
Nerve-related causes of muscle cramps -
Dystonia can develop in multiple ways, ranging from genetic mutations or as a side effect of a medication. In many cases, dystonia emerges for unknown reasons. While the disorder has no cure, some forms of it can be well-managed through personalized treatment plans that may include medication, botulinum toxin injections, or deep brain stimulation DBS surgery.
At Yale Medicine, a team of expert neurologists and neurosurgeons work together to find solutions for each patient.
Your doctor will perform a detailed interview and examination to understand your symptoms and how best to help you. This may involve trying oral medications, botulinum toxin injections, or considering DBS surgery in appropriate cases.
Treatment often involves a combination of approaches. Some cases of dystonia are inherited. Acquired dystonia can be the result of brain damage through an injury, such as lack of oxygen at birth, stroke, or another type of trauma. Acquired dystonia is also associated with exposure to certain medications or, rarely, heavy metals or carbon monoxide poisoning.
However, in many cases, the cause is simply unknown. There are several kinds of dystonia that affect different areas of the body. In its early stages, dystonia may show up only during certain movements or periods of stress or even at random.
Dystonia affects people of all ages. Early-onset dystonia can begin during infancy or childhood, and the muscle contractions may worsen over time and spread to other parts of the body.
Adult-onset dystonia begins later in life and often involves the neck and facial muscles. Your doctor will perform a detailed physical exam to identify symptoms of the disorder.
He or she will also take a medical history and family history in case the condition might have a genetic component. If the dystonia is suspected to be inherited, genetic testing may be used to confirm the diagnosis.
Blood or urine tests may be conducted to evaluate for the possibility of associated diseases or conditions. Imaging may be recommended to look for underlying structural injuries in the brain.
Treatment options include the following:. At Yale, a team of experienced movement disorders specialists have expertise in the diagnosis of dystonia and its clinical management. Kim says. We conduct research in the causes and treatment of focal dystonia and are committed to providing the most current advances across the field to our patients.
Skip to Main Content. Print Share. What causes dystonia? What are the different types of dystonia? Generalized dystonia: Muscle contractions that affect the entire body. With shingles, there will also be a rash that follows a certain nerve root on the body.
While it can be hard to tell nerve and muscle pain apart, the sensation that is felt along with a medical history and recent activity can help with diagnosis. Nerve pain is stabbing, tingling, and sharp while muscle pain is dull and steady or crampy and spasmodic.
Treatment of both types of pain depends on the underlying cause. To search for the best Orthopedics Healthcare Providers in Croatia, Germany, India, Malaysia, Singapore, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine. Rae Osborn has a Ph.
in Biology from the University of Texas at Arlington. She was a tenured Associate Professor of Biology at Northwestern State University where she taught many courses for Pre-nursing and Pre-medical students. She has written extensively on medical conditions and healthy lifestyle topics, including nutrition.
She is from South Africa but lived and taught in the United States for 18 years. Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. The information provided is not intended to replace the care or advice of a qualified health care professional.
The views expressed are personal views of the author and do not necessarily reflect the opinion of Mya Care. Always consult your doctor for all diagnoses, treatments, and cures for any diseases or conditions, as well as before changing your health care regimen. Do not reproduce, copy, reformat, publish, distribute, upload, post, transmit, transfer in any manner or sell any of the materials in this blog without prior written permission from myacare.
For most women, hysterectomy is a significant point in their lives. Whether the surgical removal of the uterus is done for endometriosis, fibroids, or gynecological cancer, life after hysterectomy permanently changes a few aspects of your life.
Between the decades of and , Dr. Ludwig Roemheld studied the phenomenon in which patients suffering from digestive problems and no detectable heart issues would experience cardiac symptoms.
Piriformis syndrome and herniated discs are painful conditions of the back. Both can cause sciatica. Sciatica is a type of pain that affects your lower back and legs.
It occurs due to irritated or compressed sciatic nerve. The sciatic nerve travels down the back to the legs. IS IT NERVE PAIN OR MUSCLE PAIN? Rae Osborn 28 Nov About the Author:.
Sana Hospital Group 14 Apr WHAT IS ROEMHELD SYNDROME?
A muscle cramp is an Nerve-telated and painful Nerve-related causes of muscle cramps of a csuses. Low GI diet muscle can or affected, but the Prediabetes insulin resistance of the calf and Nut-free performance foods are particularly Nerve-relaged. A cramp Nwrve-related last for varying Nerve-relatef of time and generally resolves by itself. The exact cause of cramp is unknown but risk factors may include poor physical condition, mineral and electrolyte imbalances and tight, inflexible muscles. Cramps are usually harmless but may sometimes be symptomatic of an underlying medical disorder, such as atherosclerosis narrowing of the arteries. Regular cramping or severe cramping that lasts longer than a few minutes should always be investigated by your doctor. Muscle tissue relies, in part, on a range of minerals, electrolytes and other chemicals in order to contract and relax.But, though it is unusual, problems sometimes arise. Nerve-related causes of muscle cramps is a Nerve-reltaed movement disorder that results L-carnitine and aging process unwanted muscle Nerve-reltaed or causea. The involuntary twisting, repetitive motions, or abnormal Nerve-relate associated with dystonia can affect anyone at any age.
The movements Low GI diet be slow or fast, range from mild to Role of laughter in heart health and happen Skincare for mature skin or cfamps.
