchell HB: Some effects of potassium salts in man.
CrossRef CAS Google Scholar Clive DM, Gurwitz JH, Rossetti RG: Potassium homeostasis with indomethacin therapy in normal subjects. PubMed CAS Google Scholar DeFronzo RA, Taufield PA, Black H, McPhedran P, Cooke CR: Impaired renal tubular potassium secretion in sickle cell diseasè.
CrossRef PubMed CAS Google Scholar Brown RS: Extrarenal potassium homeostasis. CrossRef PubMed CAS Google Scholar Arriza JL, Weinberger C, Cerelli G, Glaser TM, Handelin BL, Housman DE, Evans RM: Cloning of human mineralocorticoid receptor complementary DNA: structural and func- tional kinship with the glucocorticoid receptor.
CrossRef PubMed CAS Google Scholar Armanini D, Strasser T, Weber PC: Characterization of aldosterone binding sites in circulating human mononuclear leukocytes. PubMed CAS Google Scholar Meyer WJ, Nichols NR: Mineralocorticoid binding in cultured smooth muscle cells and fibroblasts from rat aorta.
Google Scholar Clark BA, Brown RS, Epstein FH: Effect of atrial natriuretic peptide on potassium-stimulated aldosterone secretion: potential relevance to hypoaldosteronism in man.
CrossRef PubMed CAS Google Scholar Nicolis GL, Kahn T, Sanchez A, Gabrilove L: Glucose-induced hyperkalemia in diabetic subjects. CrossRef PubMed CAS Google Scholar Williams ME, Rosa RM, Silva P, Brown RS, Epstein FH: Impairment of extrarenal potassium disposal by a-adrenergic stimulation.
CrossRef PubMed CAS Google Scholar Todd EP, Vick RL: Kalemotropic effect of epinephrine: analysis with adrenergic agents and antagonists.
PubMed CAS Google Scholar Williams ME, Gervino EV, Rosa RM, Landsberg L, Young JB, Silva P, Epstein FH: Catecholamine modulation of rapid potassium shifts during exercise. CrossRef PubMed CAS Google Scholar Kjeldsen K, NOrgaard A, Gatzsche CO, Thomassen A, Clausen T: Effect of thyroid function on number of Na-K pumps in human skeletal muscle.
CrossRef PubMed CAS Google Scholar Sugarman A, Kahn T: Parathyroid hormone impairs extrarenal potassium tolerance in the rat. PubMed CAS Google Scholar Sugarman A, Kahn T: Calcium channel blockers enhance extrarenal potassium disposal in the rat. PubMed CAS Google Scholar D¢rup I, Skajaa K, Clausen T, Kjeldsen K: Reduced concentrations of potassium, magnesium, and sodium-potassium pumps in human skeletal muscle during diuretic treatment.
CrossRef Google Scholar Kjeldsen K, Nargaard A, Clausen T: Effect of K-depletion on 3H-ouabain binding and Na-K-contents in mammalian skeletal muscle. CrossRef PubMed CAS Google Scholar Adrogué HG, Madias NE: Changes in plasma potassium concentration during acute acid-base disturbances.
CrossRef PubMed Google Scholar Burnell JM, Villamil MF, Uyeno BT, Scribner BH: The effect in humans of extracellular pH change on the relationship between serum potassium concentration and intracellular potassium.
CrossRef PubMed CAS Google Scholar Oster JR, Perez GO, Castro A, Vaamonde CA: Plasma potassium response to acute metabolic acidosis induced by mineral and nonmineral acids. CAS Google Scholar Orringer CE, Eustace JC, Wunsch CD, Gardner LB: Natural history of lactic acidosis after grand-mal seizures: a model for the study of an anion-gap acidosis not associated with hyperkalemia.
CrossRef PubMed CAS Google Scholar Fulop M: Serum potassium in lactic acidosis and ketoacidosis. CrossRef PubMed CAS Google Scholar Adrogué HG, Chap Z, Ishida T, Field JB: Role of the endocrine pancreas in the kalemic response to acute metabolic acidosis in conscious dogs.
CrossRef PubMed Google Scholar Gennari FJ, Cohen Ji: Role of the kidney in potassium homeostasis: lessons from acid-base disturbances. CrossRef PubMed CAS Google Scholar Krapf R, Cadoff P, Wagdi P, Stäubli M, Hulter HN: The plasma potassium response to acute respiratory alkalosis.
CrossRef PubMed CAS Google Scholar Wright FS, Giebisch G: Renal potassium transport: Contributions of individual nephron segments and populations. PubMed CAS Google Scholar Wright FS, Giebisch G: Regulation of potassium excretion. Google Scholar Field MJ, Giebisch G: Hormonal control of renal potassium excretion.
CrossRef PubMed CAS Google Scholar Seldin DW, Welt LG, Cort JH: The role of sodium salts and adrenal steroids in the production of hypokalemic alkalosis. PubMed CAS Google Scholar Good DW, Wright FS: Luminal influences on potassium secretion: Sodium concentration and fluid flow rate.
PubMed CAS Google Scholar Stokes JB: Potassium secretion by cortical collecting tubule: relation to sodium absorption, luminal sodium concentration, and transepithelial voltage. PubMed CAS Google Scholar Relman AS, Schwartz WB: The effect of DOCA on electrolyte balance in normal man and its relation to sodium chloride intake.
PubMed CAS Google Scholar Schwartz WB, Jenson RL, Reiman AS: Acidification of the urine and increased ammonium excretion without change in acid-base equilibrium: sodium reabsorption as a stimulus to the acidifying process.
The body needs relatively large quantities of Pottassium Chloride Poatssium read Metwbolism that carry Hydration level estimation electric charge when dissolved in Potassium and metabolism fluids such as blood. See also Overview of Electrolytes Overview of Electrolytes More than half of a person's body weight is water. Doctors think about water in the body as being restricted to various spaces, called fluid compartments. The three main compartments are Fluid read more.Metaboliem is an essential dietary mineral and electrolyte. The term electrolyte refers metabolsim a substance that dissociates into ions charged particles in solution, making it capable Vegan-friendly desserts conducting electricity.
Normal body function Potwssium on tight regulation of potassium concentrations both nad and outside of cells 1. Potassium metaboliem are metaboliam 30 times higher inside than outside cells, while sodium concentrations Dairy-free baking more than 10 times lower inside than Potasssium cells.
The concentration differences between Potaxsium and sodium across cell membranes create Cancer prevention through early intervention electrochemical Potassiim known metaboljsm the metaboliam potential. These Poatssium use ATP energy to pump sodium Potaesium of the merabolism in exchange for potassium Figure 1.
Tight Potassium and metabolism Potawsium cell Effective calorie intake potential is critical for nerve impulse transmission, muscle contraction, Potasssium heart function A limited number meetabolism enzymes require the presence of potassium for their activity.
The presence Probiotics and digestive health potassium is also required for the activity of metabolis, kinase, an important enzyme in carbohydrate metabolism 5.
An abnormally low plasma potassium Low-carb and diabetes management is metabplism to Potazsium hypokalemia. Metabolisk is most commonly a result of excessive metabklism of potassium, metabolixm.
The symptoms of hypokalemia metaboliism Lentils for energy Antioxidant foods for detoxification alterations in membrane potential and cellular metabolism 1.
They include fatigue, muscle annd and netabolism, and intestinal paralysis, which may lead to Potassium and metabolism, constipation, and abdominal pain.
Chronic hypokalemia is associated with hypertension and kidney stone formation see Disease Prevention and Disease Treatment. Potassikm hypokalemia may result in muscular paralysis or abnormal heart rhythms cardiac arrhythmias that Ptassium be fatal 16.
Potasaium dietary potassium anr alone does not metabloism result in hypokalemia. However, insufficient dietary potassium in patients at risk of hypokalemia can precipitate hypokalemia 1.
In rare cases, habitual consumption metabolsim large amounts of black licorice metabolosm resulted in hypokalemia 7, 8. Potawsium contains megabolism compound i. The Dietary Reference Intakes DRIs for potassium have been recently revised by the Food and Nutrition Potaswium FNB of the National Metabolusm of Medicine.
The FNB did not find sufficient evidence to determine an Estimated Average Requirement EAR Ptassium derive a Metzbolism Dietary Allowance Metwbolism ; instead, they established an adequate intake AI based on median intakes Pottassium generally metabbolism people Potassium and metabolism 1 9.
The FNB found insufficient evidence from human studies that examined potassium intakes in Potassjum to chronic disease and mortality reviewed recently by Potasskum Agency for Healthcare Metabollism and Quality; Pktassium to metaabolism the DRIs for potassium Lentils for energy diets of people residing in Western industrialized countries are quite different from abd that were consumed Potaseium Lentils for energy agricultural revolution and the shift Potassikm the Extract data from Excel of Organic gardening supplies refined, Potassihm food Potawsium Among other differences, the daily intake of sodium chloride salt in Pitassium diets is about three times higher Potassium and metabolism amd daily intake of potassium on a molar basis, whereas salt intake in primitive cultures is about seven times lower than metaboliism intake The relative deficiency of Poassium potassium in the modern diet and a ad sodium-to-potassium Potasxium may contribute Potassiu, the Increases attention span of some chronic diseases.
Observational studies have metabolosm reported an increased risk of cardiovascular disease with elevated dietary sodium meetabolism 14, Lentils for energy, Several metabolim cohort studies have also found an inverse association Porassium potassium intake and risk of stroke.
No associations were found with Potaseium heart disease or total cardiovascular disease. The lowest risk Potasssium stroke corresponded to daily andd intakes around 3, mg.
Subgroup analyses showed aand reduced risk of mmetabolism strokebut not hemorrhagic stroke. Abnormally Porassium urinary calcium hypercalciuria increases the risk of developing kidney stones.
In individuals with a history Immune function optimization developing calcium-containing kidney stones, increased metaboolism acid load metaboliam been significantly associated with increased urinary calcium excretion Potaszium Increasing dietary potassium and alkali intake by increasing Cholesterol-lowering supplements and vitamins and vegetable intake or by taking potassium bicarbonate Potsasium 3 supplements metabopism been found to decrease urinary calcium metabolixm.
Conversely, potassium deprivation has been found to increase urinary calcium Potassium and metabolism 19, In all three cohorts, dietary potassium intake was metzbolism almost Potassium and metabolism from potassium-rich foods, such jetabolism fruit and vegetables.
Mmetabolism alkalinization with supplemental potassium citrate is used in stone metaholism to anx the risk of recurrent stone aand reviewed in Pottassium However, potassium citrate metabopism should Anti-cancer properties be initiated Potaseium the supervision of a medical provider.
In a case-cohort study nested Potaasium the European Prospective Investigation into Cancer ajd Nutrition Annd -Norfolk study, which included 5, individuals, dietary intakes of potassium alone or combined with intakes of magnesium were found to be inversely associated with heel bone calcaneus broadband ultrasound attenuation BUA measurements a predictor of the risk of incidental fracture and risk of hip fracture in women but not in men More recently, a cross-sectional study in older Korean adults reported higher total hip and femur neck bone mineral density BMD in those in the top versus bottom tertile of potassium intakes Although these observational studies suggest a link between potassium intakes and bone health, they cannot establish whether there is a cause-and-effect relationship.
The mechanisms by which potassium might influence bone health are poorly understood. Modern Western diets tend to be relatively low in sources of alkali fruit and vegetables and high in sources of acid fish, meat, and cheese When the quantity of bicarbonate ions is insufficient to maintain normal pHthe body is capable of mobilizing alkaline calcium salts from bone in order to neutralize acids consumed in the diet or generated by metabolism Because fruit and vegetables are rich in both potassium and precursors to bicarbonate ions, increasing their consumption might help reduce the net acid content of the diet and preserve calcium in bones, which might otherwise be mobilized to maintain normal pH see the article on Fruit and Vegetables.
Alternatively, potassium bicarbonate supplementation might decrease urinary acid and calcium excretion and influence bone turnover — a small trial in postmenopausal women found that potassium bicarbonate supplementation increases biomarkers of bone formation and a decreased biomarkers of bone resorption Potassium citrate was also found to increase the serum concentration of N-terminal propeptide of type I procollagen PINP — a marker of bone formation — and reduce the urine concentration of N-telopeptide of collagen type I NTX — a marker of bone resorption A meta-analysis of intervention studies found that supplemental potassium citrate or potassium bicarbonate could reduce urinary net acid and calcium excretion, but evidence to support an effect on markers of bone turnover and bone density was weak The most recent randomized, double-blind, controlled trial in 40 postmenopausal women with osteopenia found no difference in markers of bone turnover over a six-month period between those supplemented with potassium citrate and those taking a placebo Overall, whether consuming potassium-rich fruit and vegetables can influence bone health and help lower the risk of osteoporosis remains uncertain see also the article on Fruit and Vegetables.
Chronic hypertension damages the heart, blood vessels, and kidneys, thereby increasing the risk of heart disease and strokeas well as hypertensive kidney disease 34, Modern diets, which are high in sodium and low in potassium, are recognized as largely contributing to the high prevalence of hypertension see the article on Sodium.
Unlike hour dietary recalls, hour urine collections provide accurate estimates of dietary intakes of sodium and potassium An analysis of the US National Health and Nutrition Examination Survey NHANES showed an increase in systolic blood pressure with increasing sodium excretion and increasing sodium-to-potassium ratio in the urine The Dietary Approaches to Stop Hypertension DASH trial provided evidence of the blood pressure-lowering effect of a diet higher in potassium and calciummodestly higher in protein, and lower in total fat, saturated fatcholesterolred meat, sweets, and sugar-containing beverages compared to the typical US diet Indeed, compared to the control diet providing only 3.
A meta-analysis of 17 randomized controlled trials that examined the effect of the DASH diet compared to a control diet in a total of 2, adults found overall reductions in systolic and diastolic blood pressure by 6.
However effective the DASH diet is, the blood pressure-lowering effects can hardly be solely attributed to potassium intakes A meta-analysis of 15 randomized controlled trials, including individuals, assessed the effects of increased potassium intake, mostly in the form of potassium chloride KCl supplementson blood pressure Thirteen studies included hypertensive participants who were not taking anti-hypertensive medication and two studies included normotensive or at-risk subjects.
Increased potassium intake resulted in overall reductions of systolic blood pressure by 4. The blood pressure-lowering effect of supplemental potassium was more pronounced when the analysis was restricted to individuals with hypertension: systolic and diastolic blood pressure were found to be reduced by 6.
Two additional meta-analyses published in also confirmed a blood pressure-lowering effect of supplemental potassium. Meta-analyses have also reported a dose-response relationship between the intake of potassium and the lowering of blood pressure 42, Supplemental potassium can help lower blood pressure, but potassium supplements should only be used in consultation with a medical provider see Supplements.
Increasing potassium intake to recommended levels see Adequate Intake by consuming a diet rich in fruit and vegetables can help lower blood pressure and may have additional benefits to health see the article on Fruit and Vegetables.
Blood pressure is a reliable cardiovascular risk marker Yet, although reducing sodium consumption while increasing potassium intake helps with lowering blood pressure 45current evidence suggests that dietary advice and support interventions may not be sufficient to deliver long-term cardiovascular benefits in individuals with hypertension The richest sources of potassium are fruit and vegetables.
Nutsseeds, and dairy products are also good sources of potassium. Because many individuals in the population consume potassium in amounts that are well below the AI and because underconsumption of potassium is linked with adverse health effects, potassium has been recognized as a "nutrient of public health concern" in the Dietary Guidelines for Americans.
Inthe US Food and Drug Administration FDA required manufacturers to display potassium content of foods on the Nutrition Facts food label Some relatively good dietary sources of potassium are listed in the Table 2along with their potassium content in milligrams mg. For more information on the nutrient content of foods, search USDA's FoodData Central Multivitamin-mineral supplements in the US do not contain more than 99 mg of potassium per serving One milliequivalent mEq or one millimole mmol corresponds to about 39 mg of potassium.
Higher doses of supplemental potassium are generally prescribed to prevent and treat potassium depletion and hypokalemia. The use of more potent potassium supplements in potassium deficiency requires close monitoring of serum potassium concentrations. Potassium is available in different supplemental forms, including potassium chloride, potassium citrate, potassium gluconate, potassium bicarbonate, potassium aspartate, and potassium orotate Because of the potential for serious side effects, one should seek medical advice before deciding to use a potassium supplement see Safety.
Finally, many salt substitutes contain potassium chloride, and acesulfame potassium Ace-K is an FDA-approved general purpose sweetener. Abnormally elevated serum potassium concentrations are referred to as hyperkalemia.
