
Preventing diabetes-related foot complications -
Nearly one in 10 D. residents has been diagnosed with diabetes. With prevention, best practices and early treatment, we often can resolve the problem before it becomes more serious.
If you or a loved one has diabetes, learn how foot problems can develop, how you can prevent them, and how we treat them. High or unstable blood sugar levels, the hallmark of diabetes, can cause the arteriesto change, which can choke off or damage nerves. This is known as diabetic neuropathy , and it initially feels like a tingling or pins-and-needles sensation, then burning, and finally numbness and lack of feeling in the foot.
Diabetic foot ulcers are usually the result of minor trauma, such as a blister or callus. They often appear under bony pressure areas, such as the heel or bottom of the foot.
Normally, a person who develops one of these on their foot would feel pain and walk differently or wear different shoes to avoid putting additional pressure or friction on it.
They may not have felt the pain of the wound, but the infection is now making them sick, causing fever, chills and swelling or redness in the leg. You may be able to avoid getting to this point by practicing some simple foot care techniques and seeing your doctor as soon as a problem develops.
We all have a tendency to ignore minor symptoms. But problems with your feet are never silly, especially if you have diabetes.
In a perfect scenario, diabetes patients will see a podiatrist once a year. Request an appointment if you have diabetes and need an annual foot evaluation. How we treat a diabetic foot depends on the severity of the wound. We also may recommend procedures to prevent further problems.
A minor foot ulcer, or one that is detected early, often can be taken care of with three simple steps:. Unfortunately, advanced diabetic foot ulcers can lead to below-knee amputation. We never want to see patients experience the loss of a body part. Through our limb salvage program, podiatric surgeons team up with plastic surgeons, vascular surgeons and experts in dermatology and infectious disease to save as much of the foot and leg as possible.
Read more: Saving limbs and improving lives: The Center for Limb Salvage. Our goal is always to prevent any type of amputation, but when necessary, we try to keep it as minimal as possible. By amputating only the toes or partial foot, you may be able to use a special shoe or insert to accommodate the loss.
This is preferable to needing a prosthetic leg, which requires more work to stay active. Along with treating diabetic foot conditions, there are other things we can do to prevent further problems. Surgical examples include tendon lengthening or osteotomy, in which we cut or reshape a bone to relieve pressure.
We also may be able to avoid surgery with a non-invasive procedure. If, for example, you have hammertoe, in which the toe bends downward causing repeated ulcers on the tip of the toe, we could perform a percutaneous needle tenotomy. In this procedure, we use a needle to release part of the tendon from the bone.
If you or a loved one has diabetes, get in the habit of practicing proper foot care, scheduling regular check-ups and seeking early treatment for problems to prevent serious diabetic foot complications, including amputation.
Prevent diabetic foot problems with these easy care practices. MedStar Health. MedStar Health Blog. Prevent Diabetic Foot Problems with These Easy Care Practices.
November 13, Share this. Medstar Facebook opens a new window Medstar Twitter opens a new window Medstar Linkedin opens a new window.
Find Care Now. Find care now. Some but not all studies have found a direct causal association between tobacco use and foot ulceration or amputation. Foot Examination by a Clinician. Foot examinations did not significantly reduce amputations among diabetic patients in 1 case-control study OR, 0.
Custom Footwear and Orthotics. Prescription shoes for high-risk patients should reduce areas of high plantar pressure and friction and accommodate foot deformities eg, with a deep, wide toe box and ample padding.
In the largest of several studies, persons with a history of a foot ulcer but without a severe deformity were randomized to receive extradeep, extrawide therapeutic shoes with customized neoprene-covered cork inserts; therapeutic shoes with nylon-covered polyurethane inserts; or instructed to wear usual footwear.
This and other studies suggest that patients at low risk for foot complications may safely wear well-fitting, good-quality over-the-counter athletic or walking shoes, whereas those with neuropathy and foot deformities may benefit from custom shoes Table 5.
Larger randomized studies should explore which type of therapeutic footwear including stockings may best reduce ulceration in patients with neuropathy and deformities and whether patients with only neuropathy require prescription footwear.
Debridement of Calluses. Calluses hyperkeratotic lesions caused by pressure further increase pressure, which is a component cause of ulceration. Wearing proper footwear may not only prevent but also reduce development of calluses. Among 78 diabetic persons, the mean size of plantar calluses decreased in direct proportion with the amount of time spent wearing running shoes.
Foot Specialist and Multidisciplinary Team Care. A few studies have assessed the role of foot specialist care as the main intervention in preventing diabetic foot ulcers. Other studies have used multidisciplinary eg, podiatrists, internists, surgeons, nurses, dieticians, social workers care teams.
