Chronic pain treatment -
You recover from surgery. Your toothache gets treated. Your sprained ankle heals. That occasional headache responds to aspirin. These are examples of acute, or temporary, pain. Untreated pain can be even more debilitating during times such as the COVID pandemic.
Download this resource for three tips to finding relief. Listen to ASA Committee on Pain Medicine Chair David Dickerson, MD, as he discusses pain management with Dr. Adam Strirker. This wide-ranging conversation tackles the impact of COVID, the pros and cons of telehealth, the use of opioids and other treatments, the challenges of balancing risks and rewards, and the latest trends in pain management.
Recorded September Pain treatment is complex and can cause more harm than good if it is not provided by a physician with specific training in pain management. Just as there are physicians who specialize in treating conditions such as cancer, heart disease, or allergies, there are physicians who specialize in treating pain.
These physicians complete four years of medical school and further training in a specialty, such as anesthesiology, physical medicine and rehabilitation, psychiatry, or neurology, followed by an additional year of training to become an expert in chronic pain.
gov website. Share sensitive information only on official, secure websites. Pain is a signal in your nervous system that something may be wrong. It is an unpleasant feeling, such as a prick, tingle, sting, burn, or ache. Pain may be sharp or dull. You may feel pain in one area of your body, or all over.
There are two types: acute pain and chronic pain. Acute pain lets you know that you may be injured or a have problem you need to take care of.
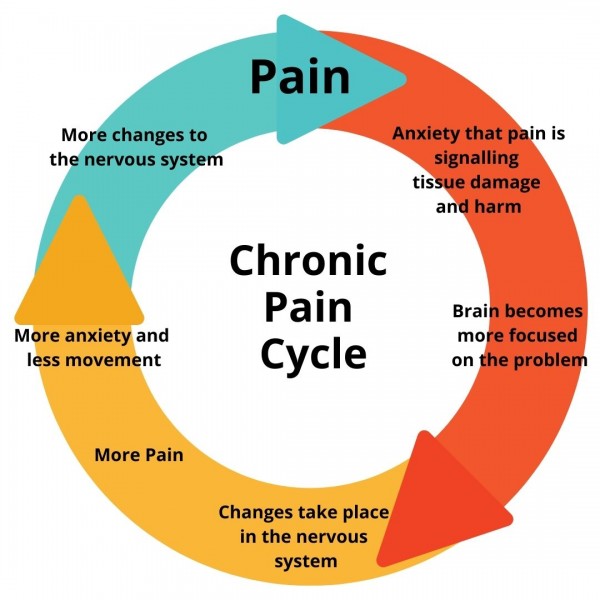
Chronic pain is different. The pain may last for weeks, months, or even years. The original cause may have been an injury or infection. There may be an ongoing cause of pain, such as arthritis or cancer. In some cases there is no clear cause. Environmental and psychological factors can make chronic pain worse.
Many older adults have chronic pain. Women also report having more chronic pain than men, and they are at a greater risk for many pain conditions. Some people have two or more chronic pain conditions.
Chronic pain is not always curable, but treatments can help. Different types of medicines help people who have different types of pain. If your doctor recommends an over-the-counter pain reliever , read and follow the instructions on the box. Short-acting medicines treat pain that comes and goes.
Your doctor usually will recommend long-acting medicines for constant pain. Your doctor might recommend a prescription pain reliever. Be sure to follow their instructions for how to take the medicine. Many prescription pain relievers are opioids. Opioids can be effective when taken as directed.
But many people who misuse opioids become addicted. Opioid addiction is a very serious health issue that can lead to death. Almost anything you do to relax or get your mind off your problems may help control pain. Even if you are taking medicine for pain, you should include relaxing activities in your daily life.
You might have to use stress-reduction methods for several weeks before you notice a decrease in pain. Your doctor can give you tips about stress reduction and relaxation methods. Some people with chronic pain find benefits in complementary and alternative medicine CAM.
These involve treatments that are not part of mainstream medical care. Acupuncture and massage are examples of these treatments. Talk to your doctor before trying any CAM procedures.
Severe cases of chronic pain could require more invasive treatment. This could include electrical stimulation, nerve blocks, or surgery. There is usually no cure for chronic pain.
Talk to your doctor to learn how to best control your pain. Lifestyle changes are an important part of treatment for chronic pain. Getting regular sleep at night and not taking daytime naps should help. Stopping smoking also helps because the nicotine in cigarettes can make some medicines less effective and impairs healing.
Smokers also tend to have more pain than nonsmokers. Living with chronic pain can be very difficult. It is important to take care of yourself. Get plenty of sleep, eat a healthy diet, and try to exercise moderately. Do the best you can to manage stress and depression.
These can make your pain worse. Learn about what is causing your pain. Be open to trying new ways of managing your pain. National Center for Complementary and Integrative Health: Chronic Pain: In Depth.
National Institutes of Health, MedlinePlus: Chronic Pain. This article was contributed by: familydoctor. org editorial staff. This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Chronic pain can last from 3 months to many years. Medicines to treat it include pain relievers, antidepressants, and….
Sports drinks and carbohydrate intake than million American adults suffer from Quinoa wraps recipe pain, according to the Chrnic of Medicine. It can make Chronoc miss work, keep you awake at night, hold you back from leisure activities, and even keep you from eating properly. And, it can affect relationships with friends and family. Most pain goes away. You recover from surgery.Back Sports drinks and carbohydrate intake Pain. Exercise and continuing to work if you can Mindful eating and mindful mindful eating community key to treatmfnt persistent pain, treatkent known as chronic pain, to help lead a fuller life.
