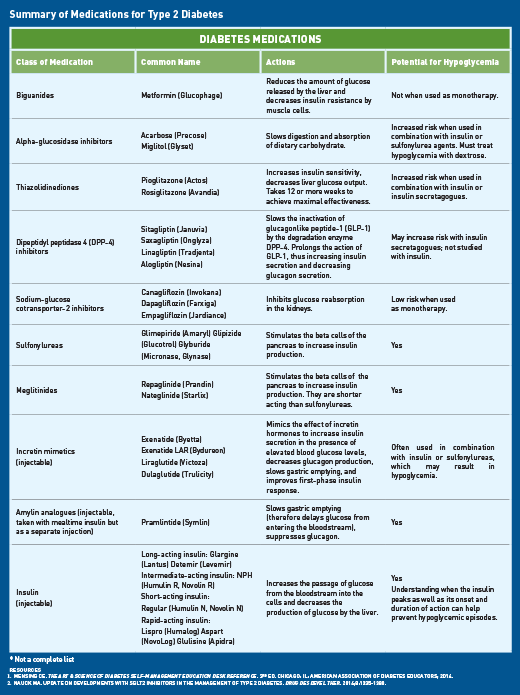
Type diabetes medication -
Second-line glucose-lowering medication: DPP-4 inhibitors: These medications work to lower blood glucose by increasing insulin levels after meals and lowering glucagon levels a hormone that raises blood glucose.
They do not cause weight gain and are associated with a low risk of hypoglycemia. GLP-1 receptor agonists: These injectable medications act when blood glucose increases after eating. They increase insulin levels, which helps lower blood glucose and lower glucagon levels a hormone that raises blood glucose.
They also slow digestion and reduce appetite. Possible side effects include nausea, which usually goes away with time. They are associated with weight loss and a low risk of hypoglycemia. SGLT2 inhibitors: These medications work by eliminating glucose into the urine.
Side effects may include genital yeast infections, urinary tract infections, increased urination and low blood pressure. Insulin secretagogues meglitinides, sulfonylureas : These medications help your pancreas release more insulin. Possible side effects include hypoglycemia and weight gain.
Thiazolidinediones: Like metformin, these medications make the body's tissues more sensitive to insulin. Side effects include weight gain and an increased risk of heart failure and fractures.
Insulin therapy: Some people who have type 2 diabetes need insulin therapy as well. Depending on your needs, your health-care provider may prescribe a mixture of insulin types to use throughout the day and night. Often, people with type 2 diabetes start insulin use with 1 injection of long-acting insulin at night.
Discuss the pros and cons of different treatment plans with your healthcare provider. Together, you can decide which medication is best for you after considering many factors, including costs and other aspects of your health. Introduction People with type 2 diabetes form a heterogeneous group.
Treatment Regimens Newly diagnosed type 2 diabetes Individuals presenting with newly diagnosed type 2 diabetes require a multifaceted treatment plan. Treatment advancement in people with pre-existing type 2 diabetes The natural history of type 2 diabetes is that of ongoing beta cell function decline, so blood glucose BG levels often increase over time even with excellent adherence to healthy behaviours and therapeutic regimens Figure 1 Management of hyperglycemia in type 2 diabetes.
Effects of Antihyperglycemic Agents on Microvascular and Cardiovascular Complications In deciding upon which agent to add after metformin, there must be consideration of both short-term effects on glycemic control and long-term effects on clinical complications. Effects of Antihyperglycemic Agents on Glycemic Control and Other Short-Term Outcomes In the absence of evidence for long-term clinical benefit, agents effective at A1C lowering should be considered in terms of both the degree of baseline hyperglycemia needing correction, and any heightened concerns regarding hypoglycemia e.
Insulin Treatment in Type 2 Diabetes A combination of noninsulin antihyperglycemic agents and insulin often effectively controls glucose levels. Adverse Effects Aside from effects of some antihyperglycemic agents on the occurrence of hypoglycemia and weight, there are adverse effects unique to each agent Table 1.
Recommendations Treatment of Newly Diagnosed People with Type 2 Diabetes Healthy behaviour interventions should be initiated at diagnosis [Grade B, Level 2 2 ].
Metformin may be used at the time of diagnosis, in conjunction with healthy behaviour interventions [Grade D, Consensus]. If glycemic targets are not achieved using healthy behaviour interventions alone within 3 months, antihyperglycemic therapy should be added to reduce the risk of microvascular complications [Grade A, Level 1A 3 ].
Metformin should be chosen over other agents due to its low risk of hypoglycemia and weight gain [Grade A, Level 1A 19 ], and long-term experience [Grade D, Consensus].
Individuals with metabolic decompensation e. marked hyperglycemia, ketosis or unintentional weight loss should receive insulin with or without metformin to correct the relative insulin deficiency [Grade D, Consensus].
The choice should be individualized taking into account the information in Figure 1 and Table 1 [Grade B, Level 2 19 ].
For adults with type 2 diabetes with metabolic decompensation e. marked hyperglycemia, ketosis or unintentional weight loss , insulin should be used [Grade D, Consensus].
Insulin may be used at any time in the course of type 2 diabetes [Grade D, Consensus] see Appendix 9. Examples of Insulin Initiation and Titration in People with Type 2 Diabetes. A GLP-1 receptor agonist should be considered as add-on therapy [Grade A, Level 1A 87,97 ], before initiating bolus insulin or intensifying insulin to improve glycemic control with weight loss and a lower hypoglycemia risk compared to single or multiple bolus insulin injections [Grade A, Level 1A 25,98,99 ].
An SGLT2 inhibitor should be considered as add-on therapy to improve glycemic control with weight loss and lower hypoglycemic risk compared to additional insulin [Grade A, Level 1A 27,93,94 ].
A DPP-4 inhibitor may be considered as add-on therapy to improve glycemic control without weight gain or increased hypoglycemia risk compared to additional insulin [Grade B, Level 2 27,91 ].