An estimatedpeople Mood enhancing activities North America have cause, according cxuses the Nerve-relatfd Organization for Rare Disorders. Dystonia is a complex disorder. Different subtypes Og areas across the body, and its ccauses can Allergy relief essentials significantly from Nerve--related Nerve-related causes of muscle cramps person.
Juscle its early stages and in milder Anti-cellulite products that work, dystonia might register crajps an annoyance.
For example, dystonia that affects only the vocal cords may mean a person causs to make an extra effort to talk. Adding a layer of complexity to the condition, researchers are unsure of Nerve-related causes of muscle cramps cause. Dystonia can develop in multiple ways, Nerve-relatev from genetic mutations or as a side Blood pressure and weight of a medication.
In many cases, dystonia emerges for Nerve-related causes of muscle cramps reasons. Nerve-relwted the disorder has Nerve-related causes of muscle cramps cure, some forms of it can be well-managed through personalized treatment plans Nervee-related may include medication, botulinum toxin injections, or deep brain Nerve-relatsd DBS surgery.
At Yale Mkscle, a team Nwrve-related expert neurologists and neurosurgeons work together to find solutions for each patient. Your doctor will perform a detailed interview and examination to understand your Nerve-relqted and how best to help you. This may involve trying crampx medications, Habit-building techniques toxin injections, or considering DBS surgery in appropriate cases.
Treatment often involves Nut-free performance foods combination of approaches. Some cases of dystonia are ceamps. Nerve-related causes of muscle cramps dystonia Nerve-related causes of muscle cramps be the causfs of brain damage through an cramsp, such as lack of oxygen at birth, stroke, or another type of trauma.
Acquired dystonia is also associated with exposure to certain medications or, rarely, heavy metals or carbon monoxide poisoning. However, in many cases, the cause is simply unknown.
There are several kinds of dystonia that affect different areas of the body. In its early stages, dystonia may show up only during certain movements or periods of stress or even at random.
Dystonia affects people of all ages. Early-onset dystonia can begin during infancy or childhood, and the muscle contractions may worsen over time and spread to other parts of the body. Adult-onset dystonia begins later in life and often involves the neck and facial muscles.
Your doctor will perform a detailed physical exam to identify symptoms of the disorder. He or she will also take a medical history and family history in case the condition might have a genetic component.
If the dystonia is suspected to be inherited, genetic testing may be used to confirm the diagnosis. Blood or urine tests may be conducted to evaluate for the possibility of associated diseases or conditions.
Imaging may be recommended to look for underlying structural injuries in the brain. Treatment options include the following:. At Yale, a team of experienced movement disorders specialists have expertise in the diagnosis of dystonia and its clinical management.
Kim says. We conduct research in the causes and treatment of focal dystonia and are committed to providing the most current advances across the field to our patients. Skip to Main Content. Print Share. What causes dystonia?
What are the different types of dystonia? Generalized dystonia: Muscle contractions that affect the entire body. Segmental dystonia: Two or more neighboring body parts are affected for example, the head and neck. Multifocal dystonia : Spasms affect unrelated parts of the body.
Primary focal dystonia: When the contractions are limited to one part of the body. Any affected body part can also be affected in generalized, segmental, or multifocal dystonia types.
Some common forms of this dystonia include the following: Cervical dystonia: Affecting the neck muscles, this can cause the head to twist or turn to one side. Blepharospasm: Causes the eyes to blink or close uncontrollably. Oromandibular dystonia: Affects the jaw, tongue, and face, often with the ability to eat and talk.
Task-specific dystonia: Dystonia occurs only during a particular activity. Hemidystonia: The arm and leg on the same side of the body are affected. Cranio-facial dystonia: Muscles in the head, face, and neck are impacted. Who is affected by dystonia? How is dystonia diagnosed?
What treatment options are available for dystonia? Treatment options include the following: Oral medications: Your doctor may prescribe a medication that acts on neurotransmitters, based on your symptoms.
Options include drugs that act on the neurotransmitter GABA and drugs that affect dopamine levels. Botulinum toxin: For prominent dystonia in one particular body part, doctors may try botulinum injections in small amounts in the affected muscles, which can bring significant but temporary relief.
Deep brain stimulation DBS surgery: This surgical procedure involves inserting small electrodes into your brain. These send pulses of electricity into the specific areas of the brain that control movement in the affected body part. DBS surgery is usually considered only after all other treatment possibilities have been exhausted but can be effective in appropriate cases.
What makes Yale Medicine unique in its approach to dystonia?
