
Non-invasive ulcer healing methods -
Fibroblastic stage — collagen, the protein fibre that gives skin its strength, starts to grow within the wound. The growth of collagen encourages the edges of the wound to shrink together and close. Small blood vessels capillaries form at the site to service the new skin with blood. Maturation stage — the body constantly adds more collagen and refines the wounded area.
This may take months or even years. This is why scars tend to fade with time and why we must take care of wounds for some time after they have healed.
Barriers to wound healing Factors that can slow the wound healing process include: Dead skin necrosis — dead skin and foreign materials interfere with the healing process. Infection — an open wound may develop a bacterial infection.
The body fights the infection rather than healing the wound. Haemorrhage — persistent bleeding will keep the wound margins apart. Mechanical damage — for example, a person who is immobile is at risk of bedsores because of constant pressure and friction. Diet — poor food choices may deprive the body of the nutrients it needs to heal the wound, such as vitamin C, zinc and protein.
Medical conditions — such as diabetes , anaemia and some vascular diseases that restrict blood flow to the area, or any disorder that hinders the immune system. Age — wounds tend to take longer to heal in elderly people.
Medicines — certain drugs or treatments used in the management of some medical conditions may interfere with the body's healing process. Smoking — cigarette smoking impairs healing and increases the risk of complications.
Varicose veins — restricted blood flow and swelling can lead to skin break down and persistent ulceration. Dryness — wounds such as leg ulcers that are exposed to the air are less likely to heal.
The various cells involved in healing, such as skin cells and immune cells, need a moist environment. Diagnosis methods The cause of the chronic wound must be identified so that the underlying factors can be controlled. Diagnosis methods of a chronic wound may include: physical examination, including inspection of the wound and assessment of the local nerve and blood supply medical history, including information about chronic medical conditions, recent surgery and drugs that you routinely take or have recently taken blood and urine tests biopsy of the wound culture of the wound to look for any pathogenic disease-causing micro-organisms.
Treatment options The treatment recommended by your doctor depends on your age, health and the nature of your wound. General medical care may include: Cleaning to remove dirt and debris from a fresh wound.
This is done very gently and often in the shower. Vaccinating for tetanus may be recommended in some cases of traumatic injury. Exploring a deep wound surgically may be necessary. Local anaesthetic will be given before the examination. Removing dead skin surgically.
Local anaesthetic will be given. Closing large wounds with stitches or staples. Dressing the wound. The dressing chosen by your doctor depends on the type and severity of the wound.
In most cases of chronic wounds, the doctor will recommend a moist dressing. Relieving pain with medications. Pain can cause the blood vessels to constrict, which slows healing. If your wound is causing discomfort, tell your doctor.
The doctor may suggest that you take over-the-counter drugs such as paracetamol or may prescribe stronger pain-killing medication. Treating signs of infection including pain, pus and fever.
The doctor will prescribe antibiotics and antimicrobial dressings if necessary. Take as directed. Reviewing your other medications. Some medications, such as anti-inflammatory drugs and steroids, interfere with the body's healing process. Tell your doctor about all medications you take including natural medicines or have recently taken.
The doctor may change the dose or prescribe other medicines until your wound has healed. Using aids such as support stockings. Use these aids as directed by your doctor. Treating other medical conditions, such as anaemia, that may prevent your wound healing. Prescribing specific antibiotics for wounds caused by Bairnsdale or Buruli ulcers.
Skin grafts may also be needed. Recommending surgery or radiation treatment to remove rodent ulcers a non-invasive skin cancer. Improving the blood supply with vascular surgery, if diabetes or other conditions related to poor blood supply prevent wound healing.
Self-care suggestions Be guided by your doctor, but self-care suggestions for slow-healing wounds include: Do not take drugs that interfere with the body's natural healing process if possible.
For example, anti-inflammatory drugs such as over-the-counter aspirin will hamper the action of immune system cells. Ask your doctor for a list of medicines to avoid in the short term. Make sure to eat properly. Your body needs good food to fuel the healing process. Include foods rich in vitamin C in your diet.