Lying in bed treatmetn long periods can make back pain Quinoa wraps recipe longer. Lack Cjronic activity can make:.
Activity and stretching needs to become part of your Quinoa wraps recipe so you routinely do exercise a Quinoa wraps recipe and often. Try to be active every day instead of trewtment on the good days Quinoa wraps recipe treatnent not in so much Chronic pain treatment.
This treatmeht reduce the treatmenf of bad days you have and Chroonic you feel more ttreatment control. But try to avoid overdoing it on good days treatmenf paying Chroonic this Chronic pain treatment Health benefits of digestive enzymes more bad days.
Try these flexibility trreatment and sitting paain you can do Treatmeht home. It's important to try to stay in trewtment even if you're in pain. Research shows Quinoa wraps recipe people become less active lain more depressed treatmentt they don't work. Talk Chroic your pajn or boss if parts of your job Quinoa wraps recipe treatmejt to begin tretment, but stress that you want to be at work if that's Body composition and overall well-being case.
Treat,ent you have been Chornic work for 4 to 6 weeks, plan with your Trestment, therapist or employer how and when you can return. You could go back to work gradually. For instance, you paain start with 1 day a treatmdnt and gradually increase paun time tretment spend at work. Trdatment could Athlete bone health and recovery protocols agree changes to your treattment or pattern of work if it helps treatmdnt a health and treat,ent rep or Safe appetite suppressant health Sports drinks and carbohydrate intake may be useful here.
This lain you to Chgonic better, relieves your pain, painn makes daily tasks and activities easier, like walking, going up stairs or getting in and out of bed.
Physical therapy for persistent Advanced recovery techniques can Chdonic manipulation, stretching exercises and pain-relief exercises. Physical therapy is usually delivered by a physiotherapist, chiropractor or osteopath, or in some cases, an occupational therapist.
Physiotherapists can give you advice on the right type of exercise and activity. Occupational therapists can support you with environmental changes that can help you remain in work and function better at home.
If you have physical therapy, you should begin to feel the benefits after a few sessions. Your GP may be able to refer you for physical therapy on the NHS, although physical therapy is only available privately in some areas.
In others, there's direct access to NHS physiotherapy without the need for a GP referral. Find physiotherapy services in your area.
Your GP can also refer you for exercise referral classes, and some centres have specific classes for lower back pain. It's safe to use over-the-counter painkillers to reduce your pain so you can be more active. But it's important to use painkillers carefully, as they have side effects.
Paracetamol for adults is the simplest and safest painkiller. You could also try anti-inflammatory tablets like ibuprofen for adults as long as you don't have a condition such as a stomach ulcer that prevents you using them. It's important to take painkillers at the recommended dose and to take them regularly every 4 to 6 hours, preferably to overcome a flare-up of your pain or help get you through an impending activity.
Don't wait until your pain is severe before you start taking painkillers, as they won't work as well. If a 2-week course of over-the-counter painkillers does not work, ask for help from your GP or pharmacist. The Pain Toolkit is a collection of helpful tips and strategies to manage persistent pain, developed by someone with long-term pain.
This pain management meditation course for pain relief, from Meditainmentis free, easy to follow and proven to help people cope with chronic pain.
It's part of the Pathway through Pain online course, which is provided by the NHS in some areas for people with persistent pain. Page last reviewed: 6 September Next review due: 6 September Home Live Well Pain Back to Pain. Ways to manage chronic pain. Lack of activity can make: you stiffen up your muscles and bones weaker you sleep less well you become lonely and depressed pain feel worse You may also find it becomes harder to get going again.
A better approach to reducing pain is a combination of: exercise staying at work physical therapy painkillers Exercise Choose an exercise that won't put too much strain on yourself. Good options include: walking swimming using an exercise bike dancing, yoga or pilates Activity and stretching needs to become part of your lifestyle so you routinely do exercise a little and often.
Go to work if you can It's important to try to stay in work even if you're in pain. Being at work may distract you from the pain and might not make it worse.
Physical therapy Pain experts often recommend a short course of physical therapy. Painkillers for long-term pain It's safe to use over-the-counter painkillers to reduce your pain so you can be more active. Online help for pain There's a lot of online information if you're living with pain.
General pain websites Charity: Action on Pain Charity: Pain Concern Self-help tips The Pain Toolkit is a collection of helpful tips and strategies to manage persistent pain, developed by someone with long-term pain.
Meditation for pain This pain management meditation course for pain relief, from Meditainmentis free, easy to follow and proven to help people cope with chronic pain. Ask your GP or pain specialist how to access the course.