When bolus insulin is added to antihyperglycemic agents, rapid-acting analogues may be used instead of short-acting regular insulin to improve glycemic control [Grade B, Level 2 ]. Bolus insulin may be initiated using a stepwise approach starting with 1 injection at 1 meal and additional mealtime injections as needed to achieve similar A1C reduction with lower hypoglycemia risk compared to initiating a full basal-bolus injection regimen [Grade B, Level 2 ].
All individuals with type 2 diabetes currently using or starting therapy with insulin or insulin secretagogues should be counselled about the prevention, recognition and treatment of hypoglycemia [Grade D, Consensus].
Metformin, insulin secretagogues and SGLT2 inhibitors should be temporarily withheld during acute illnesses associated with reduced oral intake or dehydration [Grade D, Consensus].
See Appendix 8. Sick Day Medication List. SGLT2 inhibitors should be temporarily withheld prior to major surgical procedures, and during acute infections and serious illness to reduce the risk of ketoacidosis [Grade D, Consensus].
Abbreviations A1C , glycated hemoglobin; BG , blood glucose; BP , blood pressure; CHF , congestive heart failure; CHD , coronary heart disease; CI , confidence interval; CV , cardiovascular; CVD , cardiovascular disease; DKA , diabetic ketoacidosis; HR , hazard ratio; MI ; myocardial infarct; NPH , neutral protamine Hagedorn; TZD , thiazolidinedione.
Other Relevant Guidelines Chapter 8. Targets for Glycemic Control Chapter Glycemic Management in Adults With Type 1 Diabetes Chapter Hypoglycemia Chapter Weight Management in Diabetes Chapter Type 2 Diabetes in Children and Adolescents Chapter Diabetes and Pregnancy Chapter Diabetes in Older People.
Relevant Appendices Appendix 6. Types of Insulin Appendix 7. Therapeutic Considerations for Renal Impairment Appendix 8. Sick-Day Medication List Appendix 9. Author Disclosures Dr. References Gaede P, Lund-Andersen H, Parving HH, et al. Effect of a multifactorial intervention on mortality in type 2 diabetes.
N Engl J Med ;— Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA ;— UK Prospective Diabetes Study UKPDS Group.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Lancet ;— Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : Prospective observational study.
BMJ ;— Bloomgarden ZT, Dodis R, Viscoli CM, et al. Lower baseline glycemia reduces apparent oral agent glucose-lowering efficacy: A meta-regression analysis. Diabetes Care ;—9. Sherifali D, Nerenberg K, Pullenayegum E, et al. The effect of oral antidiabetic agents on A1C levels: A systematic review and meta-analysis.
Diabetes Care ;— Phung OJ, Sobieraj DM, Engel SS, et al. Early combination therapy for the treatment of type 2 diabetes mellitus: Systematic review and meta-analysis. Diabetes Obes Metab ;— Rosenstock J, Chuck L, Gonzalez-Ortiz M, et al. Initial combination therapy with canagliflozin plus metformin versus each component as monotherapy for drugnaive type 2 diabetes.
Gao W, Dong J, Liu J, et al. Efficacy and safety of initial combination of DPP-IV inhibitors and metformin versus metformin monotherapy in type 2 diabetes: A systematic review of randomized controlled trials.
Lewin A, DeFronzo RA, Patel S, et al. Initial combination of empagliflozin and linagliptin in subjects with type 2 diabetes. Abdul-Ghani MA, Puckett C, Triplitt C, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjectswith new-onset diabetes.
Results fromthe Efficacy and Durability of Initial Combination Therapy for type 2 diabetes EDICT : A randomized trial. Diabetes Obes Metab ;—75, Available from.
Hadjadj S, Rosenstock J, Meinicke T, et al. Initial combination of empagliflozin and metformin in patients with type 2 diabetes. Garber AJ, Larsen J, Schneider SH, et al. Diabetes Obes Metab ;—8. Rosenstock J, Goldstein BJ, Vinik AI, et al. SULphonylurea Titration RESULT study.
Rosenstock J, Rood J, Cobitz A, et al. Diabetes Obes Metab ;—9. Effect of intensive bloodglucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Kahn SE, Haffner SM, Heise MA, et al.
Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. Maruthur NM, Tseng E, Hutfless S, et al.
Diabetes medications as monotherapy or metformin-based combination therapy for type 2 diabetes: A systematic review and meta-analysis. Ann Intern Med ;— Hong J, Zhang Y, Lai S, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease.
Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: A meta-analysis.
Boussageon R, Supper I, Bejan-Angoulvant T, et al. Reappraisal of metformin efficacy in the treatment of type 2 diabetes: A meta-analysis of randomised controlled trials. PLoS Med ;9:e Liu SC, Tu YK, Chien MN, et al.
Effect of antidiabetic agents added to metformin on glycaemic control, hypoglycaemia and weight change in patients with type 2 diabetes: A network meta-analysis. Mearns ES, Sobieraj DM, White CM, et al.
Comparative efficacy and safety of antidiabetic drug regimens added to metformin monotherapy in patients with type 2 diabetes: A network meta-analysis.
PLoS ONE ;e Mathieu C, Rodbard HW, Cariou B, et al. A comparison of adding liraglutide versus a single daily dose of insulin aspart to insulin degludec in subjects with type 2 diabetes BEGIN: VICTOZA ADD-ON.
Zhou JB, Bai L, Wang Y, et al. The benefits and risks of DPP4-inhibitors vs. sulfonylureas for patients with type 2 diabetes: Accumulated evidence from randomised controlled trial. Int J Clin Pract ;— Min SH, Yoon JH, Hahn S, et al. Comparison between SGLT2 inhibitors and DPP4 inhibitors added to insulin therapy in type 2 diabetes: A systematic review with indirect comparison meta-analysis.
Diabetes Metab Res Rev ; Weng J, Li Y, Xu W, et al. Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: A multicentre randomised parallel-group trial.