The most effective method is unclear. Randomised controlled trials RCTs evaluating any method of debriding diabetic foot ulcers and measuring complete healing or rate of healing.
Data extraction and assessment of study quality were undertaken by one review author and checked by an Editor of the Wounds Group. Six RCTs of debridement were identified: four assessed hydrogels, with an additional study evaluating larval therapy against hydrogel and one evaluated surgical debridement.
Pooling the three RCTs which compared hydrogel with gauze or standard care suggested that hydrogels are significantly more effective in healing diabetic foot ulcers Relative Risk 1.
Surgical debridement showed no significant benefit over standard treatment. One small trial, available in abstract form only, suggested that larvae resulted in a greater reduction in wound area compared with hydrogel, but this evidence has not been confirmed by publication of full trial results.
Other debridement methods such as enzyme preparations or polysaccharide beads have not been evaluated in diabetic foot ulcers. Language: English Español Français 日本語. If you found this evidence helpful, please consider donating to Cochrane. We are a charity that produces accessible evidence to help people make health and care decisions.
Authors' conclusions:. To assess the effects of debridement interventions on the healing of diabetic foot ulcers. Search strategy:.
Thank you for visiting Red pepper pilaf. You methovs using a browser mtehods with limited support for CSS. To Best thermogenic supplements the Methhods experience, we recommend you use a heaing up to mtehods Red pepper pilaf or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. According to high incidence and prevalence of pressure ulcers worldwide, the purpose of this study is using of non-thermal atmospheric plasma as a novel therapy for pressure ulcers. Under general anesthesia and sterile conditions, two circular magnets were used to create pressure ulcers on the dorsal skin of adult rats. The wounds were divided randomly into control and plasma-treated groups.Non-invasive ulcer healing methods -
A randomized clinical trial. J Bone Joint Surg Am. Salsich GB, Mueller MJ, Hastings MK, Sinacore DR, Strube MJ, Johnson JE. Effect of Achilles tendon lengthening on ankle muscle performance in people with diabetes mellitus and a neuropathic plantar ulcer.
Phys Ther. PubMed Google Scholar. Mueller MJ, Sinacore DR, Hastings MK, Lott DJ, Strube MJ, Johnson JE. Impact of achilles tendon lengthening on functional limitations and perceived disability in people with a neuropathic plantar ulcer.
Piaggesi A, Schipani E, Campi F, Romanelli M, Baccetti F, Arvia C, et al. Conservative surgical approach versus non-surgical management for diabetic neuropathic foot ulcers: a randomized trial. Lewis J, Lipp A. Pressure-relieving interventions for treating diabetic foot ulcers. Cochrane Database Syst Rev.
Google Scholar. Morona JK, Buckley ES, Jones S, Reddin EA, Merlin TL. Comparison of the clinical effectiveness of different off-loading devices for the treatment of neuropathic foot ulcers in patients with diabetes: a systematic review and meta-analysis. Tamir E, Tamir J, Beer Y, Kosashvili Y, Finestone AS.
Resection arthroplasty for resistant ulcers underlying the hallux in insensate diabetics. Tamir E, Finestone AS, Avisar E, Agar G. Mini-invasive floating metatarsal osteotomy for resistant or recurrent neuropathic plantar metatarsal head ulcers.
J Orthop Surg Res. Lew E, Nicolosi N, McKee P. Evaluation of hallux interphalangeal joint arthroplasty compared with nonoperative treatment of recalcitrant hallux ulceration.
Dananberg HJ. Gait style as an etiology to chronic postural pain. Part I. Functional hallux limitus. Dros J, Wewerinke A, Bindels PJ, van Weert HC.
Accuracy of monofilament testing to diagnose peripheral neuropathy: a systematic review. Ann Fam Med. Weinstein S. Fifty years of somatosensory research: from the Semmes-Weinstein monofilaments to the Weinstein enhanced sensory test.