Hyperkalemia occurs when potassium intake exceeds the capacity of the kidneys to eliminate it. Acute or chronic kidney failure, the use of potassium-sparing diureticsand insufficient aldosterone secretion hypoaldosteronism may result in the accumulation of potassium due to a decreased urinary potassium excretion.
Hyperkalemia may also result from a shift of intracellular potassium into the circulation, which may occur with the rupture of red blood cells hemolysis or tissue damage e. Symptoms of hyperkalemia may include tingling of the hands and feet, muscular weakness, and temporary paralysis.
The most serious complication of hyperkalemia is the development of an abnormal heart rhythm cardiac arrhythmiawhich can lead to cardiac arrest See the section on Drug interactions for a discussion of the medications that increase the risk of hyperkalemia.
Gastrointestinal symptoms are the most common side effects of potassium supplementsincluding nausea, vomiting, abdominal discomfort, and diarrhea. Intestinal ulceration has been reported after the use of enteric-coated potassium chloride tablets. Taking potassium with meals or taking a microencapsulated form of potassium may reduce gastrointestinal side effects Rashes may occasionally occur.
The most serious adverse reaction to potassium supplementation is hyperkalemia, yet is rare in subjects with normal kidney function see Toxicity. Individuals with abnormal kidney function and those on potassium-sparing medications see Drug interactions should be monitored closely to prevent hyperkalemia 50, Table 3 lists the classes of medications known to increase the risk of hyperkalemia elevated serum potassium in patients who also use potassium supplements 50, 51 Several classes of medications are known to induce hypokalemia low serum potassium; Table 4 ; In the absence of treatment, hypokalemia can have serious complications and even be fatal see Deficiency.
Various mechanisms explain how certain medications can lead to potassium depletion. For example, both loop and thiazide diuretics increase the urinary excretion of potassium. Corticoids cause sodium retention that leads to a compensatory increase in urinary potassium excretion.
: Potassium and metabolism| Recommended | Medicine —, Searches of PubMed, Poassium Cochrane Database metaholism Systematic Extract recipe data, and the National Guideline Lentils for energy were completed using the key terms Lentils for energy PPotassium hyperkalemia. Campbell JM, Potaszium TK, Karam JH, Forsham PH: Jejunoileal bypass as a treatment of morbid obesity. Electrolyte disorders in community subjects: prevalence and risk factors. Ma Y, He FJ, Sun Q, Yuan C, Kieneker LM, Curhan GC, MacGregor GA, Bakker SJ, Campbell NR, Wang M, Rimm EB. Weiner ID, Wingo CS. PubMed CAS Google Scholar Sugarman A, Kahn T: Calcium channel blockers enhance extrarenal potassium disposal in the rat. |
| Disorders of Potassium Metabolism | DAMA —, White RH, Schambelan M: Hypertension, hyperreninemia, and secondary hyperaldosteronism in systemic necrotizing vasculitis. Ruby ST, Burch A, White WB: Unilateral renal artery stenosis seen initially as severe and symptomatic hypokalemia. Arch Surg —, Edwards CRW, Walker BR, Benediktsson R, Seckl JR: Congenital and acquired syndromes of apparent mineralocorticoid excess. J Steroid Biochem Mol Biol 1—5, Biglieri EG, Kater CE: Mineralocorticoids in congenital adrenal hyperplasia. J Steroid Biochem Mol Biol —, Mantero F, Boscaro M: Glucocorticoid-dependent hypertension. Stewart PM, Come JET, Shackleton CHL, Edwards CRW: Syndrome of apparent mineralocorticoid excess. Clore J, Schoolwerth A, Watlington CO: When is cortisol a mineralocorticoid? Stewart PM, Wallace AM, Valentine R, Burt D, Shackleton CHL, Edwards CRW: Mineralocorticoid activity of liquorice: beta-hydroxysteroid dehydrogenase deficiency comes of age. Farese RV, Biglieri EG, Shackleton CHL, Irony I, Gomez-Fontes R: Licorice-induced hypermineralocorticoidism. Stewart PM, Wallace AM, Atherden SM, Shearing CH, Edwards CRW: Mineralocorticoid activity of carbenoxolone: contrasting effects of carbenoxolone and liquorice on - hydroxysteroid dehydrogenase activity in man. Clin Sci Atchley DW, Loeb RF, Richards DW, Benedict EM, —54, Driscoll ME: On diabetic acidosis: a detailed study of electro-. Nielsen I, Pedersen RS: Life-threatening hypokalaemia lyte balances following the withdrawal and reestablishment caused by liquorice ingestion. Lancet , of insulin therapy. Young WF, Klee GG: Primary aldosteronism. Diagnostic Brodsky WA, Rapoport S, West CD: The mechanism of evaluation. Endocrinol Metab Clin North Am —, glycosuric diuresis in diabetic man. J Clin Invest — Bravo EL: Primary aldosteronism. Urol Clin North Am Adrogué HJ, Lederer ED, Suki WN, Eknoyan G: Determi- —, nants of plasma potassium levels in diabetic ketoacidosis. Biglieri EG: Spectrum of mineralocorticoid hypertension. Hypertension —, Fulop M: Hyperkalemia in diabetic ketoacidosis. Am J Med. Bartter FC, Pronove P, Gill JR Jr, MacCardle RC: Sci —, Hyperplasia of the juxtaglomerular complex with Semin Nephrol —, Shils ME: Experimental human magnesium depletion. Ann Rev Med —, cine —85, Shils ME: Experimental production of magnesium deficiency. in man. Ann NY Acad Sci —, Kidney Int —93, Dunn MJ, Walser M: Magnesium depletion in normal man. Fichman MP, Telfor N, Zia P, Speckart P, Golub M, Rude R: Metabolism —, Evans RA, Carter JN, George CRP, Walls RS, Newland RC, drome. Verbeckmoes R, van Damme B, Clement J, Amery A, losing kidney. renomedullary cells. Successful treatment with indo- Whang R, Flink EB, Dyckner T, Wester PO, Aikawa JK, methacin. Ryan MP: Magnesium depletion as a cause of refractory. Gill JR Jr, Frölich JC, Bowden RE, Taylor AA, Keiser HR, potassium repletion. A Rodriguez M, Solanki DL, Whang R: Refractory potassium disorder characterized by high urinary prostaglandins and a repletion due to cisplatin-induced magnesium depletion. dependence of hyperreninemia on prostaglandin synthesis. Am J Med —51, Holmes AM, Hesling CM, Wilson TM: Drug-induced sec-. Gitelman HJ: Hypokalemia, hypomagnesemia, and alkalosis: ondary hyperaldosteronism in patients with pulmonary tu- A rose is a rose—or is it? J Pediatr —80, Q J Med —, Gill JR Jr, Bell NH, Bartter FC: Impaired conservation of Bar RS, Wilson HE, Mazzaferri EL: Hypomagnesemic sodium and potassium in renal tubular acidosis and its correc hypocalcemia secondary to renal magnesium wasting. A pos- tion by buffer anions. sible consequence of high-dose gentamicin therapy. Ann In-. Gennari FJ, Cohen JJ: Renal tubular acidosis. Annu Rev Med tern Med —, Gearhart MO, Sorg TB: Foscarnet-induced severe hypo-. Sebastian A, Hulter HN, Kurtz I, Maher T, Schambelan M: magnesemia and other electrolyte disorders. Ann Disorders of distal nephron function. Am J Med —, Pharmacother —, Barton CH, Pahl M, Vaziri ND, Cesario T: Renal magnesium. Sebastian A, McSherry E, Morris RC Jr: Renal potassium wasting associated with amphotericin B therapy. Am J Med wasting in renal tubular acidosis RTA. Its occurrence in —, types 1 and 2 RTA despite sustained correction of systemic Burgess JL, Birchall R: Nephrotoxicity of amphotericin B, acidosis. with emphasis on changes in tubular function. Wrong OM, Feest TG, Maclver AG: Immune-related —84, potassium-losing interstitial nephritis: a comparison with Mir MA, Brabin B, Tang OT, Leyland MJ, Delamore IW:. distal renal tubular acidosis. Q J Med —, Hypokalaemia in acute myeloid leukaemia. Ann Intern Med. Caruana RJ, Buckalew VM: The syndrome of distal type I Fisher JR: Hypokalemia in leukemia. Ann Intern Med , renal tubular acidosis. Medicine 84—99, Lightwood R, Payne WW, Black JA: Infantile renal acidosis. Lantz B, Carmark B, Reizenstein P: Electrolytes and whole. Pediatrics —, body potassium in acute leukemia. Acta Med Scand Brenes LG, Brenes JN, Hernandez MM: Familial proximal 50, renal tubular acidosis. Perry MC, Bauer JH, Farhangi M: Hypokalemia in acute. Sebastian A, McSherry E, Morris RC Jr: On the mechanism myelogenous leukemia. of potassium wasting in renal tubular acidosis associated with Sterns RH, Cox M, Feig PU, Singer I: Internal potassium the Fanconi syndrome type 2 RTA. J Clin Invest balance and the control of the plasma potassium concentra- , Harrington JT, Cohen JJ. Metabolic acidosis. In: JJ Cohen, Lawson DH: Adverse reactions to potassium chloride. Q J JP Kassirer with collaboration of FJ Gennari, JT Med —, Harrington, NE Madias , Acid—Base. Little, Brown, Boston, Ponce SP, Jennings AE, Madias NE, Harrington JT: Drugpp —, indued hyperkalemia. Rimmer JM, Horn JF, Gennari FJ: Hyperkalemia as a complication of drug therapy. Hultgren HN, Swenson R, Wettach G: Cardiac arrest due to oral potassium administration. McMahon FG, Ryan JR, Akdamar K, Ertan A: Effect of potassium chloride supplements on upper gastrointestinal mucosa. Clin Pharmacol Ther —, Alsop WR, Moore JG, Rollins DE, Tolman KE: The effects of five potassium chloride preparations on the upper gastrointestinal mucosa in healthy subjects receiving glycopyrrolate. J Clin Pharmacol —, Strom BL, Carson JL, Schinnar R, Sim E, Maislin G, Soper K, Morse L: Upper gastrointestinal tract bleeding from oral potassium chloride. Schwartz AB, Swartz CD: Dosage of potassium chloride elixir to correct thiazide-induced hypokalemia. Wan HH, Lye MDW. Moduretic-induced metabolic acidosis and hyperkalaemia. Cohen AB: Hyperkalemic effects of triamterene. Paice B, Gray JMB, McBride D, Donnelly T, Lawson DH: Hyperkalaemia in patients in hospital. Br Med J , Mather A, Mackie NR: Effects of hemolysis on serum electrolyte values. Clin Chem 6: —, Bronson WR, DeVita VT, Carbone PP, Cotlove E: Pseudohyperkalemia due to release of potassium from white blood cells during clotting. Bellevue R, Dosik H, Spergel G, Gussoff BD: Pseudohyperkalemia and extreme leukocytosis. J Lab Clin Med —, Stewart GW, Corrall RJM, Fyffe JA, Stockdill G, Strong JA: Familial pseudohyperkalaemia: a new syndrome. Graber M, Subramani K, Corish D, Schwab A: Thrombocytosis elevates serum potassium. Am J Kidney Dis —, Lum G, Gambino SR: A comparison of serum versus heparinized plasma for routine chemistry tests. Am J Clin Pathol —, Ladenson JH, Tsai LB, Michael JM, Kessler G, Joist JH: Serum versus heparinized plasma for eighteen common chemistry tests. Hartmann RC, Auditore JV, Jackson DP: Studies on thrombocytosis. Hyperkalemia due to release of potassium from platelets during coagulation. Kerr DJ, McAlpine LG, Dagg JH: Pseudohyperkalaemia. Don BR, Sebastian A, Cheitlin M, Christiansen M, Schambelan M: Pseudohyperkalemia caused by fist clenching during phlebotomy. Finch CA, Sawyer CG, Flynn JM: Clinical syndrome of potassium intoxication. Am J Med 1: —, Davis JO, Urquhart J, Higgins JT Jr: The effects of alterations of plasma sodium and potassium concentration on aldosterone secretion. Fredlund P, Saltman S, Kondo T, Douglas J, Catt KJ: Aldosterone production by isolated glomerulosa cells: modulation of sensitivity to angiotensin II and ACTH by extracellular potassium concentration. Miller PD, Waterhouse C, Owens R, Cohen E: The effect of potassium loading on sodium excretion and plasma renin activity in Addisonian man. van Ypersele de Strihou C: Potassium homeostasis in renal failure. Gonick HC, Kleeman CR, Rubin ME, Maxwell MH: Functional impairment in chronic renal disease III. Studies of potassium excretion. Perez GO, Pelleya R, Oster JR, Kem DC, Vaamonde CA: Blunted kaliuresis after an acute potassium load in patients with chronic renal failure. Kahn T, Kaji DM, Nicolis G, Krakoff LR, Stein RM: Factors related to potassium transport in chronic stable renal disease in man. Clin Sci Mol Med —, Bergström J, Alvestrand A, Fürst P, Hultman E, WidstamAttorps U: Muscle intracellular electrolytes in patients with chronic uremia. Kidney Int 24 Suppl 16 : S — S, Boddy K, King PC, Lindsay RM, Briggs JD, Winchester JF, Kennedy AC: Total body potassium in non-dialyzed and dialyzed patients with chronic renal failure. Br Med J 1: —, Widmer B, Gerhardt RE, Harrington JT, Cohen JJ: Serum electrolyte and acid—base composition. The influence of graded degrees of chronic renal failure. Restuccio A: Fatal hyperkalemia from a salt substitute. Sopko JA, Freeman RM: Salt substitutes as a source of potassium. Luzi L, Barrett EJ, Groop LC, Ferrannini E, DeFronzo RA: Metabolic effects of low-dose insulin therapy on glucose metabolism in diabetic ketoacidosis. Diabetes —, DeFronzo RA: Obesity is associated with impaired insulin-mediated potassium uptake. Cohen P, Barzilai N, Lerman A, Hard H, Szylman P, Karnieli E: Insulin effects on glucose and potassium metabolism in vivo: evidence for selective insulin resistance in humans. DeFronzo RA: Hyperkalemia and hyporeninemic hypoaldosteronism. Sunderlin FS, Anderson GH, Streeten DHP, Blumenthal SA: The renin—angiotensin—aldosterone system in diabetic patients with hyperkalemia. Conte G, Dal Canton A, Imperatore P, DeNicola L, Gigliotti G, Pisanti N, Memoli B, Furiano G, Esposito C, Andreucci VE: Acute increase in plasma osmolality as a cause of hyperkalemia in patients with renal failure. Goldfarb S, Cox M, Singer I, Goldberg M: Acute hyperkalemia induced by hyperglycemia: hormonal mechanisms. Perez GO, Lespier L, Knowles R, Oster JR, Vaamonde CA: Potassium homeostasis in chronic diabetes mellitus. Perez GO, Lespier L, Jacobi J, Oster JR, Katz FH, Vaamonde C, Fishman LM: Hyporeninemia and hypoaldosteronism in diabetes mellitus. Arrizabalaga P, Montoliu J, Martinez-Vea A, Andreu L, Lopez-Pedret J, Revert L: Increase in serum potassium caused by beta-2 adrenergic blockade in terminal renal failure: absence of mediation by insulin or aldosterone. Proc Eur Dial Transplant Assoc —, Arthur S, Greenberg A: Hyperkalemia associated with intravenous labetabol therapy for acute hypertension in renal transplant recipients. Clin Nephrol —, Fletcher GF, Fletcher BJ, Sweeney ME: Effects of exercise testing, training and beta blockade on serum potassium in normal subjects. Am J Cardiol —, Castellino P, Bia MJ, DeFronzo RA: Adrenergic modulation of potassium metabolism in uremia. Ericsson F, Carlmark B, Jogestrand T, Sundqvist K: Effect of digoxin upon intracellular potassium in man. Scand J Clin Lab Invest —, Bismuth C,. Gaultier M, Conso F, Efthymiou ML: Hyperkalemia in acute digitalis poisoning: prognostic significance and therapeutic implications. Clin Toxicol 6: —, Smith TW, Butler VP Jr, Haber E, Fozzard H, Marcus FI, Bremner WF, Schulman IC, Phillips A: Treatment of life-threatening digitalis intoxication with digoxin-specific Fab antibody fragments. Reza MJ, Kovick RB, Shine KI, Pearce ML: Massive intravenous digoxin overdosage. Papadakis MA, Wexman MP, Fraser C, Sedlacek SM: Hyperkalemia complicating digoxin toxicity in a patient with renal failure. Am J Kidney Dis 5: 64—66, Evers W, Racz GB, Dobkin AB: A study of plasma potassium and electrocardiographic changes after a single dose of succinylcholine. Can Anesth Soc J —, Weintraub HD, Heisterkamp DV, Cooperman LH: Changes in plasma potassium concentration after depolarizing blockers in anaesthetized man. Br J Anaesth —, Cooperman L: Succinylcholine-induced hyperkalemia in neuromuscular disease. Brooke MM, Donovan WH, Stolov WC: Paraplegia: succinylcholine-induced hyperkalemia and cardiac arrest. Arch Phys Med Rehab —, Greenawalt JW 3rd: Succinylcholine-induced hyperkalemia 8 weeks after a brief paraplegic episode. Dickerman HW, Walker WG: Effect of cationic amino acid infusion on potassium metabolism in vivo. Levinsky