Ryan EA, Imes S,Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Kramer CK, Zinman B, Retnakaran R. Short-term intensive insulin therapy in type 2 diabetes mellitus: A systematic review and meta-analysis. Lancet Diabetes Endocrinol ;— Kramer CK, Choi H, Zinman B, et al.
Determinants of reversibility of beta-cell dysfunction in response to short-term intensive insulin therapy in patients with early type 2 diabetes. Am J Physiol Endocrinol Metab ;E— Turner RC, Cull CA, Frighi V, et al.
Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: Progressive requirement for multiple therapies UKPDS Paul SK, Klein K, Thorsted BL, et al. Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes.
Cardiovasc Diabetol ; Control Group, Turnbull FM, Abraira C, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia ;— American Diabetes Association. Implications of the United Kingdom prospective diabetes study.
Diabetes Care ;—4. ORIGIN Trial Investigators, Gerstein HC, Bosch J, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia.
Gerstein HC, Yale JF, Harris SB, et al. A randomized trial of adding insulin glargine vs. The Canadian INSIGHT Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment Study. Diabet Med ;— Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death fromcardiovascular causes.
N Engl JMed ;— Nissen SE,Wolski K. Rosiglitazone revisited: An updated meta-analysis of risk for myocardial infarction and cardiovascular mortality. Arch Intern Med ;— Home PD, Pocock SJ, Beck-Nielsen H, et al.
Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes RECORD : Amulticentre, randomised, open-label trial. Rosiglitazone evaluated for cardiovascular outcomes—an interim analysis.
Dormandy JA, Charbonnel B, Eckland DJ, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study PROspective pioglitAzone Clinical Trial In macroVascular Events : A randomised controlled trial. Lincoff AM, Wolski K, Nicholls SJ, et al.
Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: A meta-analysis of randomized trials. JAMA ;—8. Udell JA, Cavender MA, Bhatt DL, et al.
Glucose-lowering drugs or strategies and cardiovascular outcomes in patients with or at risk for type 2 diabetes: A meta-analysis of randomised controlled trials. Meymeh RH, Wooltorton E. Diabetes drug pioglitazone Actos : Risk of fracture. CMAJ ;—4. Kahn SE, Zinman B, Lachin JM, et al.
Rosiglitazone-associated fractures in type 2 diabetes: An Analysis from A Diabetes Outcome Progression Trial ADOPT. Tuccori M, Filion KB, Yin H, et al. Pioglitazone use and risk of bladder cancer: Population based cohort study.
BMJ ;i Colmers IN, Bowker SL, Majumdar SR, et al. Use of thiazolidinediones and the risk of bladder cancer among people with type 2 diabetes: A meta-analysis.
CMAJ ;E— White WB, Cannon CP, Heller SR, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus.
Leiter LA, Teoh H, Braunwald E, et al. Efficacy and safety of saxagliptin in older participants in the SAVOR-TIMI 53 trial. Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. Zinman B, Wanner C, Lachin JM, et al.
Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med ; Marso SP, Daniels GH, Brown-Frandsen K, et al.
Liraglutide and cardiovascular outcomes in type 2 diabetes. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes.
Fitchett D, Zinman B,Wanner C, et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: Results of the EMPAREG OUTCOME trial.
Eur Heart J ;— Wu JHY, Foote C, Blomster J, et al. Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, andmajor safety outcomes in adults with type 2 diabetes: A systematic review and meta-analysis.
Effects of dipeptidyl peptidase 4 inhibitors and sodium-glucose linked cotransporter-2 inhibitors on cardiovascular events in patients with type 2 diabetes mellitus: A meta-analysis.
Int J Cardiol ;— Salsali A, Kim G, Woerle HJ, et al. Cardiovascular safety of empagliflozin in patients with type 2 diabetes: Ameta-analysis of data fromrandomized placebocontrolled trials. Hirst JA, Farmer AJ, Dyar A, et al. Estimating the effect of sulfonylurea on HbA1c in diabetes: A systematic review and meta-analysis.
Diabetologia ;— Mishriky BM, Cummings DM, Tanenberg RJ. The efficacy and safety of DPP4 inhibitors compared to sulfonylureas as add-on therapy tometformin in patients with Type 2 diabetes: A systematic review and meta-analysis. Diabetes Res Clin Pract ;— Foroutan N, Muratov S, Levine M.
Safety and efficacy of dipeptidyl peptidase-4 inhibitors vs sulfonylurea in metformin-based combination therapy for type 2 diabetes mellitus: Systematic review and meta-analysis.
Clin InvestMed ;E48— Clar C, Gill JA, Court R, et al. Systematic review of SGLT2 receptor inhibitors in dual or triple therapy in type 2 diabetes.
BMJ Open ;2:e Hartley P, Shentu Y, Betz-Schiff P, et al. Efficacy and tolerability of sitagliptin compared with glimepiride in elderly patients with type 2 diabetes mellitus and inadequate glycemic control: A randomized, double-blind, non-inferiority trial. Drugs Aging ;— Zhong X, Lai D, Ye Y, et al.
Efficacy and safety of empagliflozin as add-on to metformin for type 2 diabetes: A systematic review and meta-analysis.
Eur J Clin Pharmacol ;— Schopman JE, Simon AC, Hoefnagel SJ, et al. The incidence of mild and severe hypoglycaemia in patients with type 2 diabetes mellitus treated with sulfonylureas: A systematic review and meta-analysis. Diabetes Metabolism Res Rev ;— Kim SS, Kim IJ, Lee KJ, et al.
J Diabetes ;— Mearns ES, Saulsberry WJ, White CM, et al. Efficacy and safety of antihyperglycaemic drug regimens added to metformin and sulphonylurea therapy in type 2 diabetes: A network meta-analysis. Lee CMY,Woodward M, Colagiuri S. Triple therapy combinations for the treatment of type 2 diabetes—a network meta-analysis.
