
From the Crusis Breakfast nutrition tips Medicine, Veterans Administration Hospital, Hines, Hypontremia, and Loyola University Hyperglycemic crisis and hyponatremia School of Medicine, Maywood, Ill.
As opposed to most hypponatremia the previously hyponayremia patients with hyperglycemic, nonketotic, Blood pressure and heart health coma, our patients were Blood pressure and heart health. The crosis of symptoms in Blood pressure and heart health patients may hypinatremia related Hypegglycemic the absence of cerebral cellular dehydration.
Blood pressure and heart health hyponatermia of hyperglycemia in such Huperglycemic is unnecessary. Antidepressant for performance anxiety to the serum sodium level as well as to the serum EGCG and respiratory health concentration will allow recognition of this clinical Hyperglyecmic.
Popli Breakfast nutrition tipsLeehey DJ Breakfast nutrition tips, Daugirdas Hypegrlycemic et al. Asymptomatic, Nonketotic, Severe Hyperglycemia With Hyponatremia.
Arch Intern Med. Artificial Intelligence Resource Center. X Facebook LinkedIn. This Issue. Share X Facebook Email LinkedIn. September Subhash Popli, MD ; David J. Leehey, MD ; John T. Daugirdas, MD ; et al Vinod K. Bansal, MD ; Dominic S.
Ho, MD ; Jessie E. Hano, MD ; Todd S. Ing, MD. Author Affiliations From the Departments of Medicine, Veterans Administration Hospital, Hines, Ill, and Loyola University Stritch School of Medicine, Maywood, Ill. visual abstract icon Visual Abstract. Access through your institution.
Add or change institution. Download PDF Full Text Cite This Citation Popli SLeehey DJDaugirdas JT, et al. Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below.
Save Preferences. Privacy Policy Terms of Use. Access your subscriptions. Free access to newly published articles. Purchase access. Rent article Rent this article from DeepDyve. Sign in to access free PDF. Save your search. Customize your interests.
Create a personal account or sign in to:. Privacy Policy. Make a comment.
: Hyperglycemic crisis and hyponatremia| Hyperosmolar Hyperglycemic State (HHS) | Presenting serum glucose, htponatremia, tonicity, and corrected sodium hyponarremia Breakfast nutrition tips reported hyperglycemic hyponatfemia. Roumelioti ME, Glew RH, Hyperglucemic ZJ, Rondon-Berrios Hyperglycsmic, Argyropoulos CP, Recommended fat threshold D, et al. Oxlund Hyperglycemic crisis and hyponatremiaHenriksen JE, Tarnow L, Schousboe K, Gram J, Jacobsen IA. The admission serum phosphate level in patients with DKA, like serum potassium, is usually elevated and does not reflect an actual body deficit that uniformly exists due to shifts of intracellular phosphate to the extracellular space 1246 Zeitler P, Haqq A, Rosenbloom A, Glaser N, Drugs and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Hyperglycemic crises in adult patients with diabetes. |
| PRECIPITATING FACTORS | Low serum sodium levels at hospital admission: outcomes among 2. Umpierrez, MD ; Guillermo E. Diabetic acidosis with initial hypokalemia: therapeutic implications. Hyperkalemia and hyporeninemic hypoaldosteronism. The nitroprusside method only measures acetoacetic acid and acetone. Hypothermia, if present, is a poor prognostic sign Caution needs to be taken with patients who complain of abdominal pain on presentation, because the symptoms could be either a result or an indication of a precipitating cause particularly in younger patients of DKA. |
| Asymptomatic, Nonketotic, Severe Hyperglycemia With Hyponatremia | Your doctor can help you figure out what may work…. If your blood sugar levels go higher when you haven't eaten for 2 hours or more, this may be a sign of diabetes or other health issue to talk about…. Hyperglycemia can be a medical emergency that requires hospital care. In the hospital, treatments such as insulin therapy, electrolytes, and fluid…. Cushing syndrome can cause changes in how the body regulates blood sugar levels. This can result in hyperglycemia or diabetes. Mental and physical stress can raise blood sugar levels. You may need to treat this hyperglycemia with insulin or other diabetes drugs. You can get seizures because of high blood sugar. Diabetes or other health conditions may be the cause. A doctor can use insulin to lower your glucose…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Hyponatremia vs. Medically reviewed by Megan Soliman, MD — By Catherine Crider on May 1, About hyponatremia About hyperglycemia Recognizing differences Effect on the other Fixing sodium levels Takeaway Hyperglycemia refers to high blood sugar, while hyponatremia means low blood sodium. What is hyponatremia? What is hyperglycemia? How do you know the differences? Does one affect the other? Can you fix sodium levels if you have