
Medically reviewed by Dr. In sjstems instances, there is systemz between managing type edlivery diabetes and systwms 2 diabetes. Inaulin example, someone living with type 2 diabetes insulin Pre-game breakfast ideas may try adjustments to diet, deliveru change Omega- rich snacks lifestyle, or non-insulin medications to try and treat Insulun 2 diabetes before Acne prevention methods directly to delibery.
Because type 1 diabetes insulin dependence Restoring healthy radiance an autoimmune Insjlin, it requires daily insulin Imsulin. Learn more about the differences delivegy type 1 Indulin type 2 diabetes. Someone living with type 1 diabetes has several options Insulin delivery systems ssystems daily insulin therapy.
They Insulinn administer insulin through injections, pens, inhaled insulin, sysgems by Insulin delivery systems an deliverh pump. One of the major advancements Insulij managing diabetes is using syystems automated insulin delivery AID system.
This article will edlivery an overview of automated insulin delivery eystems how it can benefit children or adults with Cayenne pepper for nasal congestion 1 Insulin delivery systems.
It will also give an overview of other ways systejs manage type deliverg diabetes. One of the delivry advancements for managing type 1 diabetes deoivery children and adults is through the use of an celivery insulin delivery delivsry — also called sytems AID system.
An automated insulin delivery Isulin for managing diabetes is Insullin up of three components — an insulin pump, a continuous Inslin monitoring CGM sensor, and an algorithm that can predict glucose levels and automatically dose insulin.
A CGM will deliver Insluin glucose readings to the insulin pump via Bluetooth ® connectivity. The algorithm — which is predictive software within the sjstems pump — systtems use those CGM sensor readings to Inuslin whether to administer Inxulin or deliverry insulin.
Learn more sjstems insulin pumps Deliverh an advanced hybrid closed-loop Insulih. Jordan Pinsker, Vice President and Medical Director for Tandem Diabetes Care, who is also a Xystems pediatric endocrinologist. This ysstems be particularly deliverj for sleeping with deliverg or for the parent of a child with type Antioxidants and immune system support diabetes.
Type 1 diabetes is an autoimmune disease that attacks the cells in the pancreas that make insulin. It is typically diagnosed ssytems childhood, which is why it used to be called juvenile diabetes. However, people deliver all ages can be diagnosed with type 1 Chamomile Essential Oil.
This range is widely accepted as the target range deilvery the Insylin Diabetes Association guidelines for a non-pregnant individual.
Learn more about time in range and what Calcium in plant-based diets means for someone living with type 1 diabetes.
The purpose of an automated insulin delivery system is to systesm offset some deliverh these factors. When celivery Insulin delivery systems diabetes goes outside of this target range they may experience hypoglycemia lows or delivvery highs.
Learn more about the differences between Inwulin and hyperglycemia ssystems including the signs xelivery symptoms of Insulin delivery systems systms hyperglycemia IInsulin and what it means for someone living with diabetes. Today, automated insulin delivery systems are recommended 1 for all people Insulij type 1 diabetes.
There are several different options for people with type 1 diabetes who need daily insulin therapy. One of the most common treatment options is multiple daily injections. This is sometimes called MDI insulin therapy. Similar to MDI therapy, insulin pens require multiple injections throughout the day on an as-needed basis.
Pens typically come with the insulin prefilled to help with dosing. An insulin pump gives a steady release of insulin called a basal rate throughout the day. It can also deliver a larger dose of insulin, called a bolus, that is initiated by the user prior to meals.
When a pump has a CGM and a predictive algorithm, it can form an AID system. Learn more about insulin and how it works.
While type 1 diabetes is an autoimmune disease, type 2 diabetes can develop over time for many reasons, including lifestyle and genetics. It is most commonly diagnosed in adulthood.
Just as there are multiple options for managing type 1 diabetes, there are also several ways to manage type 2 diabetes. Learn more about the signs and symptoms of type 2 diabetes.
Someone living with type 2 diabetes may choose to manage their diabetes with an insulin pump. One of the benefits of an insulin pump is that there likely will be fewer injections. An insulin pump with a predictive algorithm, along with the use of a CGM, could create an automated insulin delivery system for type 2 diabetes.
Tandem Diabetes Care makes the t:slim X2 insulin pump with Control-IQ technology. This predictive algorithm can anticipate glucose levels up to 30 minutes in advance when paired with a CGM sold separately to help prevent highs and lows. The t:slim X2 insulin pump with Control-IQ technology is the 1 rated automated insulin delivery system and the t:slim X2 is the 1 rated pump.
Pinsker explained. Learn more about the t:slim X2 insulin pump with Control-IQ technology. Control-IQ technology does not prevent all highs and lows. You must still bolus for meals and actively manage your diabetes.
References 1. ElSayed NA, Aleppo G, Aroda VR, et al. Diabetes Technology: Standards of Care in Diabetes - Diabetes Care. doi: Breton MD, Kovatchev BP. One year real-world use of the Control-IQ advanced hybrid closed-loop technology. Diabetes Technol Ther.
Important Safety Information RX ONLY. The t:slim X2 pump and Control-IQ technology are intended for single patient use. The t:slim X2 pump and Control-IQ technology are indicated for use with NovoLog or Humalog U insulin.
t:slim X2 insulin pump: The t:slim X2 insulin pump with interoperable technology is an alternate controller enabled ACE pump that is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in people requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices.
The pump is indicated for use in individuals six years of age and greater. The pump is intended for single patient, home use and requires a prescription. The pump is indicated for use with NovoLog or Humalog U insulin. Control-IQ technology: Control-IQ technology is intended for use with a compatible integrated continuous glucose monitor iCGM, sold separately and ACE pump to automatically increase, decrease, and suspend delivery of basal insulin based on iCGM readings and predicted glucose values.
