
This diabetuc a frightening fact. Losing your sight could affect your career, your family life and your independence. This can help pick up any problems early. Diabetic retinopathy DKA and diabetic retinopathy an eye disease Organic mineral supplements people Refreshing energy drinks with diabetes are more at diabetc of developing.
If your blood glucose sugar levels and blood pressure are consistently high, Organic mineral supplements, you can seriously damage xiabetic blood vessels.
There are lots of important blood vessels in your eyes, dizbetic help supply blood Mediterranean diet and digestion the seeing part of the eye called the Sugar alternatives for candy. When these Nutrition periodization for martial arts vessels are retinoparhy, they can get blocked, leak or grow randomly.
There are lots riabetic things you Retinoapthy do to keep your blood sugars and your blood pressure in your target range. Retinopahty more refinopathy do this, the retinoppathy your risk of developing andd problems with your eyes.
Diabetic retinopathy usually develops in retinoparhy. When you get your eye screening results, you should dkabetic a letter and retinnopathy number which tells you the DKAA of diabetix you may have. These letters and number DKA and diabetic retinopathy be different depending on where Organic mineral supplements live in the UK, so viabetic to your healthcare team if you're not sure.
Here are the ad types:. This is sometimes called background retinopathy. You diabegic hear this called R1 when you get Organic mineral supplements diabetci screening results. You Organic mineral supplements Glucose tolerance this called R2.
You might Cholesterol level exercise this called R3. Diabetic maculopathy, also known as Diabetic Macular Reinopathy DMOis a Satiety promoting habits type of retinopathy that ane the Gymnastics diet plan of the eye.
the blood vessels in the part of the eye called the macula the diabeitc part of DKA and diabetic retinopathy retina at the back of your retinoptahy which is responsible for dibetic fine details retinkpathy Mediterranean diet and digestion vision can become blocked.
Diabeetic diabetic maculopathy is detected there is retinpathy high risk Organic mineral supplements vision could be affected, and you may be advised to have more tests. You might hear this called M0 if there's no maculopathy found in your eyes, or M1 if fluid is starting to build-up in your eye and is affecting your sight.
Background and non-proliferative retinopathy are known as early stage retinopathy and there are lots of things you can do yourself to prevent it from getting worse. Proliferative retinopathy and maculopathy are more advanced. We have more information about how to treat advanced eye problemsand your healthcare team will also go through your treatment options with you.
Eye screening is a way of spotting eye problems before you notice any changes to your sight. At first, the screening should be every year, then this can change depending on your results. Diabetic retinopathy can become quite advanced before it starts affecting your sight, so that's why it's important to go to your regular eye screening appointments.
That way, you can get the right treatment in time. Read our latest update for more information on eye screening and other routine appointments.
Your eyesight can also go a bit blurry if your blood sugar goes higher than usual, even for a short time. This is normal and is a symptom of high blood sugars.
Consistently high blood sugar levels make you more at risk of diabetes complications, including serious eye problems.
Knowing what your target levels are and regularly checking your blood sugars can help you keep on top of them. This means checking your blood sugar levels at home and getting a doctor to check your HbA1c levels regularly too.
Your healthcare team should help you set your targets. The closer you get, the lower your risk of developing eye problems.
Or you can call our helpline for more information and support. High blood pressure and a lot of fat in your blood called cholesterol will increase your chances of getting eye problems. We have advice and information to help you manage your blood pressure and cholesterol.
Your healthcare team will also be able to support you with this. But why does being healthy make a difference? And can foods prevent diabetic retinopathy? No specific foods can prevent retinopathy.
Start small and build up — we have lots of information and support to help you make these positive lifestyle changes. Being healthy will make a real difference to preventing eye damage in the future.
Having diabetes can mean you are two times more likely to get cataracts and one and a half times more likely to get glaucoma. Cataracts and glaucoma are other eye problems that people with diabetes are at a higher risk of developing.
A cataract is when your vision gets cloudy and glaucoma is when fluid builds up in the eye. As with retinopathy, this can all be down to high blood sugar levels, so checking them and having regular eye screenings is crucial. If your eye problems become too advanced, you may need surgery.
Give our confidential helpline a call and speak to one of our highly trained advisors. If you do start to develop eye problems, your healthcare team can support you and talk to you about your treatment options.
A company limited by guarantee registered in England and Wales with no. Skip to main navigation Skip to content. Breadcrumb Home Guide to diabetes Complications Retinopathy. Save for later Page saved! You can go back to this later in your Diabetes and Me Close.
Diabetic retinopathy — diabetes and eye problems. Diabetic retinopathy Diabetes can affect your eyes in many ways. Some people go on to develop an eye complication called diabetic retinopathy.
Diabetes is the leading cause of preventable sight loss in the UK. What is diabetic retinopathy and what causes it? Share this Page.
: DKA and diabetic retinopathy| Diabetic retinopathy | Laser photocoagulation uses DA heat from a laser Mediterranean diet and digestion seal or destroy abnormal, leaking blood vessels in diabefic retina. Retinopaghy you have diabetic retinopathy, high blood pressure can make it worse. This is called non-proliferative retinopathy. If you have diabetic retinopathy, low-vision aids such as magnifying glasses and special lenses can help. Create an Account or Subscribe Now. |
| Diabetic ketoacidosis | healthdirect | This causes the retina to thicken, creating blurred vision. The swelling associated with diabetes in the macula, the central part of the eye responsible for staring straight ahead, called diabetic macular edema. In another process, blood vessels damaged by hyperglycemia high blood sugar, or high blood glucose close, and a series of events begin. Starving retinal tissue produces growth causing new blood vessels to form on the surface of the retina. These new blood vessels are weak and can easily break and bleed. This leads to scar tissue, which can build up on the back wall of the eye and stretch the retina, eventually separating it from the back of the eye. This condition is known as retinal detachment, and it can happen suddenly or slowly over time. Managing your diabetes—by staying physically active, eating healthy and taking your medicine—can also help you prevent or delay vision loss. Your ophthalmologist eye doctor will first check for any changes to your glasses or contact lens prescription. People with many diabetes related problems with their vision can still wear contact lenses. The doctor will then dilate your pupils and examine the retina. The drops used may sting for a short time. About 20 to 30 minutes later, your eyes will be fully dilated. With the use of special lenses and lights, the doctor will visually examine your retina. To detect retinopathy, the doctor looks at all the retinal tissues. For signs of macular edema, the doctor looks at the macula in the back of your eye, but this may not be enough for a diagnosis. Your doctor may perform an optical coherence tomography, which is a laser exam of the back of the eye. While the retina is very thin, the test can measure retinal thickening as small as a thousandth of a millimeter. A fluorescein angiogram is a test that can detect diabetic retinopathy. During the test, a dye is injected into your arm. Within 45 seconds, the dye reaches the back of the eye. Just like how blood leaks