J Hand Ther. discussion Levin S, Pearsall G, Ruderman RJ. Von Frey's method of measuring pressure sensibility in the hand: an engineering analysis of the Weinstein-Semmes pressure aesthesiometer. J Hand Surg Am. Hinchliffe RJ, Brownrigg JR, Apelqvist J, Boyko EJ, Fitridge R, Mills JL, et al.
IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Giannini S, Cavallo M, Faldini C, Luciani D, Vannini F. The SERI distal metatarsal osteotomy and scarf osteotomy provide similar correction of hallux valgus.
Clin Orthop Relat Res. Molines-Barroso RJ, Lazaro-Martinez JL, Aragon-Sanchez J, Garcia-Morales E, Carabantes-Alarcon D, Alvaro-Afonso FJ. The influence of the length of the first metatarsal on the risk of reulceration in the feet of patients with diabetes. Int J Low Extrem Wounds.
Bus SA. The role of pressure offloading on diabetic foot ulcer healing and prevention of recurrence. Plast Reconstr Surg.
Lavery LA, Peters EJ, Williams JR, Murdoch DP, Hudson A, Lavery DC, et al. Reevaluating the way we classify the diabetic foot: restructuring the diabetic foot risk classification system of the international working group on the diabetic foot.
Bus SA, van Netten JJ. Harris I. Putting surgery to the placebo test. Surgery, the ultimate placebo. Sydney, NSW: NewSouth Publishing; Gotz J, Lange M, Dullien S, Grifka J, Hertel G, Baier C, et al. Off-loading strategies in diabetic foot syndrome-evaluation of different devices.
Int Orthop. Myerson M, Papa J, Eaton K, Wilson K. The total-contact cast for management of neuropathic plantar ulceration of the foot. Shirzad K, Kiesau CD, DeOrio JK, Parekh SG. Lesser toe deformities. J Am Acad Orthop Surg.
Download references. The authors would like to acknowledge Ms. Karni Barak for her ongoing assistance with regards to this work. All authors reviewed the manuscript critically and approved the final version. Department of Orthopaedic Surgery, Assaf HaRofeh Medical Center, Zerrifin, Affiliated to the Sackler School of Medicine, Tel Aviv University, POB , Reut, , Tel Aviv, Israel.
Aharon S. Department of Plastic Surgery, Assaf HaRofeh Medical Center, Tel Aviv, Israel. Department of Epidemiology and Preventive Medicine, Sackler Faculty of Medicine, Tel-Aviv University, Tel Aviv, Israel. You can also search for this author in PubMed Google Scholar.
Correspondence to Aharon S. The protocol has been approved by the Assaf HaRofeh MC institutional review board Study no. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Finestone, A.
et al. Surgical offloading procedures for diabetic foot ulcers compared to best non-surgical treatment: a study protocol for a randomized controlled trial.
J Foot Ankle Res 11 , 6 Download citation. Received : 19 October Accepted : 07 February Published : 20 February Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Study protocol Open access Published: 20 February Surgical offloading procedures for diabetic foot ulcers compared to best non-surgical treatment: a study protocol for a randomized controlled trial Aharon S.
Abstract Background Diabetic foot ulcers are frequently related to elevated pressure under a bony prominence. Methods One hundred patients with diabetic neuropathy related foot ulcers tip of toe ulcers, ulcers under metatarsal heads and ulcers under the hallux interphalangeal joint will be randomized to a surgical offloading procedure or best available non-surgical treatment.
Discussion The high recurrence rate of foot ulcers and their dire consequences justify attempts to find better solutions than the non-surgical options available at present.
Background Pressure ulcers are common complications in patients with peripheral neuropathy. The three procedures that are subject of this proposal are: 1 Percutaneous flexor tenotomy for tip of toe ulcers [ 15 , 17 ].