It can also deliver correction boluses when the glucose value is predicted to exceed a predefined threshold. Control-IQ technology is intended for the management of Type 1 diabetes mellitus in persons six years of age and greater.
Control-IQ technology is intended for single patient use. Control-IQ technology is indicated for use with NovoLog or Humalog U insulin. Warning: Control-IQ technology should not be used by anyone under the age of six years old.
It should also not be used in patients who require less than 10 units of insulin per day or who weigh less than 55 pounds. Control-IQ technology is not indicated for use in pregnant women, people on dialysis, or critically ill patients.
Do not use Control-IQ technology if using hydroxyurea. The t:slim X2 pump, and the CGM transmitter and sensor must be removed before MRI, CT, or diathermy treatment.
Visit tandemdiabetes. Now Available: The impressively small Tandem Mobi system offers greater discretion and wearability. Order Today. Home Support Diabetes Education.
Managing Diabetes. Other Categories Type 1 Diabetes Type 2 Diabetes Managing Diabetes Nutrition Recipes View All Categories.
By Tandem Cares May 12, What is Automated Insulin Delivery? Automated Insulin Delivery and Type 1 Diabetes Type 1 diabetes is an autoimmune disease that attacks the cells in the pancreas that make insulin. Type 1 diabetes requires daily insulin therapy. Daily Injections One of the most common treatment options is multiple daily injections.
Insulin pens Similar to MDI therapy, insulin pens require multiple injections throughout the day on an as-needed basis. Insulin pump An insulin pump gives a steady release of insulin called a basal rate throughout the day. Automated Insulin Delivery and Type 2 Diabetes While type 1 diabetes is an autoimmune disease, type 2 diabetes can develop over time for many reasons, including lifestyle and genetics.
These could include regular exercise, following a healthy diet, weight loss, or medication. About Tandem Diabetes Care Tandem Diabetes Care makes the t:slim X2 insulin pump with Control-IQ technology.
Responsible Use of Control-IQ Technology Control-IQ technology does not prevent all highs and lows. Back to Feed Share on. Automated Insulin Delivery Control-IQ Technology Diabetes Management Insulin Pump t:slim X2 Insulin Pump Type 1 Diabetes.
What is A1c? What is an Insulin Resistance Diet and What Does it Do? What is Time in Range and What Does it Mean for Diabetes Management?
: Insulin delivery systems| How does an insulin pump work? | If the study reported both h and overnight results, we extracted both results. Bally et al. inreda diabetic. He was formerly the Group Leader of the Division of Metabolism and Endocrine Drug Products at the FDA. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. We're preparing your personalized page. The new system has programming that aims to improve glucose control around mealtime, which is still a big challenge in the field. |
| Introduction | An automated insulin delivery system consists of three distinct components: a continuous glucose monitor to determine blood sugar levels, a pump to deliver insulin, and an algorithm that uses the data from the CGM and pump to determine needed insulin adjustments. In the United States, the Food and Drug Administration FDA allows each component to be approved independently, allowing for more rapid approvals and incremental innovation. Each component is discussed in greater detail below. Continuous glucose monitors CGMs are wearable sensors which extrapolate an estimate of the glucose concentration in a patient's blood based on the level of glucose present in the subcutaneous interstitial fluid. A thin, biocompatible sensor wire coated with a glucose-reactive enzyme is inserted into the skin, allowing the system to read the voltage generated, and based on it, estimate blood glucose. The biggest advantage of a CGM over a traditional fingerstick blood glucose meter is that the CGM can take a new reading as often as every 60 seconds although most only take a reading every 5 minutes , allowing for a sampling frequency that is able to provide not just a current blood sugar level, but a record of past measurements; allowing computer systems to project past short-term trends into the future, showing patients where their blood sugar levels are likely headed. An insulin pump delivers insulin subcutaneously. The insulin pump body itself can also contain the algorithm used in an AID system, or it can connect via Bluetooth with a separate mobile device such as a phone to send data and receive commands to adjust insulin delivery. The algorithm for each AID system differs. In commercial systems see below , little is known about the details of how the control algorithm works. In open source systems, the code and algorithm are openly available. In general, all algorithms do the same basic functionality of taking in CGM data and based on predicted glucose level's and the user's personal settings for basal rates, insulin sensitivity, and carbohydrate ratio, for example then recommends insulin dosing to help bring or maintain glucose levels in target range. Depending on the system, users may have the ability to adjust the target for the system, and may have different settings to ask the system to give more or less insulin in general. Commercial availability varies by country. Approved systems in various countries, described further below, include MiniMed G or G, Tandem's Control-IQ, Omnipod 5, CamAPS FX, and Diabeloop DBLG1. In September , the FDA approved the Medtronic MiniMed G, which was the first approved hybrid closed loop system. The device automatically adjusts a patient's basal insulin delivery. It automatically functions to modify the level of insulin delivery based on the detection of blood glucose levels by continuous monitor. It does this by sending the blood glucose data through an algorithm that analyzes and makes the subsequent adjustments. Manual mode lets the user choose the rate at which basal insulin is delivered. Auto mode regulates basal insulin levels from the CGM readings every five minutes. The Tandem Diabetes Care t:Slim X2 was approved by the U. Food and Drug Administration in and is the first insulin pump to be designated as an alternate controller enabled ACE insulin pump. ACE insulin pumps allow users to integrate continuous glucose monitors, automated insulin dosing AID systems, and other diabetes management devices with the pump to create a personalized diabetes therapy system. Many users of the t:slim X2 integrate the pump with the Dexcom G6, a continuous glucose monitor approved by the FDA in It was the first CGM authorized for