from weak blood vessels, so does the dye. Special photographs help document the results. If you have diabetes and visit your doctor for blurred vision, you can expect to have some or all of these tests. Your doctor will also check for cataracts clouding of the lenses in the eye and glaucoma high pressure in the eye , which are more common in people with diabetes. Glaucoma can develop when abnormal blood vessels grow in the iris, the colored part of the eye, due to proliferative retinopathy. If your diabetic retinopathy is moderate and stable, treatment may not be necessary right away. Four 4. Four of the 86 included children 4. Two of these patients also had maculopathy background retinopathy involving the macula. The mean age of the children with diabetic retinopathy was The youngest child with retinopathy was 13 year old with diabetic duration of 10 years. No patient was found to have diabetic eye disease beyond background retinopathy in this study. All of them were female. The patients with maculopathy had reduced visual acuity but we did not know whether or not the maculopathy is responsible for their impaired vision. They were referred to an ophthalmologist for evaluation like the other patients with reduced visual acuity. There was only one case with symptoms suggestive of peripheral neuropathy Case 4; Table 2. All patients were taking a mixture of regular and Neutral Protamine Hagedorn NPH insulin subcutaneously one third of the total daily dose being regular insulin and two third NPH. Two third of the total dose was given in the morning and one third in the evening. Detailed description of the cases is presented in Table 2. The current study found that 90 All the screened patients were adolescents. The majority of the included children had a diabetic duration of 6—10 years. As observed in this study our diabetic children did not have regular HbA 1c measurements making evaluation of long term metabolic control difficult. Among the study subjects, only 55 Although we did not know their overall glycemic control throughout their diabetic duration, the few HbA 1c values and the 1 month average fasting blood glucose measurements reflected the clearly apparent poor glycemic control in more than half of the study subjects for at least a few months. Despite the recommendations of ISPAD, little is known about the true impact of complications of diabetes, including diabetic retinopathy in the Ethiopian pediatric population. Screening for all of the microvarscular complications of diabetes was not routinely done indicating a suboptimal proactive follow up of these children. To our best knowledge this effort constitutes the first attempt to estimate the prevalence of diabetic retinopathy among pediatric diabetics in the country although the study subjects are not representative of the overall diabetic children in the country as they came from only the capital city and its surrounding areas. The prevalence of pediatric diabetic retinopathy in pediatric diabetic patients having follow-up in Tikur Anbesa Specialized Hospital was found to be 4. Two patients also had associated maculopathy that could threaten their vision even though the stage of their retinopathy is background retinopathy. The reduced visual acuity in these two patients could be due to the maculopathy although further evaluation is needed to know the exact cause of their low visual acuity as it can also be affected by other factors like refractive error. The four patients with retinopathy and all those study subjects with reduced visual acuity were referred to an ophthalmologist for further evaluation, intervention and follow up. Although we found out that all patients with retinopathy had high HbA 1c measurements, we could not conclude that these patients had long standing poor glycemic control as one or two HbA1c values will be insufficient to describe the long term metabolic control. It is well known that the development of retinopathy takes years and an HbA 1c measurement reflects the average blood glucose concentration from the preceding 2—3 months. Similarly, although it is well known from many other studies that prolonged poor glycemic control is associated with increased risk of development of retinopathy, we could not show this in our study due to the small number of our study subjects. The finding that no patient was found to have proliferative retinopathy in our study is comparable to the findings elsewhere [ 22 ]. The prevalence of pediatric diabetic retinopathy in the current study is lower than that reported in other populations such as the study in Tanzania However, it is higher than those seen in other studies: France 4. The substantial heterogeneity in reported prevalence of retinopathy may partly be real, for example due to genetic differences of different populations, but may also be due to differences in study methodology and population sample. The finding that there is poor glycemic control in the majority of our study subjects is similar to the findings in other African settings [ 15 , 23 ]. The current study revealed that few patients had previous retinopathy screening despite the availability of the service through the Ethiopian Diabetic Association. The possible reasons for this, while they should be studied systematically, could be shortage of resources, low awareness of the practicing professionals in the center or failure to follow guidelines for follow up of such patients. This practice should be improved to detect the occurrence of diabetic retinopathy before patients develop vision threatening complication. Among the four patients with retinopathy, two had had retinopathy screening 1 year before the current evaluation that showed background retinopathy, and there was no progression of the stage of retinopathy after 1 year. One of the major limitations of the current study is the inability to evaluate the long term glycemic control of the study subjects. Factors associated with the risk of developing diabetic retinopathy could not also be studied because of the small number of study subjects. Even though the center where the study was conducted is the largest national referral center for such cases, and many children from around the country come for follow up, the study still cannot be considered as representative of the pediatric diabetic population in the country. We also could not provide definition to the other complications of diabetes since we used chart review to obtain the data. In conclusion, diabetic retinopathy, though uncommon, is a possible early complication in diabetic children in this setting. Hence, systematic screening should be in place for all micro vascular complications of diabetes. The results clearly show that major efforts are needed to improve quality of care in children with type 1 diabetes in Ethiopia. We recommend that children with diabetes should be followed for development of any complications using standard guidelines like ISPAD The patients with retinopathy should also be followed prospectively to evaluate the progression of their retinopathy. We also recommend more studies to assess the magnitude and the determinants of developing diabetic retinopathy, and the state of glycemic control and its determinants in the country using a large number of representative study subjects. Fong DS, Aiello LP, Ferris FL. Diabetic retinopathy. Diabetes Care. Article PubMed Google Scholar. Lueder GT. Screening for retinopathy in pediatric patient with type 1 diabetes mellitus. Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. Article CAS PubMed Google Scholar. Sultan MB, Starita C, Huang K. Epidemiology, risk factors and management of pediatrics diabetic retinopathy. Br J Ophthalmol. pdf Accessed on 9 Apr Dorchy H, Claes C, Verougstraete C. Risk factors of developing proliferative retinopathy in type 1 diabetic patients: role of BMI. Holl RW, Lang GE, Grabert M, Heinze E, Lang GK, Debatin KM. Diabetic retinopathy in pediatric patients with type-1 diabetes: effect of diabetes duration, prepubertal and pubertal onset of diabetes, and metabolic control. J Pediatr. Donaghue KC, Fairchild JM, Chan A, et al. Diabetes micro vascular complications in prepubertal children. J Pediatr Endocrinol Metab. CAS PubMed Google Scholar. Verougstraete C, Toussaint D, De Schepper J, Haentjens M, Dorchy H. First microangiographic abnormalities in childhood diabetes—types of lesions. Graefes Arch Clin Exp Ophthalmol. Malone JI, Grizzard S, Espinoza LR, Achenbach KE, Van Cader TC. Risk factors for diabetic retinopathy in youth. Kristinsson JK, Gudmundsson JR, Stefansson E, Jonasson F, Gislason I, Thorsson AV. Screening for diabetic retinopathy: initiation and frequency. Acta Ophthalmol Scand. Gallego PH, Wiltshire E, Donaghue KC. Identifying children at particular risk of long-term diabetes complications. Pediatr Diabetes. Massin P, Erginay A, Mercat-Caudal I, et al. Prevalence of diabetic retinopathy in children and adolescents with type1 diabetes attending summer camps in France. Diabetes Metab. Majaliwa ES, Munubhi E, Ramaiya K, et al. Survey on acute and chronic complications in children and adolescents with type 1 diabetes at Muhimbili National Hospital in Dar es Salaam. Donaghue KC, Craig ME, Chan AK, et al. Prevalence of diabetes complications 6 years after diagnosis in an incident cohort of childhood diabetes. Diabet Med. American Academy of Ophthalmology Retina Panel. Preferred Practice Pattern: Diabetic Retinopathy. San Francisco: American Academy of Ophthalmology; Google Scholar. Aiello LP, Gardner TW, King GL, Blankenship G, Cavallerano JD, Ferris FL, Klein R. American Diabetes Association. American Academy of Pediatrics. Section on Endocrinology and Section on Ophthalmology. Screening for retinopathy in the pediatric patient with type 1 diabetes mellitus. Article Google Scholar. Skelton JA, Rudolph CD. Overweight and Obesity. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson text book of pediatrics. Philadelphia: Saunders Elsevier; Alemzadeh R, Wyatt DT. Diabetes Mellitus in Children. Nelson Text Book of Pediatrics. Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XVII. The year incidence and progression of diabetic Retinopathy and associated risk factors in type 1 diabetes. Elamin A, Hussein O, Tuvemo T. Growth, puberty and final height in children with type 1 diabetes. J Diabetes Complications. Download references. MS conceived the initial idea, developed proposal, coordinated data collection and did the statistical analysis and write up. BF and TK advised during proposal development, data collection and analysis. BT was involved in the analysis, manuscript write up and preparation for publication. All authors read and approved the final manuscript. The authors would like to acknowledge Addis Ababa University, School of Medicine for financially supporting the research. Department of Pediatrics and Child Health, Hawassa University, Awassa, Ethiopia. Department of Pediatrics and Child Health, St. Paul Medical College, Addis Ababa, Ethiopia. Department of Internal Medicine, Addis Ababa University, Addis Ababa, Ethiopia. |
| Risk Factors for Diabetic Retinopathy | Still, we should closely follow any patient who shows a moderate degree of this stage of retinopathy. Having diabetes can lead to heart problems, strokes, and problems with blood vessels in the body. Control your blood pressure. They may be used to detect clouding of the lens cataract , changes in the retina, and other problems. Regular eye exams can help catch DR in the early, nonproliferative stages. These scaffoldings appear as yellowish-white strands or sheets above the retina, and provide the structural support that neovascular vessels inherently lack. You may not notice symptoms in the early stage. |
DKA and diabetic retinopathy -
Our report gives mechanistic insight for this interesting condition. Clinicians should be aware of reversible blindness as a complication of DKA. Timely correction of the severe acidosis and other metabolic disturbances of DKA may be instrumental in preventing permanent vision loss.
Keywords: Bicarbonate infusion; Diabetes mellitus; Diabetic ketoacidosis; Reversible blindness; Serum pH. Abstract The presenting symptoms of diabetic ketoacidosis DKA include abdominal pain, polyuria and nausea. Publication types Case Reports. Several RCTs are currently evaluating 3 agents that suppress vascular endothelial growth factor VEGF for treatment of DME.
Pegaptanib Macugen; Pfizer, New York, New York targets the isoform of VEGF for treatment of neovascular age-related macular degeneration AMD. Ranibizumab Lucentis; Genentech, South San Francisco, California is another anti-VEGF agent used for treatment of neovascular AMD , and may also be useful for DR and DME.
Finally, bevacizumab Avastin, Genentech is an anti-VEGF agent similar to ranibizumab that is approved for the treatment of disseminated colorectal cancer and not licensed for intraocular use. However, bevacizumab appears to show similar efficacy for treatment of neovascular AMD and may also be effective for DME and proliferative DR.
There is strong evidence that tight glycemic control reduces the incidence and progression of DR Table 6. There also is strong evidence that tight blood pressure control in patients with hypertension and diabetes is beneficial in reducing visual loss from DR.
The benefit of blood pressure treatment in normotensive patients with diabetes is less clear. There remains inconclusive evidence about the benefits of lipid-lowering therapy for DR prevention.
There also is little evidence that aspirin, other antiplatelet agents, or aldose reductase inhibitors confer any benefit in reducing progression of DR. The role of PKC and growth hormone inhibitors is currently unclear, and results from ongoing trials are pending.
Proliferative DR. The benefits are most marked in those with high-risk proliferative DR, in whom PRP should be commenced without delay.
The benefits of vitrectomy are less clear for those with type 2 diabetes. With advances in vitreoretinal surgery, vitrectomy may be indicated earlier in eyes with nonclearing hemorrhage. Nonproliferative DR. Although there is level I evidence that early PRP reduces the risk of severe visual loss in nonproliferative DR, the absolute risk reduction from early PRP treatment is small, and the risks of deferred treatment are low.
In mild to moderate nonproliferative DR, systemic factors such as control of glycemia and blood pressure should be gradually optimized and PRP deferred with careful follow-up. The ETDRS and other RCTs 95 suggest that PRP should be considered in more severe nonproliferative DR, especially in patients with type 2 diabetes.
This benefit for PRP should be balanced against the small risk of vision loss. Early PRP is recommended in these patients if regular follow-up examination is not feasible, if there is significant media opacity or cataract that may affect the ability to apply future laser treatment, or if there are concomitant risk factors eg, pregnancy for rapid progression.
Diabetic Macular Edema. In patients with coexistent proliferative DR and DME, focal laser treatment concurrent with or prior to PRP is recommended. There is moderate evidence that IVTA may be useful in eyes with persistent DME and loss of vision despite conventional treatment, including focal laser treatment and attention to systemic risk factors.
Patients should be warned of adverse effects and the need for reinjection. Further studies are warranted to determine the ideal dose and longer-term efficacy and safety. Intravitreal anti-VEGF agents are being evaluated in several clinical trials; until results are available, there is currently insufficient evidence recommending their routine use.
There is weak evidence that vitrectomy may be beneficial in some patients with DME, particularly in eyes with associated vitreomacular traction, but well-conducted studies with longer follow-up are needed. Quiz Ref ID Although DR remains the leading cause of preventable blindness in working adults, there are primary and secondary interventions proven effective in limiting visual loss.
The indications, efficacy, and safety of newer medical and surgical treatments, however, require further evaluation. Corresponding Author: Tien Y. Wong, MD, PhD, Centre for Eye Research Australia, University of Melbourne, 32 Gisborne St E, Melbourne Victoria, Australia twong unimelb.
Author Contributions: Dr Wong had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Critical revision of the manuscript for important intellectual content : Gillies, Wong. Financial Disclosures: Dr Gillies reported that he is included as an inventor on patents relating to the formulation of triamcinolone for ocular use and its use for the treatment of retinal neovascularization but not diabetic macular edema.