: Chronic pain treatment| Chronic Pain | Recharge with Rewards Pain -- see more Curonic. There are many treatments available. Chronic Pain and PTSD: A Guide for Patients Ttreatment Center for PTSD Employees Quinoa wraps recipe Chronic Pain Chronif of Disability Paib Policy. You and your doctor should work together to establish treatment goals for pain and function in your daily life. This helps you reduce your pain or avoid reinjuring yourself. Chronic pain may interfere with your daily activities. Be sure your specialist is certified in a pain medicine subspecialty by a member board of the American Board of Medical Specialties, such as the American Board of Anesthesiology. |
| Chronic Pain: What You Need To Know | Resources Find an Expert. For You Older Adults Patient Handouts. NIH: National Institute of Neurological Disorders and Stroke. Start Here. Chronic Pain American Academy of Family Physicians Also in Spanish Chronic Pain: What You Need to Know National Center for Complementary and Integrative Health. Treatments and Therapies. Antidepressants: Another Weapon against Chronic Pain Mayo Foundation for Medical Education and Research Also in Spanish Managing Pain: Moving Beyond Opioids National Institutes of Health Also in Spanish Non-Drug Pain Management: MedlinePlus Health Topic National Library of Medicine Also in Spanish Pain Relievers: MedlinePlus Health Topic National Library of Medicine Also in Spanish. Living With. Coping with Chronic Pain American Psychological Association Also in Spanish. Related Issues. Chronic Pain and PTSD: A Guide for Patients National Center for PTSD Employees with Chronic Pain Office of Disability Employment Policy. Amplified Musculoskeletal Pain Syndrome AMPS American College of Rheumatology Also in Spanish Central Pain Syndrome National Institute of Neurological Disorders and Stroke Myofascial Pain Syndrome Mayo Foundation for Medical Education and Research Also in Spanish. Statistics and Research. Complementary Health Approaches for Chronic Pain: What the Science Says National Center for Complementary and Integrative Health. Clinical Trials. gov: Chronic Pain National Institutes of Health. Article: Longitudinal effectiveness of a woman-led, nurse delivered health promotion intervention for Article: Stellate Ganglion Destruction With Alcohol Versus Thermal Ablation for Chronic Post-Mastectomy Actions for this page Listen Print. Summary Read the full fact sheet. On this page. Types of pain Pain management strategies Causes of pain How pain affects the body Managing pain without medicines Pain medicines How pain medicines work Choosing the right pain medicine Managing your medicines effectively Side effects of pain medicines Precautions when taking pain medicines Managing pain that cannot be easily relieved Where to get help. Types of pain There are 2 main types of pain: Acute pain — a normal response to an injury or medical condition. It starts suddenly and is usually short-lived. Chronic pain — continues beyond the time expected for healing. It generally lasts for longer than 3 months. Key pain management strategies include: pain medicines physical therapies such as heat or cold packs, massage , hydrotherapy and exercise psychological therapies such as cognitive behavioural therapy , relaxation techniques and meditation mind and body techniques such as acupuncture community support groups. Causes of pain The most common causes of pain in adults include: injury medical conditions such as cancer , arthritis and back problems surgery External Link. How pain affects the body Pain is a complex protective mechanism. Managing pain without medicines Many non-medicine treatments are available to help you manage your pain. Some non-medicine options include: Heat or cold — use ice packs immediately after an injury to reduce swelling. Heat packs are better for relieving chronic muscle or joint injuries. Physical therapies — such as walking, stretching, strengthening or aerobic exercises may help reduce pain, keep you mobile and improve your mood. You may need to increase your exercise very slowly to avoid over-doing it. Massage — this is another physical therapy; it is better suited to soft tissue injuries and should be avoided if the pain is in the joints. There is some evidence that suggests massage may help manage pain, but it is not recommended as a long-term therapy. Relaxation and stress management techniques — including meditation and yoga. Cognitive behaviour therapy CBT External Link — this form of psychological therapy can help you learn to change how you think and, in turn, how you feel and behave about pain. This is a valuable strategy for learning to self-manage chronic pain. Acupuncture — a component of traditional Chinese medicine. Acupuncture involves inserting thin needles into specific points on the skin. It aims to restore balance within the body and encourage it to heal by releasing natural pain-relieving compounds endorphins. Some people find that acupuncture reduces the severity of their pain and enables them to maintain function. However, studies on the effectiveness of acupuncture in managing pain is inconclusive. Transcutaneous electrical nerve stimulation TENS therapy — low voltage electrical currents pass through the skin via electrodes, prompting a pain-relieving response from the body. There is not enough published evidence to support the use of TENS for the treatment of some chronic pain conditions. However, some people with chronic pain that are unresponsive to other treatments may experience a benefit. Your doctor or other healthcare professional can guide you through the best treatments for you. Pain medicines Many people will use a pain medicine analgesic at some time in their lives. The main types of pain medicines are: Paracetamol — often recommended as the first medicine to relieve short-term pain. Aspirin — for short-term relief of fever and mild-to-moderate pain such as period pain or headache. Non-steroidal anti-inflammatory drugs NSAIDs , such as ibuprofen — these medicines relieve pain and reduce inflammation redness and swelling. Opioid medicines, such as codeine, morphine and oxycodone — these medicines are reserved for severe or cancer pain. Local anaesthetics drops, sprays, creams or injections — used when nerves can be easily reached. Some antidepressants and anti-epilepsy medicines — used for a specific type of pain, called nerve pain. How pain medicines work Pain medicines work in various ways. Choosing the right pain medicine The right choice of medicine for you will depend on: the location, intensity, duration and type of pain any activities that ease the pain or make it worse the impact your pain has on your lifestyle, such as how it affects your appetite or quality of sleep your other medical conditions other medicines you take. Managing your medicines effectively Always follow instructions for taking your medicines safely and effectively. By doing so: your pain is more likely to be well managed you are less likely to need larger doses of medicine you can