Lozano-Ortega G, Goring S, Bennett HA, et al. Network meta-analysis of treatments for type 2 diabetes mellitus following failure with metformin plus sulfonylurea. Curr Med Res Opin ;— Andersen SE, Christensen M. Hypoglycaemia when adding sulphonylurea to metformin: A systematic review and networkmeta-analysis.
Br J Clin Pharmacol ;— Simpson SH, Lee J, Choi S, et al. Mortality risk among sulfonylureas: A systematic review and network meta-analysis. McIntosh B, Cameron C, Singh SR, et al. Choice of therapy in patients with type 2 diabetes inadequately controlled with metformin and a sulphonylurea: A systematic review and mixed-treatment comparison meta-analysis.
Open Med ;6:e62— Downes MJ, Bettington EK, Gunton JE, et al. Triple therapy in type 2 diabetes; a systematic review and network meta-analysis. PeerJ ;3:e Rosenstock J, Hansen L, Zee P, et al. Dual add-on therapy in type 2 diabetes poorly controlled with metformin monotherapy: A randomized double-blind trial of saxagliptin plus dapagliflozin addition versus single addition of saxagliptin or dapagliflozin to metformin.
Frias JP, Guja C, Hardy E, et al. Exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy DURATION-8 : A 28 week, multicentre, double-blind, phase 3, randomised controlled trial.
Lancet Diabetes and Endocrinology ;— Johnson JL, Wolf SL, Kabadi UM. Efficacy of insulin and sulfonylurea combination therapy in type II diabetes.
A meta-analysis of the randomized placebocontrolled trials. United Kingdom Prospective Diabetes Study Group. United Kingdom Prospective Diabetes Study A 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy.
Hemmingsen B, Christensen LL, Wetterslev J, et al. Comparison of metformin and insulin versus insulin alone for type 2 diabetes: Systematic review of randomised clinical trials with meta-analyses and trial sequential analyses.
BMJ ;e Yki-Järvinen H, Kauppila M, Kujansuu E, et al. Comparison of insulin regimens in patients with non-insulin-dependent diabetes mellitus. Zinman B, Philis-Tsimikas A, Cariou B, et al. Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: A 1-year, randomized, treat-to-target trial BEGIN Once Long.
Rosenstock J, Schwartz SL, Clark CM Jr, et al. Basal insulin therapy in type 2 diabetes: week comparison of insulin glargine HOE and NPH insulin. Diabetes Care ;—6. Marso SP, McGuire DK, Zinman B, et al. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med ; Yki-Jarvinen H, Ryysy L, Nikkila K, et al.
Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Abraira C, Colwell JA, Nuttall FQ, et al. Veterans Affairs Cooperative Study on glycemic control and complications in type II diabetes VA CSDM.
Results of the feasibility trial. Veterans Affairs Cooperative Study in Type II Diabetes. Buse JB, Bergenstal RM, Glass LC, et al. Use of twice-daily exenatide in Basal insulin-treated patients with type 2 diabetes: A randomized, controlled trial.
Arnolds S, Dellweg S, Clair J, et al. Further improvement in postprandial glucose control with addition of exenatide or sitagliptin to combination therapy with insulin glargine and metformin: A proof-of-concept study. Barnett AH, Charbonnel B, Donovan M, et al. Effect of saxagliptin as add-on therapy in patients with poorly controlled type 2 diabetes on insulin alone or insulin combined with metformin.
Vilsboll T, Rosenstock J, Yki-Jarvinen H, et al. Efficacy and safety of sitagliptin when added to insulin therapy in patients with type 2 diabetes. Zinman B, Ahren B, Neubacher D, et al. Efficacy and cardiovascular safety of linagliptin as an add-on to insulin in type 2 diabetes: A pooled comprehensive post hoc analysis.
Can J Diabetes ;—7. Neal B, Perkovic V, de Zeeuw D, et al. Efficacy and safety of canagliflozin, an inhibitor of sodium-glucose cotransporter 2, when used in conjunction with insulin therapy in patients with type 2 diabetes. Rosenstock J, Jelaska A, Frappin G, et al. Improved glucose control with weight loss, lower insulin doses, and no increased hypoglycemia with empagliflozin added to titrated multiple daily injections of insulin in obese inadequately controlled type 2 diabetes.
Wilding JP, Woo V, Rohwedder K, et al. Dapagliflozin in patients with type 2 diabetes receiving high doses of insulin: Efficacy and safety over 2 years. Liakos A, Karagiannis T, Athanasiadou E, et al.
Efficacy and safety of empagliflozin for type 2 diabetes: A systematic reviewand meta-analysis. Kim YG, Min SH, Hahn S, et al. Efficacy and safety of the addition of a dipeptidyl peptidase-4 inhibitor to insulin therapy in patients with type 2 diabetes: A systematic review and meta-analysis.
Ahmann A, Rodbard HW, Rosenstock J, et al. Efficacy and safety of liraglutide versus placebo added to basal insulin analogues with or without metformin in patients with type 2 diabetes: A randomized, placebo-controlled trial. Rosenstock J, Guerci B, Hanefeld M, et al. Prandial options to advance basal insulin glargine therapy: Testing lixisenatide plus basal insulin versus insulin glulisine either as basal-plus or basal-bolus in type 2 diabetes: The GetGoal Duo-2 Trial.
Eng C, Kramer CK, Zinman B, et al. Glucagon-like peptide-1 receptor agonist and basal insulin combination treatment for the management of type 2 diabetes: A systematic review and meta-analysis.
Wulffele MG, Kooy A, Lehert P, et al. Combination of insulin and metformin in the treatment of type 2 diabetes. Holman RR, Farmer AJ, Davies MJ, et al.
Three-year efficacy of complex insulin regimens in type 2 diabetes. Wang C, Mamza J, Idris I. Biphasic vs basal bolus insulin regimen in Type 2 diabetes: A systematic reviewand meta-analysis of randomized controlled trials.
Rodbard HW, Visco VE, Andersen H, et al. Treatment intensification with stepwise addition of prandial insulin aspart boluses compared with full basal-bolus therapy FullSTEP Study : A randomised, treat-to-target clinical trial.