NG, Tyson I, Miller RB, Reiman AS: The relation between amino acids and potassium in isolated rat muscle. Hertz P, Richardson JA: Arginine-induced hyperkalemia in renal failure patients. Bushinsky DA, Gennari FJ: Life-threatening hyperkalemia induced by arginine. McIvor M, Baltazar RF, Beltran J, Mower MM, Wenk R, Lustgarten J, Salomon J: Hyperkalemia and cardiac arrest from fluoride exposure during hemodialysis. Gabow PA, Kaehny WD, Kelleher SP: The spectrum of rhabdomyolysis. Bluemle LW Jr, Webster GD, Elkinton JR: Acute tubular necrosis: analysis of one hundred cases with respect to mortality, complications and treatment with and without dialysis. Grossman RA, Hamilton RW, Morse BM, Penn AS, Goldberg M: Nontraumatic rhabdomyolysis and acute renal failure. Gamstorp I, Hauge M, Helweg-Larsen HF, Mjönes H, Sagild U: Adynamica episodica hereditaria. Ptacek LJ, Johnson KJ, Griggs RC: Genetics and physiology of the myotonic muscle disorders. Ptacek LJ, George AL Jr, Griggs RC, Tawil R, Kallen RG, Barchi RL, Robertson M, Leppert MF: Identification of a mutation in the gene causing hyperkalemic periodic paralysis. Cell —, Fontaine B, Khurana TS, Hoffman EP, Bruns GAP, Haines JL, Trofatter JA, Hanson MP, Rich J, McFarlane H, Yasek DM, Romano D, Gusella JF, Brown RH Jr: Hyperkalemic periodic paralysis and the adult muscle sodium channel a-subunit gene. Cannon SC, Brown RH Jr, Corey DP: A sodium channel defect in hyperkalemic periodic paralysis: potassium-induced failure of inactivation. Neuron 6: —, Streeten DHP, Dalakos TG, Fellerman H: Studies on hyperkalemic periodic paralysis. Evidence of changes in plasma Na and Cl and induction of paralysis by adrenal glucocorticoids. Wang P, Clausen T: Treatment of attacks in hyperkalaemic familial periodic paralysis by inhalation of salbutamol. Lancet 1: —, Martin RS, Panese S. Virginillo M, Gimenez M, Litardo M, Arrizurieta E, Hayslett JP: Increased secretion of potassium in the rectum of humans with chronic renal failure. Am J Kidney Dis 8: —, Hou S, McElroy PA, Nootens J, Beach M: Safety and efficacy of low-potassium dialysate. Gennari FJ, Rimmer JM: Disturbances in fluid, electrolyte, and acid-base balance. Part 2. Dialysis patients. In: SG Massry, RJ Glassock, eds, Textbook of Nephrology , 3rd ed. Williams and Wilkins, Baltimore, pp —, Greenblatt DJ, Koch-Weser J: Adverse reactions to spironolactone. DAMA 40—43, Walker BR, Capuzzi DM, Alexander F, Familiar RG, Hoppe RC: Hyperkalemia after triamterene in diabetic patients. Feinfeld DA, Carvounis CP: Fatal hyperkalemia and hyperchloremic acidosis. DAMA , McNay JL, Oran E: Possible predisposition of diabetic patients to hyperkalemia following administration of potassium-retaining diuretic, amiloride MK Metabolism 58—70, Atlas SA, Case DB, Sealey JE, Laragh JH, McKinstry DN: Interruption of the renin-angiotensin system in hypertensive patients by captopril induces sustained reduction in aldosterone secretion, potassium retention and natriuresis. Hypertension 1: —, Textor SC, Bravo EL, Fouad FM, Tarazi RC: Hyperkalemia in azotemic patients during angiotensin-converting enzyme inhibition and aldosterone reduction with captopril. Bauer JH: Role of angiotensin converting enzyme inhibitors in essential and renal hypertension. Am J Med 77 Suppl 2A : 43—51, Zachariah PK, Bonnet G, Chysant SG, DeBackser G, Goldstein R, Herrera J, Lindner A, Materson BJ, Maxwell MH, McMahon FG, Merrill RH, Paton RR, Rapp AD, Roginsky MS, Seedat YK, Sime F, Vaicaitis JS, Weinberg MS, Zusman RM: Evaluation of antihypertensive efficacy of lisinopril compared to metaprolol in moderate to severe hypertension. J Cardiovasc Pharmacol 9 Suppl 3 : S53 - S58, Donohoe JF, Laher M, Doyle GD, Cooper WD: Lisinopril in hypertension associated with renal impairment. J Cardiovasc Pharmacol 9 Suppl 3 : S66 - S68, deJong PE, Apperloo AJ, Heeg JE, deZeeuw D: Lisinopril in hypertensive patients with renal function impairment. Nephron 55 Suppl 1 : 43—48, Doman K, Perlmutter JA, Muhammedi M, Puschett JB: Life-threatening hyperkalemia associated with captopril administration. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD: The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. Feig PU, Rutan GH: Angiotensin converting enzyme inhibitors: The end of end-stage renal disease? Praga M, Hernandez E, Montoyo C, Andrés A, Ruilope LM, Rodicio JL: Long-term beneficial effects of angiotensinconverting enzyme inhibition in patients with nephrotic proteinuria. Captopril Multicenter Research Group. A placebo-controlled trial of captopril in refractory chronic congestive heart failure. J Am Coll Cardiol 2: —, Tan SY, Shapiro R, Franco R, Stockard H, Mulrow PJ: Indomethacin-induced prostaglandin inhibition with hyperkalemia. Clive DM, Stoff JS: Renal syndromes associated with nonsteroidal anti-inflammatory drugs. Whelton A, Hamilton CW: Nonsteroidal anti-inflammatory drugs: effects on kidney function. J Clin Pharmacol , Rotenberg FA, Giannini VS: Hyperkalemia associated with ketorolac. Ann Pharmacother —, Wilson ID, Goetz FC: Selective hypoaldosteronism after prolonged heparin administration. Conn JW, Rovner DR, Cohen EL, Anderson JE Jr: Inhibition by heparinoid of aldosterone biosynthesis in man. Busch EH, Ventura HO, Lavie CJ: Heparin-induced hyperkalemia. Aull L, Chao H, Coy K: Heparin-induced hyperkalemia. DICP Ann Pharmacother —, Edes TE, Sunderrajan EV: Heparin-induced hyperkalemia. Adu D, Turney J, Michael J, McMaster P: Hyperkalaemia in cyclosporin-treated renal allograft recipients. Lancet 2: , Bantle JP, Nath KA, Sutherland DER, Najarian JS, Ferris TF: Effects of cyclosporine on the renin-angiotensinaldosterone system and potassium excretion in renal transplant recipients. Kamel KS, Ethier JH, Quaggin S, Levin A, Albert S, Carlisle EJF, Halperin ML: Studies to determine the basis for hyperkalemia in recipients of a renal transplant who are treated with cyclosporine. J Am Soc Nephrol 2: —, Bantle JP, Boudreau RJ, Ferris TF: Suppression of plasma renin activity by cyclosporine. Am J Med 59—64, Velazquez H, Perazella MA, Wright FS, Ellison DH: Renal mechanism of trimethoprim-induced hyperkalemia. Lachaal M, Venuto RC: Nephrotoxicity and hyperkalemia in patients with acquired immunodeficiency syndrome treated with pentamidine. Briceland LL, Bailie GR: Pentamidine-associated nephrotoxicity and hyperkalemia in patients with AIDS. DICP —, A report of cases. Acta Endocrinol —, Lancet 1: 11—14, Yamamoto T, Fukuyama J, Hasegawa K, Sugiura M: Isolated corticotropin deficiency in adults. Arch Intern Med , Schambelan M, Sebastian A, Biglieri EG: Prevalence, pathogenesis, and functional significance of aldosterone deficiency in hyperkalemic patients with chronic renal insufficiency. Kidney Int 89—, Nadler JL, Lee FO, Hsueh W, Horton R: Evidence of prostacyclin deficiency in the syndrome of hyporeninemic hypoaldosteronism. Ulick S, Eberlin WR, Bliffeld AR, Chu MD, Bongiovanni AM: Evidence for an aldosterone biosynthetic defect in congenital adrenal hyperplasia. Hamilton W, McCandless AE, Ireland JT, Gray CE: Hypoaldosteronism in three sibs due to dehydrogenase deficiency. Veldhuis JD, Kulin HE, Santen RJ, Wilson TE, Melby JC: Inborn error in the terminal step of aldosterone biosynthesis. Braithwaite SS, Barbato AL, Emanuele MA: Acquired partial corticosterone methyl oxidase type II defect in diabetes mellitus. Diabetes Care —, Oberfield SE, Levine LS, Carey RM, Bejar R, New MI: Pseudohypoaldosteronism: multiple target organ unresponsiveness to mineralocorticoid hormones. Armanini D, Kuhnle U, Strasser T, Dorr H, Butenandt I, Weber PC, Stockigt JR, Pearce P, Funder JW: Aldosteronereceptor deficiency in pseudohypoaldosteronism. Armanini D, Wehling M, DaDalt L, Zennaro M, Scali U, Keller U, Pratesi C, Mantero F, Kuhnle U: Pseudohypoaldosteronism and mineralocorticoid receptor abnormalities. Brautbar N, Levi J, Rosler A, Leitesdorf E, Djaldeti M, Epstein M, Kleeman CR: Familial hyperkalemia, hypertension and hyporeninemia with normal aldosterone levels. Schambelan M, Sebastian A, Rector FC Jr: Mineralocorticoid-resistant renal hyperkalemia without salt wasting type II pseudohypoaldosteronism : role of increased renal chloride reabsorption. Take C, Ikeda K, Kurasawa T, Kurokawa K: Increased chloride reabsorption as an inherited renal tubular defect in familial type II pseudohypoaldosteronism. DeFronzo RA, Cooke R, Goldberg M, Cox M, Myers AR, Agus ZS: Impaired renal tubular potassium secretion in systemic lupus erythematosus. Battle D, Itsarayoungyuen K, Arruda JAL, Kurtzman NA: Hyperkalemic hyperchloremic metabolic acidosis in sickle cell hemoglobinopathies. Batlle DC: Segmental characterization of defects in collecting tubule acidification. Battle DC, Arruda JAL, Kurtzman NA: Hyperkalemic distal renal tubular acidosis associated with obstructive uropathy. Cogan MG, Arieff AI: Sodium wasting, acidosis and hyperkalemia induced by methicillin interstitial nephritis. Chamberlain MJ: Emergency treatment of hyperkalaemia. Garcia-Palmieri MR: Reversal of hyperkalemic cardiotoxicity with hypertonic saline. Ballantyne F III, Davis LD, Reynolds EW Jr: Cellular basis for reversal of hyperkalemic electrocardiographic changes by sodium. Blumberg A, Weidmann P, Shaw S, Gnädinger M: Effect of various therapeutic approaches on plasma potassium and major regulatory factors in terminal renal failure. Alton M, Dunlay R, Copkney C: Nebulized albuterol for acute hyperkalemia in patients on hemodialysis. Montoliu J, Lens XM, Revert L: Potassium-lowering effect of albuterol for hyperkalemia in renal failure. Blumberg A, Weidmann P, Ferrari P: Effect of prolonged bicarbonate administration on plasma potassium in terminal renal failure. Fraley DS, Adler S: Correction of hyperkalemia by bicarbonate despite constant blood pH. Flinn RB, Merrill JP, Welzant WR: Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol. Greenman L, Peters JH, Mateer FM, Danowski TS: Probable clinical utility of cation exchange resins. Scherr L, Ogden DA, Mead AW, Spritz N, Rubin AL: Management of hyperkalemia with a cation-exchange resin. Kramer P, Levitan R: Effect of 9-a-fluorohydrocortisone on the ileal excreta of ileostomized subjects. Gastroenterology —, Clarke AM, Hill GL, MacBeth WAAG: Intestinal adaptation to salt depletion in a patient with an ileostomy. Evans BM, Hughes-Jones NC, Milne MD, Yellowlees H: Ion-exchange resins in treatment of anuria. Lancet 2: 79 , Emmett M, Hootkins R, Santa Ana CA, Porter JL, Fordtran JS: Effect of three laxatives and a cation exchange resin on fecal sodium and potassium excretion. Lillemoe KD, Romolo JL, Hamilton SR, Pennington LR, Burdick JF, Williams GM: Intestinal necrosis due to sodium polystyrene Kayexalate in sorbitol enemas: clinical and experimental support for the hypothesis. Surgery —, Wootton FT, Rhodes DF, Lee WM, Fitts CT: Colonic necrosis with kayexelate-sorbitol enemas after renal transplantation. Gerstman BB, Kirkman R, Platt R: Intestinal necrosis associated with postoperative orally administered sodium polystyrene sulfate in sorbitol. Berlyne GM, Janabi K, Shaw AB: Dangers of resonium A in the treatment of hyperkalaemia in renal failure. Alton M: Treatment and prevention of hyperkalemia in end-stage renal disease. Download references. Nephrology Unit, University of Vermont College of Medicine, , Burlington, VT, USA. John Gennari M. Professor of Medicine, Director. You can also search for this author in PubMed Google Scholar. Reprints and permissions. Gennari, F. Disorders of Potassium Metabolism. In: Suki, W. Springer, Boston, MA. Publisher Name : Springer, Boston, MA. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Skip to main content. Abstract The concentration of potassium in our cells is some 37 times higher than in the extracellular compartment. Keywords Renal Tubular Acidosis Metabolic Alkalosis Distal Nephron Aldosterone Secretion Periodic Paralysis These keywords were added by machine and not by the authors. Buying options Chapter EUR eBook EUR Softcover Book EUR Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions. Preview Unable to display preview. References Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, Mertz W, Smith JC: Sodium and potassium intake and balance in adults consuming self-selected diets. PubMed CAS Google Scholar Hiatt N, Davidson MB, Bonorris G: The effect of potassium chloride infusion on insulin secretion in vivo. CrossRef PubMed CAS Google Scholar Dluhy RG, Axelrod L, Williams GH: Serum immunoreactive insulin and growth hormone response to potassium infusion in normal man. PubMed CAS Google Scholar Santeusanio F, Faloona GR, Knochel JP, Unger RH: Evidence for a role of endogenous insulin and glucagon in the regulation of potassium homeostasis. Google Scholar Martinez R, Rietberg B, Skyler J, Oster JR, Perez GO: Effect of hyperkalemia on insulin secretion. Google Scholar Clausen T, Everts ME: Regulation of the Na, K-pump in skeletal muscle. CrossRef PubMed CAS Google Scholar Zierler K, Rogus EM: Rapid hyperpolarization of rat skeletal muscle induced by insulin. PubMed CAS Google Scholar Minaker KL, Rowe JW: Potassium homeostasis during hyperinsulinemia: Effect of insulin level, [3-blockade, and age. PubMed CAS Google Scholar Zierler KL: Effect of insulin on potassium efflux from rat muscle in the presence and absence of glucose. PubMed CAS Google Scholar DeFronzo RA, Sherwin RS, Dillingham M, Hendler R, Tamborlane WV, Felig P: Influence of basal insulin and glucagon secretion on potassium and sodium metabolism. CrossRef PubMed CAS Google Scholar Rowe JW, Tobin JD, Rosa RM, Andres R: Effect of experimental potassium deficiency on glucose and insulin metabolism. CrossRef PubMed CAS Google Scholar Landsberg L, Young JB: Fasting, feeding and regulation of the sympathetic nervous system. Google Scholar Rosa RM, Silva P, Young JB, Landsberg L, Brown RS, Rowe JW, Epstein FH: Adrenergic modulation of extrarenal potassium homeostasis. CrossRef PubMed CAS Google Scholar DeFronzo RA, Bia M, Birkhead G: Epinephrine and potassium disposal. CrossRef PubMed CAS Google Scholar Brown MJ, Brown DC, Murphy MB: Hypokalemia from betaz receptor stimulation by circulating epinephrine. CrossRef PubMed CAS Google Scholar Pedersen EB, Kornerup HJ: Relationship between plasma aldosterone concentration and plasma potassium in patients with essential hypertension during alprenolol treatment. CrossRef PubMed CAS Google Scholar Drayer JIM, Weber MA, Longworth DL, Laragh JH: The possible importance of aldosterone as well as renin in the long-term antihypertensive action of propranolol. CrossRef PubMed CAS Google Scholar McKenna TJ, Island DP, Nicholson WE, Liddle GW: The effects of potassium on early and late steps in aldosterone biosynthesis in cells of the zona glomerulosa. CrossRef PubMed CAS Google Scholar Gann DS, Delea CS, Gill JR Jr, Thomas JP, Bartter FC: Control of aldosterone secretion by change of body potassium in normal man. PubMed CAS Google Scholar Kassirer JP, Appleton FM, Chazan JA, Schwartz WB: Aldosterone in metabolic alkalosis. CrossRef PubMed CAS Google Scholar Pratt JH: Role of angiotensin II in potassium-mediated stimulation of aldosterone secretion in the dog. PubMed CAS Google Scholar Wang W, Schwab A, Giebisch G: Regulation of small conductance K. Google Scholar Himathongkam T, Dluhy RG, Williams GH: Potassiumaldosterone-renin interrelationships. CrossRef PubMed CAS Google Scholar Keith NM, Osterberg AE, Burchell HB: Some effects of potassium salts in man. CrossRef CAS Google Scholar Clive DM, Gurwitz