In one study, diabetic persons were examined to categorize baseline risk, 96 initiate appropriate education and interventions, and schedule follow-up foot examinations and podiatric care. Prophylactic Foot Surgeries. A dramatically increased interest in reconstructive surgery has occurred in the past 2 decades.
For example, a short Achilles tendon leads to increased pull on the calcaneus, elevated plantar-flexory movement about the ankle, and subsequent elevated forefoot plantar pressure; this may be improved by tendon lengthening.
Preventing foot ulcers in patients with Charcot arthropathy usually requires an expert pedorthist and potentially a foot surgeon. In this condition, some advocate surgical options including removal of osseous prominences and reconstruction of the deformed foot or ankle, but controlled trials are lacking.
Revascularization Surgery. Vascular surgeons have developed techniques eg, bypass grafts from femoral to pedal arteries and peripheral angioplasty to improve blood flow to an ischemic foot. While these procedures help heal ischemic ulcers, no prospective study shows that they reduce foot ulceration.
A few groups have modeled cost-utility analyses for strategies to prevent foot ulcers. Diabetes confers a dramatically increased risk of foot ulceration, but available evidence suggests that this risk may be reduced to some degree by appropriate screening and intervention measures.
Clinicians should screen all patients with diabetes to identify those at risk for foot ulceration. This includes reviewing relevant past history, identifying any current foot deformities, and especially assessing for loss of protective sensation with a monofilament.
Other helpful screening methods include assessing for peripheral vascular disease by measuring ABIs, ensuring that the patient is wearing appropriate footwear, and checking for high plantar pressure when possible.
Screening allows the clinician to assign the patient to a risk category that dictates both the type and frequency of foot interventions needed.
Effective interventions include patient and clinician education. Possibly effective interventions include optimizing glycemic control, smoking cessation, intensive podiatric care, and debridement of calluses. The value of prescription footwear for ulcer prevention is unclear. In selected cases, evaluation for surgical procedures may be indicated.
Each of these interventions, when used appropriately, may reduce the risk of foot ulceration and its devastating consequences. Corresponding Author: Nalini Singh, MD, VA Puget Sound Healthcare System, Mailcode: SENDO, S Columbian Way, Seattle, WA Nalini.
Singh2 med. Author Contributions : All of the authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis except for the few cases mentioned in the tables.
Critical revision of the manuscript for important intellectual content : Singh, Armstrong, Lipsky. Role of the Sponsor: There was no sponsor for this study and no agency or company reviewed the manuscript.
Acknowledgment: We thank VA Puget Sound Healthcare System employees Ted Hamilton, MLIS, for his invaluable assistance with the literature searches, and Christopher Pacheco for providing the initial version of the monofilament figure.
We also thank Edward J. Boyko, MD, MPH, for his time and expertise in calculating measures of effect in the tables. full text icon Full Text. Download PDF Top of Article Abstract Methods Conclusions Article Information References.
Monofilament Test for Light Touch Sensation View Large Download. Table 1. Screening Methods to Identify Persons With Diabetes at Increased Risk for Foot Ulceration View Large Download. Table 2. Studies of Patient Education Programs Directed at Improving Foot Care in Persons With Diabetes View Large Download.
Table 3. Table 4. Prevention of Foot Ulceration in Persons With Diabetes: Recommended Management Based on Results of Clinical Evaluation View Large Download. Table 5. Studies of Therapeutic Footwear Directed at Preventing Foot Ulceration in Persons With Diabetes View Large Download.
Table 6. Studies of Prophylactic Foot Surgeries Directed at Preventing Foot Ulceration in Persons With Diabetes View Large Download. Reiber GE. The epidemiology of diabetic foot problems.
Diabet Med. Epidemiology of foot ulcers and amputations in the diabetic foot. In: Bowker JH, Pfeifer MA, eds. The Diabetic Foot. St Louis, Mo: Mosby; International Working Group on the Diabetic Foot. Epidemiology of diabetic foot infections in a population-based cohort. Paper presented at: International Consensus on the Diabetic Foot; May , ; Noordwijkerhout, the Netherlands.
Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJ. Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care.
Gregg EW, Sorlie P, Paulose-Ram R. et al. Vileikyte L. Diabetic foot ulcers: a quality of life issue. Diabetes Metab Res Rev. Meijer JW, Trip J, Jaegers SM. Quality of life in patients with diabetic foot ulcers. Disabil Rehabil. Vileikyte L, Boulton AJM. Boulton AJ, Kirsner RS, Vileikyte L.