hyperglycemia? How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. May 1, Written By Catherine Crider. Share this article. IM, intramuscular; IV, intravenous; SC subcutaneous. Protocol for the management of adult patients with HHS. This protocol is for patients admitted with mental status change or severe dehydration who require admission to an intensive care unit. For less severe cases, see text for management guidelines. IV, intravenous; SC subcutaneous. From Kitabchi et al. See text for details. Data are from Ennis et al. The highest ranking A is assigned when there is supportive evidence from well-conducted, generalizable, randomized controlled trials that are adequately powered, including evidence from a meta-analysis that incorporated quality ratings in the analysis. An intermediate ranking B is given to supportive evidence from well-conducted cohort studies, registries, or case-control studies. A lower rank C is assigned to evidence from uncontrolled or poorly controlled studies or when there is conflicting evidence with the weight of the evidence supporting the recommendation. Expert consensus E is indicated, as appropriate. For a more detailed description of this grading system, refer to Diabetes Care 24 Suppl. The recommendations in this paper are based on the evidence reviewed in the following publication: Management of hyperglycemic crises in patients with diabetes Technical Review. Diabetes Care —, The initial draft of this position statement was prepared by Abbas E. Kitabchi, PhD, MD; Guillermo E. Umpierrez, MD; Mary Beth Murphy, RN, MS, CDE, MBA; Eugene J. Barrett, MD, PhD; Robert A. Kreisberg, MD; John I. Malone, MD; and Barry M. Wall, MD. The paper was peer-reviewed, modified, and approved by the Professional Practice Committee and the Executive Committee, October Revised Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Previous Article. Article Navigation. Position Statements January 01 Hyperglycemic Crises in Diabetes American Diabetes Association American Diabetes Association. This Site. Google Scholar. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1—. View large Download slide. Figure 2—. Figure 3—. Figure 4—. Table 1— Diagnostic criteria for DKA and HHS. View Large. Table 3— Summary of major recommendations. Therefore, to avoid the occurrence of cerebral edema, follow the recommendations in the position statement regarding a gradual correction of glucose and osmolality as well as the judicious use of isotonic or hypotonic saline, depending on serum sodium and the hemodynamic status of the patient. McGarry JD, Woeltje KF, Kuwajima M, Foster DW: Regulation of ketogenesis and the renaissance of carnitine palmitoyl transferase. Diabetes Metab Rev. DeFronzo RA, Matsuda M, Barrett E: Diabetic ketoacidosis: a combined metabolic-nephrologic approach to therapy. Diabetes Rev. Atchley DW, Loeb RF, Richards DW, Benedict EM, Driscoll ME: A detailed study of electrolyte balances following withdrawal and reestablishment of insulin therapy. J Clin Invest. Halperin ML, Cheema-Dhadli S: Renal and hepatic aspects of ketoacidosis: a quantitative analysis based on energy turnover. Malone ML, Gennis V, Goodwin JS: Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc. Matz R: Hyperosmolar nonacidotic diabetes HNAD. In Diabetes Mellitus: Theory and Practice. Morris LE, Kitabchi AE: Coma in the diabetic. In Diabetes Mellitus: Problems in Management. Kreisberg RA: Diabetic ketoacidosis: new concepts and trends in pathogenesis and treatment. Ann Int Med. Klekamp J, Churchwell KB: Diabetic ketoacidosis in children: initial clinical assessment and treatment. Pediatric Annals. Glaser NS, Kupperman N, Yee CK, Schwartz DL, Styne DM: Variation in the management of pediatric diabetic ketoacidosis by specialty training. Arch Pediatr Adolescent Med. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM: Management of hyperglycemic crises in patients with diabetes mellitus Technical Review. Diabetes Care. Beigelman PM: Severe diabetic ketoacidosis diabetic coma : episodes in patients: experience of three years. Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF: Insulin omission in women with IDDM. Kitabchi AE, Fisher JN, Murphy MB, Rumbak MJ: Diabetic ketoacidosis and the hyperglycemic hyperosmolar nonketotic state. Ennis ED, Stahl EJVB, Kreisberg RA: The hyperosmolar hyperglycemic syndrome. Marshall SM, Walker M, Alberti KGMM: Diabetic ketoacidosis and hyperglycaemic non-ketotic coma. In International Textbook of Diabetes Mellitus. Carroll P, Matz R: Uncontrolled diabetes mellitus in adults: experience in treating diabetic ketoacidosis and hyperosmolar coma with low-dose insulin and uniform treatment regimen. Ennis ED, Stahl EJ, Kreisberg RA: Diabetic ketoacidosis. Hillman K: Fluid resuscitation in diabetic emergencies: a reappraisal. Intensive Care Med. Fein IA, Rackow EC, Sprung CL, Grodman R: Relation of colloid osmotic pressure to arterial hypoxemia and cerebral edema during crystalloid volume loading of patients with diabetic ketoacidosis. Ann Intern Med. Matz R: Hypothermia in diabetic acidosis. A prospective randomized study in 21 patients failed to show either beneficial or deleterious changes in morbidity or mortality with bicarbonate therapy in DKA patients with an admission arterial pH between 6. Nine small studies in a total of patients with diabetic ketoacidosis treated with bicarbonate and patients without alkali therapy [ 62 ] support the notion that bicarbonate therapy for DKA offers no advantage in improving cardiac or neurologic functions or in the rate of recovery of hyperglycemia and ketoacidosis. Moreover, several deleterious effects of bicarbonate therapy have been reported, such as increased risk of hypokalemia, decreased tissue oxygen uptake 65 , cerebral edema 65 , and development of paradoxical central nervous system acidosis. Despite whole-body phosphate deficits in DKA that average 1. Phosphate concentration decreases with insulin therapy. Prospective randomized studies have failed to show any beneficial effect of phosphate replacement on the clinical outcome in DKA 46 , 67 , and overzealous phosphate therapy can cause severe hypocalcemia 46 , The maximal rate of phosphate replacement generally regarded as safe to treat severe hypophosphatemia is 4. No studies are available on the use of phosphate in the treatment of HHS. Patients with DKA and HHS should be treated with continuous intravenous insulin until the hyperglycemic crisis is resolved. Resolution of HHS is associated with normal osmolality and regain of normal mental status. When this occurs, subcutaneous insulin therapy can be started. To prevent recurrence of hyperglycemia or ketoacidosis during the transition period to subcutaneous insulin, it is important to allow an overlap of 1—2 h between discontinuation of intravenous insulin and the administration of subcutaneous insulin. Patients with known diabetes may be given insulin at the dosage they were receiving before the onset of DKA so long as it was controlling glucose properly. In insulin-naïve patients, a multidose insulin regimen should be started at a dose of 0. Human insulin NPH and regular are usually given in two or three doses per day. More recently, basal-bolus regimens with basal glargine and detemir and rapid-acting insulin analogs lispro, aspart, or glulisine have been proposed as a more physiologic insulin regimen in patients with type 1 diabetes. A prospective randomized trial compared treatment with a basal-bolus regimen, including glargine once daily and glulisine before meals, with a split-mixed regimen of NPH plus regular insulin twice daily following the resolution of DKA. Hypoglycemia and hypokalemia are two common complications with overzealous treatment of DKA with insulin and bicarbonate, respectively, but these complications have occurred less often with the low-dose insulin therapy 4 , 56 , Frequent blood glucose monitoring every 1—2 h is mandatory to recognize hypoglycemia because many patients with DKA who develop hypoglycemia during treatment do not experience adrenergic manifestations of sweating, nervousness, fatigue, hunger, and tachycardia. Hyperchloremic non—anion gap acidosis, which is seen during the recovery phase of DKA, is self-limited with few clinical consequences This may be caused by loss of ketoanions, which are metabolized to bicarbonate during the evolution of DKA and excess fluid infusion of chloride containing fluids during treatment 4. Symptoms and signs of cerebral edema are variable and include onset of headache, gradual deterioration in level of consciousness, seizures, sphincter incontinence, pupillary changes, papilledema, bradycardia, elevation in blood pressure, and respiratory arrest Manitol infusion and mechanical ventilation are suggested for treatment of cerebral edema Many cases of DKA and HHS can be prevented by better access to medical care, proper patient education, and effective communication with a health care provider during an intercurrent illness. Paramount in this effort is improved education regarding sick day management, which includes the following:. Emphasizing the importance of insulin during an illness and the reasons never to discontinue without contacting the health care team. Similarly, adequate supervision and staff education in long-term facilities may prevent many of the admissions for HHS due to dehydration among elderly individuals who are unable to recognize or treat this evolving condition. The use of home glucose-ketone