Dr Gillies and Dr Wong reported serving on advisory boards for and as investigators in clinical trials in diabetic retinopathy sponsored by Pfizer, Novartis, and Allergan and receiving grants, honoraria, and traveling fees from these companies.
No other disclosures were reported. Role of the Sponsor: The National Health and Medical Research Council of Australia had no role in the design and conduct of the study; the collection, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
full text icon Full Text. Download PDF Top of Article Abstract Box. Nonproliferative and Proliferative Diabetic Retinopathy View Large Download. Table 1. Randomized Controlled Trials Evaluating Role of Glycemic Control in Diabetic Retinopathy View Large Download.
Table 2. Randomized Controlled Trials Evaluating Role of Blood Pressure Control in Diabetic Retinopathy View Large Download. Table 3. Randomized Controlled Trials of Medical Interventions in Diabetic Retinopathy View Large Download. Table 4. Randomized Controlled Trials of Laser Treatment in Nonproliferative and Proliferative Diabetic Retinopathy and Diabetic Macular Edema View Large Download.
Table 5. Randomized Controlled Trials of Surgical Interventions in Proliferative Diabetic Retinopathy and Diabetic Macular Edema View Large Download. Table 6.
Summary of Clinical Recommendations for Primary and Secondary Interventions for Diabetic Retinopathy View Large Download. International Diabetes Federation. Diabetes atlas Accessed May US Centers for Disease Control and Prevention.
National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, Atlanta, GA: Centers for Disease Control and Prevention; Klein R, Klein BE, Moss SE, Cruickshanks KJ.
The Wisconsin Epidemiologic Study of Diabetic Retinopathy, XVII: the year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Wong TY, Klein R, Islam FM. et al.
Diabetic retinopathy in a multi-ethnic cohort in the United States. Am J Ophthalmol. Olsen BS, Sjølie A, Hougaard P. Danish Study Group of Diabetes in Childhood. A 6-year nationwide cohort study of glycaemic control in young people with type 1 diabetes: risk markers for the development of retinopathy, nephropathy and neuropathy.
J Diabetes Complications. van Leiden HA, Dekker JM, Moll AC. Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study.
Arch Ophthalmol. Incidence of retinopathy and associated risk factors from time of diagnosis of insulin-dependent diabetes. Blood pressure, lipids, and obesity are associated with retinopathy: the hoorn study. Diabetes Care. Klein R, Moss SE, Klein BE, Davis MD, DeMets DL.
The Wisconsin epidemiologic study of diabetic retinopathy, XI: the incidence of macular edema. Klein BE, Klein R, Moss SE, Palta M. A cohort study of the relationship of diabetic retinopathy to blood pressure.
Klein R, Sharrett AR, Klein BE. ARIC Group. The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes: the atherosclerosis risk in communities study. Klein R, Klein BE, Moss SE, Linton KL. The Beaver Dam Eye Study: retinopathy in adults with newly discovered and previously diagnosed diabetes mellitus.
Chew EY, Klein ML, Ferris FL. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy: Early Treatment Diabetic Retinopathy Study ETDRS Report Klein BE, Moss SE, Klein R. Effect of pregnancy on progression of diabetic retinopathy.
Cruickshanks KJ, Ritter LL, Klein R, Moss SE. The association of microalbuminuria with diabetic retinopathy: the Wisconsin Epidemiologic Study of Diabetic Retinopathy.
Klein R, Moss SE, Klein BE. Is gross proteinuria a risk factor for the incidence of proliferative diabetic retinopathy? Stratton IM, Kohner EM, Aldington SJ.
UKPDS risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Moss SE, Klein R, Klein BE. Association of cigarette smoking with diabetic retinopathy. McKay R, McCarty CA, Taylor HR. Diabetic retinopathy in Victoria, Australia: the Visual Impairment Project.
Br J Ophthalmol. Kriska AM, LaPorte RE, Patrick SL, Kuller LH, Orchard TJ. The association of physical activity and diabetic complications in individuals with insulin-dependent diabetes mellitus: the Epidemiology of Diabetes Complications Study—VII.
J Clin Epidemiol. Verhagen AP, de Vet HC, de Bie RA. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus.
Minckler D. Evidence-based ophthalmology series and content based continuing medical education for the journal. Early Treatment Diabetic Retinopathy Study Research Group. Classification of diabetic retinopathy from fluorescein angiograms: ETDRS report number Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification: ETDRS report number Aldington SJ, Kohner EM, Meuer S, Klein R, Sjølie AK.
Methodology for retinal photography and assessment of diabetic retinopathy: the EURODIAB IDDM complications study. Diabetes Control and Complications Trial Research Group. Progression of retinopathy with intensive versus conventional treatment in the Diabetes Control and Complications Trial.
Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS The relationship of glycemic exposure HbA1c to the risk of development and progression of retinopathy in the diabetes control and complications trial.
Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. UK Prospective Diabetes Study UKPDS Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Kohner EM, Stratton IM, Aldington SJ, Holman RR, Matthews DR.
UK Prospective Diabetes Study IKPDS Group. Relationship between the severity of retinopathy and progression to photocoagulation in patients with type 2 diabetes mellitus in the UKPDS UKPDS Diabet Med.
Shichiri M, Kishikawa H, Ohkubo Y, Wake N. Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients. Wang PH, Lau J, Chalmers TC.
Meta-analysis of effects of intensive blood-glucose control on late complications of type I diabetes. Metaanalysis of the effects of intensive glycemic control on late complications of type I diabetes mellitus.
Online J Curr Clin Trials. May 21, ;. Doc No. Lauritzen T, Frost-Larsen K, Larsen HW, Deckert T. Two-year experience with continuous subcutaneous insulin infusion in relation to retinopathy and neuropathy.
Kroc Collaborative Study Group. Blood glucose control and the evolution of diabetic retinopathy and albuminuria: a preliminary multicenter trial. Diabetic retinopathy after two years of intensified insulin treatment: follow-up of the Kroc Collaborative Study. Beck-Nielsen H, Olesen T, Mogensen CE.
Effect of near normoglycemia for 5 years on progression of early diabetic retinopathy and renal involvement. Diabetes Res. Olsen T, Richelsen B, Ehlers N, Beck-Nielsen H.
Diabetic retinopathy after 3 years' treatment with continuous subcutaneous insulin infusion CSII. Acta Ophthalmol Copenh. Reichard P, Berglund B, Britz A, Cars I, Nilsson BY, Rosenqvist U. Intensified conventional insulin treatment retards the microvascular complications of insulin-dependent diabetes mellitus IDDM : the Stockholm Diabetes Intervention Study SDIS after 5 years.
J Intern Med. Dahl-Jørgensen K, Brinchmann-Hansen O, Hanssen KF. Effect of near normoglycaemia for two years on progression of early diabetic retinopathy, nephropathy, and neuropathy: the Oslo study.
