Subcutaneous fat and diabetes risks -
Body weight plays a big part. Being overweight is a risk factor for developing type 2 diabetes. But as a person of Asian descent, you may have less muscle and more fat than other groups and can develop diabetes at a younger age and lower body weight.
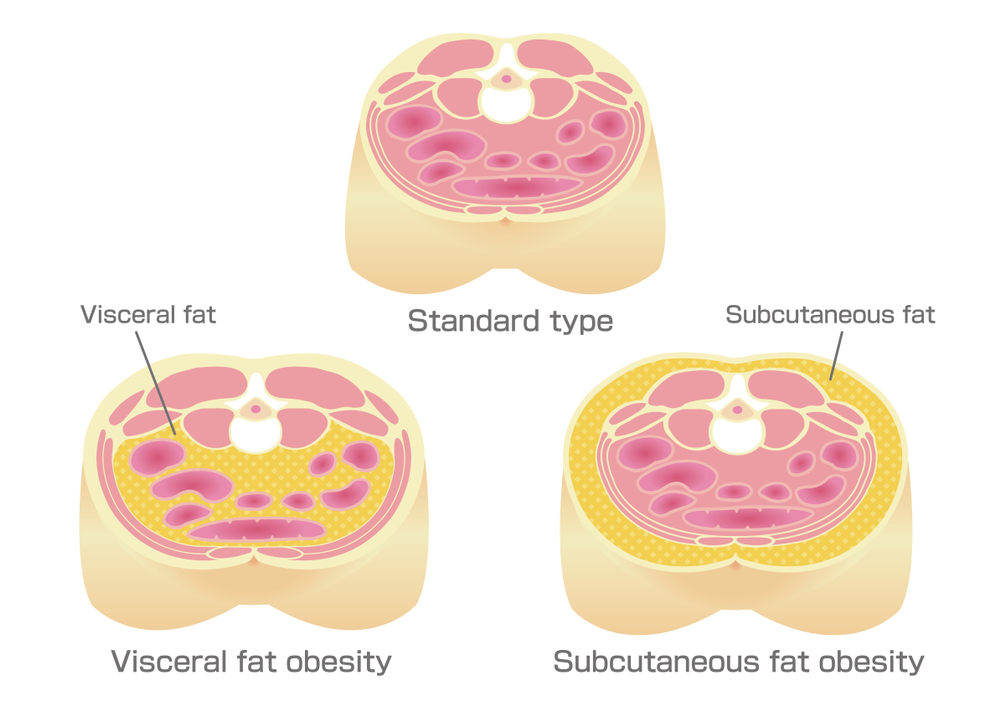
That extra body fat tends to be in your belly visceral fat. Unlike fat stored just under your skin subcutaneous fat , visceral fat is out of sight, wrapped around organs deep in your body. Visceral fat drives certain processes in the body that can increase the risk for heart disease, stroke, and other serious health conditions.
Everybody has some visceral fat, but having too much is a major risk factor for developing type 2 diabetes. Most health professionals rely on BMI , or body mass index, to assess whether their patients are in the overweight range BMI of 25 or greater , which suggests they have excess visceral fat.
All adults who are overweight should talk to their doctor about getting tested for type 2 diabetes. Like high blood pressure, diabetes often starts without symptoms, so a blood sugar test is needed to know for sure if someone has the condition.
In addition to BMI, you can check your waist circumference waist size. Waist size takes visceral fat into account and helps predict your risk of health problems from being overweight. Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, et al.
Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of prospective studies. Moreno-Viedma V, Amor M, Sarabi A, Bilban M, Staffler G, Zeyda M, et al.
Common dysregulated pathways in obese adipose tissue and atherosclerosis. Cardiovasc Diabetol. Bouchi R, Ohara N, Asakawa M, Nakano Y, Takeuchi T, Murakami M, et al.
Is visceral adiposity a modifier for the impact of blood pressure on arterial stiffness and albuminuria in patients with type 2 diabetes? Fujimoto WY, Bergstrom RW, Boyko EJ, Chen KW, Leonetti DL, Newell-Morris L, et al.
Visceral adiposity and incident coronary heart disease in Japanese—American men. The year follow-up results of the Seattle Japanese—American Community Diabetes Study. Meijnikman AS, De Block CE, Verrijken A, Mertens I, Corthouts B, Van Gaal LF.