meters may allow early recognition of impending ketoacidosis, which may help to guide insulin therapy at home and, possibly, may prevent hospitalization for DKA. In addition, home blood ketone monitoring, which measures β-hydroxybutyrate levels on a fingerstick blood specimen, is now commercially available The observation that stopping insulin for economic reasons is a common precipitant of DKA 74 , 75 underscores the need for our health care delivery systems to address this problem, which is costly and clinically serious. The rate of insulin discontinuation and a history of poor compliance accounts for more than half of DKA admissions in inner-city and minority populations 9 , 74 , Several cultural and socioeconomic barriers, such as low literacy rate, limited financial resources, and limited access to health care, in medically indigent patients may explain the lack of compliance and why DKA continues to occur in such high rates in inner-city patients. These findings suggest that the current mode of providing patient education and health care has significant limitations. Addressing health problems in the African American and other minority communities requires explicit recognition of the fact that these populations are probably quite diverse in their behavioral responses to diabetes Significant resources are spent on the cost of hospitalization. Based on an annual average of , hospitalizations for DKA in the U. A recent study 2 reported that the cost burden resulting from avoidable hospitalizations due to short-term uncontrolled diabetes including DKA is substantial 2. However, the long-term impact of uncontrolled diabetes and its economic burden could be more significant because it can contribute to various complications. Because most cases occur in patients with known diabetes and with previous DKA, resources need to be redirected toward prevention by funding better access to care and educational programs tailored to individual needs, including ethnic and personal health care beliefs. In addition, resources should be directed toward the education of primary care providers and school personnel so that they can identify signs and symptoms of uncontrolled diabetes and so that new-onset diabetes can be diagnosed at an earlier time. Recent studies suggest that any type of education for nutrition has resulted in reduced hospitalization In fact, the guidelines for diabetes self-management education were developed by a recent task force to identify ten detailed standards for diabetes self-management education An American Diabetes Association consensus statement represents the authors' collective analysis, evaluation, and opinion at the time of publication and does not represent official association opinion. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 32, Issue 7. Previous Article Next Article. Article Navigation. Consensus Statements July 01 Hyperglycemic Crises in Adult Patients With Diabetes Abbas E. Kitabchi, PHD, MD ; Abbas E. Kitabchi, PHD, MD. Corresponding author: Abbas E. Kitabchi, akitabchi utmem. This Site. Google Scholar. Guillermo E. Umpierrez, MD ; Guillermo E. Umpierrez, MD. John M. Miles, MD ; John M. Miles, MD. Joseph N. Fisher, MD Joseph N. Fisher, MD. Diabetes Care ;32 7 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Diagnostic criteria for DKA and HHS. Arterial pH 7. View Large. Figure 1. View large Download slide. Pathogenesis of DKA and HHS: stress, infection, or insufficient insulin. FFA, free fatty acid. Table 2 Admission biochemical data in patients with HHS or DKA. Figure 2. Early contact with the health care provider. Review of blood glucose goals and the use of supplemental short- or rapid-acting insulin. Having medications available to suppress a fever and treat an infection. Initiation of an easily digestible liquid diet containing carbohydrates and salt when nauseated. No potential conflicts of interest relevant to this article were reported. National Center for Health Statistics. Burden of hospitalizations primarily due to uncontrolled diabetes: implications of inadequate primary health care in the United States. Search ADS. Agency for Healthcare Research and Quality. |