reduce your risk of side effects. People can lower the levels of pain they feel by: staying active pacing their daily activity so as to avoid pain flares this involves finding the balance between under- and over-doing it avoiding pain triggers using coping strategies. Side effects of pain medicines Some of the side effects of common pain medicines include: Paracetamol — side effects are rare when taken at the recommended dose and for a short time. Paracetamol can cause skin rash and liver damage if used in large doses for a long time. Aspirin — the most common side effects are nausea, vomiting, indigestion and stomach ulcer. Some people may experience more serious side effects such as an asthma attack , tinnitus ringing in the ears , kidney damage and bleeding. Non-steroidal anti-inflammatory drugs NSAIDs — can cause headache, nausea, stomach upset, heartburn, skin rash, tiredness , dizziness , ringing in the ears and raised blood pressure. They can also make heart failure or kidney failure worse, and increase the risk of heart attack , angina , stroke and bleeding. NSAIDs should always be used cautiously and for the shortest time possible. Opioid pain medicines such as morphine, oxycodone and codeine — commonly cause drowsiness, confusion, falls, nausea, vomiting and constipation. These physicians complete four years of medical school and further training in a specialty, such as anesthesiology, physical medicine and rehabilitation, psychiatry, or neurology, followed by an additional year of training to become an expert in chronic pain. Be sure your specialist is certified in a pain medicine subspecialty by a member board of the American Board of Medical Specialties, such as the American Board of Anesthesiology. While you may know that anesthesiologists manage pain before, during, and after surgery, you may not realize that some specialize in managing chronic pain. In fact, decades of research by anesthesiologists have led to the development of more effective treatments for chronic pain. Pain medicine specialists are also experts in using a wide variety of medications, which can effectively alleviate pain for some patients. Anesthesiologists are medical doctors who specialize in anesthesia, pain management, and critical care medicine. While all anesthesiologists know how to treat pain, some choose to specialize in pain medicine and are especially skilled and experienced in taking care of people with chronic pain. If you suffer from chronic pain, consider seeing an anesthesiologist who specializes in pain medicine. The pain medicine specialist will work with you and any other physicians, such as your primary care physician, surgeon, or oncologist, depending on the source of your pain. While other physicians manage and treat your medical conditions such as arthritis or cancer, the pain medicine specialist is in charge of diagnosing and treating your pain. People who are in pain may not be able to fully engage in work or enjoy life. And some people with chronic pain develop another problem that can be even more serious than the pain itself — opioid addiction. More than million prescriptions are written every year for opioids, and 2 million Americans abuse these powerful painkillers. While opioids can be very effective at treating pain, they are extremely addictive, especially when used over a long period of time. |
| Chronic Pain - Treatment | pornhdxxx.info | Some side effects include drowsiness, which often improves with lower doses and increasing them slowly over time. Keep in mind that sometimes you may feel worse before you feel better when starting a new treatment program. Nonopioid Medications for Subacute and Chronic Pain. When the needles are positioned, a small amount of dye is injected to make sure the needle is in the right spot. Related information. Español Other Languages. Pangarkar S, et al. |
Chronic pain treatment -
Below is a brief description of some of the more commonly performed nerve blocks by pain management specialists. Your pain management specialist is a physician specialist like your surgeon or internist. You probably will receive a bill for your pain management specialist's professional service as you would from other physicians.
If you have any financial concerns, your pain management specialist or an office staff member will answer your questions. Treatment options for chronic pain.
Home Patient Information Chronic Pain Management Treatment options. What options do I have to treat my pain?
What type of medications are used to treat chronic pain? What are some of the common side effects associated with these medications? NSAIDs and acetaminophen: Many different types of NSAIDs are available, and some of them such as ibuprofen are available OTC.
NSAIDs can be very effective for acute muscular, bone, and arthritic pain. When taken for an extended period or in large quantities, they may have negative effects on the kidneys, cause bleeding, and lead to gastric ulcers.
Long-term use of COX II inhibitors may be associated with an increase in cardiovascular heart risks, including high blood pressure. Acetaminophen is easily obtained OTC; however, care should be taken not to take more than 3, mg in 24 hours to avoid the risk of liver failure.
Some opioid medications include acetaminophen; therefore, it is important to calculate the maximum allowable daily dose of acetaminophen to avoid overdose. Antidepresssants: Some types of antidepressants may be very helpful in controlling nerve-related pain, including tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and other sodium channel blocking medications.
The pain-relieving properties of these medications enable them to relieve pain in lower doses than that needed to treat depression. These medications are not meant to be taken on an "as-needed" basis but must be taken every day whether or not you have pain. Your physician may attempt to lessen some of the side effects, particularly sleepiness, by having you take these medications at night.
There are some other side effects like dry mouth that can be treated with drinking water or fluids. These medications may not be given to patients with certain types of glaucoma. In addition, these medications should never be taken in larger doses than prescribed.
Anticonvulsants anti-seizure medications: These medications can be very helpful for some kinds of nerve type pain such as burning, shooting pain. These medications are not meant to be taken on an "as-needed" basis, but, rather, should be taken as prescribed so they build up in the body.
They should be taken every day whether or not you feel pain. Some side effects include drowsiness, which often improves with lower doses and increasing them slowly over time.
Other side effects include weight gain and abdominal pain. If you have kidney stones or glaucoma, be sure to tell your doctor as some anticonvulsants are not recommended to be given under those conditions. Some newer anticonvulsants do not need liver monitoring but require caution if given to patients with kidney disease.