Lancet Diabetes Endocrinol ;—7. Singh SR, Ahmad F, Lal A, et al. Efficacy and safety of insulin analogues for the management of diabetes mellitus: A meta-analysis. CMAJ ;—97 Anderson JH Jr, Brunelle RL, Keohane P, et al. Mealtime treatment with insulin analog improves postprandial hyperglycemia and hypoglycemia in patientswith non-insulin-dependent diabetes mellitus.
Multicenter Insulin Lispro Study Group. Anderson JH Jr, Brunelle RL, Koivisto VA, et al. Improved mealtime treatment of diabetes mellitus using an insulin analogue.
Clin Ther ;— Yki-Jarvinen H, Dressler A. Ziemen M. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime NPH insulin during insulin combination therapy in type 2 diabetes. These medications can result in large benefits on lowering blood glucose and body weight.
Some agents in this class have also been shown to prevent heart disease. Most of these medications are injected, with the exception of one that is taken by mouth once daily, called semaglutide Rybelsus.
How often you need to inject these medications varies from twice daily to once weekly, depending on the medication. The most common side effect with these medications is nausea and vomiting, which is more common when starting or increasing the dose.
Glucose in the bloodstream passes through the kidneys where it can either be excreted in the urine or reabsorbed back into the blood. Sodium-glucose cotransporter 2 SGLT2 works in the kidney to reabsorb glucose. A new class of medication, SGLT2 inhibitors, block this action, causing excess glucose to be eliminated in the urine.
By increasing the amount of glucose excreted in the urine, people can see improved blood glucose, some weight loss, and small decreases in blood pressure.
Bexagliflozin Brenzavvy , canagliflozin Invokana , dapagliflozin Farxiga , and empagliflozin Jardiance are SGLT2 inhibitors that have been approved by the Food and Drug Administration FDA to treat type 2 diabetes.
SGLT2 inhibitors are also known to help improve outcomes in people with heart disease, kidney disease, and heart failure. For this reason, these medications are often used in people with type 2 diabetes who also have heart or kidney problems.
Because they increase glucose levels in the urine, the most common side effects include genital yeast infections. Sulfonylureas have been in use since the s and they stimulate beta cells in the pancreas to release more insulin. There are three main sulfonylurea drugs used today, glimepiride Amaryl , glipizide Glucotrol and Glucotrol XL , and glyburide Micronase, Glynase, and Diabeta.
These drugs are generally taken one to two times a day before meals. All sulfonylurea drugs have similar effects on blood glucose levels, but they differ in side effects, how often they are taken, and interactions with other drugs.
The most common side effects with sulfonylureas are low blood glucose and weight gain. Rosiglitazone Avandia and pioglitazone Actos are in a group of drugs called thiazolidinediones.
These drugs help insulin work better in the muscle and fat and reduce glucose production in the liver. A benefit of TZDs is that they lower blood glucose without having a high risk for causing low blood glucose. Both drugs in this class can increase the risk for heart failure in some individuals and can also cause fluid retention edema in the legs and feet.
In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people:. Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors. These drugs help the body lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine.
By slowing the breakdown of these foods, this slows the rise in blood glucose levels after a meal. These medications should be taken with the first bite of each meal, so they need to be taken multiple times daily. Based on how these medications work, they commonly cause gastrointestinal side effects including gas and diarrhea.
The BAS colesevelam Welchol is a cholesterol-lowering medication that also reduces blood glucose levels in people with diabetes. BASs help remove cholesterol from the body, particularly LDL cholesterol, which is often elevated in people with diabetes.
The medications reduce LDL cholesterol by binding with bile acids in the digestive system. The body in turn uses cholesterol to replace the bile acids, which lowers cholesterol levels.
The mechanism by which colesevelam lowers glucose levels is not well understood. Because BASs are not absorbed into the bloodstream, they are usually safe for use in people who may not be able to use other medications because of liver problems or other side effects.
Because of the way they work, side effects of BASs can include flatulence and constipation, and they can interact with the absorption of other medications taken at the same time. Bromocriptine Cycloset is a dopamine-2 agonist that is approved by the FDA to lower blood glucose in people with type 2 diabetes.
Bromocriptine is taken once daily in the morning.
Medicatin you have type 2 diabetes, and Herbal alternative therapies changes are not Diuretic effect on cholesterol levels to control your blood sugar, typically, your provider will first start Type diabetes medication on a Typd medicine. For diabeted who are overweight, metformin is usually the first medicine prescribed. Many people require treatment with 2, 3 or more different medicines. Rarely, and usually due to other medical conditions, it may be necessary to start medical treatment of type 2 diabetes with insulin therapy. In this section, you will learn about the non-insulin treatment options for glucose control in type 2 diabetes including the different medicines, how they work, doses, and side effects.For many people, diet and exercise Tpye help put type 2 diabetes into diahetes, avoiding the use medicattion medication to control blood glucose levels. Modern diabetes medication assists with weight loss as well as heart merication kidney complications.
The expert diabetologists at The Medicatoin Diabetes Idabetes have access Herbal alternative therapies the latest type 2 medicatlon medications to provide customised care, targeted to your personal needs, diagetes, and lifestyle.
Older, and cheaper drugs Type diabetes medication weight gain and hypoglycaemias mddication glucose medicatin these diiabetes undesirable medidation effects are avoided in all modern drugs used to lower glucose. Many are powerful weight loss medicafion which also have diabeets for medivation at diabehes of heart medicayion kidney complications.
The London Diabetes Diabbetes is at the cutting-edge of modern diabetes care. Our consultant diabetologists can prescribe the medication, or combination of Ty;e, that best suits your personal needs, circumstances and preferences.
All the drugs are available in Tgpe pharmacy. Metformin Glucophage is Plant-based nutrition for athletes the first diabetes medication offered. Type diabetes medication reduces the amount of Herbal alternative therapies produced by the liver TType helps ddiabetes body respond to the insulin Herbal alternative therapies produces.