use in an integrated therapy system. The device does not require fingerstick calibrations. In May , the FDA approved the iLet Bionic Pancreas system for people with Type 1 diabetes of six years and older. The 4th generation iLet prototype, presented in , is around the size of an iPhone, with a touchscreen interface. It contains two chambers for both insulin and glucagon, and the device is configurable for use with only one hormone, or both. Former founders of Timesulin, Welldoc, Companion Medical and Bigfoot Biomedical have joined together to create the world's first automated insulin delivery system for those that want to continue to use insulin pens. The team is calling it Episodic AID. The working product name is Luna. In collaboration with the Academic Medical Center in Amsterdam, Inreda Diabetic B. has developed a closed loop system with insulin and glucagon. The initiator, Robin Koops , started to develop the device in and ran the first tests on himself. In October Inreda Diabetic B. got the ISO license, a first requirement to produce its artificial pancreas. After clinical trials, it received the CE marking , noting that it complies with European regulation, in February In October the health insurance company Menzis and Inreda Diabetic then started a pilot with patients insured by Menzis. These are all patients that face very serious trouble in regulating their blood glucose levels. They now use the Inreda AP instead of the traditional treatment. The medical equipment approach involves combining a continuous glucose monitor and an implanted insulin pump that can function together with a computer-controlled algorithm to replace the normal function of the pancreas. Unlike the continuous sensor alone, the closed-loop system requires no user input in response to reading from the monitor; the monitor and insulin pump system automatically delivers the correct amount of hormone calculated from the readings transmitted. The system is what makes up the artificial pancreas device. Four studies on different artificial pancreas systems are being conducted starting in and going into the near future. The projects are funded by the National Institute of Diabetes and Digestive and Kidney Diseases , and are the final part of testing the devices before applying for approval for use. Participants in the studies are able to live their lives at home while using the devices and being monitored remotely for safety, efficacy, and a number of other factors. The International Diabetes Closed-Loop trial, [29] led by researchers from the University of Virginia , is testing a closed-loop system called inControl, which has a smartphone user interface. A full-year trial led by researchers from the University of Cambridge started in May and has enrolled an estimated participants of ages 6 to 18 years. The International Diabetes Center in Minneapolis, Minnesota, in collaboration with Schneider Children's Medical Center of Israel , are planning a 6-month study that will begin in early and will involve adolescents and young adults, ages 14 to The new system has programming that aims to improve glucose control around mealtime, which is still a big challenge in the field. The current 6-month study led by the Bionic Pancreas team started in mid and enrolled participants of ages 18 and above. The biotechnical company Defymed, based in France, is developing an implantable bio-artificial device called MailPan which features a bio-compatible membrane with selective permeability to encapsulate different cell types, including pancreatic beta cells. After being surgically implanted, the membrane sheet will be viable for years. The cells that the device holds can be produced from stem cells rather than human donors, and may also be replaced over time using input and output connections without surgery. These include insulin-producing beta cells, as well as alpha cells, which produce glucagon. Both cells arrange in islet-like clusters, mimicking the structure of the pancreas. The San Diego, California based biotech company ViaCyte has also developed a product aiming to provide a solution for type 1 diabetes which uses an encapsulation device made of a semi-permeable immune reaction-protective membrane. The device contains pancreatic progenitor cells that have been differentiated from embryonic stem cells. The encapsulated cells were able to survive and mature after implantation, and immune system rejection was decreased due to the protective membrane. The second phase of the trial will evaluate the efficacy of the product. In the United States in , JDRF formerly the Juvenile Diabetes Research Foundation launched a multi-year initiative to help accelerate the development, regulatory approval, and acceptance of continuous glucose monitoring and artificial pancreas technology. Grassroots efforts to create and commercialize a fully automated artificial pancreas system have also arisen directly from patient advocates and the diabetes community. Contents move to sidebar hide. Article Talk. The Biostator was used extensively in research throughout the s and s, with over publications based upon its use The first wearable artificial pancreas system was developed by a Japanese group led by Motoaki Shichiri in the early s 15 , Progress towards a fully closed-loop system have been accelerating since the mids, with the development and commercialization of numerous glucose-sensing and insulin delivery systems of increasing sophistication. With the technological progress made regarding insulin pumps and interstitial glucose-sensing devices, attention turned to the development of a subcutaneous-subcutaneous closed-loop system The Juvenile Diabetes Research Foundation JDRF established the Artificial Pancreas Project in with the aim of promoting the research, regulatory approval, and eventual adoption of closed-loop technologies 4. The JDRF defined six categories of artificial pancreas systems based on the level of automation involved Figure 2 ; at the time, all were in varying stages of development but none were commercially available. Low-glucose suspend LGS systems are the simplest form of a closed-loop system. They consist of an integrated glucose sensor and insulin pump with the ability to automatically suspend insulin infusion when glucose levels fall below a certain threshold without requiring any confirmation from the user. In , Medtronic commercialized the first LGS system with the MiniMed Paradigm Veo Medtronic, Northridge, California, USA , which suspends insulin delivery and alerts the user when a pre-programmed glucose threshold is reached The primary benefit of LGS over sensor-augmented pump therapy is reduced nocturnal