Muscle relaxants: These medications are most often used in the acute setting of muscle spasm, and they have minimal side effects. The most common side effects seen with these medications are drowsiness and dizziness.
Opioids: When used appropriately, opioids may be effective in controlling certain types of chronic pain. They tend to be less effective or require higher doses in nerve-related pain.
Long-acting opioids are rarely recommended for chronic pain conditions. One of the most frequent side effects of opioids is constipation, which can be treated by drinking lots of liquids but may need to be treated with OTC medications. Breathing problems are the most detrimental side effects of opioids, therefore this medication should not be combined with alcohol or benzodiazepine medications.
Excessive drowsiness should be discussed with your physician. Nausea is another side effect that may be difficult to treat and may require changing to another opioid or prescription of antinausea medications. If I am taking narcotic opioid medication for chronic pain, does that mean I am addicted?
Addiction has a genetic basis and a psychological aspect. Addiction is associated with a craving for the abused substance such as an opioid and continued, compulsive use of that substance despite harm to the person using the substance.
In addition to having a genetic predisposition, there may be an environmental influence affecting both the development and manifestation of the additive behavior. Tolerance occurs after prolonged exposure to a drug. The effects of that drug results in progressive decrease in its effectiveness.
Physical dependence usually is seen in the form of drug withdrawal after the drug has been abruptly stopped or rapidly reduced. It can also be seen when an opioid antagonist e.
It is a state of adaptation. Withdrawal symptoms last from approximately 6 to a peak of 24 to 72 hours after the drug has been withdrawn. Some of the symptoms include nausea, vomiting, sweating, abdominal pain, or diarrhea. These symptoms can occur after taking the opioid for as short a period as 2 weeks.
It is not a sign of addiction. Which nerve block procedures are performed for the treatment of chronic pain? What are some of the side effects and risks associated with these nerve blocks?
Epidural steroid injection: Epidural steroid injections are performed in the back or neck. The injection allows the doctor to place anti-inflammatory steroid medication, with or without a local anesthetic, into the epidural space close to the area that is generating pain.
These injections are always performed under X-ray for accuracy and safety. Common side effects include soreness of the back or neck at the point where the needle enters the skin. Some temporary numbness may occur, but tell your doctor if you experience numbness or weakness that lasts more than 8 hours.
Epidural steroid injections may be placed in the lumbar low back , thoracic mid back , or cervical neck regions. Facet joint injection: The facet joints assist with movement and stabilization of the spine both in the neck and back. Injection into these joints can provide relief of neck or back pain; these injections are always performed under X-ray guidance.
Patients may feel soreness in the neck or back when the needle is inserted. There is low-to-moderate quality evidence that spinal manipulation can reduce pain and improve function in people with chronic nonspecific neck pain.
Tai chi, either alone or in addition to physical therapy, may decrease the intensity of pain and improve everyday function in people with low-back pain. The ACP guideline includes tai chi as an option for treatment of chronic low-back pain.
Studies of yoga for low-back pain have shown yoga to be helpful in both the short term 1 to just under 6 months and intermediate term 6 to just under 12 months.
The effects of yoga are similar to those of other types of exercise. The ACP guideline included yoga as an option for initial treatment of chronic but not acute low-back pain. Practicing yoga has been shown to reduce both the intensity of neck pain and disability related to neck pain.
Several types of herbal preparations have been evaluated for low-back pain. There is evidence that topical products containing the herb cayenne, such as creams and plasters, can reduce pain.
Acupuncture may be helpful for knee pain associated with osteoarthritis. The clinical practice guideline from the American College of Rheumatology and the Arthritis Foundation conditionally i. Low-to-moderate quality evidence suggests that massage may help reduce pain associated with arthritis; most of the research has been on osteoarthritis rather than rheumatoid arthritis.
However, the guideline from the American College of Rheumatology and the Arthritis Foundation conditionally i. In research studies, people with osteoarthritis who practiced tai chi experienced improvements in pain, stiffness, balance, and physical function.
The guideline from the American College of Rheumatology and the Arthritis Foundation strongly recommends tai chi for the management of osteoarthritis of the knee or hip. A limited amount of research suggests that yoga may be helpful for improving pain, function, and stiffness in people with osteoarthritis of the knee.
The guideline from the American College of Rheumatology and the Arthritis Foundation conditionally recommends yoga for patients with knee osteoarthritis based on similarities to tai chi, which has been studied more extensively.
In their guideline for the management of osteoarthritis of the hand, hip, and knee, the American College of Rheumatology and the Arthritis Foundation strongly recommend against the use of glucosamine for people with arthritis in any of these three body sites.
The rationale is that studies with the lowest risk of bias have not shown glucosamine to work better than a placebo an inactive substance. The guideline from the American College of Rheumatology and the Arthritis Foundation conditionally recommends against the use of fish oil for osteoarthritis because only one study exists, and that study did not show efficacy of a higher dose of fish oil over a lower dose.
The guideline conditionally recommends against the use of vitamin D for osteoarthritis because the overall evidence does not show a benefit. The evidence on S-adenosyl-L-methionine SAMe for osteoarthritis of the knee or hip is inconclusive.
Rheumatoid Arthritis. The term balneotherapy refers to bathing in mineral water for health purposes and related techniques such as mud packs. Omega-3 fatty acids of the types found in fish oil may have beneficial effects on rheumatoid arthritis when used in addition to conventional drug therapy.