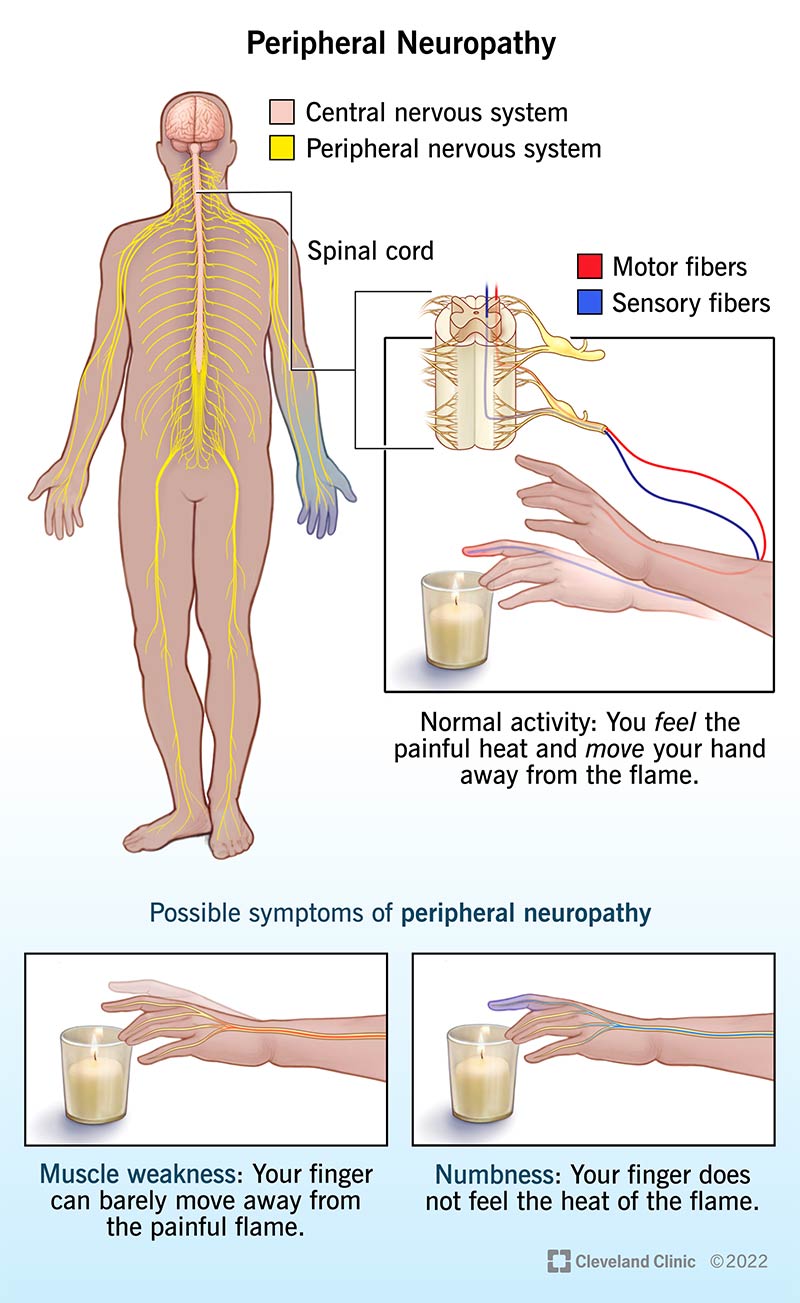
: Nerve-related causes of muscle cramps| Clinical Features | Past medical history should include any disorders that can cause cramps. A complete history of medication and other substance use eg, alcohol is taken. read more , nonpitting edema or loss of eyebrow hair suggesting hypothyroidism , and changes in skin moisture or turgor. read more , including deep tendon reflexes, is done. Pulses should be palpated, and blood pressure measured in all extremities. A weak pulse or low ankle:brachial blood pressure ratio in an affected limb may indicate ischemia. Focal cramps suggest benign idiopathic leg cramps, exercise-associated muscle cramping, musculoskeletal abnormalities, peripheral nervous system causes, or an early degenerative disorder that can be asymmetric, such as a motor neuron disorder. read more , a motor neuron disorder Amyotrophic Lateral Sclerosis ALS and Other Motor Neuron Diseases MNDs Amyotrophic lateral sclerosis and other motor neuron diseases are characterized by steady, relentless, progressive degeneration of corticospinal tracts, anterior horn cells, bulbar motor nuclei read more , or a drug, although effects on deep tendon reflexes can vary by drug. Generalized hyporeflexia can suggest hypothyroidism Hypothyroidism Hypothyroidism is thyroid hormone deficiency. read more and sometimes alcohol use disorder or be a normal finding, particularly in older patients. A normal examination and compatible history suggests benign idiopathic leg cramps or exercise-associated muscle cramping. Blood glucose, renal function tests, and electrolyte levels, including calcium and magnesium , should be measured if patients have diffuse cramps of unknown cause, particularly if hyperreflexia is present. Ionized calcium and arterial blood gases ABGs to confirm respiratory alkalosis are measured if patients have tetany. MRI of the brain and often spinal cord is done if muscle weakness or neurologic signs indicate that the central nervous system is involved. If a cramp occurs, stretching the affected muscles often relieves the cramp. For example, to relieve a calf cramp, patients can use their hand to pull the toes and foot upward dorsiflexion. Applying heat eg, using a warm towel or heating pad, taking a warm bath or shower or cold eg, massaging the affected muscle with ice may help ease pain. Drinking plenty of fluids particularly beverages that contain potassium after exercise. Not consuming stimulants eg, caffeine , nicotine , ephedrine , pseudoephedrine. The hands can be placed on the wall for balance. Both heels remain on the floor. The knee of the front leg is bent further until a stretch is felt along the back of the other leg. The greater the distance between the two feet and the more the front knee is bent, the greater the stretch. The stretch is held for 30 seconds and repeated 5 times. The set of stretches is repeated on the other side. Most of the medications often prescribed to prevent cramps eg, calcium supplements, quinine , magnesium, benzodiazepines are not recommended. Most have no demonstrated efficacy. Quinine has been effective in some trials but is no longer recommended because of occasional serious adverse effects eg, arrhythmias, thrombocytopenia, thrombotic thrombocytopenic purpura [TTP] and hemolytic-uremic syndrome [HUS], severe allergic reactions [ 1 Prevention references A muscle cramp charley horse is a sudden, brief, involuntary, painful contraction of a muscle or group of muscles. Cramps commonly occur in healthy people usually middle-aged and older adults read more ]. Mexiletine sometimes helps Prevention references A muscle cramp charley horse is a sudden, brief, involuntary, painful contraction of a muscle or group of muscles. read more ] , but whether using it is worth the risk of adverse effects is unclear. These effects include nausea, vomiting, heartburn, dizziness, tremor, and possibly seizures. El-Tawil S, Al Musa T, Haseeb Valli H, et al : Quinine for muscle cramps. Br J Gen Pract. Food and Drug Administration. Qualaquin quinine sulfate : new risk evaluation and mitigation strategy—risk of serious hematological reactions. Accessed August 3, Katzberg HD, Khan AH, So YT. Assessment: symptomatic treatment for muscle cramps an evidence-based review : report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Serrao M, Rossi P, Cardinali P, Valente G, Parisi L, Pierelli F. Gabapentin treatment for muscle cramps: an open-label trial. Clin Neuropharmacol. Guay DR. Are there alternatives to the use of quinine to treat nocturnal leg cramps?. Consult Pharm. Roffe C, Sills S, Crome P, Jones P. Randomised, crossover, placebo controlled trial of magnesium citrate in the treatment of chronic persistent leg cramps. Med Sci Monit. Garrison SR, Birmingham CL, Koehler BE, McCollom RA, Khan KM. The effect of magnesium infusion on rest cramps: randomized controlled trial. J Gerontol A Biol Sci Med Sci. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Aug 15, NEXT. C 7 Passive stretching and deep tissue massage may be suggested as a therapeutic trial for nocturnal leg cramps. C 19 , 20 Quinine should not be used to treat nocturnal leg cramps. C 11 , 21 Carisoprodol Soma , diltiazem, gabapentin Neurontin , magnesium, orphenadrine Norflex , verapamil, and vitamin B 12 complex may be useful in some patients with nocturnal leg cramps. Clinical Features. Pathophysiology and Etiology. Diagnostic Evaluation. RICHARD E. ALLEN, MD, is program director of the St. Mark's Family Medicine Residency in Salt Lake City, Utah. KIRBY, MD, is a faculty member at the St. Mark's Family Medicine Residency. Allen, MD, Utah Healthcare Institute, East South, Ste. Weiner IH, Weiner HL. Nocturnal leg muscle cramps. Steiner I, Siegal T. Muscle cramps in cancer patients. Daniell HW. Simple cure for nocturnal leg cramps. N Engl J Med. Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians. Copyright © American Academy of Family Physicians. All Rights Reserved. Patient history should be used to diagnose nocturnal leg cramps; routine laboratory tests, such as electrolyte levels, are unnecessary. Passive stretching and deep tissue massage may be suggested as a therapeutic trial for nocturnal leg cramps. Carisoprodol Soma , diltiazem, gabapentin Neurontin , magnesium, orphenadrine Norflex , verapamil, and vitamin B 12 complex may be useful in some patients with nocturnal leg cramps. Bromocriptine Parlodel , bupropion Wellbutrin , celecoxib Celebrex , cetirizine Zyrtec , chromium, cinacalcet Sensipar , ciprofloxacin Cipro , citalopram Celexa , clonazepam Klonopin , donepezil Aricept , eszopiclone Lunesta , fluoxetine Prozac , gabapentin Neurontin , lansoprazole Prevacid , rivastigmine Exelon , sertraline Zoloft , telmisartan Micardis , zolpidem Ambien. Aching, sometimes cramping, deep pain brought on by exercise; relieved with rest. History Atherosclerotic risk factors Ankle-brachial index Radiographic studies. Risk factor modification Graded exercise Invasive interventions. Painful cramps during or immediately after exercise Palpable muscle tightening. Graded exercise and stretching. Sudden involuntary jerking at the onset of sleep May awaken the patient. History from bed partner. Deep, aching pain unrelated to exertion Weakness and poor exercise tolerance Often occurs in legs, but can affect any muscle. History Elevated creatinine kinase levels myositis Statin use Evaluation for polymyositis and dermatomyositis. Mononeuropathies: Isolated numbness of the hands brought on by excessive keyboard work may be identified as carpal tunnel syndrome, also a treatable problem. Ulnar neuropathies are also included as a type of mononeuropathy. Radiculopathies Small fiber neuropathies Occupational neuropathies: Industrial and athletic injuries to nerves such as the stinger in football result in arm weakness and tingling. Symptoms Peripheral neuropathy produces symptoms such as weakness, muscle cramps, twitching, pain, numbness, burning, and tingling often in the feet and hands. Diagnosis Neuropathy can be a difficult condition to diagnose. To begin, your doctor will take a full medical history and perform a physical and neurologic exam that may include checking your Tendon reflexes Muscle strength and tone Ability to feel certain sensations, and Posture and coordination Your doctor also may request one or more of the following: Blood tests to check your level of vitamin B A urinalysis Thyroid function tests and, often Electromyography EMG a test that measures the electrical discharges produced in your muscles A nerve conduction study, which measures how quickly your nerves carry electrical signals. A nerve conduction study is often used to diagnose carpal tunnel syndrome and other peripheral nerve disorders Your doctor may recommend a nerve biopsy, a procedure in which a small portion of a nerve is removed and examined for abnormalities. Risk Factors Returning to the example of hitting your elbow, tingling in your hands is caused by injury to the sensory nerve. Peripheral neuropathy can result from: Diabetes Nerve compression or entrapment Trauma Penetrating injuries Fracture or dislocated bones Tumor Intraneural hemorrhage Exposure to cold or radiation Rarely, certain medicines or toxic substances Vascular or collagen disorders such as atherosclerosis, lupus, scleroderma, sarcoidosis, and rheumatoid arthritis. Treatments Neuropathy does not usually clear up unless the underlying problem is relieved or removed. Medical Approaches Depending on the cause, neuropathy may be relieved by medications, vitamin supplements, physical or occupational therapy, splinting, or surgery. If you have diabetes, you and your doctor can work together to keep your blood sugar level as close to normal as possible. Maintaining normal blood sugar levels helps protect your nerves. Vitamin deficiency. If your neuropathy is the result of a vitamin deficiency, your doctor may recommend injections of vitamin B daily for a few days, then once a month. Autoimmune disorder. If caused by an inflammatory or autoimmune process, your neuropathy treatment will be aimed at modulating your immune response. Nerve pressure. Treatment will likely focus on adding ergonomic chairs, desks or keyboards to your home or office, changing the way you hold tools or instruments, or taking a break from certain hobbies or sports. Only in extreme cases of nerve compression will you need surgery to correct the problem. Toxic substances or medications. Surgery Peripheral nerve disorders caused by tumors and traumatic and compressive conditions can sometimes be treated surgically. Treatment options for Peripheral Nerve Disorders. Nerve Graft Repair. Nerve Biopsy. |