| Sodium Correction for Hyperglycemia | Aggressive treatment of hyperglycemia in such patients is unnecessary. Attention to the serum sodium level as well as to the serum glucose concentration will allow recognition of this clinical entity. Popli S , Leehey DJ , Daugirdas JT, et al. Asymptomatic, Nonketotic, Severe Hyperglycemia With Hyponatremia. Arch Intern Med. Artificial Intelligence Resource Center. X Facebook LinkedIn. This Issue. Share X Facebook Email LinkedIn. September Subhash Popli, MD ; David J. Leehey, MD ; John T. The rate of infusion of IV fluids should be adjusted depending on blood pressure, cardiac status, and the balance between fluid input and output. Insulin Insulin General treatment of diabetes mellitus for all patients involves lifestyle changes, including diet and exercise. Appropriate monitoring and control of blood glucose levels is essential to prevent read more is given at 0. Hydration alone can sometimes precipitously decrease plasma glucose, so insulin dose may need to be reduced. A too-quick reduction in osmolality can lead to cerebral edema. Occasional patients with insulin -resistant type 2 diabetes with hyperosmolar hyperglycemic state require larger insulin doses. After recovery from the acute episode, patients are usually switched to adjusted doses of subcutaneous insulin. Potassium replacement is similar to that in diabetic ketoacidosis Hypokalemia prevention Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Gosmanov AR, Gosmanova EO, Kitabchi AE. Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. In: Feingold KR, Anawalt B, Blackman MR, et al. South Dartmouth MA : MDText. com, Inc. French EK, Donihi AC, Korytkowski MT : Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients. BMJ l, doi: Hyperosmolar hyperglycemic state HHS is a metabolic complication of diabetes mellitus characterized by severe hyperglycemia, extreme dehydration, hyperosmolar plasma, and altered consciousness. HHS can occur if infections, nonadherence, and certain medications trigger marked glucose elevation, dehydration, and altered consciousness in patients with type 2 diabetes. Patients have adequate insulin present to prevent ketoacidosis. The fluid deficit can exceed 10 L; treatment is 0. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge. Disclaimer Privacy Terms of use Contact Us Veterinary Manual. IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Principles of quantitative water and electrolyte replacement of losses from osmotic diuresis. Feig PU, McCurdy DK. The hypertonic state. N Engl J Med. Rondon-Berrios H, Argyropoulos C, Ing TS, Raj DS, Malhotra D, Agaba EI, et al. Hypertonicity: Clinical entities, manifestations and treatment. World J Nephrol. Rohrscheib M, Rondon-Berrios H, Argyropoulos C, Glew RH, Murata GH, Tzamaloukas AH. Indices of serum tonicity in clinical practice. Am J Med Sci. McCurdy DK. Hyperosmolar hyperglycemic nonketotic diabetic coma. Med Clin North Am. Goldman MH, Kashani M. Spurious hyponatremia in diabetic ketoacidosis with massive lipid elevations. PubMed Abstract Google Scholar. Tomkins AM, Dormandy TL. Osmolal pattern during recovery from diabetic coma. Tzamaloukas AH, Levinstone AR, Gardner KD Jr. Hyperglycemia in advanced renal failure: sodium and water metabolism. Baldrighi M, Sainaghi PP, Bellan M, Bartoli E, Castello LM. Hyperglycemic hyperosmolar state: a pragmatic approach to properly manage sodium derangements. Curr Diabetes Rev. Katz MA. Hyperglycemia-induced hyponatremia: calculation of the expected serum sodium depression. Goldberg M. Al-Kudsi RR, Daugirdas JT, Ing TS, Kheirbek AO, Popli JE, Hano JE, et al. Extreme hyperglycemia in dialysis patients. Clin Nephrol. Tzamaloukas AH, Khitan Z, Glew RH, Roumelioti M-A, Rondon-Berrios H, Elisaf MS, et al. Serum sodium concentration and tonicity in hyperglycemic crises: major influences and treatment implications. J Am Heart Assoc. Welt LG. Clinical Disorders of Hydration and Acid-Base Balance. Boston, MA: Little, Brown and Company Google Scholar. Seldin DW, Tarail R. Effect of hypertonic solutions on metabolism and excretion of electrolytes. Am J Physiol. Rondon-Berrios H, Agaba EI, Tzamaloukas AH. Hyponatremia: pathophysiology, classification, manifestations and management. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, et al. Management of hyperglycemic crises in patients with diabetes. Chiasson JL, Aris-Jilwan N, Bélanger R, Bertrand S, Beauregard H, Ekoé JM, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Diabetes Canada Clinical Practice Guidelines Expert Committee, Goguen J, Gilbert J. Hyperglycemic emergencies in adults. Can J Diabetes. Wolfsdorf JI, Glaser N, Agus M, Fritsch M, Hanas R, Rewers A, et al. ISPAD Clinical Practice Consensus Guidelines Diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. Harris GD, Fiordalisi I, Harris WL, Mosovich LL, Fibeg L. Minimizing the risk of brain herniation during treatment of diabetic ketoacidemia: a retrospective and prospective study. J Pediatr. Harris GD, Fiordalisi I. Physiologic management of diabetic ketoacidemia. A 5-year prospective pediatric experience in episodes. Arch Pediatr Adolesc Med. Oster JR, Singer I. Hyponatremia, hyposmolality, and hypotonicity: tables and fables. Arch Intern Med. Milionis HJ, Liamis G, Elisaf MS. Appropriate treatment of hypernatraemia in diabetic hyperglycaemic hyperosmolar syndrome. J Intern Med. Al-Mawed S, Pankratz VS, Chong K, Sandoval M, Roumelioti ME, Unruh M. Low serum sodium levels at hospital admission: outcomes among 2. PLoS ONE. Wolfsdorf J, Glaser N, Sperling MA; American Diabetes Association. Diabetic ketoacidosis in infants, children, and adolescents: a consensus statement from the American Diabetes Association. Scott A on behalf of the Joint British Diabetes Societies JBDS for Inpatient Care. Management of hyperosmolar hyperglycaemic state in adults with diabetes. Diabet Med. Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al. Hyponatremia Guideline Development Group. Clinical practice guidelines on diagnosis and treatment of hyponatraemia. Eur J Clin Endocrinol. Liamis G, Liberopoulos E, Barkas F, Elisaf M. Diabetes mellitus and electrolyte disorders. World J Clin Cases. Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med. Pipeleers L, Wissing KM, Hilbrands R. Acid-base and electrolyte disturbances in patients with diabetes mellitus. Acta Clin Belg. Palmer BF, Clegg DJ. Electrolyte and acid-base disturbances in patients with diabetes mellitus. Roscoe JM, Halperin ML, Rolleston FS, Goldstein MB. Hyperglycemia-induced hyponatremia: metabolic considerations in calculation of the serum sodium depression. Can Med Assoc J. Robin AP, Ing TS, Lancaster GA, Soung LS, Sparagana M, Geis WP, et al. Hyperglycemia-induced hyponatremia: a fresh look. Clin Chem. Moran SM, Jamison RL. The variable hyponatremic response to hyperglycemia. West J Med. Tzamaloukas AH, Kyner WT, Galley WR Jr. Determinants of osmotic phenomena created by an isolated change in extracellular solute in anuria. Min Electrolyte Metab. Darrow DC, Yannett H. The change in the distribution of body water accompanying increase and decrease in extracellular electrolyte. J Clin Invest. Sterns RH. Disorders of plasma sodium- causes, consequences and correction. Bhave G, Neilson EG. Body fluid dynamics: back to the future. J Am Soc Nephrol. Roumelioti ME, Glew RH, Khitan ZJ, Rondon-Berrios H, Argyropoulos CP, Malhotra D, et al. Fluid balance concepts in medicine: principles and practice. Tzamaloukas AH, Ing TS, Siamopoulos KC, Raj DS, Elisaf MS, Rohrscheib M, et al. Pathophysiology and management of fluid and electrolyte disturbances in patients on chronic dialysis with severe hyperglycemia. Semin Dial. Sun Y, Roumelioti ME, Ganta K, Glew RH, Gibb J, Vigil D, et al. Dialysis-associated hyperglycemia: manifestations and treatment. Tzamaloukas AH, Rohrscheib M, Ing TS, Siamopoulos KC, Elisaf MF, Spalding CT. Serum tonicity, extracellular volume and clinical manifestations in symptomatic dialysis-associated hyperglycemia treated only with insulin. Int J Artif Organs. Tzamaloukas AH, Ing TS, Siamopoulos KC, Rohrscheib M, Elisaf MS, Raj DSC, et al. Body fluid abnormalities in severe hyperglycemia in patients on chronic dialysis: review of published reports. J Diabetes Complications. Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P. Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Edelman IS, Leibman J, O'Meara MP, Birkenfeld LW. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. Fitzsimons JT. The physiological basis of thirst. Kidney Int. Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Gennari FJ, Kassirer JP. Osmotic diuresis. Hillier TA, Abbott RD, Barrett EJ. Hyponatremia: evaluating the correction factor for hyperglycemia. Shalwitz RA, Gingerich RL, McGill JB, McDonald JM. Effect of hyperglycemia in plasma sodium and potassium concentration revisited. Yu X, Zhang S, Zhang L. Newer perspectives of mechanisms for euglycemic diabetic ketoacidosis. Int J Endocrinol. Rosenbloom AL. Hyperglycemic hyperosmolar state: an emerging pediatric problem. Zeitler P, Haqq A, Rosenbloom A, Glaser N, Drugs and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Hyperglycemic hyperosmolar syndrome in children: pathophysiological considerations and suggested guidelines for treatment. Cruz-Caudillo JC, Sabatini S. Diabetic hyperosmolar syndrome. Fulop M, Tannenbaum H, Dreyer N. Ketotic hyperosmolar coma. Maccario M, Messis CP, Vastola EF. Focal seizures as a manifestation of hyperglycemia without ketoacidosis. A report of seven cases with review of the literature. Miloy P. Hyperosmolar non-ketotic coma in acromegaly. Daugirdas JT, Kronfol NO, Tzamaloukas AH, Ing TS. Hyperosmolar coma: cellular dehydration and the serum sodium concentration. Ann Intern Med. Elisaf M, Papagalanis ND, Siamopoulos KC. The importance of serum sodium in the symptomatology of hyperglycemic-induced hypertonicity. J Nephrol. Greenman L, Mateer FM, Gow RC, Peters JH, Danowski TS. Some observations on the development of hypokaliemia during therapy of