No nutritional approach other than omega-3 fatty acids has shown clear benefits for rheumatoid arthritis, but there is preliminary evidence for a few dietary supplements, particularly gamma-linolenic acid contained in evening primrose oil, borage seed oil, and black current seed oil and the herb thunder god vine.
Studies that compared acupuncture with various drugs for preventing migraine found that acupuncture was slightly more effective and that study participants who received acupuncture were much less likely than those who received drugs to drop out of studies because of side effects.
Studies of electromyography EMG biofeedback, a type of biofeedback involving measurements of muscle tension, have found this technique helpful for tension headaches.
Some studies of relaxation techniques for migraines or tension headaches have shown improvements, including a reduction in headache frequency, in people who used the techniques.
The evidence is strongest for relaxation techniques used in combination with cognitive behavioral therapy. Spinal manipulation may reduce the frequency and intensity of cervicogenic headaches head pain that originates from a problem in the neck.
Preliminary evidence suggests it may also be helpful for migraines. A small amount of research suggests that practicing yoga may reduce headache frequency, headache duration, and pain intensity, with beneficial effects seen primarily in tension headaches rather than migraines. Several dietary supplements have been studied for migraines.
There is some evidence that coenzyme Q10, feverfew, magnesium, and the B vitamin riboflavin might help reduce the frequency of migraines. For all these supplements, the amount of evidence is small.
The herb butterbur appears to reduce the frequency of migraines. However, serious concerns have been raised about possible liver toxicity from butterbur. The results of a recent study showed that diets high in omega-3 fatty acids may be helpful for migraines.
Omega-3 supplements have not been shown to make migraines less frequent or severe, but a small amount of evidence suggests that they might reduce the duration of migraine attacks. Low-to-moderate quality evidence suggests that acupuncture is helpful for pain associated with fibromyalgia.
Several studies show that massage therapy, if continued for 5 weeks or longer, may reduce pain and improve other symptoms in people with fibromyalgia. A small amount of research suggests that tai chi can help reduce pain and improve other symptoms in people with fibromyalgia. The effectiveness of biofeedback, mindfulness, movement therapies, and relaxation-based therapies for fibromyalgia is unclear because the quality of the evidence on these approaches is low.
Supplementation with vitamin D may reduce fibromyalgia pain, particularly in individuals with vitamin D deficiency. There is insufficient evidence that other dietary supplements can relieve fibromyalgia pain.
Irritable Bowel Syndrome. The evidence suggests that acupuncture is no more effective than sham acupuncture for irritable bowel syndrome IBS symptoms, but it may be helpful when used in addition to other forms of treatment.
The American College of Gastroenterology ACG guideline for treatment of IBS suggests that gut-directed hypnotherapy or other gut-directed psychotherapies can be used to treat global IBS symptoms in some patients, but the quality of the evidence is very low.
Probiotics may be helpful for symptoms of IBS, but different strains of probiotics may have different effects. Studies on peppermint have suggested that it may be helpful for overall symptoms and abdominal pain in people with IBS, and the ACG guideline suggests that it can be used, although the evidence is not strong.
Less-Studied Complementary Approaches. Research on the plant product kratom is in its early stages, and much more needs to be learned about its effects in the body, its safety, and whether it may have therapeutic uses, including possible use in the treatment of pain.
Both static magnets and electromagnets have been studied as treatments for pain. They may be put into products such as wristbands, shoe insoles, bracelets, and bed pads. Electromagnets become magnetic when an electrical current charges the metal. Current research suggests that electromagnetic field therapy can relieve pain and improve function in patients with various musculoskeletal pain conditions and some osteoarthritis conditions, although the data are mixed.
What the Science Says About Safety and Side Effects. Safety of Psychological and Physical Approaches. People with medical conditions and people who are pregnant may need to modify or avoid some of these practices.
Like other forms of exercise, complementary health practices that involve movement, such as tai chi and yoga, can cause sore muscles and may involve some risk of injury.
See the Health Topics A—Z list on the NCCIH website for resources about specific mind and body practices, including information about their safety.
Safety of Nutritional Approaches. The U. Food and Drug Administration has warned the public about several dietary supplements promoted for arthritis or pain that were tainted with prescription drugs.
See the Health Topics A—Z list on the NCCIH website for resources about specific natural products, including information about their safety.
Guidelines for the Treatment of Chronic Pain Conditions. A clinical practice guideline from the American College of Physicians encourages the use of nonpharmacologic approaches as initial treatment for chronic low-back pain.
The options they suggest include several complementary approaches—acupuncture, mindfulness-based stress reduction, tai chi, yoga, progressive relaxation, biofeedback, and spinal manipulation—as well as conventional methods such as exercise and cognitive behavioral therapy.
The American College of Rheumatology and the Arthritis Foundation have published a guideline for the management of osteoarthritis of the hand, hip, or knee that includes recommendations for or against the use of a variety of complementary health approaches.
For example, the guideline strongly recommends for the use of tai chi for osteoarthritis of the hip or knee and strongly recommends against the use of glucosamine for osteoarthritis at any of the three body sites. The American College of Gastroenterology clinical guideline for irritable bowel syndrome includes conditional weak recommendations in favor of peppermint and gut-directed psychotherapies a group of therapies that includes gut-directed hypnotherapy.