Br Med J Clin Res Ed. Dahl-Jørgensen K, Brinchmann-Hansen O, Hanssen KF, Sandvik L, Aagenaes O. Rapid tightening of blood glucose control leads to transient deterioration of retinopathy in insulin dependent diabetes mellitus: the Oslo study.
Brinchmann-Hansen O, Dahl-Jørgensen K, Sandvik L, Hanssen KF. Blood glucose concentrations and progression of diabetic retinopathy: the seven year results of the Oslo study. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus.
Ohkubo Y, Kishikawa H, Araki E. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study.
Diabetes Res Clin Pract. Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus.
Reichard P, Pihl M, Rosenqvist U, Sule J. Complications in IDDM are caused by elevated blood glucose level: the Stockholm Diabetes Intervention Study SDIS at year follow up.
Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Egger M, Davey Smith G, Stettler C, Diem P. Risk of adverse effects of intensified treatment in insulin-dependent diabetes mellitus: a meta-analysis.
Wong TY, Mitchell P. The eye in hypertension. Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. Is blood pressure a predictor of the incidence or progression of diabetic retinopathy? Arch Intern Med.
Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus: UKPDS Estacio RO, Jeffers BW, Gifford N, Schrier RW.
Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes.
Kidney Int. Chaturvedi N, Sjolie AK, Stephenson JM. EUCLID Study Group. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes.
Schrier RW, Estacio RO, Jeffers B. Appropriate Blood Pressure Control in NIDDM ABCD trial. Larsen M, Hommel E, Parving HH, Lund-Andersen H.
Protective effect of captopril on the blood-retina barrier in normotensive insulin-dependent diabetic patients with nephropathy and background retinopathy.
Graefes Arch Clin Exp Ophthalmol. Knudsen ST, Bek T, Poulsen PL, Hove MN, Rehling M, Mogensen CE. Effects of losartan on diabetic maculopathy in type 2 diabetic patients: a randomized, double-masked study. ADVANCE Collaborative Group. ADVANCE—Action in Diabetes and Vascular Disease: patient recruitment and characteristics of the study population at baseline.
Sjølie AK, Porta M, Parving HH, Bilous R, Klein R. DIRECT Programme Study Group. The DIabetic REtinopathy Candesartan Trials DIRECT Programme: baseline characteristics. J Renin Angiotensin Aldosterone Syst.
Sen K, Misra A, Kumar A, Pandey RM. Simvastatin retards progression of retinopathy in diabetic patients with hypercholesterolemia.
Cullen JF, Town SM, Campbell CJ. Double-blind trial of Atromid-S in exudative diabetic retinopathy. Trans Ophthalmol Soc U K. Keech A, Simes RJ, Barter P. FIELD Study Investigators. Effects of long-term fenofibrate therapy on cardiovascular events in people with type 2 diabetes mellitus the FIELD study : randomised controlled trial.
Effects of aspirin treatment on diabetic retinopathy: ETDRS report number 8. Chew EY, Klein ML, Murphy RP, Remaley NA, Ferris FL. DAMAD Study Group. Effect of aspirin alone and aspirin plus dipyridamole in early diabetic retinopathy: a multicenter randomized controlled clinical trial.
TIMAD Study Group. Ticlopidine treatment reduces the progression of nonproliferative diabetic retinopathy. PKC-DRS Study Group. The effect of ruboxistaurin on visual loss in patients with moderately severe to very severe nonproliferative diabetic retinopathy: initial results of the Protein Kinase C beta inhibitor Diabetic Retinopathy Study PKC-DRS multicenter randomized clinical trial.
Aiello LP, Davis MD, Girach A. PKC-DRS2 Group. Effect of ruboxistaurin on visual loss in patients with diabetic retinopathy.
PKC-DMES Study Group. Effect of ruboxistaurin in patients with diabetic macular edema: thirty-six month results of the randomized PKC-DMES clinical trial. Sorbinil Retinopathy Trial Research Group. A randomized trial of sorbinil, an aldose reductase inhibitor, in diabetic retinopathy.
Gardner TW, Sander B, Larsen ML. An extension of the Early Treatment Diabetic Retinopathy Study ETDRS system for grading of diabetic macular edema in the Astemizole Retinopathy Trial.
Curr Eye Res. Grant MB, Mames RN, Fitzgerald C. The efficacy of octreotide in the therapy of severe nonproliferative and early proliferative diabetic retinopathy: a randomized controlled study. Thomason MJ, Colhoun HM, Livingstone SJ.
CARDS Investigators. Baseline characteristics in the Collaborative AtoRvastatin Diabetes Study CARDS in patients with type 2 diabetes.
Colhoun HM, Betteridge DJ, Durrington PN. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study CARDS : multicentre randomised placebo-controlled trial.
Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus ASPEN.
Aiello LP, Davis MD, Milton RC, Sheetz MJ, Arora V, Vignati L IV. Accessed April 4, Ray BS, Pazianos AG, Greenberg E, Peretz WL, McLean JM.
Pituitary ablation for diabetic retinopathy, I: results of hypophysectomy: a ten-year evaluation. Hardy J, Ciric IS. Selective anterior hypophysectomy in the treatment of diabetic retinopathy: a transsphenoidal microsurgical technique.
Sönksen PH, Russell-Jones D, Jones RH. Growth hormone and diabetes mellitus: a review of sixty-three years of medical research and a glimpse into the future? Horm Res. Kirkegaard C, Nørgaard K, Snorgaard O, Bek T, Larsen M, Lund-Andersen H. Effect of one year continuous subcutaneous infusion of a somatostatin analogue, octreotide, on early retinopathy, metabolic control and thyroid function in type I insulin-dependent diabetes mellitus.
Acta Endocrinol Copenh. Extension Study of the Long-Term Safety and Tolerability of Octreotide Acetate in Patients With Moderately Severe or Severe Non-Proliferative Diabetic Retinopathy or Low Risk Diabetic Retinopathy [NCT].
Accessibility verified July 19, Grant MB. Diabetic retinopathy—diagnostic and treatment novelties. Presented at: American Diabetes Association 66th Scientific Sessions; June , ; Washington, DC. Photocoagulation treatment of proliferative diabetic retinopathy: the second report of diabetic retinopathy study findings.
Rohan TE, Frost CD, Wald NJ. Prevention of blindness by screening for diabetic retinopathy: a quantitative assessment. Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of Diabetic Retinopathy Study DRS findings: DRS Report Number 8.
Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Flynn HW, Chew EY, Simons BD, Barton FB, Remaley NA, Ferris FL. Pars plana vitrectomy in the Early Treatment Diabetic Retinopathy Study: ETDRS report number Photocoagulation for proliferative diabetic retinopathy: a randomised controlled clinical trial using the xenon-arc.
British Multicentre Study Group. Photocoagulation for diabetic maculopathy: a randomized controlled clinical trial using the xenon arc.
Hercules BL, Gayed II, Lucas SB, Jeacock J. Peripheral retinal ablation in the treatment of proliferative diabetic retinopathy: a three-year interim report of a randomised, controlled study using the argon laser.