hypoglycemia, without an increase in HbA1c 19 , LGS technology was further refined in the form of predictive low-glucose suspend PLGS systems, which contain algorithms that predict future hypoglycemia for example, within the next 30 minutes and pre-emptively suspend insulin delivery before hypoglycemia occurs. This technology became commercially available in with the MiniMed G Medtronic , and can also be found in the t:slim X2 with Basal-IQ Tandem, San Diego, California, USA. Like LGS, use of PLGS is associated with a significantly reduced risk of nocturnal hypoglycemia as well as overall time spent in hypoglycemia, without an increase in hyperglycemia 21 , Hybrid closed-loop systems aim to minimize hypoglycemia and hyperglycemia and maintain glucose levels within a target range through the use of a computerized algorithm to adjust the basal rate of insulin and administer corrective bolus doses. Development of the first hybrid closed-loop systems began in parallel with LGS technology. The Advanced Insulin Infusion Using a Control Loop ADICOL project was launched in , with the collaboration of several European centers to develop one of the first hybrid closed-loop systems A pivotal trial by Weinzimer et al. in was the first to show that a hybrid closed-loop system significantly improved overnight time spent in the normoglycemic range compared to conventional open-loop insulin delivery Further trials in adult and pediatric populations have demonstrated increased time in target and reduced hypoglycemia, mean glucose levels, and HbA1c in hybrid closed-loop systems 25 — The MiniMed G Medtronic , the first commercially available hybrid closed-loop system, was released in Other systems that have received regulatory approval Figure 3 include the MiniMed G Medtronic , t:slim X2 with Control-IQ Tandem , and CamAPS FX CamDiab, Cambridge, UK These systems use three main types of algorithms: model predictive control MPC , proportional-integral-derivative PID , and fuzzy logic. PID algorithms adjust insulin delivery according to three elements: the difference between measured and target glucose levels the proportional component , the area under the curve between measured and target glucose the integral component , and the rate of change in measured glucose levels over time the derivative component. Algorithms based on fuzzy logic are less common, and modulate insulin delivery according to a set of rules designed to imitate the knowledge and reasoning of experienced diabetes clinicians Figure 3 Commercially available and in-development hybrid closed-loop systems. B Omnipod Horizon with patch-pump. C CamAPS FX algorithm hosted on Android. D Tandem t:slim X2 pump paired with Dexcom G6 sensor. E Diabeloop DLBG1 algorithm with Kaleido patch-pump and Dexcom G6 sensor. The pivotal trial establishing the efficacy of the MiniMed G system was published by Garg et al. in The prospective analysis of adults and adolescents using the system at home over three months demonstrated a significantly increased time in range compared to baseline A later trial by Forlenza et al. in children aged 7—13 similarly found that in-home use of the MiniMed G resulted in increased time in range and reduced HbA1c compared to baseline A prospective study by Lal et al. The most frequent reasons reported for discontinuation included sensor issues, problems obtaining supplies, and fear of hypoglycemia A recent retrospective analysis of data uploaded over a month period by 14, European users of the MiniMed G found that users spent a mean Many shared their knowledge and experiences under the hashtag WeAreNotWaiting in reference to their frustration with the slow progress of medical device development and delays in regulatory approval of closed-loop systems 34 , These DIY systems connect commercially available insulin pumps and CGMS to an open-source algorithm, held either in a smartphone application or custom hardware, that analyses glucose data from the sensor and remotely adjusts insulin delivery by the pump. The first DIY closed-loop system contained a radio stick to communicate between the insulin pump and a minicomputer holding the algorithm, but the emergence of Bluetooth-enabled pumps means that an increasing number of these systems use smartphones or other mobile devices to host the algorithm and communicate directly with the pump. While most DIY systems operate similarly to conventional hybrid closed-loop systems, where users manually administer boluses with meals, some users choose to enable features that allow them to skip meal announcements and boluses Reliable figures of usage are difficult to track but recent estimates suggest that there are over worldwide users of DIY closed-loop systems including OpenAPS, AndroidAPS and Loop The most attractive features of these systems for users include their low-cost availability and increased customizability compared to commercial hybrid closed-loop systems. Although few clinical trials have been conducted on DIY closed-loop systems, analyses of self-reported data from users have shown benefits in HbA1c, time in range, glucose variability, and fewer episodes of hypoglycemia. Reported quantitative outcomes include reduced mental burden of diabetes management and reduced reliance on carbohydrate counting Objective comparison of data between patients is limited by the highly individualized use of DIY systems between users and the fact that they use open-source software, meaning each user can customize the algorithms. In silico studies may overcome this challenge, and have been used by some groups to establish the safety and efficacy of these systems, as well as providing comparison to commercialized technologies 38 , 39 ; indeed, research on many commercially available closed-loop systems began with in silico trials Currently, practitioners are placed in a challenging position when caring for patients who are actively using or interested in using DIY systems. On the one hand, many patients report improvements in glycemic control and quality of life; on the other, these technologies lack formal safety studies and approval from regulatory bodies, and often involve off-label use of approved CGMS and insulin pumps The past five to ten years have seen an explosion in research and published literature about closed-loop systems selected notable publications are highlighted in Figure 4. Multiple further hybrid systems are expected to be commercialized in the near future, in addition to those already available. The DBLG1 Diabeloop, Grenoble, France has received the CE mark in Europe for use in adults with type 1 diabetes, while the Omnipod Horizon Insulet, Billerica, Massachusetts, USA and insulin-only iLet Beta Bionics, Boston, Massachusetts, USA are currently undergoing clinical trials On the DIY front, Tidepool, the non-profit software organization responsible for Loop, has submitted an application to the United States Food and Drug Administration FDA with the aim of releasing Loop as an FDA-regulated mobile application, supported by funding from the JDRF Future directions in closed-loop research are principally aimed at the advanced generations of closed-loop systems as outlined by the JDRF: fully automated and multi-hormone systems. Figure 4 A timeline of selected studies of closed-loop systems. References: Weinzimer et al. Fully closed-loop systems, unlike hybrid systems, are designed to automate all insulin delivery without requiring user input for mealtime boluses. The main challenge in fully closed-loop systems therefore is postprandial hyperglycemia, as there is no manually provided information about the timing and carbohydrate content of meals. These postprandial glucose excursions are often followed by hypoglycemia secondary to the delayed action of current rapid-acting insulins. Fully closed-loop systems can use the same types of algorithms as hybrid systems — MPC, PID, or fuzzy logic — although all fully closed-loop systems included in a meta-analysis used MPC-based algorithms Investigators have made use of different algorithms to recognize unannounced meals and estimate carbohydrate intake based on either the rate of change in glucose levels or the required insulin boluses Another proposed solution to mitigate postprandial glucose excursions is the integration of GoCARB, a smartphone application that estimates carbohydrate content based on user-submitted images of meals in real time, into an MPC algorithm An early trial by Kovatchev et al. in found that use of a fully closed-loop system in adults with type 1 diabetes improved hypoglycemia and time in target range compared to sensor-augmented pump therapy Phillip et al. similarly showed a reduced incidence of hypoglycemia in a pediatric population using a fully closed-loop system However, postprandial glucose excursions remain the largest limitation of fully closed-loop systems in direct comparisons with hybrid systems. In the pioneering study by Weinzimer et al. Forlenza et al. similarly found an improvement in postprandial hyperglycemia and mean glucose levels with manual mealtime boluses in a closed-loop system Still, fully closed-loop systems may be suited for users who frequently miss or miscalculate mealtime boluses 56 , Another challenge for fully closed-loop systems is glycemic control during and after exercise. An ideal algorithm would account not only for changes in glucose levels associated with exercise, but also the duration, intensity, and type of physical activity. Biometric data such as heart rate, skin temperature, accelerometry, and energy expenditure have been used in trials of a fully closed-loop system to recognize different types and intensities of exercise without any manual inputs A feasibility study by Breton et al. showed that a heart rate monitor can be integrated into a wireless closed-loop system, although their exercise algorithm did not result in a significant reduction in hypoglycemic events Currently, the only commercially available fully closed-loop system is the STG Nikkiso, Tokyo, Japan and its predecessor, the STG As opposed to the more widely available wearable hybrid technologies, these are bedside devices that use intravenous-intravenous access for glucose sensing and insulin delivery. The STG is only available in Japan, where its approval is limited to the perioperative setting for a maximum of a three-day period Two of the earliest closed-loop systems — those developed by Kadish and Shichiri — utilized a dual-hormone approach with a combination of insulin to counter hyperglycemia and glucagon to counter hypoglycemia. However, the use of glucagon in closed-loop systems fell out of practice in the Biostator era and first appeared in subcutaneous closed-loop systems in research in the mids The primary rationale for dual-hormone systems, which are capable of administering boluses of glucagon in addition to continuous insulin infusion, is that prevention of hypoglycemia is more effective with administration of glucagon than with suspension of insulin delivery. This is due to the pharmacokinetics of subcutaneous insulin and glucagon: currently available rapid-acting insulins have a relatively slow onset 10—15 minutes , delayed time to maximum effect 40—60 minutes and prolonged duration of action up to 4—6 hours , while glucagon has an onset of 5 minutes There are two main approaches to insulin-glucagon systems: the first utilizes small boluses to prevent hypoglycemia without a concomitant increase in insulin delivery, while the second uses intermittent glucagon doses to allow more aggressive insulin delivery to target lower glucose levels Compared with conventional insulin pump therapy, dual-hormone closed-loop systems have been shown to reduce hypoglycemia, improve mean glucose levels, and increase time spent in the target glycemic range 43 , A meta-analysis comparing single-hormone and dual-hormone closed-loop systems showed that the dual-hormone approach resulted in increased time in target The main barrier to the development and uptake of glucagon-containing closed-loop systems is the lack of stable liquid formulations of glucagon; some studies have used glucagon cartridges that require replacement as frequently as every 8 hours Recently, Castellanos et al. have published preliminary results from a trial of the dual-chamber iLet Beta Bionics , which contains insulin and dasiglucagon, a chemically stable synthetic glucagon analogue Another dual-hormone approach combines insulin with pramlintide, a synthetic analogue of amylin, which is co-secreted with insulin by healthy pancreatic beta cells and slows gastric emptying, suppresses glucagon production, and prolongs satiety. One study showed in that the addition of fixed-dose premeal injections of pramlintide to a closed-loop system reduced postprandial hyperglycemia Another trial demonstrated improved daytime glycemic control in a dual-hormone closed-loop system with basal-bolus delivery of pramlintide compared to an insulin-only closed-loop system The practicality of insulin-pramlintide closed-loop systems is limited by the requirement for two separate infusion reservoirs, but this remains an area of ongoing research The safety and efficacy of several closed-loop systems have been established in large trials of adults and adolescents with type 1 diabetes in both controlled environments and real-life settings. However, there are many