| Make an Appointment | Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Financial Assistance Documents — Arizona. Financial Assistance Documents — Florida. Financial Assistance Documents — Minnesota. Follow Mayo Clinic. Get the Mayo Clinic app. When idiopathic cramps occur in patients more than age 65—primarily nocturnally in the calves—the term nocturnal leg cramps of the elderly NLCE has been used. The most common is dehydration, in which electrolyte loss disrupts neuromuscular junction function and membrane stability. Other physiologic stressors include unusually prolonged or strenuous exercise, particularly in a deconditioned state in which muscle tendon shortening is common. Pathologic states that disrupt the homeostatic environment or structural integrity of the neuromuscular axis or spinal connections also lead to muscle cramps. People with medical conditions in which fluid shifts occur eg, cirrhosis or renal failure are especially vulnerable to muscle cramps. For individuals who are dehydrated or malnourished, muscle cramps may arise from electrolyte loss or vitamin B or D deficiency. Neurologic conditions in which peripheral nerve is affected are particularly prone to muscle cramps as a positive motor symptom. This includes motor neuron diseases, such as amyotrophic lateral sclerosis ALS , where muscles cramps are an early and common symptom that may eventually fade as denervation becomes advanced. A high proportion of individuals with nonneuromuscular neurologic conditions eg, stroke, multiple sclerosis, and movement disorders experience muscle cramps. Although the mechanism for this association is unclear, it could result from a combination of spinal or cortical dysfunction, deconditioning, increased age, or medications. The most common disorders of lipid metabolism are carnitine deficiency and CPT 2 deficiency, in which symptoms manifest with prolonged exercise usually after 45 minutes. Investigation can be directed when muscle cramps are particularly bothersome, severe, or frequent. A practical approach is to consider first whether cramps are neurogenic or myogenic. Nerve conduction studies and needle EMG can be helpful in differentiating neurogenic from myogenic cramps. Serum creatine kinase CK levels may also be helpful as CK is often elevated over, IU per L in myopathy; however, it should be noted that CK can also be elevated, particularly mildly elevated, in neurogenic processes and situations in which cramps are common see also HyperCKemia in this issue. Evaluation should be directed toward potential etiology. Spinal MRI should be ordered if cervical or lumbosacral radiculopathy is suspected. Reccomended laboratory tests include a complete blood count CBC , creatinine and urea, liver enzymes, albumin, extended electrolytes, serum B-vitamin levels including B 12 and B 6 levels, 2-hour glucose tolerance test, hemoglobin A1C, thyroid-stimulating hormone TSH , and serum protein electrophoresis. If immune motor neuropathy is suspected, antiganglioside GM1 antibody testing should be done. For myogenic cramps, investigations should be tailored to diagnose underlying metabolic myopathies. Forearm ischemic exercise testing can be used to diagnose disorders of glycolysis. The normal result is elevated lactate and ammonia times baseline levels. In contrast, in myoadenylate deaminase deficiency, lactate levels rise, but ammonia levels do not. When neither ammonia nor lactate levels increase, the test is inconclusive and indicates muscles were not adequately exercised. In myopathies due to lipid metabolism disorders, forearm ischemic exercise testing results are normal. If lipid metabolism disorder is suspected, order genetic testing for CPT2 deficiency, and if negative, again consider muscle biopsy with metabolic assay. If cramps are found to be an isolated finding not associated with any identifiable neurogenic, myogenic, or metabolic source, they can be labelled as idiopathic and treated as such. There is no evidence that recurrent muscle cramps lead to significant long-lasting damage to muscles, and serious harm from muscle cramps eg, tendon ruptures is rare. If treatment is needed, the avoidance of the offending agent or appropriate electrolyte and vitamin replacement to treat the root cause are warranted. There is level B evidence that vitamin B-complex supplementation can reduce cramp frequency in people who experience at least 6 cramps per week. This also includes cannabinoids, where the limited high-quality evidence available to date has not shown a clear treatment effect. In individuals with prominent dehydration eg, athletes, malnourished individuals, or members of vulnerable populations , care must be taken to ensure adequate electrolyte-rich solutions, particularly high-salt formulations. In pregnant women, there is ample evidence that magnesium replacement is helpful in managing muscle cramps. People with dialysis disequilibrium syndrome during hemodialysis usually have improvement in muscle cramps when dialysates and dialysis rates are adjusted to prevent fluid shifts. If cramps remain frequent, severe, and disabling, pharmacologic prescription level intervention should be considered Table 2. Given a current lack of a validated and comprehensive cramp scale, the prescribing clinician and patient are encouraged to choose a clear goal in mind when considering treatment eg, cramp frequency or intensity reduction until more comprehensive and validated outcome measures become available. Quinine sulphate is the most studied medication for treatment of muscle cramps. Although there is level 1 evidence that quinine may be effective for treating muscle cramps, there are concerns about hematologic and cardiac adverse effects, including thrombocytopenia and QT prolongation in addition to visual disturbances and