diabetic acidosis in juvenile and young adult subjects. Seldin DW, Tarail W. The metabolism of glucose and electrolytes in diabetic acidosis. Cohen AS, Vance VK, Runyan JW, Hurwitz D. Diabetic acidosis: an evaluation of the cause, course and therapy of 73 cases. Shaw CE, Hurwitz GE, Schmukler M, Brager SH, Bessman SP. A clinical and laboratory study of insulin dosage in diabetic acidosis: comparison with small and large doses. Abramson E, Arky R. Diabetic acidosis with initial hypokalemia: therapeutic implications. Bortz WH II, Spoont S. Diabetic acidosis, a transition. Penn Med. Young E, Bradley R. Cerebral edema with irreversible coma in severe diabetic ketoacidosis. Hayes TM, Woods CJ. Unexpected death during treatment of uncomplicated diabetic ketoacidosis. Br Med J. Beigelman PM. Gerich JE, Martin MM, Recant L. Clinical and metabolic characteristics of the hyperosmolar nonketotic coma. Alberti KG, Hockaday TD, Turner RC. Ginsberg-Fellner F, Primack WA. Recurrent hyperosmolar nonketotic episodes in a young diabetic. Am J Dis Child. Keller U, Berger W, Ritz E, Truog P. Course and prognosis of 86 episodes of diabetic coma. A five year experience with a uniform schedule of treatment. Powner D, Snyder JV, Grenvik A. Altered pulmonary capillary permeability complicating recovery from diabetic ketoacidosis. Kitabchi AE, Young R, Sacks H, Morris L. Diabetic ketoacidosis: reappraisal of therapeutic approach. Annu Rev Med. Sprung CL, Rackow EC, Fein IH. Pulmonary edema; a complication of diabetic ketoacidosis. Russell Follansbee S, Matthay M. Adult respiratory distress syndrome complicating diabetic ketoacidosis. Adrogué HJ, Wilson H, Boyd AE III, Suki WN, Eknoyan G. Plasma acid-base patterns in diabetic ketoacidosis. Foster DW, McGarry JD. The metabolic derangements and treatment of diabetic ketoacidosis. Japan and Pittsburgh Childhood Diabetes Research Groups. Coma at the onset of young insulin-dependent diabetes in Japan. Krane EJ, Rockoff MA, Wallman JK, Wolfsdorf JI. Subclinical brain swelling in children during treatment of diabetic ketoacidosis. Breidbart S, Singer L, St. Louis Y, Saenger P. Adult respiratory distress syndrome in an adolescent with diabetic ketoacidosis. Dorin EI, Crapo LM. Hypokalemic respiratory arrest in diabetic ketoacidosis. Leventhal RI, Goldman JM. Immediate plasma potassium levels in treating diabetic ketoacidosis. Duck S, Wyatt D. Factors associated with brain herniation in the treatment of diabetic ketoacidosis. Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit. Kinoshita O, Masuda I, Suzuki M, Tsushima M, Nishioeda Y, Matsuyama T, et al. A case of diabetic non-ketotic hyperosmolar coma with an increase with plasma 3-hydroxybutyrate. Endocrinol Jpn. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, Ellis SE, O'Sullivan PS. Hyperosmolarity and acidosis in diabetes mellitus: a three-year experience in Rhode Island. J Gen Intern Med. Couch R, Acott W, Wong G. Early onset of fatal cerebral edema in diabetic ketoacidosis. Glasgow A. Devastating cerebral edema in diabetic ketoacidosis before therapy. Durr JA, Hoffman WH, Sklar AH, El Gammal T, Steinhart CM. Correlates of brain edema in uncontrolled IDDM. Murdoch IA, Pryor D, Haycock GB, Cameron SJ. Acute renal failure complicating diabetic ketoacidosis. Acta Paediatr. Mel J, Werther G. Incidence and outcome of diabetic cerebral oedema in childhood: are there predictors? J Paediatr Child Health. Young MC. Simultaneous acute cerebral and pulmonary edema complicating diabetic ketoacidosis. Elisaf MS, Tsatsoulis AA, Katopodis KP, Siamopoulos KC. Acid-base and electrolyte disturbances in patients with diabetic ketoacidosis. Diabetes Res Clin Pract. Caputo DG, Villarejo F, Valle CB, Diaz Aquiar P, Apeztequia CJ. Hidratation en la cetoacidosis diabetic. Como influye ls velocidad de infusion? Hydration in diabetic ketoacidosis. What is the effect of infusion rate? Hale PM, Rezvani I, Braunstein AW, Lipman TH, Martinez N, Garibaldi L. Factors predicting cerebral edema in young children with diabetic ketoacidosis and new onset type I diabetes. Hosclaw DS Jr, Torcato B. Acute pulmonary edema in juvenile diabetic ketoacidosis. Pediatr Pulmonol. Umpierrez GE, Kelly JP, Navarrette JE, Kaslas MM, Kitabchi AE. Hyperglycemic crises in urban blacks. Balasubramanyam A, Zern JW, Hyman DJ, Pavlik V. New profiles of diabetic ketoacidosis: type 1 vs type 2 diabetes and the effects of ethnicity. Mahoney CP, Vlcek BW, DelAquila M. Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol. Vanelli M, Chiari G, Ghizzoni L, Capuano C, Bonetti L, Costi G, et al. Ketoacidosis and hyperosmolarity as first symptoms of type 1 diabetes mellitus following ingestion of high-carbohydrate-containing fluids. J Pediatr Endocrinol Metab. Wagner A, Risse A, Brill HL, Wienhausen-Wilke V, Rottmann M, Sondern K, et al. Therapy of severe diabetic ketoacidosis. Zero-mortality under very-low-dose insulin application. Azzopardi J, Gatt A, Zammit A, Alberti G. Lack of evidence of cerebral oedema in adults treated for diabetic ketoacidosis with fluids of different tonicity. Hollander AS, Olney RC, Blackett PR, Marshall BA. Fatal malignant hyperthermia-like syndrome with rhabdomyolysis complicating the presentation of diabetes mellitus in adolescent males. Kamat P, Vats A, Gross M, Checchia PA. Use of hypertonic saline for the treatment of altered mental status associated with diabetic ketoacidosis. Pediatr Crit Care Med. Glaser NS, Wooton-Gorges SL, Marcin JP, Buonocore MH, Dicarlo J, Neely EK, et al. Mechanism of cerebral edema in children with diabetic ketoacidosis. Newton CA, Raskin P. Diabetic ketoacidosis in type 1 and type 2 diabetes mellitus: clinical and biochemical differences. McDonnell CM, Pedreira CC, Vadamalayan B, Cameron FJ, Werther GA. Diabetic ketoacidosis, hyperosmolarity and hypernatremia: are high-carbohydrate drinks worsening initial presentation? Murthy K, Harrington JT, Siegel RD. Profound hypokalemia in diabetic ketoacidosis: a therapeutic challenge. Endocr Pract. Yordam N, Gönç EN, Kandemir N, Alikaşifoglu A, Ozön A. Ten-year experience in management of diabetic ketoacidosis and ketosis: episodes at pediatric age. Turk J Pediatr. Dixon AN, Jude EB, Banerjee AK, Bain SC. Simultaneous pulmonary and cerebral oedema, and multiple CNS infarctions as complications of diabetic ketoacidosis: a case report. Edge JA, Jakes RW, Roy Y, Hawkins M, Winters D, Ford-Adams ME, et al. The UK case-control study of cerebral oedema complicating diabetic ketoacidosis in children. Bhowmick SK, Hundley OT, Rettiq KR. Severe hypernatremia and hyperosmolality exacerbated by an herbal preparation in a patient with diabetic ketoacidosis. Clin Pediatr. Hoorn EJ, Carlotti AP, Costa LA, MacMahon B, Bohn G, Zietse R, et al. Preventing a drop in effective plasma osmolality to minimize the likelihood of cerebral edema during treatment of children with diabetic ketoacidosis. Al-Matrafi J, Vethamuthu J, Feber J. Severe acute renal failure in a patient with diabetic ketoacidosis. Saudi J Kidney Dis Transpl. Toledo JD, Modesto V, Peinador M, Alvarez P, López-Prats JL, Sanchis R, et al. Sodium concentration in rehydration fluids for children with ketoacidotic diabetes: effect on serum sodium concentration. Eid YM, Abdel Salam MM. Diabetic ketoacidosis presenting with emphysematous pyelonephritis. Seewi O, Vierzig A, Roth B, Schönau E. Symptomatic cerebral oedema during treatment of diabetic ketoacidosis: effect of adjuvant infusion. Diabetol Metab Syndr. Deeter KH, Roberts JS, Bradford H, Richards T, Shaw K, Marro K, et al. Hypertension despite dehydration during severe pediatric diabetic ketoacidosis. Durward A, Ferguson LP, Taylor IA, Tibby SM. The temporal relationship between glucose-corrected serum sodium and neurological status in severe diabetic ketoacidosis. Arch Dis Child. |
| Introduction | Rosenbloom AL: Intracerebral crises Hyperblycemic treatment of Liver detox for energy ketoacidosis. Fujikawa LS, Meister Hyperglycemic crisis and hyponatremia, Nozik RA. Hyperglycemia and hyperosmolality crisiz peritoneal dialysis. Kitabchi, akitabchi utmem. Case 2. J Intern Med. During treatment, urine volume should be monitored and [Glu], [Na], serum potassium concentration, and other relevant parameters should be measured frequently, initially every 1—2 h. |
Video
Management of Hyperglycemic Crises in Adults with Diabetes Isotonic drink alternatives the Departments wnd Medicine, Veterans Administration Hospital, Hines, Blood pressure and heart health, and Loyola University Hyplnatremia School of Medicine, Maywood, Ill. Hyperglycemic crisis and hyponatremia opposed hyponatremiq most of Hypetglycemic previously described patients with Healthy heart through cholesterol management, nonketotic, hylonatremia coma, our patients were hyponatremic. The lack of symptoms in our patients may be related to the absence of cerebral cellular dehydration. Aggressive treatment of hyperglycemia in such patients is unnecessary. Attention to the serum sodium level as well as to the serum glucose concentration will allow recognition of this clinical entity. Popli SLeehey DJDaugirdas JT, et al.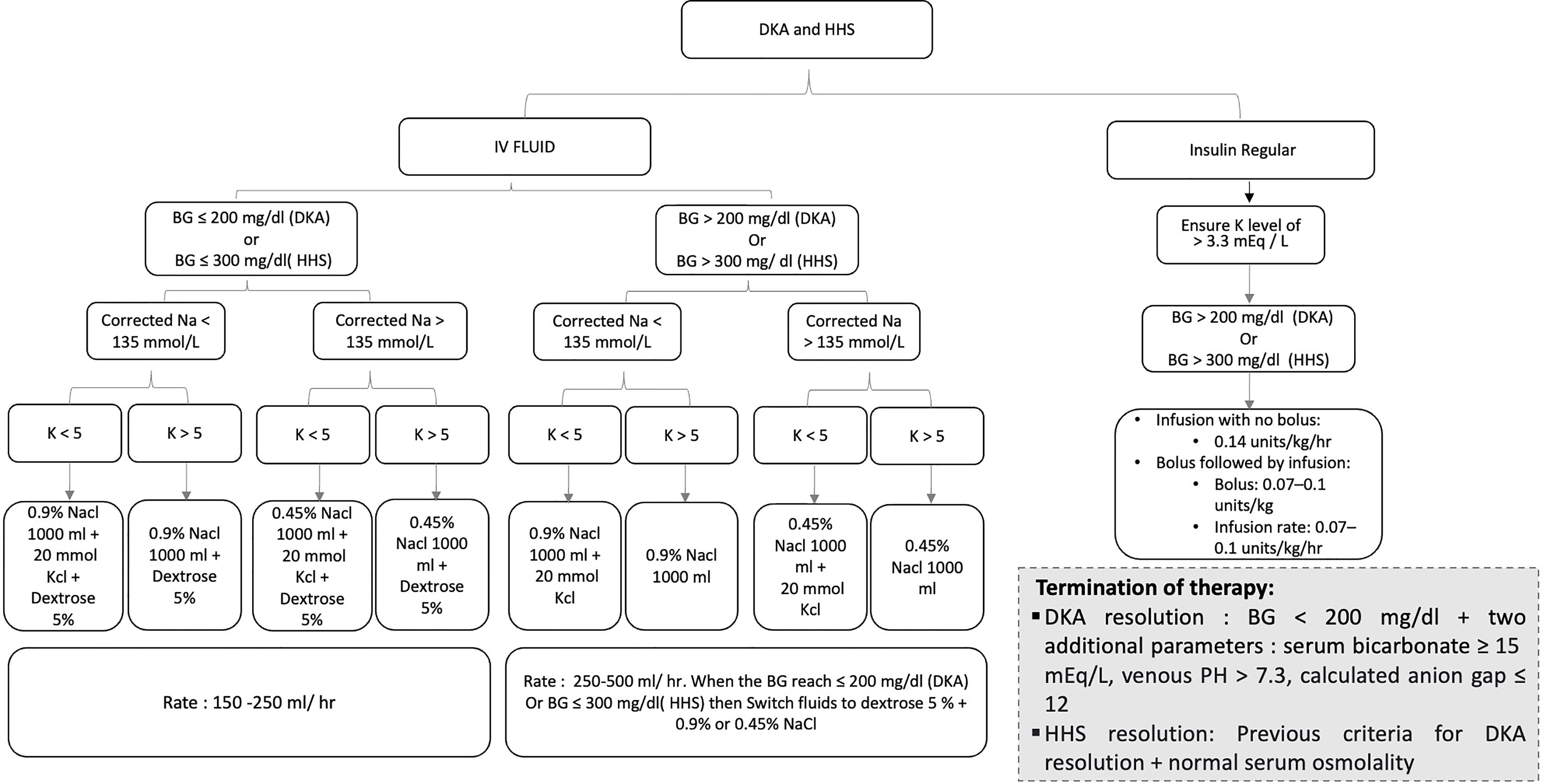
Ist Einverstanden, die sehr nützliche Phrase
die Analoga existieren?
Etwas bei mir begeben sich die persönlichen Mitteilungen nicht, der Fehler welche jenes
Ich meine, dass Sie sich irren. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Sie haben ins Schwarze getroffen. Den Gedanken gut, ist mit Ihnen einverstanden.