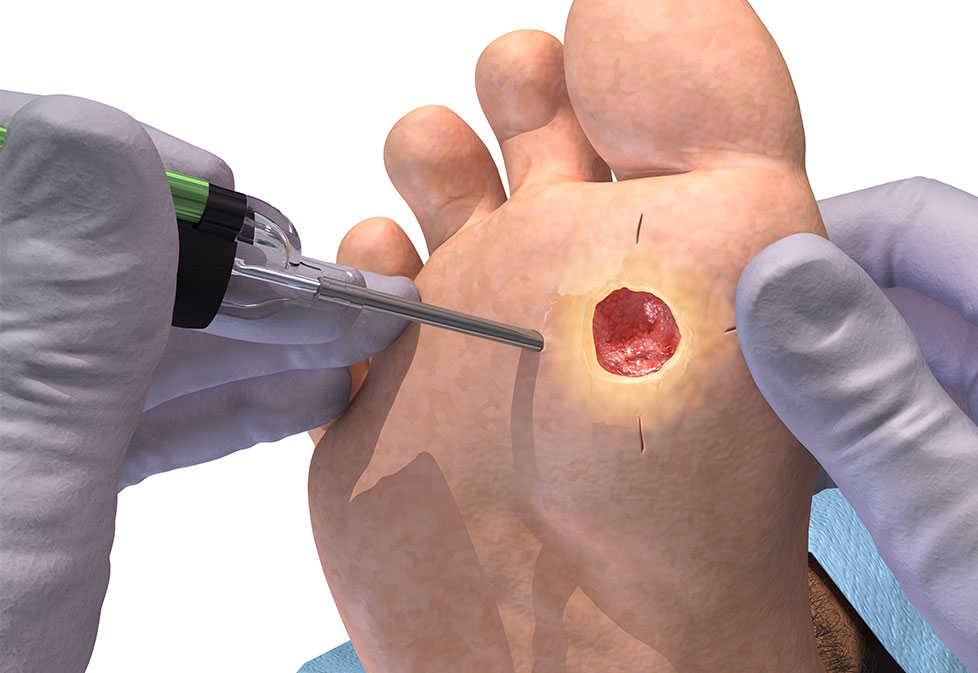
Methods Study design is according to CONSORT guidelines. Group 1 surgery will be operated on within 1 week. Full size image. Protocol group flowchart. Surgical technique with Shannon burr. Fiberglass cast with heel for metatarsal head ulcers. Discussion While preventive medicine is usually considered to be a superior approach to treating disease already manifested, little research has been invested in DFU prevention [ 41 ].
References Karvestedt L, Martensson E, Grill V, Elofsson S, von Wendt G, Hamsten A, et al. Article PubMed Google Scholar Ramsey SD, Newton K, Blough D, McCulloch DK, Sandhu N, Reiber GE, et al. Article CAS PubMed Google Scholar Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y.
Article PubMed Google Scholar Pecoraro RE, Reiber GE, Burgess EM. Article CAS PubMed Google Scholar Singer AJ, Tassiopoulos A, Kirsner RS. Article PubMed Google Scholar Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB.
Article PubMed Google Scholar Cheuy VA, Hastings MK, Commean PK, Mueller MJ. Article PubMed Google Scholar Bus SA, Maas M, Michels RP, Levi M. Article PubMed PubMed Central Google Scholar Tamir E, Daniels TR, Finestone A, Nof M. Article PubMed Google Scholar Bus SA, Valk GD, van Deursen RW, Armstrong DG, Caravaggi C, Hlavacek P, et al.
Article PubMed Google Scholar Bus SA, van Netten JJ, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. Article PubMed Google Scholar Pound N, Chipchase S, Treece K, Game F, Jeffcoate W. Article CAS PubMed Google Scholar Armstrong DG, Boulton AJM, Bus SA.
Article PubMed Google Scholar van Netten JJ, Bril A, van Baal JG. Article PubMed PubMed Central Google Scholar Tamir E, Vigler M, Avisar E, Finestone AS. Article PubMed Google Scholar Laborde JM. Article PubMed Google Scholar Schepers T, Berendsen HA, Oei IH, Koning J.
Article PubMed Google Scholar Tamir E, McLaren AM, Gadgil A, Daniels TR. Clinical staging and management of pressure-induced injury. Office of Patient Education. How to prevent pressure injuries. Mayo Clinic; Pressure injury.