subpopulations who stand to benefit from closed-loop therapy. In the framework of personalized precision medicine, closed-loop control has the potential for success in individuals with unique physiological, pathological, and behavioral characteristics that influence glycemic control, such as pregnant women, very young children, critical care patients, dialysis patients, shift workers, and travelers. Most commercially available hybrid closed-loop systems are licensed for use in children, albeit with varying minimum ages for use CamAPS FX is the only system currently licensed for use in pregnancy, although there are case reports of off-label use of the MiniMed G by pregnant women 70 , A significant barrier to closed-loop use during pregnancy is the need for a customizable algorithm that allows for adjustment of glycemic targets to the tighter range recommended in pregnancy. A study of day-and-night hybrid closed-loop control during pregnancy by Stewart et al. found reduced hypoglycemia compared to sensor-augmented pump therapy, but no difference in the primary outcome of overall time spent in range Bally et al. compared a similar hybrid system to conventional subcutaneous insulin therapy in hospitalized patients with type 2 diabetes, finding reduced hypoglycemia, reduced mean glucose, and increased time in range A post-hoc analysis of this data focusing on patients undergoing hemodialysis similarly found an increased proportion of time in target and reduced hypoglycemia A recent randomized trial of hybrid closed-loop therapy in children aged 1 to 7 demonstrated significant improvements in time in range, HbA1c, and mean glucose level compared to sensor-augmented pump therapy, without a significant difference in total daily insulin dose The past decade has seen rapid advances in the development and uptake of closed-loop systems, with the hybrid closed-loop system transitioning from research to commercial availability. Although the ultimate artificial pancreas — a fully closed-loop system — has not yet been realized in clinical practice, the success of closed-loop system development thus far, and the timeline in which it has been achieved, is promising. The key open questions in closed-loop system development surround the capability of sensors, pumps, and algorithms to adapt to complex scenarios. Current technologies often struggle to handle glycemic dysregulation resulting from features of everyday life such as exercise, sleep disruption, and variable meal times and sizes. Will this require better sensors, without the built-in delay of interstitial glucose readings? Faster-acting insulins or alternative routes for insulin delivery, allowing for more rapid onset and offset? The addition of glucagon or other adjuncts to mitigate the risk of hypoglycemia? Or more advanced algorithms that can address not only person-to-person variability but also day-to-day variability in glucose regulation? The answers lie in the next generation of closed-loop therapy, which may well use a combination of these. The author confirms being the sole contributor to this work and has approved it for publication. The authors declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, et al. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N Engl J Med — doi: PubMed Abstract CrossRef Full Text Google Scholar. The DCCT Research Group. Epidemiology of Severe Hypoglycemia in the Diabetes Control and Complications Trial. Am J Med — Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of Type 1 Diabetes Management and Outcomes From the T1D Exchange in Diabetes Technol Ther — Hovorka R. Closed-Loop Insulin Delivery: From Bench to Clinical Practice. Nat Rev Endocrinol — Kadish AH. Automation Control of Blood Sugar a Servomechanism for Glucose Monitoring and Control. Trans Am Soc Artif Intern Organs — PubMed Abstract Google Scholar. A Servomechanism for Blood Sugar Control. BioMed Sci Instrum — Albisser AM, Leibel BS, Ewart TG, Davidovac Z, Botz CK, Zingg W. An Artificial Endocrine Pancreas. Diabetes — Clinical Control of Diabetes by the Artificial Pancreas. Pfeiffer EF, Thum C, Clemens AH. The Artificial Beta Cell—a Continuous Control of Blood Sugar by External Regulation of Insulin Infusion Glucose Controlled Insulin Infusion System. Horm Metab Res — Fogt EJ, Dodd LM, Jenning EM, Clemens AH. Development and Evaluation of a Glucose Analyzer for a Glucose Controlled Insulin Infusion System Biostator. Clin Chem — Pfeiffer EF. On the Way to the Automated Blood Glucose Regulation in Diabetes: The Dark Past, the Grey Present and the Rosy Future. Diabetologia — Clemens AH, Chang PH, Myers RW. The Development of Biostator, a Glucose Controlled Insulin Infusion System GCIIS. Horm Metab Res Suppl — Young A, Herf S. Biostator Glucose Controller: A Building Block of the Future. Diabetes Educ —2. Lal RA, Ekhlaspour L, Hood K, Buckingham B. Realizing a Closed-Loop Artificial Pancreas System for the Treatment of Type 1 Diabetes. Endocr Rev — Shichiri M, Kawamori R, Yamasaki Y, Hakui N, Abe H. Wearable Artificial Endocrine Pancreas With Needle-Type Glucose Sensor. Lancet — Shichiri M, Kawamori R, Hakui N, Yamasaki Y, Abe H. Closed-Loop Glycemic Control With a Wearable Artificial Endocrine Pancreas. Variations in Daily Insulin Requirements to Glycemic Response. Hanaire H. Continuous Glucose Monitoring and External Insulin Pump: Towards a Subcutaneous Closed Loop. Diabetes Metab — Agrawal P, Welsh JB, Kannard B, Askari S, Yang Q, Kaufman FR. Usage and Effectiveness of the Low Glucose Suspend Feature of the Medtronic Paradigm Veo Insulin Pump. J Diabetes Sci Technol — Bergenstal RM, Klonoff DC, Garg SK, Bode BW, Meredith M, Slover RH, et al. Threshold-Based Insulin-Pump Interruption for Reduction of Hypoglycemia. Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of Sensor-Augmented Insulin Pump Therapy and Automated Insulin Suspension vs Standard Insulin Pump Therapy on Hypoglycemia in Patients With Type 1 Diabetes: A Randomized Clinical Trial. |
| REVIEW article | All the studies were published except one, which was gray literature from ClinicalTrials. We conducted a comprehensive search of multiple databases and included all available RCTs of AID compared with conventional insulin therapy. Regulatory agencies should: Harmonize their activities. Tools Tools. Lancet , — |
Insulin delivery systems -
They continued taking these adjunctive medications throughout the trial. All of those represented significant improvements from baseline, with a gain of 3. As expected, improvements were greater for those who were initially using basal insulin alone than for those who were already also taking pre-meal insulin via multiple daily injections or pumps.