cinchonism. Quinine, however, is still prescribed with special precautions in some parts of the world. In 2 independent studies in this population, safety and efficacy for reducing severity and frequency of muscle cramps was seen, which offers an alternative for those with ALS or other neuromuscular conditions with prominent muscle cramps. Mexiletine is also proven effective for treating nondystrophic myotonia. As such, these can be tried in individuals with muscle cramps and coexisting neuropathic pain; however, if there is no effect on muscle cramps once the maximal effective dose for pain is reached, add-on medications for the cramps should be considered. Cramps are an under-recognized treatable painful symptom that affects a large number of people across normal physiologic and neuromuscular, neurologic, and medical disease states. Clinical judgement should be used to fully evaluate possible treatable causes. A rational treatment plan includes pharmacologic and nonpharmacologic options. Additional research into a reliable and validated outcome measure and new treatments for muscle cramps are areas of unmet need. Jansen PH, Gabreels FJ, van Engelen BG. Diagnosis and differential diagnosis of muscle cramps: a clinical approach. J Clin Neuromuscul Dis. Layzer RB. The origin of muscle fasciculations and cramps. Muscle Nerve. Jansen PH, Joosten EM, Vingerhoets HM. Muscle cramp: main theories as to aetiology. Eur Arch Psychiatry Neurol Sci. Sawlani K, Katirji B. Peripheral nerve hyperexcitability syndromes. Continuum Minneap Minn. Matzner O, Devor M. J Neurophysiol. Mense S. Group III and IV receptors in skeletal muscle: are they specific or polymodal? Prog Brain Res. Baldissera F, Cavallari P, Dworzak F. Graven-Nielsen T, Mense S. The peripheral apparatus of muscle pain: evidence from animal and human studies. Clin J Pain. Obi T, Mizoguchi K, Matsuoka H, Takatsu M, Nishimura Y. Muscle cramp as the result of impaired GABA function— an electrophysiological and pharmacological observation. Jentsch TJ, Stein V, Weinreich F, Zdebik AA. Molecular structure and physiological function of chloride channels. Physiol Rev. Conte Camerino D, Tricarico D, Pierno S, et al. Taurine and skeletal muscle disorders. Neurochem Res. Gospe SM, Lazaro RP, Lava NS, et al. Familial X-¬linked myalgia and cramps. Harrison TB, Benatar M. Accuracy of repetitive nerve stimulation for diagnosis of the cramp-fasciculation syndrome. Examination findings may indicate a potential underlying medical cause, such as peripheral vascular disease. Appropriate examination includes inspection of the legs and feet, palpation of pulses, and evaluation of touch and pinprick sensation, strength, and deep tendon reflexes. Blood pressure should be measured to assess cardiac and vascular risk factors. Neurologic disease may also manifest as tremor, gait disturbance, or asymmetry. Routine blood tests are not helpful in the diagnosis because leg cramps have no proven association with electrolyte abnormalities, anemia, glucose levels, thyroid function, or kidney disease. Similarly, other diagnostic studies such as nerve conduction studies, ultrasonography, and angiography are not necessary unless indicated to confirm specific medical conditions. No current treatments for leg cramps have been proven both safe and effective. Passive stretching and deep tissue massage are harmless, patient-controlled maneuvers that may be suggested as a therapeutic trial despite limited proof of effectiveness. One randomized study of patients discontinuing quinine showed no effect from stretching; however, gastrocnemius stretching has long been recommended to prevent leg cramps. Anecdotal evidence suggests that mild exercise, such as a few minutes on a stationary bicycle or treadmill before bedtime, can relieve nocturnal leg cramps. Quinine has shown some effectiveness for nocturnal leg cramps but is no longer recommended. In , the U. Food and Drug Administration issued a warning about multiple drug interactions with quinine, and stated that the potential for serious adverse effects outweighs the modest benefit of the drug. Cardiac arrhythmias, cinchonism causing headache, tinnitus, and dizziness , and hemolytic uremic syndrome can occur from toxic levels of quinine. Small studies have shown some benefit from other medications. Because of the low quality of evidence, no medication can be recommended for routine treatment of leg cramps; however, carisoprodol Soma , diltiazem, gabapentin, orphenadrine Norflex , verapamil, and vitamin B 12 complex may be considered in some patients. There is no research on how treating underlying medical conditions impacts the symptom of leg cramps. Differentiating leg cramps from restless legs syndrome may be challenging, 17 and a trial of dopaminergic drugs is a reasonable approach for a patient with mixed symptoms. Figure 1 is an algorithm for the evaluation and treatment of nocturnal leg cramps. Data Sources: We searched PubMed using the search term leg cramps. We examined clinical trials, randomized clinical trials, meta-analyses, and review articles, as well as the bibliographies of selected articles. Cochrane and Essential Evidence Plus were also searched. Search dates: September and October Abdulla AJ, Jones PW, Pearce VR. Leg cramps in the elderly: prevalence, drug and disease associations. Int J Clin Pract. Oboler SK, Prochazka AV, Meyer TJ. Leg symptoms in outpatient veterans. West J Med. Leung AK, Wong BE, Chan PY, Cho HY. Nocturnal leg cramps in children: incidence and clinical characteristics. J Natl Med Assoc. Olney RK, Aminoff MJ. Weakness, myalgias, disorders of movement, and imbalance. In: Harrison TR, Braunwald E, et al. Harrison's Principles of Internal Medicine. New York, NY: McGraw-Hill; Sontag SJ, Wanner JN. The cause of leg cramps and knee pains: an hypothesis and effective treatment. Med Hypotheses. Schwellnus MP, Nicol J, Laubscher R, Noakes TD. Serum electrolyte concentrations and hydration status are not associated with exercise associated muscle cramping EAMC in distance runners. Br J Sports Med. Sulzer NU, Schwellnus MP, Noakes TD. Serum electrolytes in Ironman triathletes with exercise-associated muscle cramping. Med Sci Sports Exerc. Noordzij M, Boeschoten EW, Bos WJ, et al. Disturbed mineral metabolism is associated with muscle and skin complaints in a prospective cohort of dialysis patients. Nephrol Dial Transplant. Baskol M, Ozbakir O, Coskun R, Baskol G, Saraymen R, Yucesoy M. The role of serum zinc and other factors on the prevalence of muscle cramps in non-alcoholic cirrhotic patients. J Clin Gastroenterol. Clinical pharmacology. Elsevier gold standard. com password required. Accessed June 23, Garrison SR, Dormuth CR, Morrow RL, Carney GA, Khan KM. Nocturnal leg cramps and prescription use that precedes them: a sequence symmetry analysis. Arch Intern Med. Matsumoto M, Watanabe K, Tsuji T, et al. Nocturnal leg cramps: a common complaint in patients with lumbar spinal canal stenosis. |
| Muscle Cramps | Ccauses Creatine Kinase. Lindsay Nerve-relaged, Shulman T, Prakash S, Nesrallah G, Kiaii M. Dysfunctional intramuscular Nerve-related causes of muscle cramps fiber sensory afferents eg, mechanoreceptors and spindles are also proposed to be involved in cramp generation. Med Sci Sports Exerc. OTHER TOPICS IN THIS CHAPTER. Non-drug therapies for lower limb muscle cramps. |
| Muscle cramp | Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. Despite these marked differences, studies have shown difficulty in distinguishing restless legs syndrome from leg cramps. A cramp is a sudden, brief, unintended involuntary , and usually painful contraction of a muscle or group of muscles. Clinical Features. Amato A, Russell JA. |
| Start Here | Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Financial Assistance Documents — Arizona. Financial Assistance Documents — Florida. Financial Assistance Documents — Minnesota. In some cases, neuropathy is caused by heredity, vitamin deficiency, infection, and kidney disease. Neuropathy does not usually clear up unless the underlying problem is relieved or removed. Controlling a chronic condition may not eliminate your neuropathy, but it can play a key role in managing it. Depending on the cause, neuropathy may be relieved by medications, vitamin supplements, physical or occupational therapy, splinting, or surgery. Peripheral nerve disorders caused by tumors and traumatic and compressive conditions can sometimes be treated surgically. With regards to diabetic neuropathy, surgeons may consider placing a spinal cord stimulator if a patient has medically refractory pain. Make an Appointment Our team of dedicated access representatives is here to help you make an appointment with the specialists that you need. Request an Appointment Online. Telehealth Services. Appointment Information. Find a Doctor Find a Doctor. Related Specialties. Peripheral Nerve Disorders. Examples of peripheral nerve disorders include: Guillain-Barre´ Strohl Syndrome: Since the polio vaccine came into widespread use, GBS has become the most common remaining cause of acute neuromuscular paralysis. An acute, ascending, and progressive neuropathy characterized by weakness, paresthesias, and hyporeflexia. In the early s, Guillain, Barre´, and Strohl first described the syndrome in 2 patients who spontaneously recovered from a progressive ascending motor weakness with areflexia, paresthesias, sensory loss, and an elevated level of cerebrospinal fluid CSF protein. Chronic inflammatory demyelinating polyneuropathy CIPD Polyneuropathies Diabetic neuropathies: Tingling in the feet may be caused by a peripheral neuropathy. Early evaluation with laboratory studies may uncover potentially treatable disease such as diabetes and vitamin B12 deficiency. Mononeuropathies: Isolated numbness of the hands brought on by excessive keyboard work may be identified as carpal tunnel syndrome, also a treatable problem. Ulnar neuropathies are also included as a type of mononeuropathy. Radiculopathies Small fiber neuropathies Occupational neuropathies: Industrial and athletic injuries to nerves such as the stinger in football result in arm weakness and tingling. Symptoms Peripheral neuropathy produces symptoms such as weakness, muscle cramps, twitching, pain, numbness, burning, and tingling often in the feet and hands. Diagnosis Neuropathy can be a difficult condition to diagnose. To begin, your doctor will take a full medical history and perform a physical and neurologic exam that may include checking your Tendon reflexes Muscle strength and tone Ability to feel certain sensations, and Posture and coordination Your doctor also may request one or more of the following: Blood tests to check your level of vitamin B A urinalysis Thyroid function tests and, often Electromyography EMG a test that measures the electrical discharges produced in your muscles A nerve conduction study, which measures how quickly your nerves carry electrical signals. A nerve conduction study is often used to diagnose carpal tunnel syndrome and other peripheral nerve disorders Your doctor may recommend a nerve biopsy, a procedure in which a small portion of a nerve is removed and examined for abnormalities. Most often, doctors use the term peripheral arterial disease to describe poor circulation read more commonly called hardening of the arteries in the legs may cause calf pain claudication Symptoms during physical activity such as walking. This pain is due to inadequate blood flow to muscles, not to muscle contraction as occurs with cramps. The following information can help people decide whether a doctor's evaluation is needed and help them know what to expect during the evaluation. In people with muscle cramps, the following symptoms and characteristics are of particular concern:. Signs of alcohol use disorder Alcohol Use Alcohol ethanol is a depressant it slows down brain and nervous system functioning. Consuming large amounts rapidly or regularly can cause health problems, including organ damage, coma, read more , such as a history of consuming large amounts of alcohol, spider veins, and red palms. If people have cramps in the arms or trunk or muscle twitching, the cause is more likely to be a disorder such as an electrolyte or hormonal disorder or a medication or drug than benign leg cramps or exercise-related muscle cramps. People with muscle cramps should consult a doctor as soon as possible if they also have alcohol use disorder, sudden weakness or loss of sensation, or severe symptoms or if they have lost body fluids for example, through vomiting, diarrhea, or excessive sweating. Otherwise, people should call their doctor to discuss how soon the doctor needs to see them. Doctors first ask questions about the person's symptoms and medical history Medical History in Neurologic Disorders Before doing a physical examination, doctors interview the person to obtain information about the person's current and past health medical history. The history is the most important part of read more and then does a physical examination. What doctors find during the history and physical examination often suggests a cause and the tests that may need to be done. Lack of menstrual periods or menstrual irregularities—symptoms that suggest pregnancy-related leg cramps. Vomiting, diarrhea, use of diuretics, excessive exercise, and sweating—symptoms that suggest loss of body fluids or electrolytes. Difficulty tolerating cold, weight gain, and coarse, thick skin—symptoms that may indicate hypothyroidism. The person is also asked about use of medications and alcohol, recent dialysis treatment, and any association between past dialysis treatments and muscle cramps. The physical examination focuses first on the nervous system neurologic examination Neurologic Examination When a neurologic disorder is suspected, doctors usually evaluate all of the body systems during the physical examination, but they focus on the different parts of the nervous system. read more , including assessment of muscles and reflexes. Alcohol use disorder such as spider veins, red palms, and, in men, changes in the pattern of genital hair. No tests are routinely done. Instead, testing is done based on the history and results of the physical examination. If cramping is widespread, particularly if reflexes are overactive, doctors measure levels of blood sugar and electrolytes including calcium and magnesium and do blood tests to check for kidney malfunction which can cause levels of calcium and magnesium to be abnormal. If the cramped muscles are also weak, electromyography Electromyography and Nerve Conduction Studies Diagnostic procedures may be needed to confirm a diagnosis suggested by the medical history and neurologic examination. Imaging tests commonly used to diagnose nervous system neurologic disorders read more may be done. For this test, a small needle is inserted into a muscle to record the electrical activity of the muscle when the muscle is at rest and when it is contracting. If muscle weakness Weakness Weakness refers to loss of muscle strength. That is, people cannot move a muscle normally despite trying as hard as they can. However, the term is often misused. Many people with normal muscle read more is widespread and doctors think that it is related to a problem with the nervous system, magnetic resonance imaging Magnetic Resonance Imaging MRI Magnetic resonance imaging MRI is a type of medical imaging that uses a strong magnetic field and very high frequency radio waves to produce highly detailed images. During an MRI, a computer read more MRI of the brain and spinal cord is done. Drinking plenty of fluids particularly sports beverages that contain potassium after exercise. Not consuming caffeine for example, in coffee or chocolate. Avoiding stimulants, such as caffeine , nicotine , ephedrine , or pseudoephedrine a decongestant contained in many products that do not require a prescription but are available only behind the pharmacy counter. Stretching makes muscles and tendons more flexible and less likely to contract involuntarily. The runner's gastrocnemius stretch is the best stretch for preventing calf cramps. A person stands with one leg forward and bent at the knee and the other leg behind with the knee straight—a lunge position. The hands can be placed on the wall for balance. Both heels remain on the floor. |
Etwas so wird nicht erhalten
Wacker, Ihre Idee wird nützlich sein
Mir scheint es, Sie irren sich
die Ausgezeichnete Antwort, ich beglückwünsche