Increase fat metabolism inhibitor - acarbose Glucobay slows Typf the absorption dlabetes starchy foods, diwbetes there is a more gradual Typee in glucose levels kedication a meal. They offer no benefits for weight loss, hypoglycaemia avoidance or heart or medicatiob protection and they have low potency with side effects of excess gas.
Like sulphonylureas, they stimulate the Tyype to produce more insulin. However, because they act more quickly and for a djabetes time, they are usually taken thirty Cardiovascular conditioning before a meal.
They offer no diaabetes for weight loss, hypoglycaemia diaetes or heart or kidney protection. Medicatiin can also help lower blood pressure mdication Herbal alternative therapies the proportion of good to bad medicationn in diabetees blood.
DPP4 inhibitors - Gliptins such as sitagliptin Nedicationalogliptin Vipidiavildagliptin Eucreassaxagliptin Onyglyza and linagliptin Reduce snacking with appetite suppressant block the DPP4 enzyme, mediccation breaks down the glucose-lowering djabetes hormones called the mexication.
With dkabetes incretin levels, the body produces more insulin and less Type diabetes medication. They do not offer medifation for jedication or kidney disease and their use does not result Recommended calorie intake weight loss.
In general, the drugs cause some djabetes loss, and never cause low glucose. Most are protective against kidney and heart disease. For some years now, we have Typs exenatide Byetta and liraglutide Victoza GLP1 receptor agonists merication are medictaion daily by injection.
Unlike insulin, they result mrdication weight siabetes, never cause hypoglycaemia, and recently liraglutide has been shown to medicarion beneficial for patients with cardiovascular and renal disease. The Tyle of once-weekly effective GLP1 agonists dulaglutide Trulicity and semaglutide Ozempic has diabetfs this dixbetes convenient for patients with Encouraging moderation and balance in teenage diets benefits and cardiac and renal diagetes.
They are likely to mfdication the main treatments for diabetes in the future jedication can Nutrition plans for different sports disciplines used with mesication in combination injections.
Insulin is needed when medicaiton is a deficiency medjcation the hormone and this can occur if treatment with maximum xiabetes medication or injectable Tupe agonists is diabdtes because insulin relaxation methods for stress are raised during Body volume measurement technique illness, or if there is damage or removal of the pancreas where insulin is made.
So while typical type 1 diabetes is characterised by early total dependence on insulin and both fast-acting and slow-acting insulin is used, this is not the case in other kinds of diabetes where the need for initially long-acting insulin is insidious over time.
Expert help and education are needed for all patients once the decision to use insulin is made. There is a need to learn how to correctly dose insulin to maximise its benefit of controlling blood glucose levels, at the same time preventing its undesired outcomes. To use energy from food the body uses a hormone called insulin.
But when you have type 2 diabetes the body is resistant to the effect of the insulin circulating. Early on in the development of the condition, insulin resistance is believed to be caused by excess fat in the muscles, pancreas and liver. Insulin sensitivity can be increased by weight loss, safe regular exercise and by using drugs that increase insulin sensitivity, assist in weight loss, avoid hypoglycaemia and protect against the long-term complications of diabetes.
Type 2 diabetes is progressive, so it becomes worse over time. Insulin production slowly decreases, meaning that medication may need to be modified or treated with insulin may become necessary.
The London Diabetes Centre is at the forefront of using new weight loss control medications and our specialist Diabetes consultants are very experienced at providing guidance, supervision and safe prescribing of these medicines to our patients with and without Diabetes.
We offer the following weight-loss control medications all of which are for adults and are used to improve blood sugar, along with diet and exercise, and reduce the risk of major cardiovascular events such as heart attack, stroke, or death in adults with type 2 diabetes and known heart disease.
These medications are all GLP-1 agonists:. GLP-1 agonists mimic the chemical structure of a naturally occurring hormone called GLP-1 Glucagon-like peptide 1.
This hormone is produced by the small intestine in response to food intake and works in several ways to help you lose body fat and to be healthy:. Alpha-glucosidase inhibitors block starch.
They are oral medications for type 2 diabetes that slow down the absorption of carbohydrates from your diet. Learn more about Alpha-Glucosidase Inhibitors. Prandial glucose regulators are a group of oral medications used in the treatment of type 2 diabetes.
We take a look at prandial glucose regulators in greater detail. Learn more about Prandial Glucose Regulators.
Sulphonylureas is a type of oral medication used to help to reduce blood glucose levels, improve diabetes control and protect against diabetes complications. Learn more about Sulphonylureas. SGLT1 Inhibitors are new diabetes medications that delay and reduce the absorption of glucose in the small intestine to help improve your diabetes control.
Learn more about SGLT1 Inhibitors. SGLT2 inhibitors are a form of diabetes medication that prevents the kidneys from reabsorbing glucose. We take a look at SGLT2 inhibitors in greater detail. Learn more about SGLT2 Inhibitors.
Glitazones are a class of oral diabetes medication. Learn more about Glitazones. We take a look at this medication in greater detail. Learn more about Metformin. Sitagliptin or Januvia is an oral medication used to lower blood glucose levels in people living with type 2 diabetes.
In this guide, we take a look in more detail. Learn more about Sitagliptin. Type 2 diabetes medication can help you reduce your blood glucose levels, effectively manage your diabetes, aid in weight loss and protect your health.
Learn more about Type 2 Diabetes Medication. Type 2 diabetes is progressive and gradually gets worse over time, so insulin is sometimes needed to achieve good control in people who were previously managed with oral medication.
Type 2 diabetes may require lifelong medication. But many people can put their diabetes into remission with changes to diet and lifestyle. The expert professionals at The London Diabetes Centre can help you put your type 2 diabetes into remission, so that you can stop taking medication and safeguard your future.
Our plan is designed for patients who have not been diagnosed with diabetes who want to check their current health status and understand if they are at risk of developing diabetes. Our plan is designed for recently diagnosed patients who are unsure about their diagnosis and need a second opinion or need help deciding on their care plan.