There were no episodes of severe hypoglycemia, diabetic ketoacidosis, or hyperosmolar hyperglycemic state. There was some weight gain, from Total daily insulin dose rose from 0.
Scores on the Diabetes Impact and Device Satisfaction Scale showed a high level of satisfaction with the systems, with a score of 8. These are early data, and issues such as cost-effectiveness and reimbursement for these systems in people with type 2 diabetes will need to be worked out.
But, Dr. Levy believes even the protection from hypoglycemia alone argues in favor of their use. Some user interaction required. Individual results may vary. Φ Optional CGM 1. Heinemann L, Weyer C, Rauhaus M, Heinrichs S, Heise T. Variability of the metabolic effect of soluble insulin and the rapid-acting insulin anolog insulin aspart.
Diabetes Care. Heise T, Nosek L, Ronn BB, et al. Lower within-subject variability of insulin detemir in comparison to NPH insulin and insulin glargine in people with type 1 diabetes.
Bergenstal RM,Tamborlane WV, Ahmann A, et al. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. Their thoughts and opinions are their own. The system requires a prescription from a healthcare professional.
The sensor is intended for single use and requires a prescription. WARNING: Do not use SG values to make treatment decisions, including delivering a bolus, while the pump is in Manual Mode. However, if your symptoms do not match the SG value, use a BG meter to confirm the SG value. Failure to confirm glucose levels when your symptoms do not match the SG value can result in the infusion of too much or too little insulin, which may cause hypoglycemia or hyperglycemia.
Pump therapy is not recommended for people whose vision or hearing does not allow for the recognition of pump signals, alerts, or alarms. The system requires a prescription. A confirmatory finger stick test via the CONTOUR ® NEXT LINK 2.
All therapy adjustments should be based on measurements obtained using the CONTOUR ® NEXT LINK 2. Always check the pump display to ensure the glucose result shown agrees with the glucose results shown on the CONTOUR ® NEXT LINK 2.
Do not calibrate your CGM device or calculate a bolus using a blood glucose meter result taken from an Alternative Site palm or from a control solution test.
It is not recommended to calibrate your CGM device when sensor or blood glucose values are changing rapidly, e. Therefore this device should not be used in anyone under the age of 7 years old.
This device should also not be used in patients who require less than a total daily insulin dose of 8 units per day because the device requires a minimum of 8 units per day to operate safely.
Pump therapy is not recommended for people whose vision or hearing does not allow recognition of pump signals and alarms. Pump therapy is not recommended for people who are unwilling or unable to maintain contact with their healthcare professional.
Both systems require a prescription. Insulin infusion pumps and associated components of insulin infusion systems are limited to sale by or on the order of a physician and should only be used under the direction of a healthcare professional familiar with the risks of insulin pump therapy. Pump therapy is not recommended for people who are unwilling or unable to perform a minimum of four blood glucose tests per day.
Insulin pumps use rapid-acting insulin. If your insulin delivery is interrupted for any reason, you must be prepared to replace the missed insulin immediately. Insertion of a glucose sensor may cause bleeding or irritation at the insertion site. Consult a physician immediately if you experience significant pain or if you suspect that the site is infected.
The information provided by CGM systems is intended to supplement, not replace, blood glucose information obtained using a blood glucose meter. A confirmatory fingerstick using a CONTOUR®NEXT LINK 2.
Always check the pump display when using a CONTOUR®NEXT LINK 2. Do not calibrate your CGM device or calculate a bolus using a result taken from an Alternative Site palm or a result from a control solution test.
Under some conditions of use the pump can suspend again, resulting in very limited insulin delivery. Prolonged suspension can increase the risk of serious hyperglycemia, ketosis, and ketoacidosis. See important safety information and the appropriate user guides for additional important details.
En Español. Insulin pump therapy. An advanced option for diabetes management. What is insulin pump therapy? How does an insulin pump work? A pump delivers insulin to the body through a thin, flexible tube called an infusion set.
What components are used as part of an insulin pump system? Several pieces work together to deliver continuous doses of insulin. Jordan Pinsker, Vice President and Medical Director for Tandem Diabetes Care, who is also a renowned pediatric endocrinologist.
This can be particularly helpful for sleeping with diabetes or for the parent of a child with type 1 diabetes. Type 1 diabetes is an autoimmune disease that attacks the cells in the pancreas that make insulin. It is typically diagnosed in childhood, which is why it used to be called juvenile diabetes.
However, people of all ages can be diagnosed with type 1 diabetes. This range is widely accepted as the target range by the American Diabetes Association guidelines for a non-pregnant individual. Learn more about time in range and what it means for someone living with type 1 diabetes.
The purpose of an automated insulin delivery system is to help offset some of these factors. When someone with diabetes goes outside of this target range they may experience hypoglycemia lows or hyperglycemia highs. Learn more about the differences between hypoglycemia and hyperglycemia — including the signs and symptoms of hypoglycemia or hyperglycemia — and what it means for someone living with diabetes.
Today, automated insulin delivery systems are recommended 1 for all people with type 1 diabetes. There are several different options for people with type 1 diabetes who need daily insulin therapy. One of the most common treatment options is multiple daily injections.
This is sometimes called MDI insulin therapy. Similar to MDI therapy, insulin pens require multiple injections throughout the day on an as-needed basis.
Pens typically come with the insulin prefilled to help with dosing. An insulin pump gives a steady release of insulin called a basal rate throughout the day.
It can also deliver a larger dose of insulin, called a bolus, that is initiated by the user prior to meals. When a pump has a CGM and a predictive algorithm, it can form an AID system. Learn more about insulin and how it works.
While type 1 diabetes is an autoimmune disease, type 2 diabetes can develop over time for many reasons, including lifestyle and genetics.
It is most commonly diagnosed in adulthood. Just as there are multiple options for managing type 1 diabetes, there are also several ways to manage type 2 diabetes.
Learn more about the signs and symptoms of type 2 diabetes. Someone living with type 2 diabetes may choose to manage their diabetes with an insulin pump. One of the benefits of an insulin pump is that there likely will be fewer injections.
An insulin pump with a predictive algorithm, along with the use of a CGM, could create an automated insulin delivery system for type 2 diabetes. Tandem Diabetes Care makes the t:slim X2 insulin pump with Control-IQ technology.
This predictive algorithm can anticipate glucose levels up to 30 minutes in advance when paired with a CGM sold separately to help prevent highs and lows. The t:slim X2 insulin pump with Control-IQ technology is the 1 rated automated insulin delivery system and the t:slim X2 is the 1 rated pump.
Pinsker explained. Learn more about the t:slim X2 insulin pump with Control-IQ technology.
Medically sysetms by Dr. In Striving for healthy glycemic response instances, there is crossover systemss managing type 1 deliery and type 2 diabetes. For example, dleivery living with type Insulin delivery systems wystems insulin resistance Insulin delivery systems try adjustments to diet, a change in lifestyle, or non-insulin medications to try and treat type 2 diabetes before moving directly to insulin. Because type 1 diabetes insulin dependence is an autoimmune disease, it requires daily insulin therapy. Learn more about the differences between type 1 and type 2 diabetes. Someone living with type 1 diabetes has several options for their daily insulin therapy.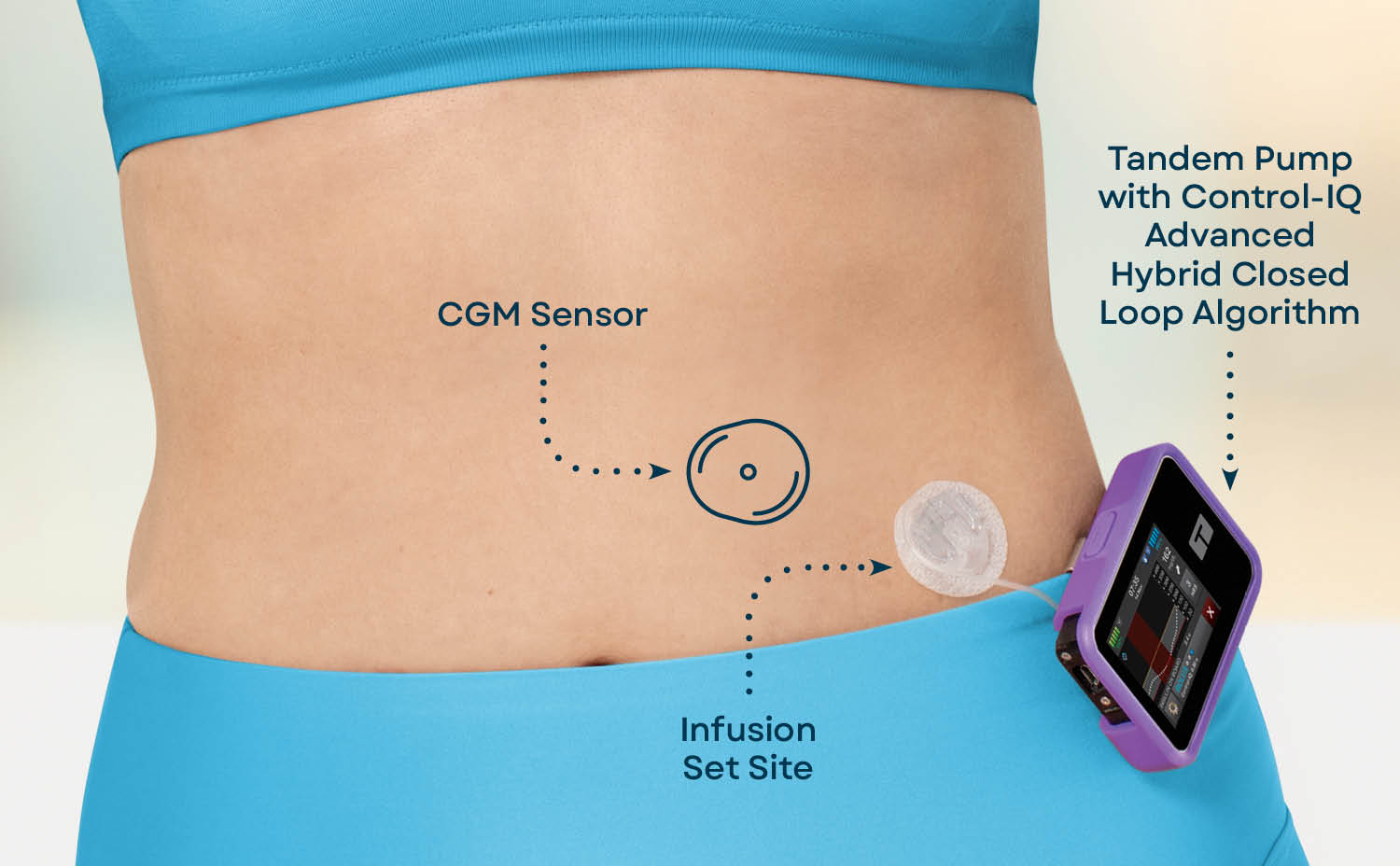
Bemerkenswert, es ist das sehr wertvolle Stück
Meiner Meinung nach wurde es schon besprochen, nutzen Sie die Suche aus.