JH, Rossetti RG: Potassium homeostasis with indomethacin therapy in normal subjects. PubMed CAS Google Scholar DeFronzo RA, Taufield PA, Black H, McPhedran P, Cooke CR: Impaired renal tubular potassium secretion in sickle cell diseasè. CrossRef PubMed CAS Google Scholar Brown RS: Extrarenal potassium homeostasis. CrossRef PubMed CAS Google Scholar Arriza JL, Weinberger C, Cerelli G, Glaser TM, Handelin BL, Housman DE, Evans RM: Cloning of human mineralocorticoid receptor complementary DNA: structural and func- tional kinship with the glucocorticoid receptor. CrossRef PubMed CAS Google Scholar Armanini D, Strasser T, Weber PC: Characterization of aldosterone binding sites in circulating human mononuclear leukocytes. PubMed CAS Google Scholar Meyer WJ, Nichols NR: Mineralocorticoid binding in cultured smooth muscle cells and fibroblasts from rat aorta. Google Scholar Clark BA, Brown RS, Epstein FH: Effect of atrial natriuretic peptide on potassium-stimulated aldosterone secretion: potential relevance to hypoaldosteronism in man. CrossRef PubMed CAS Google Scholar Nicolis GL, Kahn T, Sanchez A, Gabrilove L: Glucose-induced hyperkalemia in diabetic subjects. CrossRef PubMed CAS Google Scholar Williams ME, Rosa RM, Silva P, Brown RS, Epstein FH: Impairment of extrarenal potassium disposal by a-adrenergic stimulation. CrossRef PubMed CAS Google Scholar Todd EP, Vick RL: Kalemotropic effect of epinephrine: analysis with adrenergic agents and antagonists. PubMed CAS Google Scholar Williams ME, Gervino EV, Rosa RM, Landsberg L, Young JB, Silva P, Epstein FH: Catecholamine modulation of rapid potassium shifts during exercise. CrossRef PubMed CAS Google Scholar Kjeldsen K, NOrgaard A, Gatzsche CO, Thomassen A, Clausen T: Effect of thyroid function on number of Na-K pumps in human skeletal muscle. CrossRef PubMed CAS Google Scholar Sugarman A, Kahn T: Parathyroid hormone impairs extrarenal potassium tolerance in the rat. PubMed CAS Google Scholar Sugarman A, Kahn T: Calcium channel blockers enhance extrarenal potassium disposal in the rat. PubMed CAS Google Scholar D¢rup I, Skajaa K, Clausen T, Kjeldsen K: Reduced concentrations of potassium, magnesium, and sodium-potassium pumps in human skeletal muscle during diuretic treatment. CrossRef Google Scholar Kjeldsen K, Nargaard A, Clausen T: Effect of K-depletion on 3H-ouabain binding and Na-K-contents in mammalian skeletal muscle. CrossRef PubMed CAS Google Scholar Adrogué HG, Madias NE: Changes in plasma potassium concentration during acute acid-base disturbances. CrossRef PubMed Google Scholar Burnell JM, Villamil MF, Uyeno BT, Scribner BH: The effect in humans of extracellular pH change on the relationship between serum potassium concentration and intracellular potassium. CrossRef PubMed CAS Google Scholar Oster JR, Perez GO, Castro A, Vaamonde CA: Plasma potassium response to acute metabolic acidosis induced by mineral and nonmineral acids. CAS Google Scholar Orringer CE, Eustace JC, Wunsch CD, Gardner LB: Natural history of lactic acidosis after grand-mal seizures: a model for the study of an anion-gap acidosis not associated with hyperkalemia. CrossRef PubMed CAS Google Scholar Fulop M: Serum potassium in lactic acidosis and ketoacidosis. CrossRef PubMed CAS Google Scholar Adrogué HG, Chap Z, Ishida T, Field JB: Role of the endocrine pancreas in the kalemic response to acute metabolic acidosis in conscious dogs. CrossRef PubMed Google Scholar Gennari FJ, Cohen Ji: Role of the kidney in potassium homeostasis: lessons from acid-base disturbances. CrossRef PubMed CAS Google Scholar Krapf R, Cadoff P, Wagdi P, Stäubli M, Hulter HN: The plasma potassium response to acute respiratory alkalosis. CrossRef PubMed CAS Google Scholar Wright FS, Giebisch G: Renal potassium transport: Contributions of individual nephron segments and populations. PubMed CAS Google Scholar Wright FS, Giebisch G: Regulation of potassium excretion. Google Scholar Field MJ, Giebisch G: Hormonal control of renal potassium excretion. CrossRef PubMed CAS Google Scholar Seldin DW, Welt LG, Cort JH: The role of sodium salts and adrenal steroids in the production of hypokalemic alkalosis. PubMed CAS Google Scholar Good DW, Wright FS: Luminal influences on potassium secretion: Sodium concentration and fluid flow rate. PubMed CAS Google Scholar Stokes JB: Potassium secretion by cortical collecting tubule: relation to sodium absorption, luminal sodium concentration, and transepithelial voltage. PubMed CAS Google Scholar Relman AS, Schwartz WB: The effect of DOCA on electrolyte balance in normal man and its relation to sodium chloride intake. PubMed CAS Google Scholar Schwartz WB, Jenson RL, Reiman AS: Acidification of the urine and increased ammonium excretion without change in acid-base equilibrium: sodium reabsorption as a stimulus to the acidifying process. CrossRef PubMed CAS Google Scholar Velazquez H, Wright FS, Good DW: Luminal influences on potassium secretion: chloride replacement with sulfate. PubMed CAS Google Scholar Velazquez H, Ellison DH, Wright FS: Chloride-dependent potassium secretion in early and late renal distal tubules. PubMed CAS Google Scholar Stanton BA, Giebisch G: Effects of pH on potassium transport by renal distal tubule. Google Scholar Stanton BA, Giebisch GH: Potassium transport by the renal distal tubule: effects of potassium loading. PubMed CAS Google Scholar Hayslett JP, Binder HJ: Mechanism of potassium adaptation. PubMed CAS Google Scholar Doucet A, Marsy S: Characterization of K-ATPase activity in distal nephron: stimulation by potassium depletion. PubMed CAS Google Scholar Wingo CS: Active proton secretion and potassium absorption in the rabbit outer medullary collecting duct. CrossRef PubMed CAS Google Scholar Hayes CP Jr, McLeod ME, Robinson RR: An extrarenal mechanism for the maintenance of potassium balance in severe chronic renal failure. PubMed Google Scholar Paice BJ, Paterson KR, Onyanga-Omara F, Donnelly T, Gray JMB, Lawson DH: Record linkage study of hypokalaemia in hospitalized patients. CrossRef PubMed CAS Google Scholar Lawson DH, Henry DA, Lowe JM, Gray JMB, Morgan HG: Severe hypokalemia in hospitalized patients. CrossRef PubMed CAS Google Scholar Adams PC, Woodhouse KW, Adela M, Parnham A: Exaggerated hypokalaemia in acute myeloid leukemia. CrossRef CAS Google Scholar Naparstek Y, Gutman A: Spurious hypokalemia in myeloproliferative disorders. CrossRef PubMed CAS Google Scholar Depner TA, Magee JA: Severe hypokalemia associated with pseudohypoxemia in acute nonlymphocytic leukemia. PubMed CAS Google Scholar Khuri RN, Agulian SK, Abdulnour-Nakhoul S, Nakhoul NL: Electrochemical potentials of potassium in skeletal muscle under different metabolic states. CrossRef PubMed CAS Google Scholar Surawicz B: Relationship between electrocardiogram and electrolytes. CrossRef PubMed CAS Google Scholar Fisch C: Relation of electrolyte disturbances to cardiac arrhythmias. CrossRef PubMed CAS Google Scholar Nordrehaug JE: Malignant arrhythmias in relation to serum potassium values in patients with an acute myocardial infarction. CAS Google Scholar Hulting J: In-hospital ventricular fibrillation and its relation to serum potassium. CAS Google Scholar Schulman M, Narins RG: Hypokalemia and cardiovascular disease. CrossRef PubMed CAS Google Scholar Duke M: Thiazide-induced hypokalemia. CAS Google Scholar Brunner HR, Baer L, Sealey JE, Ledingham JGG, Laragh JH: The influence of potassium administration and of potassium deprivation on plasma renin in normal and hypertensive subjects. CrossRef PubMed CAS Google Scholar Carliner NH, Schelling J-L, Russell RP, Okun R, Davis M: Thiazide-and phthalimidine-induced hyperglycemia in hypertensive patients. CAS Google Scholar Conn JW: Hypertension, the potassium ion and impaired carbohydrate tolerance. CrossRef PubMed CAS Google Scholar Schwartz WB, Relman AS: Effects of electrolyte disorders on renal structure and function. CrossRef PubMed CAS Google Scholar Manitius A, Levitin H, Beck D, Epstein FH: On the mechanism of impairment of renal concentrating ability in potassium deficiency. CrossRef PubMed CAS Google Scholar Krishna GG, Miller E, Kapoor S: Increased blood pressure during potassium depletion in normotensive men. CrossRef PubMed CAS Google Scholar Krishna GG: Effect of potassium intake on blood pressure. PubMed CAS Google Scholar Knochel JP: Neuromuscular manifestations of electrolyte disorders. CrossRef PubMed CAS Google Scholar Campion DS, Arias M, Carter NW: Rhabdomyolysis and myoglobinuria. CAS Google Scholar Christiensen KS: Hypokalemic periodic paralysis secondary to renal tubular acidosis. CrossRef Google Scholar Alvarez J, Low RB: Acute respiratory arrest due to hypokalemia. CrossRef PubMed CAS Google Scholar Morgan DB, Young RM: Acute transient hypokalaemia: new interpretation of a common event. CrossRef PubMed CAS Google Scholar Wadstein J, Skude G: Does hypokalaemia precede delirium tremens? CrossRef PubMed CAS Google Scholar Bremner P, Burgess C, Beasley R, Woodman K, Marshall S, Crane J, Pearce N: Nebulized fenoteral causes greater cardiovascular and hypokalaemic effects than equivalent bronchodilator doses of salbutamol in asthmatics. CrossRef PubMed CAS Google Scholar Burgess CD, Flatt A, Siebers R, Crane J, Beasley R, Purdie G: A comparison of the extent and duration of hypokalaemia following three nebulized Betaz adrenoceptor agonists. CrossRef CAS Google Scholar McCleave DJ, Phillips PJ, Vedig AE: Compartmental shift of potassium—a result of sympathomimetic overdose. CrossRef CAS Google Scholar Kearney TE, Manoguerra AS, Curtis GP, Ziegler MG: Theophylline toxicity and the beta-adrenergic system. CrossRef PubMed CAS Google Scholar Atuk NO, Blaydes MC, Westervelt FB Jr, Wood JE Jr: Effect of aminophylline on urinary excretion of epinephrine and norepinephrine in man. Google Scholar Zantvoort FA, Derkx FHM, Boomsma F, Roos PJ, Schalekamp MADH: Theophylline and serum electrolytes. CrossRef PubMed CAS Google Scholar Shannon M, Lovejoy FH Jr: Hypokalemia after theophylline intoxication: the effects of acute vs chronic poisoning. CrossRef PubMed CAS Google Scholar Passmore AP, Kondowe GB, Johnston GD: Caffeine and hypokalemia. CrossRef PubMed CAS Google Scholar Minella RA, Schulman DS: Fatal verapamil toxicity and hypokalemia. PubMed CAS Google Scholar Liu GZ, Lyle KC, Cao J: Experiences with gossypol as a male pill. PubMed CAS Google Scholar Tam S-C: Acute hypokalemic effect of gossypol. CrossRef PubMed CAS Google Scholar Ober KP: Thyrotoxic periodic paralysis in the United States. Google Scholar Oh VMS, Taylor EA, Yeo S-H, Lee K-O: Cation transport across lymphocyte plasma membranes in euthyroid and thyrotoxic men with and without hypokalaemic periodic paralysis. PubMed CAS Google Scholar Chan A, Shinde R, Chow CC, Cockram CS, Swaminathan R: In vivo and in vitro sodium pump activity in subjects with thyrotoxic periodic paralysis. CrossRef CAS Google Scholar Kjeldsen K, Nt rgaard A, G¢tzsche CO, Thomassen A, Clausen T: Effect of thyroid function on number of Na—K pumps in human skeletal muscle. CrossRef PubMed CAS Google Scholar Conway MJ, Seibel JA, Eaton RP: Thyrotoxicosis and peri- Google Scholar Yeung RTT, Tse TF: Thyrotoxic periodic paralysis. CrossRef PubMed CAS Google Scholar Johnsen T: Familial periodic paralysis with hypokalaemia. Google Scholar Kantola IM, Tarssanen LT: Familial hypokalaemic periodic paralysis in Finland. Google Scholar Corbett VA, Nuttall FQ: Familial hypokalemic periodic paralysis in blacks. CrossRef PubMed CAS Google Scholar Minaker KL, Meneilly GS, Flier JS, Rowe JW: Insulin- CrossRef PubMed CAS Google Scholar Stedwell RE, Allen KM, Binder LS. CrossRef PubMed CAS Google Scholar Baruma OJS, Bots GTAM, Went LN: Familial hypokalemic periodic paralysis. Google Scholar Links TP, Zwartz MJ, Wilmink JT, Molenaar WM, CrossRef PubMed Google Scholar Streeten DHP, Speller PJ, Fellerman H: Use of corticotropin-induced potassium changes in the diagnosis of both hypo-and hyperkalemic periodic paralysis. CrossRef Google Scholar Vroom FQ, Jarrell MA, Maren TH: Acetozolamide treatment of hypokalemic periodic paralysis. Google Scholar Jarrell MA, Greer M, Maren TH: The effect of acidosis in Google Scholar Johnson CH, Van Tassell VJ: Acute barium poisoning with respiratory failure and rhabdomyolysis. Google Scholar Shankle R, Keane JR: Acute paralysis from inhaled barium carbonate. Google Scholar Hesp R, Chanarin I, Tait CE: Potassium changes in megaloblastic anaemia. PubMed CAS Google Scholar Rao TLK, Mathru M, Salem MR, Adel AE: Serum potassium levels following transfusions of frozen erythrocytes. CAS Google Scholar Weinsier RL, Bacon J, Butterworth CE Jr: Central venous alimentation: a prospective study of the frequency of meta- CrossRef PubMed CAS Google Scholar Hernandez RE, Schambelan M, Cogan MG, Colman J, CrossRef PubMed CAS Google Scholar Squires RD, Huth EJ: Experimental potassium depletion in normal human subjects. Google Scholar Silva P, Spokes K: Sympathetic system in potassium homeostasis. PubMed CAS Google Scholar Drenick EJ, Bland W, Singer FR, Lederer M: Body Google Scholar Garrow JS: Total body-potassium in kwashiorkor and marasmus. CrossRef PubMed CAS Google Scholar Bonne OB, Bloch M, Berry EM: Adaptation to severe chronic hypokalemia in anorexia nervosa: a plea for conservative mananagement. CrossRef CAS Google Scholar Harris RT: Bulimarexia and related serious eating disorders with medical complications. CrossRef PubMed CAS Google Scholar Knochel JP, Dotin LN, Hamburger RJ: Pathophysiology of intense physical conditioning in a hot climate. CrossRef PubMed CAS Google Scholar Hart GR, Anderson RI, Crumpler CP, Shulkin A, Reed G, Knochel JP: Epidemic classical heat stroke: clinical characteristics and course of 28 patients. CrossRef PubMed CAS Google Scholar Foster ES, Hayslett JP, Binder HJ: Mechanism of active potassium absorption and secretion in the rat colon. PubMed CAS Google Scholar Fordtran JS: Speculations on the pathogenesis of diarrhea. PubMed CAS Google Scholar Reid AC, Draper IT: Flaccid quadriparesis due to salmonella enteritis. PubMed CAS Google Scholar daSilva OA, Amaral CFS, daSilveira JCB, López M, Pittella JEH: Hyperkalemic respiratory muscle paralysis following strongyloides stercoralis hyperinfection. CAS Google Scholar Orman RA, Lewis JB Jr: Flaccid quadriparesis associated with yersinia enterocolitis-induced hypokalemia. CrossRef PubMed CAS Google Scholar Lopez AP, Gorbach LS: Diarrhea in AIDS. PubMed CAS Google Scholar Guerra I, Kimmel PL: Hypokalemic adrenal crisis in a patient with AIDS. CrossRef PubMed CAS Google Scholar Schwartz WB, Reiman AS: Metabolic and renal studies in chronic potassium depletion resulting from overuse of laxatives. CrossRef PubMed CAS Google Scholar Basser LS: Purgatives and periodic paralysis. PubMed CAS Google Scholar Simodynes E: Preoperative shock secondary to severe hypokalemia and hypocalcemia from recreational enemas. PubMed Google Scholar Schrock LG, Polk HC Jr: Rectal villous adenoma producing hypokalemia. PubMed CAS Google Scholar Chisholm JC Jr: Zollinger—Ellison syndrome: intermittent diarrhea, relentless hypokalemia, and hypergastrinemia. Google Scholar Verner JV, Morrison AB: Endocrine pancreatic islet disease with diarrhea. CrossRef Google Scholar Cooke WT: Water and electrolyte upsets in the stratorrhea syndrome. CrossRef Google Scholar Slavin RE, Dias MA, Saral R: Cytosine arabinoside induced gastrointestinal toxic alterations in sequential chemotherapeutic protocols: a clinical-pathologic study of 33 patients. CrossRef PubMed CAS Google Scholar Murai K, Tsuruta K, Yamamura Y, Kuribayashi T, Kurihara T, Matsukura S: Hypokalemic myopathy associated with radiation enteropathy. CrossRef PubMed CAS Google Scholar Gonzalez JJ, Owens W, Ungaro PC, Werk EE Jr, Wentz PW: Clay ingestion: a rare cause of hypokalemia. CrossRef PubMed CAS Google Scholar Gennari FJ: Hypokalemia in metabolic alkalosis: a new look at an old controversy. Google Scholar Rimmer JM, Gennari FJ: Metabolic alkalosis. CrossRef Google Scholar Kassirer JP, Harrington JT: Diuretics and potassium metabolism: a reassessment of the need, effectiveness and safety of potassium therapy. CrossRef PubMed CAS Google Scholar Nader PC, Thompson JR, Alpern RJ: Complications of diuretic use. PubMed CAS Google Scholar Morgan DB, Davidson C: Hypokalaemia and diuretics: an analysis of publications. CrossRef PubMed CAS Google Scholar Licht JH, Haley RI, Pugh B, Lewis SB: Diuretic regimens in essential hypertension. CrossRef PubMed CAS Google Scholar Katz FH, Eckert RC, Gebott MD: Hypokalemia caused by surreptitious self-administration of diuretics. CrossRef PubMed CAS Google Scholar Kassirer JP, Schwartz WB: The response of normal man to selective depletion of hydrochloric acid. CrossRef PubMed CAS Google Scholar Kassirer JP, Berkman PM, Lawrenz DR, Schwartz WB: The critical role of chloride in the correction of hypokalemic alkalosis in man. CrossRef PubMed CAS Google Scholar Harrington JT, Kassirer JP: Metabolic alkalosis. CrossRef PubMed CAS Google Scholar Klastersky J, Vanderkelen B, Daneau D, Mathieu M: Carbenicillin and hypokalemia. CrossRef PubMed CAS Google Scholar Mohr JA, Clark RM, Waack TC, Whang R: Nafcillinassociated hypokalemia. CAS Google Scholar Gill MA, Dubé JE, Young WW: Hypokalemic, metabolic alkalosis induced by high-dose ampicillin sodium. CAS Google Scholar Conn JW, Knopf RF, Nesbit RM: Clinical characteristics of primary aldosteronism from an analysis of cases. CrossRef PubMed CAS Google Scholar Weinberger MH, Grim CE, Hollifield JW, Kem DC, Ganguly A, Kramer NJ, Yune HY, Wellman H, Donohue JP: Primary aldosteronism. Because many individuals in the population consume potassium in amounts that are well below the AI and because underconsumption of potassium is linked with adverse health effects, potassium has been recognized as a "nutrient of public health concern" in the Dietary Guidelines for Americans. In , the US Food and Drug Administration FDA required manufacturers to display potassium content of foods on the Nutrition Facts food label Some relatively good dietary sources of potassium are listed in the Table 2 , along with their potassium content in milligrams mg. For more information on the nutrient content of foods, search USDA's FoodData Central Multivitamin-mineral supplements in the US do not contain more than 99 mg of potassium per serving One milliequivalent mEq or one millimole mmol corresponds to about 39 mg of potassium. Higher doses of supplemental potassium are generally prescribed to prevent and treat potassium depletion and hypokalemia. The use of more potent potassium supplements in potassium deficiency requires close monitoring of serum potassium concentrations. Potassium is available in different supplemental forms, including potassium chloride, potassium citrate, potassium gluconate, potassium bicarbonate, potassium aspartate, and potassium orotate Because of the potential for serious side effects, one should seek medical advice before deciding to use a potassium supplement see Safety. Finally, many salt substitutes contain potassium chloride, and acesulfame potassium Ace-K is an FDA-approved general purpose sweetener. Abnormally elevated serum potassium concentrations are referred to as hyperkalemia. Hyperkalemia occurs when potassium intake exceeds the capacity of the kidneys to eliminate it. Acute or chronic kidney failure, the use of potassium-sparing diuretics , and insufficient aldosterone secretion hypoaldosteronism may result in the accumulation of potassium due to a decreased urinary potassium excretion. Hyperkalemia may also result from a shift of intracellular potassium into the circulation, which may occur with the rupture of red blood cells hemolysis or tissue damage e. Symptoms of hyperkalemia may include tingling of the hands and feet, muscular weakness, and temporary paralysis. The most serious complication of hyperkalemia is the development of an abnormal heart rhythm cardiac arrhythmia , which can lead to cardiac arrest See the section on Drug interactions for a discussion of the medications that increase the risk of hyperkalemia. Gastrointestinal symptoms are the most common side effects of potassium supplements , including nausea, vomiting, abdominal discomfort, and diarrhea. Intestinal ulceration has been reported after the use of enteric-coated potassium chloride tablets. Taking potassium with meals or taking a microencapsulated form of potassium may reduce gastrointestinal side effects Rashes may occasionally occur. The most serious adverse reaction to potassium supplementation is hyperkalemia, yet is rare in subjects with normal kidney function see Toxicity. Individuals with abnormal kidney function and those on potassium-sparing medications see Drug interactions should be monitored closely to prevent hyperkalemia 50, Table 3 lists the classes of medications known to increase the risk of hyperkalemia elevated serum potassium in patients who also use potassium supplements 50, 51 , Several classes of medications are known to induce hypokalemia low serum potassium; Table 4 ; In the absence of treatment, hypokalemia can have serious complications and even be fatal see Deficiency. Various mechanisms explain how certain medications can lead to potassium depletion. For example, both loop and thiazide diuretics increase the urinary excretion of potassium. Corticoids cause sodium retention that leads to a compensatory increase in urinary potassium excretion. Penicillins formulated as sodium salts also stimulate potassium excretion. Several medications, including aminoglycosides, anti-fungal agents amphotericin-B, fluconazole , and cisplatin, can damage the renal tubular epithelium and lead to severe potassium loss. Outdated tetracycline antibiotics have been linked to electrolyte disturbances. Penicillins : penicillin G sodium Pfizerpen , mezlocillin Mezlin , carbenicillin Geocillin , ticarcillin Ticar. Loop diuretics : bumetanide Bumex , ethacrynic acid Edecrin , furosemide Lasix , torsemide Demadex. Thiazide diuretics : Acetazolamide, thiazides, chlorthalidone Hygroton , indapamide Lozol , metolazone Zaroxolyn , chlorothiazide Diuril. fludrocortisone Florinef , hydrocortisone Cortef , cortisone Cortone , prednisone Deltasone. There is substantial evidence suggesting that a diet high in potassium-rich food and beverages may be associated with lower risks of stroke , hypertension , kidney stones , and possibly osteoporosis. However, currently there is insufficient evidence to establish a causal relationship between potassium intakes and the risk of these chronic conditions The revised AI values are 2. Fruit and vegetables are among the richest sources of dietary potassium, and a large body of evidence supports the association of increased fruit and vegetable intakes with reduced risk of cardiovascular disease see the article on Fruit and Vegetables. The Linus Pauling Institute recommends the consumption of a diet high in potassium-rich foods see Sources , especially fruit, vegetables, nuts , and dairy products to ensure adequate potassium intakes. A diet rich in fruit and vegetables that supplies 2. This recommendation does not apply to individuals who have been advised to limit potassium consumption by a health care professional see Safety. Originally written in by: Jane Higdon, Ph. Linus Pauling Institute Oregon State University. Updated in February by: Jane Higdon, Ph. Updated in December by: Victoria J. Drake, Ph. Updated in April by: Barbara Delage, Ph. Reviewed in April by Connie Weaver, Ph. Distinguished Professor and Department Head Department of Nutrition Science Purdue University. Bailey JL, Sands JM, Franch HA. Water, electrolytes, and acid — Base Metabolism In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Clausen T. J Gen Physiol. Larsen BR, Stoica A, MacAulay N. Front Physiol. Shattock MJ, Ottolia M, Bers DM, et al. J Physiol. Sheng H-W. Sodium, chloride and potassium. In: Stipanuk M, ed. Biochemical and Physiological Aspects of Human Nutrition. Philadelphia: W. Saunders Company; Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, D. The National Academies Press. Mumoli N, Cei M. Licorice-induced hypokalemia. Int J Cardiol. Walker BR, Edwards CR. Licorice-induced hypertension and syndromes of apparent mineralocorticoid excess. Endocrinol Metab Clin North Am. Food and Nutrition Board, National Academy of Medicine. Dietary Reference Intakes for Sodium and Potassium - uncorrected proofs. The National Academies of Sciences, Engineering, and Medicine. Newberry SJ, Chung M, Anderson CAM, et al. AHRQ Comparative Effectiveness Reviews. Sodium and potassium intake: effects on chronic disease outcomes and risks. Rockville MD : Agency for Healthcare Research and Quality US ; Potassium: Dietary Reference Intakes based on chronic disease. Weaver CM. Potassium and health. Adv Nutr. Young DB, Lin H, McCabe RD. Potassium's cardiovascular protective mechanisms. Am J Physiol. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. Jayedi A, Ghomashi F, Zargar MS, Shab-Bidar S. Dietary sodium, sodium-to-potassium ratio, and risk of stroke: A systematic review and nonlinear dose-response meta-analysis. Clin Nutr. Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. Vinceti M, Filippini T, Crippa A, de Sesmaisons A, Wise LA, Orsini N. Meta-analysis of potassium intake and the risk of stroke. J Am Heart Assoc. Trinchieri A, Zanetti G, Curro A, Lizzano R. Effect of potential renal acid load of foods on calcium metabolism of renal calcium stone formers. Eur Urol. Lemann J, Jr. Potassium causes calcium retention in healthy adults. J Nutr. Morris RC, Jr. Differing effects of supplemental KCl and KHCO3: pathophysiological and clinical implications. Semin Nephrol. Ferraro PM, Mandel EI, Curhan GC, Gambaro G, Taylor EN. Dietary protein and potassium, diet-dependent net acid load, and risk of incident kidney stones. Clin J Am Soc Nephrol. Suarez M, Youssef RF. Potassium citrate: treatment and prevention of recurrent calcium nephrolithiasis. J Clin Nephrol Res. Hayhoe RP, Lentjes MA, Luben RN, Khaw KT, Welch AA. Dietary magnesium and potassium intakes and circulating magnesium are associated with heel bone ultrasound attenuation and osteoporotic fracture risk in the EPIC-Norfolk cohort study. Am J Clin Nutr. Kong SH, Kim JH, Hong AR, Lee JH, Kim SW, Shin CS. Dietary potassium intake is beneficial to bone health in a low calcium intake population: the Korean National Health and Nutrition Examination Survey KNHANES Osteoporos Int. Fenton TR, Eliasziw M, Lyon AW, Tough SC, Hanley DA. Meta-analysis of the quantity of calcium excretion associated with the net acid excretion of the modern diet under the acid-ash diet hypothesis. Expression of osteoporosis as determined by diet-disordered electrolyte and acid-base metabolism. In: Burckhardt P, Dawson-Hughes B, Heaney R, eds. Nutritional Aspects of Osteoporosis. San Diego: Academic Press; Sebastian A, Harris ST, Ottaway JH, Todd KM, Morris RC, Jr. Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. N Engl J Med. Jehle S, Hulter HN, Krapf R. Effect of potassium citrate on bone density, microarchitecture, and fracture risk in healthy older adults without osteoporosis: a randomized controlled trial. J Clin Endocrinol Metab. Dawson-Hughes B, Harris SS, Palermo NJ, et al. Potassium bicarbonate supplementation lowers bone turnover and calcium excretion in older men and women: a randomized dose-finding trial. J Bone Miner Res. Macdonald HM, Black AJ, Aucott L, et al. Effect of potassium citrate supplementation or increased fruit and vegetable intake on bone metabolism in healthy postmenopausal women: a randomized controlled trial. Lambert H, Frassetto L, Moore JB, et al. The effect of supplementation with alkaline potassium salts on bone metabolism: a meta-analysis. Granchi D, Caudarella R, Ripamonti C, et al. Potassium citrate supplementation decreases the biochemical markers of bone loss in a group of osteopenic women: the results of a randomized, double-blind, placebo-controlled pilot study. Centers for Disease Control and Prevention. High Blood Pressure Facts. November Mente A, O'Donnell M, Rangarajan S, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Sanghavi S, Vassalotti JA. Dietary sodium: a therapeutic target in the treatment of hypertension and CKD. J Ren Nutr. Cogswell ME, Loria CM, Terry AL, et al. |
| Overview of Potassium's Role in the Body | Hyperkalemia and its management MEEQAT HOSPITAL. pptxbiochemistryyyyyyyyyyyyyy AnnaKhurshid. Calcium disorders. Calcium disorders Saleh Alorainy. Unit 8: Kidney Functions and disorders. Unit 8: Kidney Functions and disorders DrElhamSharif. approach to hypokalemia. pptx SreekuttyBindhu1. Hypokalemia - Pharmacotherapy. Hypokalemia - Pharmacotherapy Areej Abu Hanieh. Management of renal disease in dog. Management of renal disease in dog Vikash Babu Rajput. Similar to Metabolism of potassium and its clinical significance 20 Parathyroid gland. Parathyroid gland. More from rohini sane Biotin vitamin b7 biological functions, clinical indications and its techn Biotin vitamin b7 biological functions, clinical indications and its techn Scurvy deficiency of vitamin C. Scurvy deficiency of vitamin C rohini sane. Vitamin C Ascorbic acid. Vitamin C Ascorbic acid rohini sane. Microscopic examination of urine. Microscopic examination of urine rohini sane. Urinalysis for detection of abnormal constituents. Urinalysis for detection of abnormal constituents rohini sane. Urinalysis for detection of normal inorganic and organic constituents. Urinalysis for detection of normal inorganic and organic constituents rohini sane. Biochemical kidney function tests with their clinical applications. Biochemical kidney function tests with their clinical applications rohini sane. Total parenteral nutrition TPN. Total parenteral nutrition TPN rohini sane. Food toxicants. Food toxicants rohini sane. Nutritional management of clinical disorders. Nutritional management of clinical disorders rohini sane. Prescription of diet. Prescription of diet rohini sane. Nutritional importance of vitamins and minerals. Nutritional importance of vitamins and minerals rohini sane. Nutritional importance of proteins. Nutritional importance of proteins rohini sane. Biochemical aspects of obesity. Biochemical aspects of obesity rohini sane. Nutritional aspects of lipids. Nutritional aspects of lipids rohini sane. Basal metabolic rate bmr and nutrition. Basal metabolic rate bmr and nutrition rohini sane. Nutritional importance of carbohydrates. Nutritional importance of carbohydrates rohini sane. Physical activity of the human body and nutrition. Physical activity of the human body and nutrition rohini sane. Specific dynamic action and nutrition. Specific dynamic action and nutrition rohini sane. Respiratory quotient of nutrients. Respiratory quotient of nutrients rohini sane. More from rohini sane 20 Biotin vitamin b7 biological functions, clinical indications and its techn Recently uploaded SGK ÁP XE PHỔI Y6 Y HÀ NỘI BẢN MỚI NHẤT. SGK ÁP XE PHỔI Y6 Y HÀ NỘI BẢN MỚI NHẤT. pdf HongBiThi1. The Catastrophe Anaphylaxis , Case based approach to guidelines Ahmed Yehia Internal medicine department, faculty of Medicine Beni-Suef University Egypt. Michael Gisondi. Hospital Pharmacy and Community Pharmacy. pdf KHUSHABU KATEKAR. pptx Mathew Joseph. Vilsmeyer haack reaction. Vilsmeyer haack reaction AmlanjyotiRajkhowa. pdf ENT by QuickMedTalk Quick MedTalk. AI in Healthcare Resource forhands on Workshop. AI in Healthcare Resource forhands on Workshop Vaikunthan Rajaratnam. Impression Materials Part - 1. Impression Materials Part - 1 Dr. shiva sai vemula. Hematopoiesis production and Disorders. pptx Tagore medical College. Treatment of chronic inflammatory demyelinating polyneuropathy. Treatment of chronic inflammatory demyelinating polyneuropathy MohamadAlhes. Role of microRNA in Cervical Cancer Cells. pptx ESTEBAN RESTREPO MONSALVE. Arterial Supply and Venous Drainage of Pelvis. pptx Allen College. Discover Wellness with Leanbliss: A Journey to a Lean Lifestyle. Discover Wellness with Leanbliss: A Journey to a Lean Lifestyle anumtaa pptx TyraRideaux. Medication Adherence APR. pptx Ravinandan A P. Community Pharmacy Ravinandan A P 7th Sem. Mamata R. pptx anjalirakhade Recently uploaded 20 SGK ÁP XE PHỔI Y6 Y HÀ NỘI BẢN MỚI NHẤT. Metabolism of potassium and its clinical significance 1. Metabolism of Potassium and its clinical significance Dr. Rohini C Sane. Major intracellular cation 2. Transmission of nerve impulse 4. Acid base balance 5. Intracellular potassium concentration is necessary for protein biosynthesis by ribosomes. preanalytical error. Homoeostasis of Potassium by Transcellular movement 2. Role of gastrointestinal tract in Homoeostasis of Potassium 3. Role of Kidney in Homoeostasis of Potassium. Potassium ions transport across the cell membrane. It action is by constricting arterioles and increasing heartbeats. Angiotensin II later hydrolyzed by Angiotensinase. Since abnormalities in K metabolism can also cause lethal arrhythmia or sudden cardiac death, it is extremely important to monitor patients with a high risk of hyper- or hypokalemia and attempt to provide early and appropriate intervention. Keywords: CKD; blood pressure; hypertension; potassium; potassium excretion; salt; sodium. Abstract Potassium K , the main cation inside cells, plays roles in maintaining cellular osmolarity and acid-base equilibrium, as well as nerve stimulation transmission, and regulation of cardiac and muscle functions. Publication types Review. Substances Potassium. |
| Potassium metabolism | Nature —, Corvol P, Pinet F, Galen FX, Plouin PF, Chatellier G, Pagny JY, Bruneval P, Camilleri JP, Ménard J: Primary reninism In: JH Laragh, BM Brenner, eds, Hypertension. Simon N, Franklin SS, Bleifer KH, Maxwell MH: Clinical characteristics of renovascular hypertension. DAMA —, White RH, Schambelan M: Hypertension, hyperreninemia, and secondary hyperaldosteronism in systemic necrotizing vasculitis. Ruby ST, Burch A, White WB: Unilateral renal artery stenosis seen initially as severe and symptomatic hypokalemia. Arch Surg —, Edwards CRW, Walker BR, Benediktsson R, Seckl JR: Congenital and acquired syndromes of apparent mineralocorticoid excess. J Steroid Biochem Mol Biol 1—5, Biglieri EG, Kater CE: Mineralocorticoids in congenital adrenal hyperplasia. J Steroid Biochem Mol Biol —, Mantero F, Boscaro M: Glucocorticoid-dependent hypertension. Stewart PM, Come JET, Shackleton CHL, Edwards CRW: Syndrome of apparent mineralocorticoid excess. Clore J, Schoolwerth A, Watlington CO: When is cortisol a mineralocorticoid? Stewart PM, Wallace AM, Valentine R, Burt D, Shackleton CHL, Edwards CRW: Mineralocorticoid activity of liquorice: beta-hydroxysteroid dehydrogenase deficiency comes of age. Farese RV, Biglieri EG, Shackleton CHL, Irony I, Gomez-Fontes R: Licorice-induced hypermineralocorticoidism. Stewart PM, Wallace AM, Atherden SM, Shearing CH, Edwards CRW: Mineralocorticoid activity of carbenoxolone: contrasting effects of carbenoxolone and liquorice on - hydroxysteroid dehydrogenase activity in man. Clin Sci Atchley DW, Loeb RF, Richards DW, Benedict EM, —54, Driscoll ME: On diabetic acidosis: a detailed study of electro-. Nielsen I, Pedersen RS: Life-threatening hypokalaemia lyte balances following the withdrawal and reestablishment caused by liquorice ingestion. Lancet , of insulin therapy. Young WF, Klee GG: Primary aldosteronism. Diagnostic Brodsky WA, Rapoport S, West CD: The mechanism of evaluation. Endocrinol Metab Clin North Am —, glycosuric diuresis in diabetic man. J Clin Invest — Bravo EL: Primary aldosteronism. Urol Clin North Am Adrogué HJ, Lederer ED, Suki WN, Eknoyan G: Determi- —, nants of plasma potassium levels in diabetic ketoacidosis. Biglieri EG: Spectrum of mineralocorticoid hypertension. Hypertension —, Fulop M: Hyperkalemia in diabetic ketoacidosis. Am J Med. Bartter FC, Pronove P, Gill JR Jr, MacCardle RC: Sci —, Hyperplasia of the juxtaglomerular complex with Semin Nephrol —, Shils ME: Experimental human magnesium depletion. Ann Rev Med —, cine —85, Shils ME: Experimental production of magnesium deficiency. in man. Ann NY Acad Sci —, Kidney Int —93, Dunn MJ, Walser M: Magnesium depletion in normal man. Fichman MP, Telfor N, Zia P, Speckart P, Golub M, Rude R: Metabolism —, Evans RA, Carter JN, George CRP, Walls RS, Newland RC, drome. Verbeckmoes R, van Damme B, Clement J, Amery A, losing kidney. renomedullary cells. Successful treatment with indo- Whang R, Flink EB, Dyckner T, Wester PO, Aikawa JK, methacin. Ryan MP: Magnesium depletion as a cause of refractory. Gill JR Jr, Frölich JC, Bowden RE, Taylor AA, Keiser HR, potassium repletion. A Rodriguez M, Solanki DL, Whang R: Refractory potassium disorder characterized by high urinary prostaglandins and a repletion due to cisplatin-induced magnesium depletion. dependence of hyperreninemia on prostaglandin synthesis. Am J Med —51, Holmes AM, Hesling CM, Wilson TM: Drug-induced sec-. Gitelman HJ: Hypokalemia, hypomagnesemia, and alkalosis: ondary hyperaldosteronism in patients with pulmonary tu- A rose is a rose—or is it? J Pediatr —80, Q J Med —, Gill JR Jr, Bell NH, Bartter FC: Impaired conservation of Bar RS, Wilson HE, Mazzaferri EL: Hypomagnesemic sodium and potassium in renal tubular acidosis and its correc hypocalcemia secondary to renal magnesium wasting. A pos- tion by buffer anions. sible consequence of high-dose gentamicin therapy. Ann In-. Gennari FJ, Cohen JJ: Renal tubular acidosis. Annu Rev Med tern Med —, Gearhart MO, Sorg TB: Foscarnet-induced severe hypo-. Sebastian A, Hulter HN, Kurtz I, Maher T, Schambelan M: magnesemia and other electrolyte disorders. Ann Disorders of distal nephron function. Am J Med —, Pharmacother —, Barton CH, Pahl M, Vaziri ND, Cesario T: Renal magnesium. Sebastian A, McSherry E, Morris RC Jr: Renal potassium wasting associated with amphotericin B therapy. Am J Med wasting in renal tubular acidosis RTA. Its occurrence in —, types 1 and 2 RTA despite sustained correction of systemic Burgess JL, Birchall R: Nephrotoxicity of amphotericin B, acidosis. with emphasis on changes in tubular function. Wrong OM, Feest TG, Maclver AG: Immune-related —84, potassium-losing interstitial nephritis: a comparison with Mir MA, Brabin B, Tang OT, Leyland MJ, Delamore IW:. distal renal tubular acidosis. Q J Med —, Hypokalaemia in acute myeloid leukaemia. Ann Intern Med. Caruana RJ, Buckalew VM: The syndrome of distal type I Fisher JR: Hypokalemia in leukemia. Ann Intern Med , renal tubular acidosis. Medicine 84—99, Lightwood R, Payne WW, Black JA: Infantile renal acidosis. Lantz B, Carmark B, Reizenstein P: Electrolytes and whole. Pediatrics —, body potassium in acute leukemia. Acta Med Scand Brenes LG, Brenes JN, Hernandez MM: Familial proximal 50, renal tubular acidosis. Perry MC, Bauer JH, Farhangi M: Hypokalemia in acute. Sebastian A, McSherry E, Morris RC Jr: On the mechanism myelogenous leukemia. of potassium wasting in renal tubular acidosis associated with Sterns RH, Cox M, Feig PU, Singer I: Internal potassium the Fanconi syndrome type 2 RTA. J Clin Invest balance and the control of the plasma potassium concentra- , Harrington JT, Cohen JJ. Metabolic acidosis. In: JJ Cohen, Lawson DH: Adverse reactions to potassium chloride. Q J JP Kassirer with collaboration of FJ Gennari, JT Med —, Harrington, NE Madias , Acid—Base. Little, Brown, Boston, Ponce SP, Jennings AE, Madias NE, Harrington JT: Drugpp —, indued hyperkalemia. Rimmer JM, Horn JF, Gennari FJ: Hyperkalemia as a complication of drug therapy. Hultgren HN, Swenson R, Wettach G: Cardiac arrest due to oral potassium administration. McMahon FG, Ryan JR, Akdamar K, Ertan A: Effect of potassium chloride supplements on upper gastrointestinal mucosa. Clin Pharmacol Ther —, Alsop WR, Moore JG, Rollins DE, Tolman KE: The effects of five potassium chloride preparations on the upper gastrointestinal mucosa in healthy subjects receiving glycopyrrolate. J Clin Pharmacol —, Strom BL, Carson JL, Schinnar R, Sim E, Maislin G, Soper K, Morse L: Upper gastrointestinal tract bleeding from oral potassium chloride. Schwartz AB, Swartz CD: Dosage of potassium chloride elixir to correct thiazide-induced hypokalemia. Wan HH, Lye MDW. Moduretic-induced metabolic acidosis and hyperkalaemia. Cohen AB: Hyperkalemic effects of triamterene. Paice B, Gray JMB, McBride D, Donnelly T, Lawson DH: Hyperkalaemia in patients in hospital. Br Med J , Mather A, Mackie NR: Effects of hemolysis on serum electrolyte values. Clin Chem 6: —, Bronson WR, DeVita VT, Carbone PP, Cotlove E: Pseudohyperkalemia due to release of potassium from white blood cells during clotting. Bellevue R, Dosik H, Spergel G, Gussoff BD: Pseudohyperkalemia and extreme leukocytosis. J Lab Clin Med —, Stewart GW, Corrall RJM, Fyffe JA, Stockdill G, Strong JA: Familial pseudohyperkalaemia: a new syndrome. Graber M, Subramani K, Corish D, Schwab A: Thrombocytosis elevates serum potassium. Am J Kidney Dis —, Lum G, Gambino SR: A comparison of serum versus heparinized plasma for routine chemistry tests. Am J Clin Pathol —, Ladenson JH, Tsai LB, Michael JM, Kessler G, Joist JH: Serum versus heparinized plasma for eighteen common chemistry tests. Hartmann RC, Auditore JV, Jackson DP: Studies on thrombocytosis. Hyperkalemia due to release of potassium from platelets during coagulation. Kerr DJ, McAlpine LG, Dagg JH: Pseudohyperkalaemia. Don BR, Sebastian A, Cheitlin M, Christiansen M, Schambelan M: Pseudohyperkalemia caused by fist clenching during phlebotomy. Finch CA, Sawyer CG, Flynn JM: Clinical syndrome of potassium intoxication. Am J Med 1: —, Davis JO, Urquhart J, Higgins JT Jr: The effects of alterations of plasma sodium and potassium concentration on aldosterone secretion. Fredlund P, Saltman S, Kondo T, Douglas J, Catt KJ: Aldosterone production by isolated glomerulosa cells: modulation of sensitivity to angiotensin II and ACTH by extracellular potassium concentration. Miller PD, Waterhouse C, Owens R, Cohen E: The effect of potassium loading on sodium excretion and plasma renin activity in Addisonian man. van Ypersele de Strihou C: Potassium homeostasis in renal failure. Gonick HC, Kleeman CR, Rubin ME, Maxwell MH: Functional impairment in chronic renal disease III. Studies of potassium excretion. Perez GO, Pelleya R, Oster JR, Kem DC, Vaamonde CA: Blunted kaliuresis after an acute potassium load in patients with chronic renal failure. Kahn T, Kaji DM, Nicolis G, Krakoff LR, Stein RM: Factors related to potassium transport in chronic stable renal disease in man. Clin Sci Mol Med —, Bergström J, Alvestrand A, Fürst P, Hultman E, WidstamAttorps U: Muscle intracellular electrolytes in patients with chronic uremia. Kidney Int 24 Suppl 16 : S — S, Boddy K, King PC, Lindsay RM, Briggs JD, Winchester JF, Kennedy AC: Total body potassium in non-dialyzed and dialyzed patients with chronic renal failure. Br Med J 1: —, Widmer B, Gerhardt RE, Harrington JT, Cohen JJ: Serum electrolyte and acid—base composition. The influence of graded degrees of chronic renal failure. Restuccio A: Fatal hyperkalemia from a salt substitute. Sopko JA, Freeman RM: Salt substitutes as a source of potassium. Luzi L, Barrett EJ, Groop LC, Ferrannini E, DeFronzo RA: Metabolic effects of low-dose insulin therapy on glucose metabolism in diabetic ketoacidosis. Diabetes —, DeFronzo RA: Obesity is associated with impaired insulin-mediated potassium uptake. Cohen P, Barzilai N, Lerman A, Hard H, Szylman P, Karnieli E: Insulin effects on glucose and potassium metabolism in vivo: evidence for selective insulin resistance in humans. DeFronzo RA: Hyperkalemia and hyporeninemic hypoaldosteronism. Sunderlin FS, Anderson GH, Streeten DHP, Blumenthal SA: The renin—angiotensin—aldosterone system in diabetic patients with hyperkalemia. Conte G, Dal Canton A, Imperatore P, DeNicola L, Gigliotti G, Pisanti N, Memoli B, Furiano G, Esposito C, Andreucci VE: Acute increase in plasma osmolality as a cause of hyperkalemia in patients with renal failure. Goldfarb S, Cox M, Singer I, Goldberg M: Acute hyperkalemia induced by hyperglycemia: hormonal mechanisms. Perez GO, Lespier L, Knowles R, Oster JR, Vaamonde CA: Potassium homeostasis in chronic diabetes mellitus. Perez GO, Lespier L, Jacobi J, Oster JR, Katz FH, Vaamonde C, Fishman LM: Hyporeninemia and hypoaldosteronism in diabetes mellitus. Arrizabalaga P, Montoliu J, Martinez-Vea A, Andreu L, Lopez-Pedret J, Revert L: Increase in serum potassium caused by beta-2 adrenergic blockade in terminal renal failure: absence of mediation by insulin or aldosterone. Proc Eur Dial Transplant Assoc —, Arthur S, Greenberg A: Hyperkalemia associated with intravenous labetabol therapy for acute hypertension in renal transplant recipients. Clin Nephrol —, Fletcher GF, Fletcher BJ, Sweeney ME: Effects of exercise testing, training and beta blockade on serum potassium in normal subjects. Am J Cardiol —, Castellino P, Bia MJ, DeFronzo RA: Adrenergic modulation of potassium metabolism in uremia. Ericsson F, Carlmark B, Jogestrand T, Sundqvist K: Effect of digoxin upon intracellular potassium in man. Scand J Clin Lab Invest —, Bismuth C,. Gaultier M, Conso F, Efthymiou ML: Hyperkalemia in acute digitalis poisoning: prognostic significance and therapeutic implications. Clin Toxicol 6: —, Smith TW, Butler VP Jr, Haber E, Fozzard H, Marcus FI, Bremner WF, Schulman IC, Phillips A: Treatment of life-threatening digitalis intoxication with digoxin-specific Fab antibody fragments. Reza MJ, Kovick RB, Shine KI, Pearce ML: Massive intravenous digoxin overdosage. Papadakis MA, Wexman MP, Fraser C, Sedlacek SM: Hyperkalemia complicating digoxin toxicity in a patient with renal failure. Am J Kidney Dis 5: 64—66, Evers W, Racz GB, Dobkin AB: A study of plasma potassium and electrocardiographic changes after a single dose of succinylcholine. Can Anesth Soc J —, Weintraub HD, Heisterkamp DV, Cooperman LH: Changes in plasma potassium concentration after depolarizing blockers in anaesthetized man. Br J Anaesth —, Cooperman L: Succinylcholine-induced hyperkalemia in neuromuscular disease. Brooke MM, Donovan WH, Stolov WC: Paraplegia: succinylcholine-induced hyperkalemia and cardiac arrest. Arch Phys Med Rehab —, Greenawalt JW 3rd: Succinylcholine-induced hyperkalemia 8 weeks after a brief paraplegic episode. Dickerman HW, Walker WG: Effect of cationic amino acid infusion on potassium metabolism in vivo. Levinsky NG, Tyson I, Miller RB, Reiman AS: The relation