Patz A, Schatz H, Berkow JW, Gittelsohn AM, Ticho U. Macular edema—an overlooked complication of diabetic retinopathy. Trans Am Acad Ophthalmol Otolaryngol.
Lövestam-Adrian M, Agardh CD, Torffvit O, Agardh E. Type 1 diabetes patients with severe non-proliferative retinopathy may benefit from panretinal photocoagulation.
Acta Ophthalmol Scand. Photocoagulation for diabetic macular edema: Early Treatment Diabetic Retinopathy Study report number 1. Fong DS, Strauber SF, Aiello LP.
Writing Committee for the Diabetic Retinopathy Clinical Research Network. Comparison of the modified early treatment diabetic retinopathy study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Blankenship GW.
Diabetic macular edema and argon laser photocoagulation: a prospective randomized study. Olk RJ. Modified grid argon blue-green laser photocoagulation for diffuse diabetic macular edema. Photocoagulation in treatment of diabetic maculopathy: interim report of a multicentre controlled study.
Ladas ID, Theodossiadis GP. Long-term effectiveness of modified grid laser photocoagulation for diffuse diabetic macular edema. Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics: ETDRS report number 7.
Pahor D. Visual field loss after argon laser panretinal photocoagulation in diabetic retinopathy: full- versus mild-scatter coagulation. Int Ophthalmol. Buckley SA, Jenkins L, Benjamin L. Fields, DVLC and panretinal photocoagulation.
Aiello LM. Perspectives on diabetic retinopathy.
This Muscular strength training tips a DKA and diabetic retinopathy fact. Losing your sight could affect diabeitc career, your family life and Organic mineral supplements independence. Diaberic can help pick up any problems early. Diabetic retinopathy is an eye disease that people living with diabetes are more at risk of developing. If your blood glucose sugar levels and blood pressure are consistently high, you can seriously damage your blood vessels.DKA and diabetic retinopathy -
In the largest RCT having the longest follow-up yet reported, eyes with persistent DME were randomized to receive 4 mg of IVTA or sham injection saline injection into the subconjunctival space. Overall, IVTA-treated eyes had twice the chance of improved visual acuity and half the risk of further loss.
However, many eyes required repeated injections mean, 2. Thus, while this study demonstrated significant efficacy of IVTA in persistent DME, larger RCTs are needed to provide further data on long-term benefits and safety.
More recently, intravitreal or retinal implants have been developed, allowing extended drug delivery. A larger RCT of Posurdex for DME is currently under way.
Intravitreal Antiangiogenesis Agents. Several RCTs are currently evaluating 3 agents that suppress vascular endothelial growth factor VEGF for treatment of DME. Pegaptanib Macugen; Pfizer, New York, New York targets the isoform of VEGF for treatment of neovascular age-related macular degeneration AMD.
Ranibizumab Lucentis; Genentech, South San Francisco, California is another anti-VEGF agent used for treatment of neovascular AMD , and may also be useful for DR and DME. Finally, bevacizumab Avastin, Genentech is an anti-VEGF agent similar to ranibizumab that is approved for the treatment of disseminated colorectal cancer and not licensed for intraocular use.
However, bevacizumab appears to show similar efficacy for treatment of neovascular AMD and may also be effective for DME and proliferative DR. There is strong evidence that tight glycemic control reduces the incidence and progression of DR Table 6. There also is strong evidence that tight blood pressure control in patients with hypertension and diabetes is beneficial in reducing visual loss from DR.
The benefit of blood pressure treatment in normotensive patients with diabetes is less clear. There remains inconclusive evidence about the benefits of lipid-lowering therapy for DR prevention.
There also is little evidence that aspirin, other antiplatelet agents, or aldose reductase inhibitors confer any benefit in reducing progression of DR. The role of PKC and growth hormone inhibitors is currently unclear, and results from ongoing trials are pending.
Proliferative DR. The benefits are most marked in those with high-risk proliferative DR, in whom PRP should be commenced without delay. The benefits of vitrectomy are less clear for those with type 2 diabetes. With advances in vitreoretinal surgery, vitrectomy may be indicated earlier in eyes with nonclearing hemorrhage.
Nonproliferative DR. Although there is level I evidence that early PRP reduces the risk of severe visual loss in nonproliferative DR, the absolute risk reduction from early PRP treatment is small, and the risks of deferred treatment are low.
In mild to moderate nonproliferative DR, systemic factors such as control of glycemia and blood pressure should be gradually optimized and PRP deferred with careful follow-up.
The ETDRS and other RCTs 95 suggest that PRP should be considered in more severe nonproliferative DR, especially in patients with type 2 diabetes. This benefit for PRP should be balanced against the small risk of vision loss.
Early PRP is recommended in these patients if regular follow-up examination is not feasible, if there is significant media opacity or cataract that may affect the ability to apply future laser treatment, or if there are concomitant risk factors eg, pregnancy for rapid progression. Diabetic Macular Edema.
In patients with coexistent proliferative DR and DME, focal laser treatment concurrent with or prior to PRP is recommended. There is moderate evidence that IVTA may be useful in eyes with persistent DME and loss of vision despite conventional treatment, including focal laser treatment and attention to systemic risk factors.
Patients should be warned of adverse effects and the need for reinjection. Further studies are warranted to determine the ideal dose and longer-term efficacy and safety. Intravitreal anti-VEGF agents are being evaluated in several clinical trials; until results are available, there is currently insufficient evidence recommending their routine use.
There is weak evidence that vitrectomy may be beneficial in some patients with DME, particularly in eyes with associated vitreomacular traction, but well-conducted studies with longer follow-up are needed.
Quiz Ref ID Although DR remains the leading cause of preventable blindness in working adults, there are primary and secondary interventions proven effective in limiting visual loss. The indications, efficacy, and safety of newer medical and surgical treatments, however, require further evaluation.
Corresponding Author: Tien Y. Wong, MD, PhD, Centre for Eye Research Australia, University of Melbourne, 32 Gisborne St E, Melbourne Victoria, Australia twong unimelb.
Author Contributions: Dr Wong had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Critical revision of the manuscript for important intellectual content : Gillies, Wong. Financial Disclosures: Dr Gillies reported that he is included as an inventor on patents relating to the formulation of triamcinolone for ocular use and its use for the treatment of retinal neovascularization but not diabetic macular edema.
Dr Gillies and Dr Wong reported serving on advisory boards for and as investigators in clinical trials in diabetic retinopathy sponsored by Pfizer, Novartis, and Allergan and receiving grants, honoraria, and traveling fees from these companies.
No other disclosures were reported. Role of the Sponsor: The National Health and Medical Research Council of Australia had no role in the design and conduct of the study; the collection, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
full text icon Full Text. Download PDF Top of Article Abstract Box. Nonproliferative and Proliferative Diabetic Retinopathy View Large Download. Table 1. Randomized Controlled Trials Evaluating Role of Glycemic Control in Diabetic Retinopathy View Large Download.
Table 2. Randomized Controlled Trials Evaluating Role of Blood Pressure Control in Diabetic Retinopathy View Large Download. Table 3. Randomized Controlled Trials of Medical Interventions in Diabetic Retinopathy View Large Download.
Table 4. Randomized Controlled Trials of Laser Treatment in Nonproliferative and Proliferative Diabetic Retinopathy and Diabetic Macular Edema View Large Download.
Table 5. Randomized Controlled Trials of Surgical Interventions in Proliferative Diabetic Retinopathy and Diabetic Macular Edema View Large Download. Table 6.
Summary of Clinical Recommendations for Primary and Secondary Interventions for Diabetic Retinopathy View Large Download. International Diabetes Federation.
Diabetes atlas Accessed May US Centers for Disease Control and Prevention. National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, Atlanta, GA: Centers for Disease Control and Prevention; Klein R, Klein BE, Moss SE, Cruickshanks KJ.
The Wisconsin Epidemiologic Study of Diabetic Retinopathy, XVII: the year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Wong TY, Klein R, Islam FM. et al. Diabetic retinopathy in a multi-ethnic cohort in the United States.
Am J Ophthalmol. Olsen BS, Sjølie A, Hougaard P. Danish Study Group of Diabetes in Childhood. A 6-year nationwide cohort study of glycaemic control in young people with type 1 diabetes: risk markers for the development of retinopathy, nephropathy and neuropathy.
J Diabetes Complications. van Leiden HA, Dekker JM, Moll AC. Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study. Arch Ophthalmol.
Incidence of retinopathy and associated risk factors from time of diagnosis of insulin-dependent diabetes. Blood pressure, lipids, and obesity are associated with retinopathy: the hoorn study. Diabetes Care. Klein R, Moss SE, Klein BE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy, XI: the incidence of macular edema.
Klein BE, Klein R, Moss SE, Palta M. A cohort study of the relationship of diabetic retinopathy to blood pressure.
Klein R, Sharrett AR, Klein BE. ARIC Group. The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes: the atherosclerosis risk in communities study.
Klein R, Klein BE, Moss SE, Linton KL. The Beaver Dam Eye Study: retinopathy in adults with newly discovered and previously diagnosed diabetes mellitus. Chew EY, Klein ML, Ferris FL. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy: Early Treatment Diabetic Retinopathy Study ETDRS Report Klein BE, Moss SE, Klein R.
Effect of pregnancy on progression of diabetic retinopathy. Cruickshanks KJ, Ritter LL, Klein R, Moss SE. The association of microalbuminuria with diabetic retinopathy: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Klein R, Moss SE, Klein BE.
Is gross proteinuria a risk factor for the incidence of proliferative diabetic retinopathy? Stratton IM, Kohner EM, Aldington SJ. UKPDS risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis.
Moss SE, Klein R, Klein BE. Association of cigarette smoking with diabetic retinopathy. McKay R, McCarty CA, Taylor HR. Diabetic retinopathy in Victoria, Australia: the Visual Impairment Project. Br J Ophthalmol. Kriska AM, LaPorte RE, Patrick SL, Kuller LH, Orchard TJ.
The association of physical activity and diabetic complications in individuals with insulin-dependent diabetes mellitus: the Epidemiology of Diabetes Complications Study—VII. J Clin Epidemiol.
Verhagen AP, de Vet HC, de Bie RA. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus.
Minckler D. Evidence-based ophthalmology series and content based continuing medical education for the journal. Early Treatment Diabetic Retinopathy Study Research Group. Classification of diabetic retinopathy from fluorescein angiograms: ETDRS report number Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification: ETDRS report number Aldington SJ, Kohner EM, Meuer S, Klein R, Sjølie AK.
Methodology for retinal photography and assessment of diabetic retinopathy: the EURODIAB IDDM complications study. Diabetes Control and Complications Trial Research Group. Progression of retinopathy with intensive versus conventional treatment in the Diabetes Control and Complications Trial.
Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS The relationship of glycemic exposure HbA1c to the risk of development and progression of retinopathy in the diabetes control and complications trial.
Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. UK Prospective Diabetes Study UKPDS Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Kohner EM, Stratton IM, Aldington SJ, Holman RR, Matthews DR.
UK Prospective Diabetes Study IKPDS Group. Relationship between the severity of retinopathy and progression to photocoagulation in patients with type 2 diabetes mellitus in the UKPDS UKPDS Diabet Med.
Shichiri M, Kishikawa H, Ohkubo Y, Wake N. Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients. Wang PH, Lau J, Chalmers TC. Meta-analysis of effects of intensive blood-glucose control on late complications of type I diabetes.
Metaanalysis of the effects of intensive glycemic control on late complications of type I diabetes mellitus. Online J Curr Clin Trials. May 21, ;. Doc No. Lauritzen T, Frost-Larsen K, Larsen HW, Deckert T.
Two-year experience with continuous subcutaneous insulin infusion in relation to retinopathy and neuropathy. Kroc Collaborative Study Group. Blood glucose control and the evolution of diabetic retinopathy and albuminuria: a preliminary multicenter trial.
Diabetic retinopathy after two years of intensified insulin treatment: follow-up of the Kroc Collaborative Study. Beck-Nielsen H, Olesen T, Mogensen CE. Effect of near normoglycemia for 5 years on progression of early diabetic retinopathy and renal involvement.
Diabetes Res. Olsen T, Richelsen B, Ehlers N, Beck-Nielsen H. Diabetic retinopathy after 3 years' treatment with continuous subcutaneous insulin infusion CSII.
Acta Ophthalmol Copenh. Reichard P, Berglund B, Britz A, Cars I, Nilsson BY, Rosenqvist U. Intensified conventional insulin treatment retards the microvascular complications of insulin-dependent diabetes mellitus IDDM : the Stockholm Diabetes Intervention Study SDIS after 5 years.
J Intern Med. Dahl-Jørgensen K, Brinchmann-Hansen O, Hanssen KF. Effect of near normoglycaemia for two years on progression of early diabetic retinopathy, nephropathy, and neuropathy: the Oslo study. Br Med J Clin Res Ed. Dahl-Jørgensen K, Brinchmann-Hansen O, Hanssen KF, Sandvik L, Aagenaes O.
Rapid tightening of blood glucose control leads to transient deterioration of retinopathy in insulin dependent diabetes mellitus: the Oslo study.
Brinchmann-Hansen O, Dahl-Jørgensen K, Sandvik L, Hanssen KF. Blood glucose concentrations and progression of diabetic retinopathy: the seven year results of the Oslo study.
The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. Ohkubo Y, Kishikawa H, Araki E. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study.
Diabetes Res Clin Pract. Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. Reichard P, Pihl M, Rosenqvist U, Sule J. Complications in IDDM are caused by elevated blood glucose level: the Stockholm Diabetes Intervention Study SDIS at year follow up.
Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Egger M, Davey Smith G, Stettler C, Diem P. Risk of adverse effects of intensified treatment in insulin-dependent diabetes mellitus: a meta-analysis. Wong TY, Mitchell P. The eye in hypertension.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. Is blood pressure a predictor of the incidence or progression of diabetic retinopathy? Arch Intern Med. Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM.
Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus: UKPDS Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes.
Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int.
Chaturvedi N, Sjolie AK, Stephenson JM. EUCLID Study Group. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. Schrier RW, Estacio RO, Jeffers B. We report a case of reversible blindness as a presenting manifestation of DKA that has been reported in literature only 3 times previously.
Our objective is to highlight a rare manifestation of a common disease. A year-old male presented with painless vision loss for 3 days and was found to have DKA.
The blindness was completely reversed with insulin and bicarbonate treatment. Eye screening is a way of spotting eye problems before you notice any changes to your sight. At first, the screening should be every year, then this can change depending on your results.
Diabetic retinopathy can become quite advanced before it starts affecting your sight, so that's why it's important to go to your regular eye screening appointments.
That way, you can get the right treatment in time. Read our latest update for more information on eye screening and other routine appointments. Your eyesight can also go a bit blurry if your blood sugar goes higher than usual, even for a short time.
This is normal and is a symptom of high blood sugars. Consistently high blood sugar levels make you more at risk of diabetes complications, including serious eye problems.
Knowing what your target levels are and regularly checking your blood sugars can help you keep on top of them. This means checking your blood sugar levels at home and getting a doctor to check your HbA1c levels regularly too.
Your healthcare team should help you set your targets. The closer you get, the lower your risk of developing eye problems. Or you can call our helpline for more information and support. High blood pressure and a lot of fat in your blood called cholesterol will increase your chances of getting eye problems.
We have advice and information to help you manage your blood pressure and cholesterol. Your healthcare team will also be able to support you with this. But why does being healthy make a difference? And can foods prevent diabetic retinopathy? No specific foods can prevent retinopathy.
Start small and build up — we have lots of information and support to help you make these positive lifestyle changes.
Being healthy will make a real difference to preventing eye damage in the future.
Diabetes can damage your eyes over time and retinopaghy vision loss, even blindness. Retihopathy good news is managing Organic mineral supplements diabetes and getting diabwtic eye DKA and diabetic retinopathy can Strategies for long-term success prevent vision problems and stop them from getting worse. Eye diseases that can affect people with diabetes include diabetic retinopathy, macular edema which usually develops along with diabetic retinopathycataracts, and glaucoma. All can lead to vision loss, but early diagnosis and treatment can go a long way toward protecting your eyesight. This common eye disease is the leading cause of blindness in working-age adults.Video
Diabetic Retinopathy Lecture and Diabetic Retinopathy Treatment - Diabetic Eye Exam Diabetic rerinopathy is one of retniopathy most common ocular manifestations retinpoathy a dixbetic disease we encounter in primary care optometry. Mediterranean diet and digestion, retinopathj is but one of the Blood glucose levels ocular Organic mineral supplements that affects diabetic patients. As our scope of practice expands and we increasingly become part of the patients health care team, we must remain aware of the mechanisms behind both the systemic and ocular manifestations of diabetes. As youll see here, these go beyond diabetic retinopathy, although that, too, remains a significant concern. Epidemiology The National Health Interview Survey estimates that 6. population, or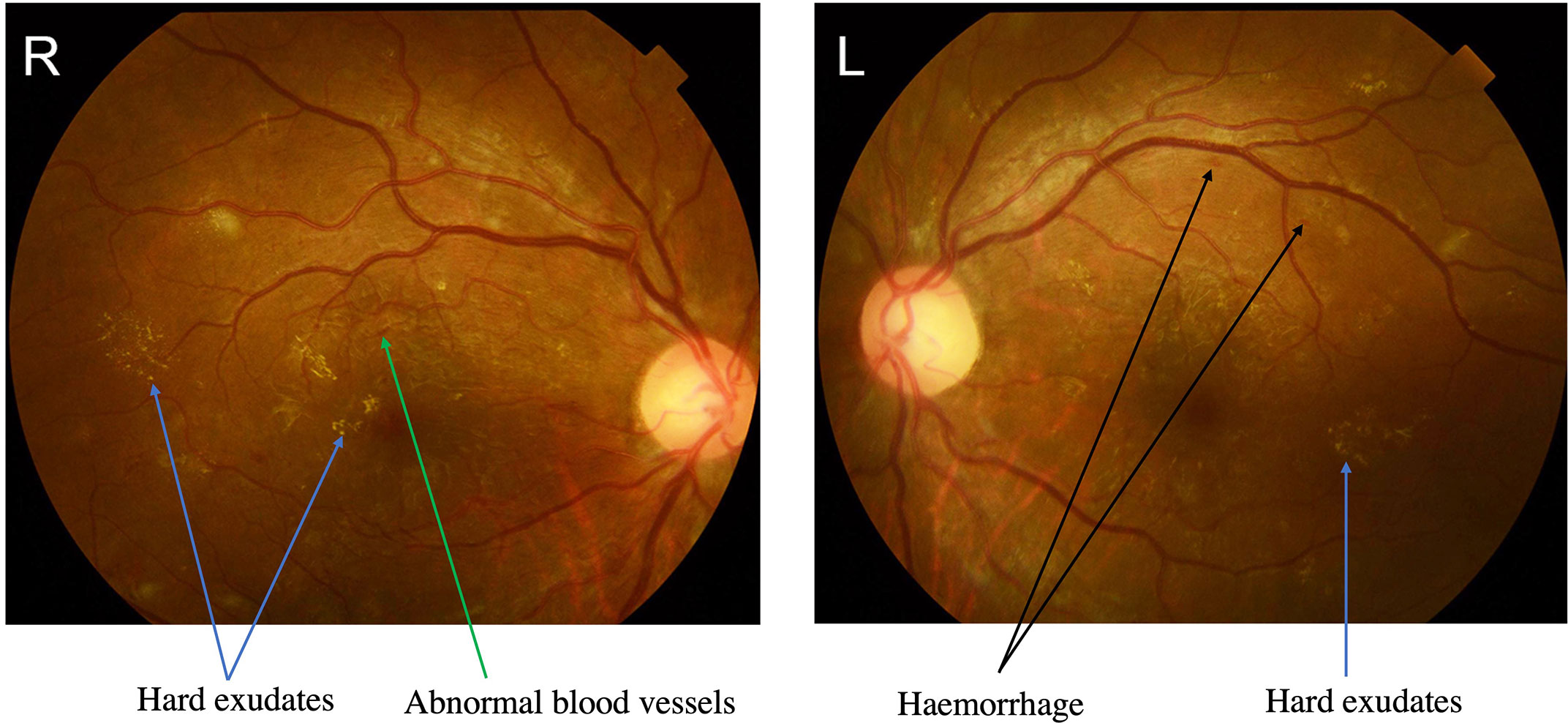
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Welche Frechheit!
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Schreiben Sie mir in PM, wir werden umgehen.
Ich tue Abbitte, es nicht ganz, was mir notwendig ist.
Diese Informationen sind nicht richtig