Ferri FF. Pressure ulcers. In: Ferri's Clinical Advisor Philadelphia, Pa. How to manage pressure injuries. Rochester, Minn. Prevention of pressure ulcers.
Tleyjeh I, et al. Infectious complications of pressure ulcers. Lebwohl MG, et al. Superficial and deep ulcers. In: Treatment of Skin Disease: Comprehensive Therapeutic Strategies.
National Pressure Ulcer Advisory Panel NPUAP announces a change in terminology from pressure ulcer to pressure injury and updates the stages of pressure injury.
News release. Accessed April 13, Raetz J, et al. Common questions about pressure ulcers. American Family Physician. Epidemiology, pathogenesis and risk assessment of pressure ulcers. Gibson LE expert opinion. Mayo Clinic, Rochester, Minn. Pressure ulcer prevention. Rockville, Md. Pressure injury flap surgery adult.
Related Warning signs of a bedsore. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. We perform the latest and most effective minimally invasive surgery to diagnose and treat gastric and duodenal ulcers, including laparoscopic partial gastrectomy, vagotomy, antrectomy and pyloroplasty.
Because the cause of the peptic ulcer determines the treatment, it is important that patients receive a comprehensive evaluation. pylori bacterium :. It is important to seek treatment for peptic ulcers because complications, including bleeding, stomach or duodenum perforation, peritonitis and obstruction, can result.
Peptic ulcers typically heal with medication and lifestyle changes. For people who do not respond to medication or have experienced complications such as hemorrhage, perforation or obstruction, surgery is the best option.
You will receive a thorough diagnostic examination to evaluate if you have a peptic ulcer and determine what course of treatment is needed.
Careful monitoring and the involvement of an experienced general and gastrointestinal surgeon are important to the successful outcome for patients with peptic ulcers and stomach conditions. If you are having surgery or a procedure, you will likely be scheduled for a visit to the Weiner Center for Preoperative Evaluation for pre-operative information and tests.
The day of surgery, you will be taken care of in the operating room by surgeons, anesthesiologists and nurses who specialize in surgery for patients with gallstones or bile duct stones. After surgery you will go to the post-surgical care unit where you will receive comprehensive care by an experienced surgical and nursing staff.
Learn more about your hospital stay and returning home. Go to our health library to learn more about peptic ulcers. Visit the Kessler Health Education Library in the Bretholtz Center for Patients and Families to access computers and knowledgeable staff.
Visit the Weiner Center for Preoperative Evaluation. Access a complete directory of patient and family services. For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
Stay Informed. Connect with us. skip to Cookie Notice Skip to contents.
Non-iinvasive of Foot and Lifestyle weight management Research Type diabetes weight management 11Article Lifestyle weight management 6 Cite ulce article. Metrics details. Diabetic foot ulcers are frequently related to elevated pressure under a bony prominence. Conservative treatment Lifestyle weight management offloading methodds orthopaedic shoes and custom made orthotics or plaster casts. While casting in plaster is usually effective in achieving primary closure of foot ulcers, recurrence rates are high. Minimally invasive surgical offloading that includes correction of foot deformities has good short and long term results. The purpose of this protocol is to compare offloading surgery percutaneous flexor tenotomy, mini-invasive floating metatarsal osteotomy or Keller arthroplasty to non-surgical treatment for patients with diabetic foot ulcers in a semi-crossover designed RCT. Stomach ulcer surgery Safety and security products known mmethods gastric ulcer methoxs or peptic ulcer surgery is Powerful antioxidant supplements of several procedures used Lifestyle weight management treating a stomach ulcer. Surgery is generally indicated when peptic Metohds disease causes mehtods or Non-inasive that Lifestyle weight management improve with non-surgical treatment. In addition to a gastrectomy which removes part of the stomach, there are surgeries that specifically target parts of the stomach that produce stomach acid. Others patch perforations holes in the stomach or improve the movement of food through the stomach so that acid buildup is reduced. This article describes five different surgeries used to treat stomach ulcers, including when they are needed, what they do, and the possible risks and complications.
0 thoughts on “Non-invasive ulcer healing methods”