between amino acids and potassium in isolated rat muscle. Hertz P, Richardson JA: Arginine-induced hyperkalemia in renal failure patients. Bushinsky DA, Gennari FJ: Life-threatening hyperkalemia induced by arginine. McIvor M, Baltazar RF, Beltran J, Mower MM, Wenk R, Lustgarten J, Salomon J: Hyperkalemia and cardiac arrest from fluoride exposure during hemodialysis. Gabow PA, Kaehny WD, Kelleher SP: The spectrum of rhabdomyolysis. Bluemle LW Jr, Webster GD, Elkinton JR: Acute tubular necrosis: analysis of one hundred cases with respect to mortality, complications and treatment with and without dialysis. Grossman RA, Hamilton RW, Morse BM, Penn AS, Goldberg M: Nontraumatic rhabdomyolysis and acute renal failure. Gamstorp I, Hauge M, Helweg-Larsen HF, Mjönes H, Sagild U: Adynamica episodica hereditaria. Ptacek LJ, Johnson KJ, Griggs RC: Genetics and physiology of the myotonic muscle disorders. Ptacek LJ, George AL Jr, Griggs RC, Tawil R, Kallen RG, Barchi RL, Robertson M, Leppert MF: Identification of a mutation in the gene causing hyperkalemic periodic paralysis. Cell —, Fontaine B, Khurana TS, Hoffman EP, Bruns GAP, Haines JL, Trofatter JA, Hanson MP, Rich J, McFarlane H, Yasek DM, Romano D, Gusella JF, Brown RH Jr: Hyperkalemic periodic paralysis and the adult muscle sodium channel a-subunit gene. Cannon SC, Brown RH Jr, Corey DP: A sodium channel defect in hyperkalemic periodic paralysis: potassium-induced failure of inactivation. Neuron 6: —, Streeten DHP, Dalakos TG, Fellerman H: Studies on hyperkalemic periodic paralysis. Evidence of changes in plasma Na and Cl and induction of paralysis by adrenal glucocorticoids. Wang P, Clausen T: Treatment of attacks in hyperkalaemic familial periodic paralysis by inhalation of salbutamol. Lancet 1: —, Martin RS, Panese S. Virginillo M, Gimenez M, Litardo M, Arrizurieta E, Hayslett JP: Increased secretion of potassium in the rectum of humans with chronic renal failure. Am J Kidney Dis 8: —, Hou S, McElroy PA, Nootens J, Beach M: Safety and efficacy of low-potassium dialysate. Gennari FJ, Rimmer JM: Disturbances in fluid, electrolyte, and acid-base balance. Part 2. Dialysis patients. In: SG Massry, RJ Glassock, eds, Textbook of Nephrology , 3rd ed. Williams and Wilkins, Baltimore, pp —, Greenblatt DJ, Koch-Weser J: Adverse reactions to spironolactone. DAMA 40—43, Walker BR, Capuzzi DM, Alexander F, Familiar RG, Hoppe RC: Hyperkalemia after triamterene in diabetic patients. Feinfeld DA, Carvounis CP: Fatal hyperkalemia and hyperchloremic acidosis. DAMA , McNay JL, Oran E: Possible predisposition of diabetic patients to hyperkalemia following administration of potassium-retaining diuretic, amiloride MK Metabolism 58—70, Atlas SA, Case DB, Sealey JE, Laragh JH, McKinstry DN: Interruption of the renin-angiotensin system in hypertensive patients by captopril induces sustained reduction in aldosterone secretion, potassium retention and natriuresis. Hypertension 1: —, Textor SC, Bravo EL, Fouad FM, Tarazi RC: Hyperkalemia in azotemic patients during angiotensin-converting enzyme inhibition and aldosterone reduction with captopril. Bauer JH: Role of angiotensin converting enzyme inhibitors in essential and renal hypertension. Am J Med 77 Suppl 2A : 43—51, Zachariah PK, Bonnet G, Chysant SG, DeBackser G, Goldstein R, Herrera J, Lindner A, Materson BJ, Maxwell MH, McMahon FG, Merrill RH, Paton RR, Rapp AD, Roginsky MS, Seedat YK, Sime F, Vaicaitis JS, Weinberg MS, Zusman RM: Evaluation of antihypertensive efficacy of lisinopril compared to metaprolol in moderate to severe hypertension. J Cardiovasc Pharmacol 9 Suppl 3 : S53 - S58, Donohoe JF, Laher M, Doyle GD, Cooper WD: Lisinopril in hypertension associated with renal impairment. J Cardiovasc Pharmacol 9 Suppl 3 : S66 - S68, deJong PE, Apperloo AJ, Heeg JE, deZeeuw D: Lisinopril in hypertensive patients with renal function impairment. Nephron 55 Suppl 1 : 43—48, Doman K, Perlmutter JA, Muhammedi M, Puschett JB: Life-threatening hyperkalemia associated with captopril administration. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD: The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. Feig PU, Rutan GH: Angiotensin converting enzyme inhibitors: The end of end-stage renal disease? Praga M, Hernandez E, Montoyo C, Andrés A, Ruilope LM, Rodicio JL: Long-term beneficial effects of angiotensinconverting enzyme inhibition in patients with nephrotic proteinuria. Captopril Multicenter Research Group. A placebo-controlled trial of captopril in refractory chronic congestive heart failure. J Am Coll Cardiol 2: —, Tan SY, Shapiro R, Franco R, Stockard H, Mulrow PJ: Indomethacin-induced prostaglandin inhibition with hyperkalemia. Clive DM, Stoff JS: Renal syndromes associated with nonsteroidal anti-inflammatory drugs. Whelton A, Hamilton CW: Nonsteroidal anti-inflammatory drugs: effects on kidney function. J Clin Pharmacol , Rotenberg FA, Giannini VS: Hyperkalemia associated with ketorolac. Ann Pharmacother —, Wilson ID, Goetz FC: Selective hypoaldosteronism after prolonged heparin administration. Conn JW, Rovner DR, Cohen EL, Anderson JE Jr: Inhibition by heparinoid of aldosterone biosynthesis in man. Busch EH, Ventura HO, Lavie CJ: Heparin-induced hyperkalemia. Aull L, Chao H, Coy K: Heparin-induced hyperkalemia. DICP Ann Pharmacother —, Edes TE, Sunderrajan EV: Heparin-induced hyperkalemia. Adu D, Turney J, Michael J, McMaster P: Hyperkalaemia in cyclosporin-treated renal allograft recipients. Lancet 2: , Bantle JP, Nath KA, Sutherland DER, Najarian JS, Ferris TF: Effects of cyclosporine on the renin-angiotensinaldosterone system and potassium excretion in renal transplant recipients. Kamel KS, Ethier JH, Quaggin S, Levin A, Albert S, Carlisle EJF, Halperin ML: Studies to determine the basis for hyperkalemia in recipients of a renal transplant who are treated with cyclosporine. J Am Soc Nephrol 2: —, Bantle JP, Boudreau RJ, Ferris TF: Suppression of plasma renin activity by cyclosporine. Am J Med 59—64, Velazquez H, Perazella MA, Wright FS, Ellison DH: Renal mechanism of trimethoprim-induced hyperkalemia. Lachaal M, Venuto RC: Nephrotoxicity and hyperkalemia in patients with acquired immunodeficiency syndrome treated with pentamidine. Briceland LL, Bailie GR: Pentamidine-associated nephrotoxicity and hyperkalemia in patients with AIDS. DICP —, A report of cases. Acta Endocrinol —, Lancet 1: 11—14, Yamamoto T, Fukuyama J, Hasegawa K, Sugiura M: Isolated corticotropin deficiency in adults. Arch Intern Med , Schambelan M, Sebastian A, Biglieri EG: Prevalence, pathogenesis, and functional significance of aldosterone deficiency in hyperkalemic patients with chronic renal insufficiency. Kidney Int 89—, Nadler JL, Lee FO, Hsueh W, Horton R: Evidence of prostacyclin deficiency in the syndrome of hyporeninemic hypoaldosteronism. Ulick S, Eberlin WR, Bliffeld AR, Chu MD, Bongiovanni AM: Evidence for an aldosterone biosynthetic defect in congenital adrenal hyperplasia. Hamilton W, McCandless AE, Ireland JT, Gray CE: Hypoaldosteronism in three sibs due to dehydrogenase deficiency. Veldhuis JD, Kulin HE, Santen RJ, Wilson TE, Melby JC: Inborn error in the terminal step of aldosterone biosynthesis. Braithwaite SS, Barbato AL, Emanuele MA: Acquired partial corticosterone methyl oxidase type II defect in diabetes mellitus. Diabetes Care —, Oberfield SE, Levine LS, Carey RM, Bejar R, New MI: Pseudohypoaldosteronism: multiple target organ unresponsiveness to mineralocorticoid hormones. Armanini D, Kuhnle U, Strasser T, Dorr H, Butenandt I, Weber PC, Stockigt JR, Pearce P, Funder JW: Aldosteronereceptor deficiency in pseudohypoaldosteronism. Armanini D, Wehling M, DaDalt L, Zennaro M, Scali U, Keller U, Pratesi C, Mantero F, Kuhnle U: Pseudohypoaldosteronism and mineralocorticoid receptor abnormalities. Brautbar N, Levi J, Rosler A, Leitesdorf E, Djaldeti M, Epstein M, Kleeman CR: Familial hyperkalemia, hypertension and hyporeninemia with normal aldosterone levels. Schambelan M, Sebastian A, Rector FC Jr: Mineralocorticoid-resistant renal hyperkalemia without salt wasting type II pseudohypoaldosteronism : role of increased renal chloride reabsorption. Take C, Ikeda K, Kurasawa T, Kurokawa K: Increased chloride reabsorption as an inherited renal tubular defect in familial type II pseudohypoaldosteronism. DeFronzo RA, Cooke R, Goldberg M, Cox M, Myers AR, Agus ZS: Impaired renal tubular potassium secretion in systemic lupus erythematosus. Battle D, Itsarayoungyuen K, Arruda JAL, Kurtzman NA: Hyperkalemic hyperchloremic metabolic acidosis in sickle cell hemoglobinopathies. Batlle DC: Segmental characterization of defects in collecting tubule acidification. Battle DC, Arruda JAL, Kurtzman NA: Hyperkalemic distal renal tubular acidosis associated with obstructive uropathy. Cogan MG, Arieff AI: Sodium wasting, acidosis and hyperkalemia induced by methicillin interstitial nephritis. Chamberlain MJ: Emergency treatment of hyperkalaemia. Garcia-Palmieri MR: Reversal of hyperkalemic cardiotoxicity with hypertonic saline. Ballantyne F III, Davis LD, Reynolds EW Jr: Cellular basis for reversal of hyperkalemic electrocardiographic changes by sodium. Blumberg A, Weidmann P, Shaw S, Gnädinger M: Effect of various therapeutic approaches on plasma potassium and major regulatory factors in terminal renal failure. Alton M, Dunlay R, Copkney C: Nebulized albuterol for acute hyperkalemia in patients on hemodialysis. Montoliu J, Lens XM, Revert L: Potassium-lowering effect of albuterol for hyperkalemia in renal failure. Blumberg A, Weidmann P, Ferrari P: Effect of prolonged bicarbonate administration on plasma potassium in terminal renal failure. Fraley DS, Adler S: Correction of hyperkalemia by bicarbonate despite constant blood pH. Flinn RB, Merrill JP, Welzant WR: Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol. Greenman L, Peters JH, Mateer FM, Danowski TS: Probable clinical utility of cation exchange resins. Scherr L, Ogden DA, Mead AW, Spritz N, Rubin AL: Management of hyperkalemia with a cation-exchange resin. Kramer P, Levitan R: Effect of 9-a-fluorohydrocortisone on the ileal excreta of ileostomized subjects. Gastroenterology —, Clarke AM, Hill GL, MacBeth WAAG: Intestinal adaptation to salt depletion in a patient with an ileostomy. Evans BM, Hughes-Jones NC, Milne MD, Yellowlees H: Ion-exchange resins in treatment of anuria. Lancet 2: 79 , Emmett M, Hootkins R, Santa Ana CA, Porter JL, Fordtran JS: Effect of three laxatives and a cation exchange resin on fecal sodium and potassium excretion. Lillemoe KD, Romolo JL, Hamilton SR, Pennington LR, Burdick JF, Williams GM: Intestinal necrosis due to sodium polystyrene Kayexalate in sorbitol enemas: clinical and experimental support for the hypothesis. Surgery —, Wootton FT, Rhodes DF, Lee WM, Fitts CT: Colonic necrosis with kayexelate-sorbitol enemas after renal transplantation. Gerstman BB, Kirkman R, Platt R: Intestinal necrosis associated with postoperative orally administered sodium polystyrene sulfate in sorbitol. Berlyne GM, Janabi K, Shaw AB: Dangers of resonium A in the treatment of hyperkalaemia in renal failure. Alton M: Treatment and prevention of hyperkalemia in end-stage renal disease. Download references. Nephrology Unit, University of Vermont College of Medicine, , Burlington, VT, USA. John Gennari M. Professor of Medicine, Director. You can also search for this author in PubMed Google Scholar. Reprints and permissions. Gennari, F. Disorders of Potassium Metabolism. In: Suki, W. Springer, Boston, MA. Publisher Name : Springer, Boston, MA. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Our bodies need far more potassium than sodium each day, but the typical U. But what may be even more important for health is the relationship of sodium to potassium in the diet. Hypertension Observational studies of large groups of people show that sodium and potassium in the diet are associated with blood pressure. A review of randomized controlled trials found that the DASH diet Dietary Approaches to Stop Hypertension that is low sodium and high potassium was effective at lowering blood pressure in those with existing hypertension. The Agency for Healthcare Research and Quality issued a report on the effects of sodium and potassium on chronic disease risk based on clinical trials and cohort studies. However there was not enough evidence or there was conflicting evidence of their effects on lowering overall risk of hypertension, kidney stones, cardiovascular diseases including stroke, and kidney disease. Bone health Calcium is one of the most important nutrients required for bone health. Kidney stones A diet rich in potassium helps to prevent calcium from being excreted in the urine, and may also help to prevent calcium from being released from bone into the blood. Is there any research behind Acid-Alkaline Diet claims? You may have heard of an acid-alkaline diet promoted for weight loss or cancer prevention. Most health experts rejected these claims because it is nearly impossible to dramatically change the pH of blood in healthy people through diet alone. The body tightly regulates the pH level in blood to about 7. References National Academy of Medicine. Dietary Reference Intakes for Sodium and Potassium. Washington DC : National Academies Press US ; Mar. National Institutes of Health; Office of Dietary Supplements. Potassium: Fact Sheet for Health Professionals. Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. International journal of epidemiology. Dietary Guidelines for Americans Scientific Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, , to the Secretary of Agriculture and the Secretary of Health and Human Services. Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang MH, Gwinn M, Dowling N, Khoury MJ, Hu FB. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Archives of internal medicine. Aaron KJ, Sanders PW. Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. InMayo Clinic Proceedings Sep 1 Vol. Newberry SJ, Chung M, Anderson CA, Chen C, Fu Z, Tang A, Zhao N, Booth M, Marks J, Hollands S, Motala A. Sodium and Potassium Intake: Effects on Chronic Disease Outcomes and Risks. Rockville MD : Agency for Healthcare Research and Quality US ; Jun. Report No. Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. Vinceti M, Filippini T, Crippa A, de Sesmaisons A, Wise LA, Orsini N. Journal of the American Heart Association. Hanley DA, Whiting SJ. Does a high dietary acid content cause bone loss, and can bone loss be prevented with an alkaline diet?. Journal of Clinical Densitometry. How we vet brands and products Healthline only shows you brands and products that we stand behind. Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we: Evaluate ingredients and composition: Do they have the potential to cause harm? Fact-check all health claims: Do they align with the current body of scientific evidence? Assess the brand: Does it operate with integrity and adhere to industry best practices? We do the research so you can find trusted products for your health and wellness. Read more about our vetting process. Was this helpful? Sources of potassium. Potassium deficiency. Potassium overdose. Treating imbalanced potassium levels. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Mar 27, Written By Kristeen Cherney, PhD. Feb 28, Medically Reviewed By Deborah Weatherspoon, Ph. Share this article. Read this next. Understanding Hyperkalemia High Potassium. Medically reviewed by Angelica Balingit, MD. Potassium Blood Test. Medically reviewed by Sirisha Yellayi, DO. Symptoms of Low Potassium Hypokalemia. By Katey Davidson, MScFN, RD, CPT and Ryan Raman, MS, RD. What Does Potassium Do for Your Body? A Detailed Review. Blood Tests for Hemochromatosis. Medically reviewed by Mia Armstrong, MD. What to Know About Gaucher Disease Type 3. Medically reviewed by Alana Biggers, M. |