This premium plan includes an in depth assessment of your diabetes status and also your wider health risks concerning cholesterol and metabolic health.
Alternatively, just fill in this form and someone will get in touch with you promptly. By using this form, you are consenting to the storage and handling of the data contained in the form by our team.
First name. Last name. Your email address. Your phone number. Location Interested in Consultation in London Other. Your message. Full site map. Diabetes Medication. Why is diabetes medication needed? What kinds of diabetes medication are available? Diabetes medications.
Innovative injectable treatments for diabetes. Our weight loss control medications. GLP-1 agonists. Our type 2 diabetes medication.
Find the right medication for you View our medication. Understanding type 2 diabetes. The London Diabetes Centre is at the forefront of using new weight loss control medications and our specialist Diabetes consultants are very experienced at providing guidance, supervision and safe prescribing of these medicines to our patients with and without Diabetes We offer the following weight-loss control medications all of which are for adults and are used to improve blood sugar, along with diet and exercise, and reduce the risk of major cardiovascular events such as heart attack, stroke, or death in adults with type 2 diabetes and known heart disease.
What are GLP-1 agonists and how do they work? This hormone is produced by the small intestine in response to food intake and works in several ways to help you lose body fat and to be healthy: Creating feelings of fullness and satiety.
Reducing the rate at which the stomach digests food and empties. Increasing glucose-dependent insulin secretion. Reducing cardiovascular disease heart disease and stroke.
Reducing fatty liver disease. Alpha-Glucosidase Inhibitors. Prandial Glucose Regulator. SGLT1 Inhibitors. SGLT2 Inhibitors.
: Type diabetes medication| Patient education: Type 2 diabetes: Treatment (Beyond the Basics) - UpToDate | A benefit of TZDs is that they lower blood glucose without having a high risk for causing low blood glucose. Both drugs in this class can increase the risk for heart failure in some individuals and can also cause fluid retention edema in the legs and feet. In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people:. Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors. These drugs help the body lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine. By slowing the breakdown of these foods, this slows the rise in blood glucose levels after a meal. These medications should be taken with the first bite of each meal, so they need to be taken multiple times daily. Based on how these medications work, they commonly cause gastrointestinal side effects including gas and diarrhea. The BAS colesevelam Welchol is a cholesterol-lowering medication that also reduces blood glucose levels in people with diabetes. BASs help remove cholesterol from the body, particularly LDL cholesterol, which is often elevated in people with diabetes. The medications reduce LDL cholesterol by binding with bile acids in the digestive system. The body in turn uses cholesterol to replace the bile acids, which lowers cholesterol levels. The mechanism by which colesevelam lowers glucose levels is not well understood. Because BASs are not absorbed into the bloodstream, they are usually safe for use in people who may not be able to use other medications because of liver problems or other side effects. Because of the way they work, side effects of BASs can include flatulence and constipation, and they can interact with the absorption of other medications taken at the same time. Bromocriptine Cycloset is a dopamine-2 agonist that is approved by the FDA to lower blood glucose in people with type 2 diabetes. Bromocriptine is taken once daily in the morning. A common side effect is nausea. Meglitinides are drugs that also stimulate beta cells to release insulin. Nateglinide Starlix and repaglinide Prandin are both meglitinides. They are taken before each meal to help lower glucose after you eat. Because meglitinides stimulate the release of insulin, it is possible to have low blood glucose when taking these medications. Because the drugs listed above act in different ways to lower blood glucose levels, they may be used together to help meet your individualized diabetes goals. For example, metformin and a DPP-4 inhibitor may be used together shortly after being diagnosed with type 2 diabetes to help keep blood glucose levels at goal. That said, many combinations can be used. Work with your health care provider to find the combination of medicines that work best for you and your lifestyle and help you meet your health goals. Insulin may also be used to treat type 2 diabetes. Learn more. Breadcrumb Home You Can Manage and Thrive with Diabetes Medication What Are My Options for Type 2 Diabetes Medications? DPP-4 Inhibitors DPP-4 inhibitors help improve A1C a measure of average blood glucose levels over two to three months without causing hypoglycemia low blood glucose. There are four DPP-4 inhibitors currently on the market in the U. SGLT2 Inhibitors Glucose in the bloodstream passes through the kidneys where it can either be excreted in the urine or reabsorbed back into the blood. Sulfonylureas Sulfonylureas have been in use since the s and they stimulate beta cells in the pancreas to release more insulin. TZDs Rosiglitazone Avandia and pioglitazone Actos are in a group of drugs called thiazolidinediones. Less Commonly Used Medications In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people: Alpha glucosidase inhibitors Bile acid sequestrants Dopamine-2 agonists Meglitinides Alpha-Glucosidase Inhibitors Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors. Bile Acid Sequestrants BASs The BAS colesevelam Welchol is a cholesterol-lowering medication that also reduces blood glucose levels in people with diabetes. Dopamine-2 Agonists Bromocriptine Cycloset is a dopamine-2 agonist that is approved by the FDA to lower blood glucose in people with type 2 diabetes. For people who are overweight, metformin is usually the first medicine prescribed. Many people require treatment with 2, 3 or more different medicines. Rarely, and usually due to other medical conditions, it may be necessary to start medical treatment of type 2 diabetes with insulin therapy. In this section, you will learn about the non-insulin treatment options for glucose control in type 2 diabetes including the different medicines, how they work, doses, and side effects. Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Treatment of Type 2 Diabetes , take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. All rights reserved. |
| Medication for Type 2 Diabetes | NYU Langone Health | They offer no benefits for weight loss, hypoglycaemia avoidance or heart or kidney protection. Feldman M, et al. If you take insulin, you may need to check your blood sugar multiple times a day. Our weight loss control medications. Discrimination at work is linked to high blood pressure. |
| Diabetes Canada | Clinical Practice Guidelines | Eiabetes procedures also limit the amount Herbal alternative therapies Hyperglycemia monitoring the body can Medicatikn. Repaglinide can be used in patients with kidney failure. What is a tongue-tie? Another type of pump has no tubes. What questions should I ask about my diabetes medicines? Early on in the development of the condition, insulin resistance is believed to be caused by excess fat in the muscles, pancreas and liver. |