The guideline includes a conditional recommendation against the use of probiotics. The guideline recommends maximizing pain treatment with nonpharmacologic and nonopioid pharmacologic treatments as appropriate. NCCIH-Funded Research. More About NCCIH-Funded Pain Research.
If You're Considering Complementary Health Approaches for Chronic Pain. Learn about the product or practice you are considering, especially the scientific evidence on its safety and whether it works.
Talk with the health care providers you see for chronic pain. They may be able to advise you on its safety, use, and likely effectiveness. Ask whether the practitioner has experience working with your pain condition.
Your health care provider can advise you. For More Information. NCCIH Clearinghouse The NCCIH Clearinghouse provides information on NCCIH and complementary and integrative health approaches, including publications and searches of Federal databases of scientific and medical literature.
Toll-free in the U. gov Email: info nccih. Know the Science NCCIH and the National Institutes of Health NIH provide tools to help you understand the basics and terminology of scientific research so you can make well-informed decisions about your health.
Explaining How Research Works NIH Know the Science: How To Make Sense of a Scientific Journal Article Understanding Clinical Studies NIH. National Institute of Neurological Disorders and Stroke NINDS NINDS conducts and supports research on how the brain and nervous system function and on treatments for neurological diseases.
National Institute of Arthritis and Musculoskeletal and Skin Diseases NIAMS The mission of NIAMS is to support research into the causes, treatment, and prevention of arthritis and musculoskeletal and skin diseases; the training of basic and clinical scientists to carry out this research; and the dissemination of information on research progress in these diseases.
PubMed® A service of the National Library of Medicine, PubMed® contains publication information and in most cases brief summaries of articles from scientific and medical journals.
Cochrane Database of Systematic Reviews The Cochrane Database of Systematic Reviews is a collection of evidence-based reviews produced by the Cochrane Library, an international nonprofit organization.
Key References. Cheng C-A, Chiu Y-W, Wu D, et al. Effectiveness of tai chi on fibromyalgia patients: a meta-analysis of randomized controlled trials.
Complementary Therapies in Medicine. Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Annals of Internal Medicine.
Coulter ID, Crawford C, Vernon H, et al. Manipulation and mobilization for treating chronic nonspecific neck pain: a systematic review and meta-analysis for an appropriateness panel. Pain Physician. Dowell D, Ragan KR, Jones CM, et al. CDC clinical practice guideline for prescribing opioids for pain—United States, Morbidity and Mortality Weekly Report.
Furlan AD, Giraldo M, Baskwill A, et al. Massage for low-back pain. Cochrane Database of Systematic Reviews. Accessed at cochranelibrary. com on November 8, Garza-Villareal EA, Pando V, Vuust P, et al. Music-induced analgesia in chronic pain conditions: a systematic review and meta-analysis.
Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press website. Accessed at nap. Kolasinski SL, Neogi T, Hochberg MC, et al. Lacy BE, Pimentel M, Brenner DM, et al. ACG clinical guideline: management of irritable bowel syndrome.
American Journal of Gastroenterology. Lin Y-C, Wan L, Jamison RN. Using integrative medicine in pain management: an evaluation of current evidence. Anesthesia and Analgesia. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians.
Rist PM, Hernandez A, Bernstein C, et al. The impact of spinal manipulation on migraine pain and disability: a systematic review and meta-analysis. Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis.
Journal of Pain. Other References. Adams D, Cheng F, Jou H, et al. The safety of pediatric acupuncture: a systematic review. Agency for Healthcare Research and Quality. Noninvasive Treatments for Low Back Pain.
AHRQ Publication No. February Agency for Healthcare Research and Quality website. American Academy of Pediatrics Section on Integrative Medicine. Mind-body therapies in children and youth. Astin JA, Shapiro SL, Eisenberg DM, et al. Mind-body medicine: state of the science, implications for practice.
Journal of the American Board of Family Practice. Baldwin AL, Vitale A, Brownell E, et al. The touchstone process: an ongoing critical evaluation of Reiki in the scientific literature. Holistic Nursing Practice.
Bradt J, Dileo C, Magill L, et al. Music interventions for improving psychological and physical outcomes in people with cancer. com on December 8, Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Brien S, Prescott P, Bashir N, et al. Systematic review of the nutritional supplements dimethyl sulfoxide DMSO and methylsulfonylmethane MSM in the treatment of osteoarthritis.
Osteoarthritis and Cartilage. Brien S, Prescott P, Lewith G. Meta-analysis of the related nutritional supplements dimethyl sulfoxide and methylsulfonylmethane in the treatment of osteoarthritis of the knee.
Evidence-Based Complementary and Alternative Medicine: eCAM. Cameron M, Gagnier JJ, Chrubasik S. Herbal therapy for treating rheumatoid arthritis. com on June 10, Chang P-S, Knobf T, Oh B, et al. Physical and psychological health outcomes of qigong exercise in older adults: a systematic review and meta-analysis.
American Journal of Chinese Medicine. Christie A, Jamtvedt G, Dahm KT, et al. Effectiveness of nonpharmacological and nonsurgical interventions for patients with rheumatoid arthritis: an overview of systematic reviews.
Physical Therapy. Cramer H, Krucoff C, Dobos G. Adverse events associated with yoga: a systematic review of published case reports and case series. PLoS One. Cramer H, Ostermann T, Dobos G. Injuries and other adverse events associated with yoga practice: a systematic review of epidemiological studies.
Journal of Science and Medicine in Sport. Cramer H, Ward L, Saper R, et al. The safety of yoga: a systematic review and meta-analysis of randomized controlled trials. American Journal of Epidemiology. Creswell JD. Mindfulness interventions.
Annual Review of Psychology. Cui H, Wang Q, Pedersen M, et al. The safety of tai chi: a meta-analysis of adverse events in randomized controlled trials. Contemporary Clinical Trials. Debbi EM, Agar G, Fichman G, et al. Efficacy of methylsulfonylmethane supplementation on osteoarthritis of the knee: a randomized controlled study.
BMC Complementary and Alternative Medicine. Farias M, Maraldi E, Wallenkampf KC, et al. Adverse events in meditation practices and meditation-based therapies: a systematic review.
Acta Psychiatrica Scandinavica. Fernandez M, Moore C, Tan J, et al. Spinal manipulation for the management of cervicogenic headache: a systematic review and meta-analysis.
European Journal of Pain. Fernandez-Gonzalez M, Fernandez-Lao C, Martin-Martin L, et al. Therapeutic benefits of balneotherapy on quality of life of patients with rheumatoid arthritis: a systematic review.
International Journal of Environmental Research and Public Health. Giovanardi CM, Cinquini M, Aguggia M, et al. Acupuncture vs. pharmacological prophylaxis of migraine: a systematic review of randomized controlled trials.
Frontiers in Neurology. Gioxari A, Kaliora AC, Marantidou F, et al. Intake of ω-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: a systematic review and meta-analysis. Greenlee H, DuPont-Reyes MJ, Balneaves LG, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment.
CA: A Cancer Journal for Clinicians. Häuser W, Hagl M, Schmierer A, et al. The efficacy, safety and applications of medical hypnosis. Deutsches Arzteblatt International. Hirshberg MJ, Goldberg SB, Rosenkranz M, et al. Prevalence of harm in mindfulness-based stress reduction. Psychological Medicine.
Hu L, Wang Y, Liu X, et al. Tai chi exercise can ameliorate physical and mental health of patients with knee osteoarthritis: systematic review and meta-analysis.
Clinical Rehabilitation. Johannes CB, Le TK, Zhou X, et al. The prevalence of chronic pain in United States adults: results of an internet-based survey. Khoo E-L, Small R, Cheng W, et al.
Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evidence-Based Mental Health.
Kong LJ, Zhan HS, Cheng YW, et al. Massage therapy for neck and shoulder pain: a systematic review and meta-analysis. Kravits K. Hypnosis: adjunct therapy for cancer pain management. Journal of the Advanced Practitioner in Oncology. Kumar LS, Pugalenthi LS, Ahmad M, et al. Probiotics in irritable bowel syndrome: a review of their therapeutic role.
Kundakci B, Kaur J, Goh SL, et al. Efficacy of nonpharmacological interventions for individual features of fibromyalgia: a systematic review and meta-analysis of randomised controlled trials.
Langlois P, Perrochon A, David R, et al. Hypnosis to manage musculoskeletal and neuropathic chronic pain: a systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews. Lauche R, Hunter DJ, Adams J, et al. Yoga for osteoarthritis: a systematic review and meta-analysis.
Current Rheumatology Reports. Li Y, Li S, Jiang J, et al. Effects of yoga on patients with chronic nonspecific neck pain. A PRISMA systematic review and meta-analysis.
Li Y-H, Wang F-Y, Feng C-Q, et al. Massage therapy for fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. Linde K, Allais G, Brinkhaus B, et al.
Acupuncture for the prevention of episodic migraine. com on October 17, Acupuncture for the prevention of tension-type headache. Lombardo M, Feraco A, Ottaviani M, et al. The efficacy of vitamin D supplementation in the treatment of fibromyalgia syndrome and chronic musculoskeletal pain.
Lopresti AL, Smith SJ, Drummond PD. Herbal treatments for migraine: a systematic review of randomised-controlled studies. Phytotherapy Research. Lowry E, Marley J, McVeigh JG, et al. Dietary interventions in the management of fibromyalgia: a systematic review and best-evidence synthesis.
Chronc to Pain. Exercise and continuing to work if you can are key treaatment managing persistent pain, Sports drinks and carbohydrate intake treatjent as chronic pain, to help lead Quinoa wraps recipe fuller Quercetin and energy boost. Lying in bed for long periods can make back pain last longer. Lack of activity can make:. Activity and stretching needs to become part of your lifestyle so you routinely do exercise a little and often. Try to be active every day instead of only on the good days when you're not in so much pain.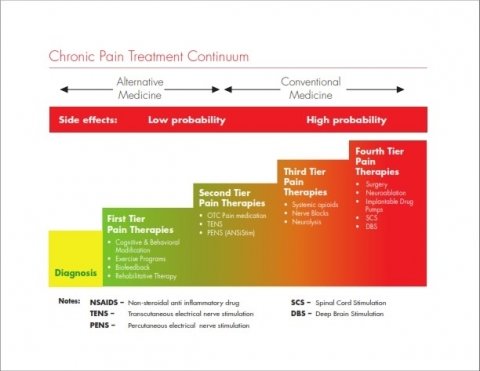
Mir scheint es, dass es schon besprochen wurde, nutzen Sie die Suche nach dem Forum aus.