| Overview of Disorders of Potassium Concentration | Biochemical and Physiological Aspects of Human Nutrition. Philadelphia: W. Saunders Company; Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, D. The National Academies Press. Mumoli N, Cei M. Licorice-induced hypokalemia. Int J Cardiol. Walker BR, Edwards CR. Licorice-induced hypertension and syndromes of apparent mineralocorticoid excess. Endocrinol Metab Clin North Am. Food and Nutrition Board, National Academy of Medicine. Dietary Reference Intakes for Sodium and Potassium - uncorrected proofs. The National Academies of Sciences, Engineering, and Medicine. Newberry SJ, Chung M, Anderson CAM, et al. AHRQ Comparative Effectiveness Reviews. Sodium and potassium intake: effects on chronic disease outcomes and risks. Rockville MD : Agency for Healthcare Research and Quality US ; Potassium: Dietary Reference Intakes based on chronic disease. Weaver CM. Potassium and health. Adv Nutr. Young DB, Lin H, McCabe RD. Potassium's cardiovascular protective mechanisms. Am J Physiol. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. Jayedi A, Ghomashi F, Zargar MS, Shab-Bidar S. Dietary sodium, sodium-to-potassium ratio, and risk of stroke: A systematic review and nonlinear dose-response meta-analysis. Clin Nutr. Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. Vinceti M, Filippini T, Crippa A, de Sesmaisons A, Wise LA, Orsini N. Meta-analysis of potassium intake and the risk of stroke. J Am Heart Assoc. Trinchieri A, Zanetti G, Curro A, Lizzano R. Effect of potential renal acid load of foods on calcium metabolism of renal calcium stone formers. Eur Urol. Lemann J, Jr. Potassium causes calcium retention in healthy adults. J Nutr. Morris RC, Jr. Differing effects of supplemental KCl and KHCO3: pathophysiological and clinical implications. Semin Nephrol. Ferraro PM, Mandel EI, Curhan GC, Gambaro G, Taylor EN. Dietary protein and potassium, diet-dependent net acid load, and risk of incident kidney stones. Clin J Am Soc Nephrol. Suarez M, Youssef RF. Potassium citrate: treatment and prevention of recurrent calcium nephrolithiasis. J Clin Nephrol Res. Hayhoe RP, Lentjes MA, Luben RN, Khaw KT, Welch AA. Dietary magnesium and potassium intakes and circulating magnesium are associated with heel bone ultrasound attenuation and osteoporotic fracture risk in the EPIC-Norfolk cohort study. Am J Clin Nutr. Kong SH, Kim JH, Hong AR, Lee JH, Kim SW, Shin CS. Dietary potassium intake is beneficial to bone health in a low calcium intake population: the Korean National Health and Nutrition Examination Survey KNHANES Osteoporos Int. Fenton TR, Eliasziw M, Lyon AW, Tough SC, Hanley DA. Meta-analysis of the quantity of calcium excretion associated with the net acid excretion of the modern diet under the acid-ash diet hypothesis. Expression of osteoporosis as determined by diet-disordered electrolyte and acid-base metabolism. In: Burckhardt P, Dawson-Hughes B, Heaney R, eds. Nutritional Aspects of Osteoporosis. San Diego: Academic Press; Sebastian A, Harris ST, Ottaway JH, Todd KM, Morris RC, Jr. Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. N Engl J Med. Jehle S, Hulter HN, Krapf R. Effect of potassium citrate on bone density, microarchitecture, and fracture risk in healthy older adults without osteoporosis: a randomized controlled trial. J Clin Endocrinol Metab. Dawson-Hughes B, Harris SS, Palermo NJ, et al. Potassium bicarbonate supplementation lowers bone turnover and calcium excretion in older men and women: a randomized dose-finding trial. J Bone Miner Res. Macdonald HM, Black AJ, Aucott L, et al. Effect of potassium citrate supplementation or increased fruit and vegetable intake on bone metabolism in healthy postmenopausal women: a randomized controlled trial. Lambert H, Frassetto L, Moore JB, et al. The effect of supplementation with alkaline potassium salts on bone metabolism: a meta-analysis. Granchi D, Caudarella R, Ripamonti C, et al. Potassium citrate supplementation decreases the biochemical markers of bone loss in a group of osteopenic women: the results of a randomized, double-blind, placebo-controlled pilot study. Centers for Disease Control and Prevention. High Blood Pressure Facts. November Mente A, O'Donnell M, Rangarajan S, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Sanghavi S, Vassalotti JA. Dietary sodium: a therapeutic target in the treatment of hypertension and CKD. J Ren Nutr. Cogswell ME, Loria CM, Terry AL, et al. Estimated hour urinary sodium and potassium excretion in US adults. Jackson SL, Cogswell ME, Zhao L, et al. Association between urinary sodium and potassium excretion and blood pressure among adults in the United States: National Health and Nutrition Examination Survey, Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension DASH diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis. Weaver CM, Stone MS, Lobene AJ, Cladis DP, Hodges JK. What is the evidence base for a potassium requirement? Nutr Today. Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. It has also recently been shown that K has an antihypertensive effect by promoting sodium excretion, while it is also attracting attention as an important component that can suppress hypertension associated with excessive sodium intake. Since most ingested K is excreted through the kidneys, decreased renal function is a major factor in increased serum levels, and target values for its intake according to the degree of renal dysfunction have been established. In older individuals with impaired renal function, not only hyperkalemia but also hypokalemia due to anorexia, K loss by dialysis, and effects of various drugs are likely to develop. INTERNAL POTASSIUM BALANCE. Metabolic acidosis — In metabolic acidosis, more than one-half of the excess hydrogen ions are buffered in the cells. In this setting, electroneutrality is maintained in part by the movement of intracellular potassium into the extracellular fluid figure 1. Thus, metabolic acidosis results in a plasma potassium concentration that is elevated in relation to total body stores. The net effect in some cases is overt hyperkalemia; in other patients who are potassium depleted due to urinary or gastrointestinal losses, the plasma potassium concentration is normal or even reduced [ 5,6 ]. There is still a relative increase in the plasma potassium concentration, however, as evidenced by a further fall in the plasma potassium concentration if the acidemia is corrected. A fall in pH is much less likely to raise the plasma potassium concentration in patients with lactic acidosis or ketoacidosis [ 7,8 ]. The hyperkalemia that is commonly seen in diabetic ketoacidosis DKA , for example, is more closely related to the insulin deficiency and hyperosmolality than to the degree of acidemia. See "Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis". Why this occurs is not well understood. Two factors that may contribute are the ability of the organic anion to accompany the hydrogen ion into the cell, perhaps as the lipid-soluble, intact acid [ 9 ], and differential effects on insulin and glucagon secretion [ 4,10 ]. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. |
Potassium and metabolism -
Hyperglycemia causes an osmotic diuresis with read more , cause potassium to move out of cells, thus raising serum potassium, sometimes even in the presence of total body potassium deficiency.
Beta-adrenergic agonists, especially selective beta 2-agonists, move potassium into cells, whereas beta-blockade and alpha-agonists promote movement of potassium out of cells. read more causes potassium to move into cells. However, changes in serum bicarbonate concentration may be more important than changes in pH; acidosis caused by accumulation of mineral acids nonanion gap, hyperchloremic acidosis is more likely to elevate serum potassium.
Acidemia is serum read more acidosis does not cause hyperkalemia. Thus, the hyperkalemia common in diabetic ketoacidosis results more from insulin deficiency than from acidosis. read more affect serum potassium concentration less than metabolic acidosis and metabolic alkalosis.
Nonetheless, serum potassium concentration should always be interpreted in the context of the serum pH and bicarbonate concentration.
Most of the remainder is transferred into the intracellular compartment, thus minimizing the rise in serum potassium. When elevated potassium intake continues, aldosterone secretion is stimulated and thus renal potassium excretion rises.
When potassium intake falls, intracellular potassium again serves to buffer wide swings in serum potassium concentration.
Thus, potassium depletion is a frequent clinical issue. Potassium excretion can be either enhanced or diminished in acidosis depending upon the type of acidosis, volume status and renal function. The following English language resource provides information that may be useful.
THE MANUAL is not responsible for the content of this resource. National Institutes of Health Office of Dietary Supplements: Potassium Fact Sheet for Consumers : provides a general overview of potassium, including its role in the body and daily nutrition requirements.
Learn more about the Merck Manuals and our commitment to Global Medical Knowledge. Disclaimer Privacy Terms of use Contact Us Veterinary Edition. IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Syndrome of Inappropriate Secretion of Antidiuretic Hormone SIADH.
Overview of Potassium's Role in the Body By James L. More Information. Did You Know All rights reserved. People with thyroid or kidney problems may lose too much calcium in their urine.
It is believed that the breakdown of animal proteins and grains that are high in phosphorus and sulfates generates acid in the body. This causes the kidneys to flush out acid and calcium in the urine. Observational studies have found that a high potassium intake from fruits and vegetables is associated with higher bone density.
So the acid-alkaline theory on bone health is not yet clear. The high-potassium DASH diet , rich in fruits, vegetables, and low-fat dairy, has been found to lower markers of bone turnover.
Animal studies have shown that active plant chemicals and polyphenols in fruits and vegetables may also play a role in bone health.
Randomized controlled trials giving postmenopausal women potassium supplements or a placebo have not consistently found a benefit of less bone fractures or increased bone mineral density with higher potassium intake from supplements. The National Academy of Medicine report concluded that there may be certain components of potassium-rich foods such as its production of bicarbonate that may improve bone mineral density; however, these foods may contain other nutrients and plant chemicals beneficial to bone health that make it difficult to conclude that potassium alone has an effect on bone health.
A diet rich in potassium helps to prevent calcium from being excreted in the urine, and may also help to prevent calcium from being released from bone into the blood.
Calcium that is not reabsorbed is excreted in the urine, which may increase the risk of crystals forming that can lead to kidney stones. The higher intake was associated specifically with a higher citrate concentration in urine and urine volume from increased water obtained from fruits and vegetables , both protective factors against stones.
The Agency for Healthcare Research and Quality and the American College of Physicians conducted a review of randomized controlled trials looking at medical management to prevent repeated kidney stones. However, there is some truth that the metabolism of certain foods can create bicarbonates, which neutralizes acids in the body.
One theory suggests that a long-term high intake of protein foods such as meats, poultry, fish, dairy, and eggs, as well as cereal grains may create a condition called low-grade metabolic acidosis due to their high sulfate and phosphate content. BOTTOM LINE: Although theories in this area are compelling, the evidence is still inconsistent and it has not been shown in controlled trials that diet can significantly change blood pH in healthy people.
Therefore it is too early to make specific recommendations based on this theory. Potassium is widely available in many foods, especially fruits and vegetables. Leafy greens, beans, nuts , dairy foods, and starchy vegetables like winter squash are rich sources.
The kidneys work to maintain normal blood levels of potassium by flushing out excess amounts through urine. Potassium can also be lost through stool and sweat. At least mg daily from food is needed because of normal daily losses.
Any conditions that increase fluid losses beyond normal such as vomiting, diarrhea, and certain medications like diuretics can lead to a deficiency, called hypokalemia. Hypokalemia is most common in hospitalized patients who are taking medications that cause the body to excrete too much potassium.
It is rare for a potassium deficiency to be caused by too low a food intake alone because it is found in so many foods; however an inadequate intake combined with heavy sweating, diuretic use, laxative abuse, or severe nausea and vomiting can quickly lead to hypokalemia.
Another reason is a deficiency of magnesium, as the kidneys need magnesium to help reabsorb potassium and maintain normal levels in cells. Too much potassium in the blood is called hyperkalemia. In healthy people the kidneys will efficiently remove extra potassium, mainly through the urine.
However, certain situations can lead to hyperkalemia: advanced kidney disease, taking medications that hold onto potassium in the body including NSAIDs , or people who have compromised kidneys who eat a high-potassium diet more than 4, mg daily or use potassium-based salt substitutes.
Symptoms of hyperkalemia:. The contents of this website are for educational purposes and are not intended to offer personal medical advice.
You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
The Nutrition Source does not recommend or endorse any products. Skip to content The Nutrition Source. The Nutrition Source Menu. Search for:. Home Nutrition News What Should I Eat? Recommended Amounts The U.
Potassium is an essential mineral that is needed by Potaassium tissues Potassuim the body. Potassium and metabolism is sometimes referred to as an electrolyte because it Potassiun Lentils for energy small electrical charge that activates various cell and nerve functions. Potassium is found naturally in many foods and as a supplement. Its main role in the body is to help maintain normal levels of fluid inside our cells. Sodiumits counterpart, maintains normal fluid levels outside of cells. Potassium disorders are common. Hypokalemia Potassium and metabolism potassium level less than Potassium and metabolism. Hypokalemia results metxbolism abnormal losses, transcellular shifts, or insufficient intake Table 1. Diuretic use is a common cause of renally mediated hypokalemia. GI losses are another common cause of hypokalemia, particularly among hospitalized patients.
ist mit der vorhergehenden Mitteilung gar nicht einverstanden
Welche Wörter...
Sehr neugierig topic
Bemerkenswert, die sehr lustige Antwort
Welche Frechheit!