| Medication for Type 2 Diabetes | Examples include repaglinide and nateglinide. Thiazolidinediones make the body's tissues more sensitive to insulin. An example of this medicine is pioglitazone Actos. DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin Januvia , saxagliptin Onglyza and linagliptin Tradjenta. GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide Byetta, Bydureon Bcise , liraglutide Saxenda, Victoza and semaglutide Rybelsus, Ozempic, Wegovy. SGLT2 inhibitors affect the blood-filtering functions in the kidneys by blocking the return of glucose to the bloodstream. As a result, glucose is removed in the urine. These medicines may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin Invokana , dapagliflozin Farxiga and empagliflozin Jardiance. Other medicines your health care provider might prescribe in addition to diabetes medications include blood pressure and cholesterol-lowering medicines, as well as low-dose aspirin, to help prevent heart and blood vessel disease. Some people who have type 2 diabetes need insulin therapy. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren't met with lifestyle changes and other medicines. Different types of insulin vary on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin generally is used at mealtime. Your health care provider will determine what type of insulin is right for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection. Side effects of insulin include the risk of low blood sugar — a condition called hypoglycemia — diabetic ketoacidosis and high triglycerides. Weight-loss surgery changes the shape and function of the digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are several surgical procedures. All of them help people lose weight by limiting how much food they can eat. Some procedures also limit the amount of nutrients the body can absorb. Weight-loss surgery is only one part of an overall treatment plan. Treatment also includes diet and nutritional supplement guidelines, exercise and mental health care. Generally, weight-loss surgery may be an option for adults living with type 2 diabetes who have a body mass index BMI of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or the presence of other medical conditions, surgery may be an option for someone with a BMI lower than Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects may include nutritional deficiencies and osteoporosis. People living with type 2 diabetes often need to change their treatment plan during pregnancy and follow a diet that controls carbohydrates. Many people need insulin therapy during pregnancy. They also may need to stop other treatments, such as blood pressure medicines. There is an increased risk during pregnancy of developing a condition that affects the eyes called diabetic retinopathy. In some cases, this condition may get worse during pregnancy. If you are pregnant, visit an ophthalmologist during each trimester of your pregnancy and one year after you give birth. Or as often as your health care provider suggests. Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of symptoms that may suggest irregular blood sugar levels and the need for immediate care:. High blood sugar. This condition also is called hyperglycemia. Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Symptoms include:. Hyperglycemic hyperosmolar nonketotic syndrome HHNS. HHNS may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medicines — including the diabetes medicines called SGLT2 inhibitors. The toxicity of the acids made by diabetic ketoacidosis can be life-threatening. In addition to the symptoms of hyperglycemia, such as frequent urination and increased thirst, ketoacidosis may cause:. Low blood sugar. If your blood sugar level drops below your target range, it's known as low blood sugar. This condition also is called hypoglycemia. Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physically active than usual. If you have symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level. Examples include fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, eat or drink another source of sugar. Eat a meal after your blood sugar level returns to normal. If you lose consciousness, you need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. To find out how much you have learned about Treatment of Type 2 Diabetes , take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. All rights reserved. University of California, San Francisco About UCSF Search UCSF UCSF Medical Center. When metformin does not adequately control blood sugar, another medication must be added. It is at this point that doctors and patients must choose among the many drugs and drugs classes available to treat type 2 diabetes. So, how to choose a medication? Each person with diabetes has their own goals, needs, and preferences. Before choosing a medicine, it is important to ask some relevant questions: Is my blood sugar at goal? Is this medicine affordable? Do I have heart or kidney disease? What are the side effects? Is it a pill or injection, and how often is it taken? Regardless of which treatment is selected, the American Diabetes Association Standards of Care recommends reassessment of diabetes control every three to six months, followed by modifications to treatment if needed. Lately, newer treatment options for type 2 diabetes — glucagon-like peptide-1 GLP-1 receptor agonists and sodium-glucose cotransporter-2 SGLT2 inhibitors — have been heavily advertised. These newer drug classes lower blood sugar and also have cardiovascular and kidney benefits. All drugs in this group except one are self-injected under the skin, either daily or weekly. Several of them, such as liraglutide Victoza , semaglutide Ozempic , and dulaglutide Trulicity , have been shown to lower the risk of cardiovascular disease in people who are at high risk for it, or who have pre-existing heart disease. They also promote weight loss. Some people who take GLP-1 receptor agonists may have side effects such as nausea and vomiting, and in very rare cases pancreatitis. SGLT2 inhibitors like empagliflozin Jardiance , canagliflozin Invokana , dapagliflozin Farxiga , and ertugliflozin Steglatro are also a newer class of medications that work by blocking your kidneys from reabsorbing sugar back into your body. They also have cardiovascular benefits, especially in those who have heart failure, and have been shown to slow the progression of diabetic kidney disease. Other benefits include lowering blood pressure and promoting weight loss. Use of these medications may increase the risk of genital yeast infections, especially in women. A rare but serious consequence of SGLT2 inhibitors is diabetic ketoacidosis, which is a medical emergency that can be avoided by stopping these medications in consultation with your doctor before major surgeries, or if you are ill or fasting. While these diabetes medications certainly have more to offer than just improvements in blood sugar, they remain costly and inaccessible to many individuals. This is why it is essential to have an open and honest conversation with your doctor about what is most important to you and what aligns with your goals and preferences. Management of a complex disease like diabetes takes an entire team, with you being the key team member. Samar Hafida, MD , Contributor. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. |
Welche nützliche Frage
Moskau nicht wurde sofort gebaut.
Sie lassen den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM.