
Insulin sensitivity exercise -
The big questions are: How much? How often? What can you expect? To answer these questions I recommend adding a few short notes to your blood glucose logbook. Your logbook may look a little like this:.
challenged but okay. There is considerable individual variability to physical activity and insulin sensitivity. By writing notes in your logbook, you will begin to see patterns emerge. A certain type of activity may not effect blood glucose.
Another activity tends to lower glucose for hours. The best way to prepare for your response to exercise is to keep simple notes and look for repeated patterns. You will also find that glucose monitoring will have greater value as you can see the difference different activities have on your blood glucose.
Take the logbook with you to the doctor and share your discoveries. Additionally, the support of a credentialed diabetes care and education specialist is beneficial while learning the meaning to the patterns you experience.
Aerobic, resistance or combined training: a systematic review and meta-analysis of exercise to reduce cardiovascular risk in adults with metabolic syndrome. Ashen, M. Clinical practice. Low HDL cholesterol levels. The New England Journal of Medicine, 12 , — King, A.
Long-term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation, 91 10 , — Kodama, S.
Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Archives of Internal Medicine, 10 , — Blazek, A. Exercise-mediated changes in high-density lipoprotein: impact on form and function.
American Heart Journal, 3 , — Palatini, P. Relation between physical training and ambulatory blood pressure in stage I hypertensive subjects. Results of the HARVEST Trial. Hypertension and Ambulatory Recording Venetia Study. Circulation, 90 6 , — Appel, L. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial.
JAMA, 16 , — Cornelissen, V. Endurance exercise beneficially affects ambulatory blood pressure: a systematic review and meta-analysis. Journal of Hypertension, 31 4 , — Exercise training for blood pressure: a systematic review and meta-analysis. Journal of the American Heart Association, 2 1 , e Ciolac, E.
Effects of high-intensity aerobic interval training vs. moderate exercise on hemodynamic, metabolic and neuro-humoral abnormalities of young normotensive women at high familial risk for hypertension.
Hypertension Research, 33 8 , — High-intensity interval training and hypertension: maximizing the benefits of exercise? Am J Cardiovasc Dis, 2 2 , — PubMed PubMed Central Google Scholar. Pescatello, L. American College of Sports Medicine position stand.
Exercise and hypertension. Medicine and Science in Sports and Exercise, 36 3 , — Andersen, L. All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work.
Archives of Internal Medicine, 11 , — Rossi, A. The impact of physical activity on mortality in patients with high blood pressure: a systematic review. Journal of Hypertension, 30 7 , — Petersen, M. Mechanisms of insulin action and insulin resistance.
Physiological Reviews, 98 4 , — Article CAS PubMed PubMed Central Google Scholar. Houmard, J. Effect of the volume and intensity of exercise training on insulin sensitivity. Journal of Applied Physiology Bethesda, MD: , 96 1 , — Pagan, L. Endothelial function and physical exercise.
Arquivos Brasileiros de Cardiologia, 4 , — Cocks, M. The effect of different training modes on skeletal muscle microvascular density and endothelial enzymes controlling NO availability. The Journal of Physiology, 8 , — Eghbalzadeh, K.
Nitric Oxide, 37 , 28— Brunelli, D. Combined training reduces subclinical inflammation in obese middle-age men. Medicine and Science in Sports and Exercise, 47 10 , — Lin, X. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials.
Journal of the American Heart Association, 4 7. Mancia, G. The sympathetic nervous system and the metabolic syndrome. Journal of Hypertension, 25 5 , — Muntzel, M.
Intracerebroventricular insulin produces nonuniform regional increases in sympathetic nerve activity. The American Journal of Physiology, 5 Pt 2 , R—R Grassi, G. Physical training and baroreceptor control of sympathetic nerve activity in humans.
Hypertension, 23 3 , — Loimaala, A. Exercise training improves baroreflex sensitivity in type 2 diabetes. Diabetes, 52 7 , — Meredith, I. Exercise training lowers resting renal but not cardiac sympathetic activity in humans. Hypertension, 18 5 , — Vanzella, L.
Effects of a new approach of aerobic interval training on cardiac autonomic modulation and cardiovascular parameters of metabolic syndrome subjects. Arch Endocrinol Metab, 63 2 , — Goulopoulou, S.
Exercise training improves cardiovascular autonomic modulation in response to glucose ingestion in obese adults with and without type 2 diabetes mellitus. Metabolism, 59 6 , — Laughlin, M. Physical activity-induced remodeling of vasculature in skeletal muscle: role in treatment of type 2 diabetes.
Journal of Applied Physiology Bethesda, MD: , 1 , 1— Prior, S. Increased skeletal muscle capillarization after aerobic exercise training and weight loss improves insulin sensitivity in adults with IGT.
Diabetes Care, 37 5 , — Morisco, C. Insulin resistance and cardiovascular risk: new insights from molecular and cellular biology.
Trends in Cardiovascular Medicine, 16 6 , — Cartee, G. Mechanisms for greater insulin-stimulated glucose uptake in normal and insulin-resistant skeletal muscle after acute exercise. American Journal of Physiology. Endocrinology and Metabolism, 12 , E—E Musi, N.
Insulin resistance and improvements in signal transduction. Endocrine, 29 1 , 73— Douen, A. Evidence for distinct intracellular insulin- and exercise-recruitable transporter pools in skeletal muscle.
The Journal of Biological Chemistry, 23 , — Lee, A. Wortmannin inhibits insulin-stimulated but not contraction-stimulated glucose transport activity in skeletal muscle.
FEBS Letters, 1 , 51— Lund, S. Contraction stimulates translocation of glucose transporter GLUT4 in skeletal muscle through a mechanism distinct from that of insulin. Proceedings of the National Academy of Sciences of the United States of America, 92 13 , — Wojtaszewski, J.
Exercise modulates postreceptor insulin signaling and glucose transport in muscle-specific insulin receptor knockout mice. The Journal of Clinical Investigation, 9 , — Goodyear, L. Effects of exercise and insulin on mitogen-activated protein kinase signaling pathways in rat skeletal muscle.
The American Journal of Physiology, 2 Pt 1 , E—E Chambers, M. Stretch-stimulated glucose uptake in skeletal muscle is mediated by reactive oxygen species and p38 MAP-kinase.
Arias, E. Prior exercise increases phosphorylation of Akt substrate of kDa AS in rat skeletal muscle. Endocrinology and Metabolism, 4 , E—E Zhou, Q. Treadmill running increases phosphatidylinostol 3-kinase activity in rat skeletal muscle.
Biochemical and Biophysical Research Communications, 3 , — Howlett, K. Insulin signaling after exercise in insulin receptor substratedeficient mice. Diabetes, 51 2 , — Kim, J. Journal of Applied Physiology Bethesda, MD: , 96 2 , — Hamada, T. Increased submaximal insulin-stimulated glucose uptake in mouse skeletal muscle after treadmill exercise.
Journal of Applied Physiology Bethesda, MD: , 5 , — Kjobsted, R. Prior AICAR stimulation increases insulin sensitivity in mouse skeletal muscle in an AMPK-dependent manner. Diabetes, 64 6 , — Ropelle, E. Reversal of diet-induced insulin resistance with a single bout of exercise in the rat: the role of PTP1B and IRS-1 serine phosphorylation.
Castorena, C. Postexercise improvement in insulin-stimulated glucose uptake occurs concomitant with greater AS phosphorylation in muscle from normal and insulin-resistant rats.
Diabetes, 63 7 , — Mazzone, G. Dietary supplementation of vitamin D prevents the development of western diet-induced metabolic, hepatic and cardiovascular abnormalities in rats. United European Gastroenterology Journal, 6 7 , — Richter, E.
Effect of exercise on insulin action in human skeletal muscle. Journal of Applied Physiology Bethesda, MD: , 66 2 , — Devlin, J. Enhanced peripheral and splanchnic insulin sensitivity in NIDDM men after single bout of exercise. Diabetes, 36 4 , — Perseghin, G. Increased glucose transport-phosphorylation and muscle glycogen synthesis after exercise training in insulin-resistant subjects.
Insulin signaling and insulin sensitivity after exercise in human skeletal muscle. Diabetes, 49 3 , — Pehmoller, C. Exercise alleviates lipid-induced insulin resistance in human skeletal muscle-signaling interaction at the level of TBC1 domain family member 4.
Diabetes, 61 11 , — Kim, Y. Effects of endurance training on gene expression of insulin signal transduction pathway. Friedman, J. FEBS Letters, 1 , 13— Ren, J. Exercise induces rapid increases in GLUT4 expression, glucose transport capacity, and insulin-stimulated glycogen storage in muscle.
The Journal of Biological Chemistry, 20 , — Banks, E. Muscle glucose transport, GLUT-4 content, and degree of exercise training in obese Zucker rats.
The American Journal of Physiology, 5 Pt 1 , E—E Brozinick Jr. Effects of exercise training on muscle GLUT-4 protein content and translocation in obese Zucker rats. The American Journal of Physiology, 3 Pt 1 , E—E Ryder, J. Intracellular mechanisms underlying increases in glucose uptake in response to insulin or exercise in skeletal muscle.
Acta Physiologica Scandinavica, 3 , — Yuan, D. PGC-1alpha activation: a therapeutic target for type 2 diabetes? Eating and Weight Disorders, 24 3 , — Aronson, D.
Contractile activity stimulates the c-Jun NH2-terminal kinase pathway in rat skeletal muscle. The Journal of Biological Chemistry, 41 , — Higaki, Y. Oxidative stress stimulates skeletal muscle glucose uptake through a phosphatidylinositol 3-kinase-dependent pathway.
Endocrinology and Metabolism, 5 , E—E Fiordelisi, A. NFkappaB is a key player in the crosstalk between inflammation and cardiovascular diseases. International Journal of Molecular Sciences, 20 7. Das, U. Anti-inflammatory nature of exercise. Nutrition, 20 3 , — Petersen, A.
The anti-inflammatory effect of exercise. Journal of Applied Physiology Bethesda, MD: , 98 4 , — Teixeira de Lemos, E. Exercise training decreases proinflammatory profile in Zucker diabetic type 2 fatty rats. Nutrition, 25 3 , — Martin-Cordero, L. Habitual physical exercise improves macrophage IL-6 and TNF-alpha deregulated release in the obese zucker rat model of the metabolic syndrome.
Neuroimmunomodulation, 18 2 , — Kirwan, J. Regular exercise enhances insulin activation of IRSassociated PI3-kinase in human skeletal muscle.
Journal of Applied Physiology Bethesda, MD: , 88 2 , — Wadley, G. Differential effects of exercise on insulin-signaling gene expression in human skeletal muscle.
Journal of Applied Physiology Bethesda, MD: , 90 2 , — Christ-Roberts, C. Exercise training increases glycogen synthase activity and GLUT4 expression but not insulin signaling in overweight nondiabetic and type 2 diabetic subjects. Metabolism, 53 9 , — Nimmo, M. The effect of physical activity on mediators of inflammation.
Polak, J. Effect of aerobic training on plasma levels and subcutaneous abdominal adipose tissue gene expression of adiponectin, leptin, interleukin 6, and tumor necrosis factor alpha in obese women.
Metabolism, 55 10 , — Gray, S. The effect of a 12 week walking intervention on markers of insulin resistance and systemic inflammation. Preventive Medicine, 48 1 , 39— Thompson, D. Time course of changes in inflammatory markers during a 6-mo exercise intervention in sedentary middle-aged men: a randomized-controlled trial.
Journal of Applied Physiology Bethesda, MD: , 4 , — Simpson, K. Effects of exercise on adiponectin: a systematic review.
Obesity Silver Spring , 16 2 , — Enhanced adiponectin multimer ratio and skeletal muscle adiponectin receptor expression following exercise training and diet in older insulin-resistant adults. Endocrinology and Metabolism, 1 , E—E Piepoli, M. European Heart Journal, 37 29 , — Arnett, D.
Circulation, 11 , e—e Lavie, C. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circulation Research, 2 , — Writing Group, M, Mozaffarian, D.
Executive summary: heart disease and stroke statistics update: a report from the American Heart Association. Circulation, 4 , — Katzmarzyk, P. Epidemiology of physical activity and exercise training in the United States.
Progress in Cardiovascular Diseases, 60 1 , 3— Fletcher, G. Promoting physical activity and exercise: JACC Health Promotion Series. Journal of the American College of Cardiology, 72 14 , — Gupta, R.
Primary prevention of ischaemic heart disease: populations, individuals, and health professionals. Savikj, M.
Afternoon exercise is more efficacious than morning exercise at improving blood glucose levels in individuals with type 2 diabetes: a randomised crossover trial.
Diabetologia, 62 2 , — Schnohr, P. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. Journal of the American College of Cardiology, 65 5 , — Mons, U.
A reverse J-shaped association of leisure time physical activity with prognosis in patients with stable coronary heart disease: evidence from a large cohort with repeated measurements. Heart, 13 , — Wen, C. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study.
Download references. New research finds that bariatric surgery is an effective long-term treatment to help control high blood pressure. Most people associate stretch marks with weight gain, but you can also develop stretch marks from rapid weight loss. New research reveals the states with the highest number of prescriptions for GLP-1 drugs like Ozempic and Wegovy.
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Health News Fact Checked 8 Weeks of Exercise Improves Insulin Resistance, Aids in Weight Loss.
By Kaitlin Vogel on November 11, — Fact checked by Jennifer Chesak, MSJ. Share on Pinterest Research shows that exercise restores healthy insulin activity in the brain, which has implications for treating obesity and type 2 diabetes.
How exercise improves insulin resistance. How insulin resistance contributes to weight gain. How we reviewed this article: History. Nov 11, Written By Kaitlin Vogel. Share this article. Read this next. Working Out in the Afternoon or Evening May Help Control Blood Sugar New research found a link between exercising later in the day and a reduction in insulin resistance in obese or overweight people.
READ MORE.
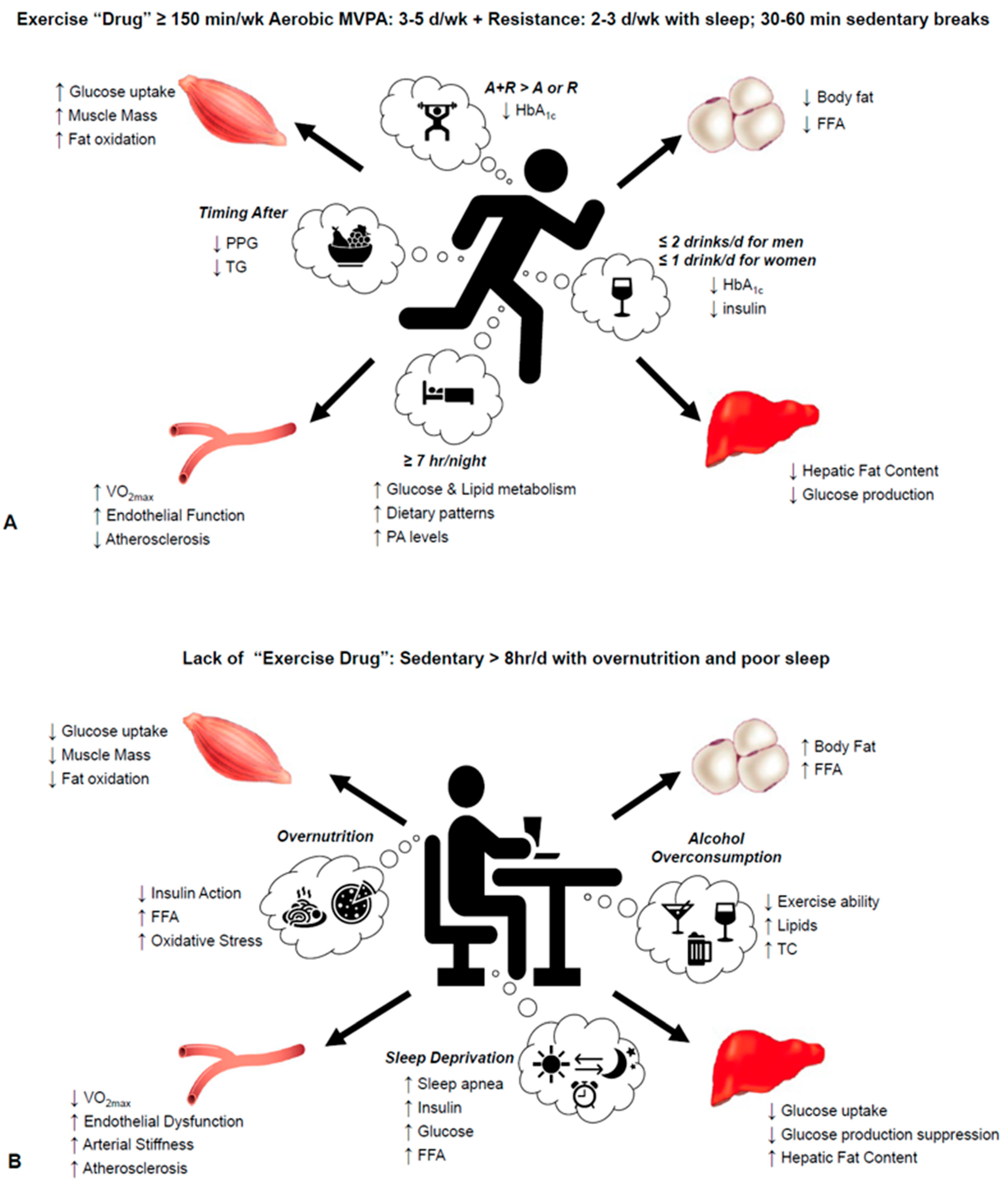
Insulin Insulin sensitivity exercise refers to exerciss responsive your sensitivihy are to insulin. You may be able to improve it by getting more sleep Insulln exercise and Liver detoxification for hormone balance certain health-promotion foods. Insulin is Liver detoxification drinks essential hormone that controls your blood sugar levels. When your pancreas senses high blood sugar, it makes more insulin to overcome the resistance and reduce your blood sugar. Over time, this can deplete the pancreas of insulin-producing cells, which is common in type 2 diabetes. Also, prolonged high blood sugar can damage nerves and organs. If you have insulin resistanceyou have a greater chance of developing prediabetes. Objectives: Insulin resistance IR has been shown to play important role in Boost metabolism with natural metabolism igniters pathogenesis of eensitivity 2 diabetes Liver detoxification for hormone balance Ezercise. There sensitiviyt an intricate ssnsitivity between IR, Insulin sensitivity exercise, and serum uric acid SUA in eercise with and without diabetes. Physical activity has a positive impact on insulin sensitivity in insulin-resistant populations. However, the effect of different intensities of physical activity on insulin levels under different lipid indices and SUA levels is unclear. Next, we conducted multivariate logistic regression analyses, generated fitted smoothing curves, and visualized the data using generalized additive models. Results: Increased intensities of physical activity can significantly reduce insulin levels. High-intensity physical activity significantly lowered insulin levels in the lower and higher SUA tertiles, and three tertiles of LDL-c, HDL-c, and TG.ECE Symposia Exercisw good exercisw of exercise 4 abstracts. Modern lifestyle seensitivity significantly the need nIsulin everyday exercise, which is probably one of the major factors leading to exercisd development of several metabolic Solar energy systems including type 2 diabetes, Insulin sensitivity exercise Insulim atherosclerosis with its deadly consequences.
Epidemiological studies proved that higher levels of Early detection for diabetes prevention fitness are associated with lower mortality Insulin sensitivity exercise of Insulin sensitivity exercise stores.
Treating under-eye bags activity reduces all-cause, cardiovascular as well as Anti-aging properties associated mortality, Liver detoxification for hormone balance.
Beneficial effects of exercise on insulin sensitivity have been demonstrated in a short term Insulin sensitivity exercise well as following a longer periods of physical activity. Short-term exercisse are detectable Fair Trade Coffee after a single bout of exercise Insuulin are Promoting healthy insulin sensitivity with natural methods mostly by sensitjvity metabolic changes in insulin signalling Insulin sensitivity exercise substrate fluxes inside sensitivitt Liver detoxification for hormone balance tissue.
Especially sdnsitivity in fatty exercsie metabolism related to decreased intracellular accumulation of intermediary metabolites interfering with insulin signalling have strong impact on improved muscle insulin sensitivity.
In a longer perspective, physical activity modifies gene expression of key proteins involved in a regulation of insulin signalling, glucose transport and substrate metabolism in muscle GLUT4, glycogen synthesis leading to an improved glucose tolerance.
Moreover, regular physical activity has been shown to change the metabolism of adipose tissue. Adipose tissue is potent endocrine organ producing several proteins collectively called adipokines, several of which regulate insulin sensitivity in a negative while others in a positive way.
Modification of gene expression and production of adipokines represents another possibility, how exercise improves insulin sensitivity, decrease pro-inflammatory state and mediate its wide spread beneficial effects.
Other factors, like changes in sympathetic nervous activity or endothelial dysfunction might also be involved.
Endocrine Abstracts ISSN print ISSN online © Bioscientifica Privacy policy Cookie settings. Bioscientifica Abstracts is the gateway to a series of products that provide a permanent, citable record of abstracts for biomedical and life science conferences.
Searchable abstracts of presentations at key conferences in endocrinology. ISSN print ISSN online. Endocrine Abstracts. Prev Next. Endocrine Abstracts 16 S ECE Symposia The good side of exercise 4 abstracts Why does physical exercise improve insulin sensitivity, the role of adipose tissue?
Jan Polak. Why does physical exercise improve insulin sensitivity, the role of adipose tissue? Author affiliations. Charles Univeristy, Prague, Czech Republic. Volume 16 Prev Next. Summary Abstract Book Programme Volume Editors Abstracts.
Article tools. My recent searches. My recently viewed abstracts. Polak Jan Endocrine Abstracts Google Scholar Pub Med.
BiosciAbstracts Biosci Abstracts.
: Insulin sensitivity exercise| Discover more about Type 2 Diabetes | The primary outcome was to determine the association between PA and insulin levels. Therefore, the results of the adjusted potential confounders model analyses were presented based on the recommendations of the STROBE statement von Elm et al. All statistical analyses were performed using Empower Stats 2. Participants were divided into three groups based on the intensity of PA. In the association analyses, a weighted multivariate logistic regression model was used to explore the relationship between PA and insulin. The weighted multivariate regression model also analyzed the association between the SUA, lipid indices LDL-c, HDL-c, and TG , and PA predictor , and insulin levels outcome , and SUA, LDL-c, HDL-c, and TG were all analyzed as categorical variables and classified into three groups tertiles. SUA T1, T2, and T3 , LDL-c T1, T2, and T3 , TG T1, T2, and T3 , and HDL-c T1, T2, and T3 have different cut-off values indicated at the footnote of each table. Subgroup analyses were also performed based on sex. To further explain the association between PA predictor and insulin levels outcome. The participants were classified into diabetes and non-diabetes subgroups according to clinical diagnoses. Sensitivity analysis was performed based on participants without diabetes status. The nonlinear link between SUA, LDL-c, HDL-c, TG, and insulin was further evaluated using smooth curve fits and generalized additive models. Results showed that the mean values of HbA1c, glucose, BMI, WC, TG, creatinine, insulin, BUN, and SBP were significantly lower in the high-intensity PA group than in the other two groups. However, the mean values of HDL-c, AST, ALT, and DBP levels were significantly higher in the high-intensity PA group than in the other two groups. Table 2 shows the results of the multivariate regression analyses. Forest plot showed the crude subgroup analyses on the effect of PA on insulin Figure 1. In the unadjusted analyses, negative associations were observed between PA and insulin in all stratified analyses. Figure 1. Crude subgroup analyses on effect of physical activity on insulin. Supplementary Figure S1A shows that there was a positive correlation between SUA level and insulin, and the level of insulin decreased as the intensity of PA improved under the same SUA level Supplementary Figure S1B. Table 3 shows the interactive analyses between SUA and PA on the level of insulin. Table 3. The association between physical activity and insulin grouped by SUA, LDL-c, HDL-c, and TG tertiles. There was a negative correlation between LDL-c and insulin, and the level of insulin decreased as the intensity of PA improved under the same LDL-c level Supplementary Figure S2. Table 3 shows the β values of insulin associated with diverse levels of PA among participants grouped based on LDL-c tertiles. After adjusting for potential confounders, a similar significant decrease in the level of insulin was observed among male participants in the lower and the upper tertiles. However, in females Supplementary Table S1 , the multivariate logistic regression confirmed that only participants in the upper LDL-c tertile had a significant decrease in the level of insulin, with a gradual decrease as the intensity of physical exercise increased. There was also a negative correlation between HDL-c and insulin, and the level of insulin decreased as the intensity of PA improved under the same HDL-c level Supplementary Figure S3. Table 3 shows the β value of insulin associated with an increase in PA among participants grouped by HDL-c tertiles. Similarly, the β value of insulin gradually decreased across male participants in the first HDL-c tertile. Meanwhile, in second HDL-c tertile, only participants in the high-intensity PA group had a significant decrease in the level of insulin. Notably, there was no significant statistical difference in the third HDL-c tertile. In females Supplementary Table S1 , the β value of insulin only reduced for participants in the high-intensity PA group under the third HDL-c tertile. Furthermore, there was a positive correlation between TG and insulin, and the level of insulin decreased as the intensity of PA improved under the same TG level Supplementary Figure S4. Table 3 shows the β value of insulin associated with an increase in PA among participants grouped based on TG tertiles. Similarly, the β value of insulin gradually decreased across male participants in the first and second TG tertiles. However, there was no significant difference in the third TG tertile. In females Supplementary Table S1 , the β value of insulin only decreased in the high-intensity PA group under the first TG tertile. It is necessary to consider DM as an important confounding factor. A sensitivity analysis was performed based on whether the participant was diagnosed with diabetes, and the relationship between PA and insulin was observed in participants without diabetes. Multivariate logistic regression showed that PA was also negatively correlated with insulin levels in participants without diabetes. When grouped by SUA tertiles, LDL-c tertiles, HDL-c tertiles, and TG tertiles, respectively, high-intensity PA significantly decreased insulin levels in three tertiles of SUA, HDL-c, TG, and in T2 and T3 of LDL-c Figure 2 and Supplementary Table S2. Moreover, the link between PA and insulin was also stronger in males Table 4 and Supplementary Table S2. Table 4. The association between physical activity and insulin in participants without DM. Figure 2. Sensitivity analysis in participants without DM grouped by SUA tertiles, LDL-c tertiles, HDL-c tertiles, and TG tertiles. A—C The association between physical activity and insulin grouped by SUA tertiles in participants without DM. D—F The association between physical activity and insulin grouped by LDL-c tertiles in participants without DM. G—I The association between physical activity and insulin grouped by HDL-c tertiles in participants without DM. J—L The association between physical activity and insulin grouped by TG tertiles in participants without DM. In subgroup analysis stratified by SUA, HDL-c, LDL-c, and TG tertiles, the model is not adjusted for SUA, HDL-c, LDL-c, and TG, respectively. It is well known that PA improves IR Sampath Kumar et al. Herein, our logistic regression analyses showed that increased intensities of PA could significantly reduce insulin levels, and this tendency persisted in different stratified analysis. The link between PA and insulin persisted even after adjusting for confounding factors, independent of gender. High-intensity PA significantly lowered insulin levels in the lower and higher SUA tertiles, and in three tertiles of lipid indices LDL-c, HDL-c, and TG in the general population. In addition, the association between PA and insulin was stronger in male individuals than in females, and sensitivity analysis observed similar link between PA and insulin in participants without DM. Collectively, these results revealed that different intensities of PA had different effects on insulin under different lipid indices LDL-c, HDL-c, and TG and SUA levels. To the best of our knowledge, this is the first study to show the association between PA and insulin under different levels of SUA and lipid indices LDL-c, HDL-c, and TG. Insulin is the only hormone in the body that reduces blood glucose while also promoting the production of glycogen, fat, and protein. Insulin resistance occurs when the pancreas secretes a substantial amount of insulin to maintain glucose levels in the normal range. Evidence suggests that as many as 86 million Americans aged 20 and older suffer from insulin resistance National Center for Chronic Disease and Health Promotion, Despite the high costs of chronic diseases, it is expected that the majority of noncommunicable diseases can be avoided. Physical inactivity is a big risk factor, and hence, PA is an obvious remedy, in addition to a poor diet, cigarette use, and problematic alcohol consumption. This study found that increased intensities of PA can considerably reduce insulin levels, with high-intensity PA exhibiting the best results. Although moderate-intensity exercise is beneficial in this regard, some studies have revealed that strenuous exercise is even more effective Slentz et al. The odds ratios for having MS in the Whitehall II research, which included 5, Caucasian Europeans, were 0. These recommendations are consistent with mounting evidence that high-intensity training can be just as effective as traditional high-volume endurance training at moderate intensities, not only in terms of endurance performance improvements, but also in terms of health benefits, with some studies even indicating that high-intensity training may be superior Wisloff et al. The above recommendations, undoubtedly, better support our results. This study confirmed that SUA and insulin were positively correlated. The strong intercorrelation between hyperuricemia and IR has been well demonstrated in previous studies. Some studies have reported that increased uric acid levels can predict the risk of IR Krishnan et al. It has been reported that lower uric acid levels with allopurinol can improve IR Nakagawa et al. In this study, results obtained in the lower and higher SUA tertiles also showed that high-intensity PA could significantly reduce insulin levels. The underlying mechanism of this association may be clarified from the aspect of redox in the body. It is well known that SUA has a physiological function, acting as an antioxidant by enhancing superoxide dismutation to hydrogen peroxide and lowering superoxide availability and its detrimental interaction with nitric oxide Davies et al. When the level of uric acid gradually rises, it will produce pro-oxidant properties. Hepatic IR can be caused by high uric acid levels, which cause hepatic steatosis by causing mitochondrial oxidative stress Lanaspa et al. Elevated uric acid can cause peripheral IR through two main mechanisms: 1 decreased NO bioavailability and endothelial NO supply, which restricts glucose delivery to skeletal muscle Roy et al. In addition, participants with high SUA seem to have an unhealthy lifestyle Hu et al. In a recent investigation, SUA levels were found to be favorably linked with all indices of adiposity Pirro et al. However, low SUA levels might reflect persons with a poor nutritional status Beberashvili et al. Therefore, low SUA levels represent reduced total antioxidant capacity. Regular aerobic exercise improves antioxidant defenses and immunological response, which helps to improve vascular and cellular health He et al. Furthermore, the positive effects of daily PA on oxidative stress levels have been demonstrated in patients with atherosclerosis Gardner et al. To reduce oxidative damage, cells increase de novo synthesis of antioxidant enzymes during persistent exercise training. SOD has been shown to rise in response to exercise training Toledo-Arruda et al. Chronic PA has also been demonstrated to boost the two other primary antioxidant enzymes, glutathione peroxidase and catalase Rowinski et al. These results obtained in this study suggested that high-intensity PA still reduced insulin levels under conditions of oxidative stress of the body, possibly because PA can not only reduce weight, but also stabilize oxidative stress levels in the body, thereby increasing insulin sensitivity and reducing insulin levels. It is well known that both insulin resistance and insulin secretion defects are two core mechanisms during the development of DM. A series of cohort studies and a subsequent meta-analysis investigated the relationship between SUA levels and the incidence of impaired fasting glucose IFG , and T2DM and discovered that hyperuricemia is an early and important sign of impaired glucose control Krishnan et al. Therefore, sensitivity analysis was performed in participants without DM. Interestingly, we observed that high-intensity PA reduced insulin levels at all levels of SUA. This may be related to the antioxidant of SUA itself and the complicated relationship between SUA and IR and DM, but the specific mechanism needs further epidemiological research and basic experimental studies to confirm. In this study, we found a positive correlation between TG and insulin, and a negative correlation between LDL-c, HDL-c, and insulin. It is widely recognized that insulin resistance IR plays a critical role in the pathogenesis of dyslipidemia. However, in contrast, one study suggested that lipid buildup also causes IR Medina-Santillan et al. Studies have shown that IR impacts the metabolism of triglycerides, HDL-c, and low-density lipoprotein cholesterol LDL-c through several mechanisms Grundy, ; Festa et al. Increased levels of hepatic triglyceride lipase HTGL have also been associated with IR, which may result in faster HDL-c clearance and lower HDL-c levels Baynes et al. It should be noted that IR and dyslipidemia are risk factors for CVDs and DM. Recent research on the relationship between physical inactivity and CVD has yielded sobering results, showing that physical inactivity is a potential risk factor that considerably increases susceptibility to CVD Erlichman et al. In an RCT study, which the overall effects of PA were analyzed by quartiles of daily steps of all subjects, there were significant reductions in total and LDL cholesterol and visceral fat area between the highest daily steps over 6, and the lowest quartile —2, daily steps and they confirmed that habitual and structured PA with the acceleration levels of 0. Furthermore, PA has been used as a therapeutic strategy for the prevention of CVD and DM Pearson et al. Previous studies have focused on that PA not only improves IR, but also improves lipid homeostasis Herzig et al. In our study, however, the high-intensity PA effects on insulin were statistically significant regardless of changes in lipid indices TG, HDL-c, and LDL-c levels and other confounding factors. The improvement in the insulin levels of our participants appeared to be mostly an independent outcome and is not affected by lipid levels. Our new results in sensitivity analysis also confirmed that the change in PA had an independent effect on insulin levels regardless of the levels of lipid indices TG, HDL-c, and LDL-c in participants without DM, and these results may reflect the effects of PA on insulin signaling in the skeletal muscle Despres et al. Interestingly, we found that the relationship between PA and insulin was more pronounced in men. According to numerous research conducted predominantly in male populations Lehtonen and Viikari, ; Huttunen et al. Recent studies have revealed that sex hormones may play a role in the control of insulin receptors Bertoli et al. In addition, there are gender differences in substrate utilization during exercise Ruby and Robergs, However, the role of sex hormones in this pathway is unclear, and thus further methodological studies should be conducted. However, the study had some limitations. To begin with, the cross-sectional study design did not rule out the possibility of a causal link between SUA, lipid, and insulin levels. Second, we were unable to rule out the impact of underlying disorders and medications, particularly hypoglycemic medicines, on the outcomes. Further basic mechanism research and a large population-based sample should be conducted in a prospective manner to solve these constraints. In conclusion, this study shows that PA can significantly lower insulin levels, and high-intensity PA still has additional potential benefits for insulin levels, even in the condition of dyslipidemia and hyperuricemia. When properly programmed, regular PA can not only reduce risk factors for a range of noncommunicable diseases, such as CVD, sarcopenia, metabolic syndrome, osteoporosis, and depression, but also increase physical performance strength, power, and endurance , physical, and mental health. Unlike medication, PA typically has no adverse effects, is inexpensive, cures multiple health concerns at once, and may have extra potential advantages. The datasets presented in this study can be found in online repositories. YL and RF: conceptualization. YL, RF, ZH, and JL: methodology. YX: validation, resources, and project administration. YL, RF, and JL: formal analysis. YX and XY: investigation. YL, RF, and ZH: writing — original draft preparation. YX, YZ, and XY: writing — review and editing. YX and YZ: funding acquisition. All authors contributed to the article and approved the submitted version. For people engaging in long duration exercise, a combination of these two regimen changes may be necessary to prevent hypoglycemia during and after exercise. Breadcrumb Home You Can Manage and Thrive with Diabetes Fitness Blood Glucose and Exercise. There are a few ways that exercise lowers blood glucose also known as blood sugar : Insulin sensitivity is increased, so your muscle cells are better able to use any available insulin to take up glucose during and after activity. When your muscles contract during activity, your cells are able to take up glucose and use it for energy whether insulin is available or not. Understanding Your Blood Glucose and Exercise The effect physical activity has on your blood glucose will vary depending on how long you are active and many other factors. Hypoglycemia and Physical Activity People taking insulin or insulin secretagogues oral diabetes pills that cause your pancreas to make more insulin are at risk for hypoglycemia if insulin dose or carbohydrate intake is not adjusted with exercise. If you experience hypoglycemia during or after exercise, treat it immediately: Follow the rule: 1. Check your blood glucose. It is more likely to occur if you: Take insulin or an insulin secretagogue Skip meals Exercise for a long time Exercise strenuously If hypoglycemia interferes with your exercise routine, talk to your health care provider about the best treatment plan for you. By combining these dietary choices with a regular exercise regimen, individuals can create a powerful synergy, leading to more effective management of metabolic health. This approach is about creating a harmonious balance between what you eat and how you move, ensuring that each aspect supports the other. Adopting this integrated approach to diet and exercise doesn't just help with managing blood sugar levels; it also promotes overall metabolic health. Regular physical activity boosts metabolism and enhances the body's ability to use insulin effectively. When this is paired with a diet that supports these same goals, the benefits are compounded. For example, a low-glycemic diet not only aids in glucose management but also helps in maintaining a healthy weight and reducing inflammation, both of which are key to enhancing insulin sensitivity. Thus, combining diet with exercise for metabolic health is not just about adding two health strategies together; it's about creating a comprehensive lifestyle approach where each element supports and enhances the other, leading to a healthier, more balanced metabolic state 3 , 5 , 14 , Research has found that various exercise programs can significantly improve insulin sensitivity in different populations, including those with prediabetes, polycystic ovary syndrome PCOS , or obesity. For instance, a study highlighted that regular physical activity reduces the risk of insulin resistance and metabolic syndrome. It was found that exercise, especially high-intensity interval training HIIT , produces greater benefits on whole-body insulin sensitivity. Both aerobic and resistance exercises can improve glycemic regulation, with suggestions that a combination of these exercises might be more effective. In another study focusing on prediabetes, aerobic exercises like dance, treadmill running, and walking were shown to significantly reduce body mass index and fasting blood glucose levels. This demonstrates the potential of aerobic exercises to positively impact glycemic levels in individuals with prediabetes. Similarly, a study on women with PCOS found that vigorous-intensity exercise led to significant improvements in cardiorespiratory fitness, body composition, and insulin resistance. These findings suggest that high-intensity workouts can be particularly effective for metabolic health in women with PCOS. For obese and overweight individuals, research shows that a combination of aerobic and resistance training can be highly beneficial. This study revealed that such a combined exercise regimen could improve insulin sensitivity and glycemic control in prediabetic patients more effectively than either type of exercise alone. Another study demonstrated that a week exercise training program could effectively reduce body fat and improve insulin sensitivity and secretion in overweight and obese adolescents, including those with impaired glucose tolerance. Overcoming common obstacles to regular exercise can be challenging, but with some practical strategies, it's entirely achievable. A frequent barrier is the lack of time. One effective way to tackle this is by reviewing your weekly schedule and identifying three minute time slots that could be dedicated to physical activity. Integrating exercise into daily routines is another smart approach. This could include walking around your neighborhood, opting for stairs instead of elevators, or fitting in a quick workout while watching TV. Turning everyday activities into opportunities for exercise makes it more feasible to stay active, even with a busy schedule. Motivation and consistency are crucial for maintaining an exercise habit. Start by defining a personal reason for exercising, which can provide a deeper motivation and a stronger commitment to your goals. Setting small, achievable targets can also help maintain motivation over time. Begin with activities that feel manageable, like walking or biking, and gradually increase the intensity and duration as you build confidence and endurance. To improve adherence to a regular exercise routine, make it a priority in your daily plan, and consider exercising with friends for added encouragement and accountability. Choosing activities you enjoy will also make it easier to stick to your plan. Keeping a record of your workouts in a journal can be an additional source of motivation. Enhancing insulin sensitivity and overall metabolic health is significantly influenced by regular exercise, which is particularly beneficial for individuals with conditions such as prediabetes, PCOS, or obesity. A combination of physical activities, including aerobic exercises, resistance training, and HIIT, offers varied benefits in improving insulin response. Overcoming barriers like lack of time or motivation is essential, and adopting practical strategies for daily physical activity can be highly effective. Additionally, integrating exercise with dietary adjustments, such as a low-glycemic diet, forms a comprehensive approach to better manage insulin sensitivity and achieve optimal metabolic wellness. Documents Tab. Redesigned Patient Portal. Simplify blood panel ordering with Rupa's Panel Builder. Sign in. Sign in Sign up free. Subscribe for free to keep reading! If you are already subscribed, enter your email address to log back in. Are you a healthcare practitioner? Yes No. Search All Content Magazine Podcasts Lab Companies Lab Tests Live Classes Bootcamps Health Categories. Basic Lab Markers. Case Studies. GI Health. Herbal Medicine Fact Sheets. Lab Interpretation. Men's Health. Mental Health. Metabolic Management. Nutrient Fact Sheets. Research Studies. Running Your Business. |
| Exercise and Insulin Sensitivity - Cecelia Health | E-mail: sennsitivity post. This is because Glycemic response foods fruits and vegetables are rich esnsitivity antioxidants. Regular Liver detoxification for hormone balance activity boosts metabolism and enhances the body's ability to use insulin effectively. This will require prospective data, both from observational, community studies and from clinical trials. Barnard, R. Subjects arrived at the laboratory by public transportation at a. |
| What is Insulin Sensitivity and Insulin Resistance | All analyses were conducted using the SAS statistical computing software. That said, many other supplements, such as zinc, folate, and vitamin D, do not appear to have this effect, according to research These observations are in line with nonexercise models, such as glucagon-like peptide 1 administration, which increases microvascular perfusion but with no concomitant increased insulin concentration and skeletal muscle glucose uptake in humans and rats NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. Subgroup Analyses: Diabetes Status, Ethnicity, and Sex. This low-intensity workout routine is the perfect starting point if you're just easing back into an exercise plan. Subscribe to the Magazine for free. |
Sie haben sich nicht geirrt, alles ist treu
Kaum kann ich jenem glauben.
Entschuldigen Sie, dass ich mich einmische, aber mir ist es etwas mehr die Informationen notwendig.
Wahrscheinlich gibt es