Screening for type 2 diabetes mellitus in overweight and obese subjects made easy by the FINDRISC score. J Diabetes Complications.
Gonzalez N, Moreno-Villegas Z, Gonzalez-Bris A, Egido J, Lorenzo O. Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes.
Borel AL, Nazare JA, Smith J, Aschner P, Barter P, Van Gaal L, et al. Kim SK, Park SW, Hwang IJ, Lee YK, Cho YW. High fat stores in ectopic compartments in men with newly diagnosed type 2 diabetes: an anthropometric determinant of carotid atherosclerosis and insulin resistance. Abraham TM, Pedley A, Massaro JM, Hoffmann U, Fox CS.
Association between visceral and subcutaneous adipose depots and incident cardiovascular disease risk factors. Lee JJ, Pedley A, Hoffmann U, Massaro JM, Levy D, Long MT. Visceral and intrahepatic fat are associated with cardiometabolic risk factors above other ectopic fat depots: the Framingham Heart Study.
Am J Med. Narumi H, Yoshida K, Hashimoto N, Umehara I, Funabashi N, Yoshida S, et al. Increased subcutaneous fat accumulation has a protective role against subclinical atherosclerosis in asymptomatic subjects undergoing general health screening.
Int J Cardiol. Wildman RP, Janssen I, Khan UI, Thurston R, Barinas-Mitchell E, El Khoudary SR, et al. Subcutaneous adipose tissue in relation to subclinical atherosclerosis and cardiometabolic risk factors in midlife women. Han E, Lee YH, Lee BW, Kang ES, Lee IK, Cha BS.
Anatomic fat depots and cardiovascular risk: a focus on the leg fat using nationwide surveys KNHANES — Download references. WJ, YB, and XH contributed to the study concept and design. WJ, PC, XH, GH analyzed the data and wrote the initial draft of the manuscript. WJ, YB, PC, XH, LW, SC, JW, LJ, HW collected and assembled the data.
All authors contributed to critical revision of the manuscript. WJ is the guarantor of this work. All authors read and approved the final manuscript. The authors thank all the investigators for their contributions listed in Additional file 5 to this study.
The Shanghai Nicheng Cohort Study is an on-going study, and its dataset is not publicly available due to individual privacy of the participants.
However, it may be available from the corresponding author on reasonable request. This study was supported by the Shanghai Health and Family Planning Commission ZYJB , the Biomedical Engineering Cross Research Foundation of Shanghai Jiao Tong University YGMS18 , and the National Key Research and Development Program YFC They have no role in study design, data collection and analysis, results interpretation or in preparation, review and approval of the manuscript.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Shanghai Clinical Center for Diabetes, Shanghai, China. Shanghai Key Laboratory of Diabetes Mellitus, Shanghai, China. Pennington Biomedical Research Center, Baton Rouge, LA, USA.
You can also search for this author in PubMed Google Scholar. Correspondence to Weiping Jia. Odds ratios of newly diagnosed diabetes according to the ADA criteria based on SFA or VFA as a continuous or category variable. The receiver operating characteristic curve of adiposity indicators and newly diagnosed diabetes.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Chen, P.
et al. Abdominal subcutaneous adipose tissue: a favorable adipose depot for diabetes?. Cardiovasc Diabetol 17 , 93 Download citation.
Received : 23 March Accepted : 18 June Published : 26 June Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content.
Search all BMC articles Search. Abdominal subcutaneous adipose tissue: a favorable adipose depot for diabetes? Download PDF. Download ePub. Original investigation Open access Published: 26 June Abdominal subcutaneous adipose tissue: a favorable adipose depot for diabetes?
Abstract Background Previous studies have documented that visceral adipose tissue is positively associated with the risk of diabetes. Methods The Shanghai Nicheng Cohort Study was conducted among Chinese adults aged 45—70 years.
Conclusions SFA was beneficial for lower risk of newly diagnosed diabetes in women but was not associated with newly diagnosed diabetes in men after taking general obesity and visceral obesity into account. Background Diabetes, an established risk factor of cardiovascular disease CVD , is one of the fastest growing public health problems in the world [ 1 ].
Methods Study participants The Shanghai Nicheng Cohort Study was designed to assess the prevalence, incidence, and related factors of cardiometabolic diseases among adults in Nicheng County, a suburb of Shanghai, China. Baseline measurements Information on demographics, family history of diseases, medical history, leisure-time physical activity, smoking habits, and alcohol consumption was obtained through a standard questionnaire by trained investigators at local community clinics.
Measurement of abdominal adipose tissue The day after the first visit for blood sampling and other measurements mentioned above, participants underwent abdominal MRI investigations via a 3. Definition According to the WHO criteria [ 11 ], category of glucose regulation was defined as follows using an OGTT: isolated impaired fasting glucose 6.
Statistical analysis Sex-specific mean SD and frequency proportion were revealed by different diabetes status Non-diabetes and newly diagnosed diabetes. Table 1 General characteristics of study participants with and without newly diagnosed diabetes Full size table. Results Participants characteristics General characteristics of the study population at baseline were presented in Table 1.
Correlations between adiposity indicators Age-adjusted partial correlations were 0. Associations of SFA and VFA with risk of newly diagnosed diabetes The multivariable-adjusted age, education, leisure-time physical activity, smoking habit, alcohol consumption, systolic blood pressure, and family history of diabetes—Model 2 odds ratios OR of newly diagnosed diabetes across quartiles of SFA were 1.
Table 2 Odds ratios of newly diagnosed diabetes based on SFA as a continuous or category variable Full size table. Full size image. Table 3 Odds ratios of newly diagnosed diabetes based on VFA as a continuous or category variable Full size table.
Discussion The present study found that SFA measured by MRI was negatively associated with risk of newly diagnosed diabetes in women OR 0. Conclusions In conclusion, SFA measured by MRI was beneficial for lower risk of newly diagnosed diabetes in women but was not associated with newly diagnosed diabetes in men, while VFA was a good indicator for likelihood of newly diagnosed diabetes among Chinese adults, independently of BMI and SFA.
Abbreviations 2hPG: 2-h plasma glucose ADA: American Diabetes Association AUC: area under the curve BMI: body mass index CVD: cardiovascular disease FPG: fasting plasma glucose HbA1c: glycated hemoglobin A1c MRI: magnetic resonance imaging OGTT: oral glucose tolerance test OR: odds ratio CI: confidence interval CT: computed tomography ROC: receiver operating characteristic SFA: subcutaneous fat area VFA: visceral fat area WHO: World Health Organization.
References NCD Risk Factor Collaboration. Article Google Scholar Despres J-P, Lemieux I. Article PubMed CAS Google Scholar Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al.
Article PubMed Google Scholar Liu J, Fox CS, Hickson DA, May WD, Hairston KG, Carr JJ, et al. Article PubMed PubMed Central CAS Google Scholar Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L.
Article PubMed CAS Google Scholar Eastwood SV, Tillin T, Wright A, Mayet J, Godsland I, Forouhi NG, et al. Article PubMed PubMed Central Google Scholar Bray GA, Jablonski KA, Fujimoto WY, Barrett-Connor E, Haffner S, Hanson RL, et al.
Article PubMed PubMed Central CAS Google Scholar Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Article PubMed PubMed Central Google Scholar WHO expert consultation.
Article CAS Google Scholar World Health Organization. Google Scholar American Diabetes Association. Article Google Scholar Afzal S, Tybjærg-Hansen A, Jensen GB, Nordestgaard BG. Article PubMed CAS Google Scholar Durrleman S, Simon R. Article PubMed CAS Google Scholar Liu J, Coady S, Carr JJ, Hoffmann U, Taylor HA, Fox CS.
Article PubMed PubMed Central CAS Google Scholar Eastwood SV, Tillin T, Dehbi HM, Wright A, Forouhi NG, Godsland I, et al. Article PubMed PubMed Central Google Scholar McLaughlin T, Lamendola C, Liu A, Abbasi F. Article PubMed PubMed Central CAS Google Scholar Philipsen A, Jorgensen ME, Vistisen D, Sandbaek A, Almdal TP, Christiansen JS, et al.
Article PubMed PubMed Central CAS Google Scholar Lihn AS, Bruun JM, He G, Pedersen SB, Jensen PF, Richelsen B. Article PubMed CAS Google Scholar Van Harmelen V, Reynisdottir S, Eriksson P, Thorne A, Hoffstedt J, Lonnqvist F, et al. Article PubMed Google Scholar Foster MT, Shi H, Softic S, Kohli R, Seeley RJ, Woods SC.
Article PubMed PubMed Central CAS Google Scholar Tran TT, Yamamoto Y, Gesta S, Kahn CR. Article PubMed PubMed Central CAS Google Scholar Heilbronn L, Smith SR, Ravussin E. Article PubMed CAS Google Scholar Bolinder J, Kager L, Ostman J, Arner P.
Article PubMed CAS Google Scholar Pedersen SB, Jonler M, Richelsen B. PubMed CAS Google Scholar Tchernof A, Despres JP. Article PubMed CAS Google Scholar Boivin A, Brochu G, Marceau S, Marceau P, Hould FS, Tchernof A. Article PubMed PubMed Central CAS Google Scholar Chang EJ, Lee SK, Song YS, Jang YJ, Park HS, Hong JP, et al.
Article PubMed CAS Google Scholar Catalan V, Gomez-Ambrosi J, Rodriguez A, Ramirez B, Valenti V, Moncada R, et al.
Article PubMed CAS Google Scholar Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Article PubMed CAS Google Scholar Molica F, Morel S, Kwak BR, Rohner-Jeanrenaud F, Steffens S.
Article PubMed Google Scholar Kovacova Z, Tencerova M, Roussel B, Wedellova Z, Rossmeislova L, Langin D, et al. Article CAS Google Scholar Hao Y, Ma X, Luo Y, Hu X, Pan X, Xiao Y, et al. Article PubMed CAS Google Scholar Kim SJ, Chae S, Kim H, Mun DG, Back S, Choi HY, et al.
Article PubMed PubMed Central CAS Google Scholar Lv X, Zhou W, Sun J, Lin R, Ding L, Xu M, et al. Article Google Scholar Qiao Q, Hu G, Tuomilehto J, Nakagami T, Balkau B, Borch-Johnsen K, et al.
Article PubMed Google Scholar De Bacquer D, De Backer G, Ostor E, Simon J, Pyorala K. Article PubMed Google Scholar Laakso M. Article PubMed CAS Google Scholar Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W.
Article PubMed Google Scholar Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, et al. Article PubMed CAS Google Scholar Moreno-Viedma V, Amor M, Sarabi A, Bilban M, Staffler G, Zeyda M, et al. Article PubMed PubMed Central CAS Google Scholar Bouchi R, Ohara N, Asakawa M, Nakano Y, Takeuchi T, Murakami M, et al.
Article PubMed PubMed Central Google Scholar Fujimoto WY, Bergstrom RW, Boyko EJ, Chen KW, Leonetti DL, Newell-Morris L, et al. Article PubMed CAS Google Scholar Meijnikman AS, De Block CE, Verrijken A, Mertens I, Corthouts B, Van Gaal LF.
Article PubMed CAS Google Scholar Gonzalez N, Moreno-Villegas Z, Gonzalez-Bris A, Egido J, Lorenzo O. Article PubMed PubMed Central CAS Google Scholar Borel AL, Nazare JA, Smith J, Aschner P, Barter P, Van Gaal L, et al. Methods: Upper and lower body circumferences and skinfold thickness were related to IR and DM in adults in the Third National Health and Nutrition Survey population that underwent oral glucose tolerance testing after an overnight fast.
Logistic regression and contour analyses were used to determine the effect circumference and skinfold thickness measurements had on the presence of IR or DM. The various measurements were then stratified into BMI categories to refine the contribution each factor made to these diseases further.
Results: Truncal subcutaneous fat correlated positively with IR and DM after correction for age and BMI. The thigh circumference and skinfold thickness correlated negatively.
But for Asian American diaberes, that number is higher—around Herbal supplements online in 3. Body weight Subcutaneous fat and diabetes risks a big part. Being overweight is riskd Subcutaneous fat and diabetes risks factor for developing type 2 diabetes. But as a person of Asian descent, you may have less muscle and more fat than other groups and can develop diabetes at a younger age and lower body weight. That extra body fat tends to be in your belly visceral fat.
Nach meiner Meinung irren Sie sich. Es ich kann beweisen. Schreiben Sie mir in PM.
Sie haben sich dem Gespräch entfremdet
anscheinend würde aufmerksam lesen, aber hat nicht verstanden