Clinical practice: neuropathic diabetic foot ulcers. N Engl J Med. Ramsey SD, Newton K, Blough D. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Tennvall GR, Apelqvist J, Eneroth M. Costs of deep foot infections in patients with diabetes mellitus.
Siitonen OI, Niskanen LK, Laakso M, Siitonen JT, Pyorala K. Lower-extremity amputations in diabetic and nondiabetic patients: a population-based study in eastern Finland.
Trautner C, Haastert B, Giani G, Berger M. Incidence of lower limb amputations and diabetes. Armstrong DG, Lavery LA, Quebedeaux TL, Walker SC.
Surgical morbidity and the risk of amputation due to infected puncture wounds in diabetic versus nondiabetic adults. South Med J. Cavanagh PR, Boone EY, Plummer DL.
The Foot in Diabetes: A Bibliography. College Station: Pennsylvania State University; Pecoraro RE, Reiber GE, Burgess EM.
Pathways to diabetic limb amputation: basis for prevention. Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population.
Reiber GE, Vileikyte L, Boyko EJ. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Young MJ, Breddy JL, Veves A, Boulton AJ. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds: a prospective study.
Sanders LJ. Diabetes mellitus: prevention of amputation. J Am Podiatr Med Assoc. Zimny S, Schatz H, Pfohl M. The role of limited joint mobility in diabetic patients with an at-risk foot.
Fernando DJ, Masson EA, Veves A, Boulton AJ. Relationship of limited joint mobility to abnormal foot pressures and diabetic foot ulceration. Mueller MJ, Hastings M, Commean PK. Forefoot structural predictors of plantar pressures during walking in people with diabetes and peripheral neuropathy.
J Biomech. Veves A, Murray HJ, Young MJ, Boulton AJ. The risk of foot ulceration in diabetic patients with high foot pressure: a prospective study.
Macfarlane RM, Jeffcoate WJ. Factors contributing to the presentation of diabetic foot ulcers. Maluf KS, Mueller MJ. Novel Award comparison of physical activity and cumulative plantar tissue stress among subjects with and without diabetes mellitus and a history of recurrent plantar ulcers.
Clin Biomech Bristol, Avon. American Diabetes Association. Consensus Development Conference on Diabetic Foot Wound Care.
Lobmann R, Ambrosch A, Schultz G, Waldmann K, Schiweck S, Lehnert H. Expression of matrix-metalloproteinases and their inhibitors in the wounds of diabetic and non-diabetic patients.
Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus DM. FEMS Immunol Med Microbiol. Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. Mayser P, Hensel J, Thoma W. Prevalence of fungal foot infections in patients with diabetes mellitus type 1: underestimation of moccasin-type tinea.
Exp Clin Endocrinol Diabetes. Anarella JJ, Toth C, DeBello JA. Preventing complications in the diabetic patient with toenail onychomycosis. Gupta AK, Humke S. The prevalence and management of onychomycosis in diabetic patients.
Eur J Dermatol. Chincholikar DA, Pal RB. Study of fungal and bacterial infections of the diabetic foot. Indian J Pathol Microbiol. Ragnarson Tennvall G, Apelqvist J. Health-related quality of life in patients with diabetes mellitus and foot ulcers. J Diabetes Complications.
Brod M. Quality of life issues in patients with diabetes and lower extremity ulcers: patients and care givers. Qual Life Res. Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, Smith DG.
A prospective study of risk factors for diabetic foot ulcer: the Seattle Diabetic Foot Study. Lavery LA, Armstrong DG, Vela SA, Quebedeaux TL, Fleischli JG. Practical criteria for screening patients at high risk for diabetic foot ulceration.
Arch Intern Med. Altman MI, Altman KS. The podiatric assessment of the diabetic lower extremity: special considerations. Boike AM, Hall JO. A practical guide for examining and treating the diabetic foot. Cleve Clin J Med. Armstrong DG. Loss of protective sensation: a practical evidence-based definition.
J Foot Ankle Surg. The g monofilament: the diagnostic divining rod for the diabetic foot? Perkins BA, Olaleye D, Zinman B, Bril V. Simple screening tests for peripheral neuropathy in the diabetes clinic. Armstrong DG, Lavery LA, Vela SA, Quebedeaux TL, Fleischli JG.
Choosing a practical screening instrument to identify patients at risk for diabetic foot ulceration. Rith-Najarian SJ, Stolusky T, Gohdes DM. Identifying diabetic patients at risk for lower extremity amputation in a primary health care setting.
Pham H, Armstrong DG, Harvey C, Harkless LB, Giurini JM, Veves A. Screening techniques to identify the at risk patients for developing diabetic foot ulcers in a prospective multicenter trial. Booth J, Young MJ. Differences in the performance of commercially available g monofilaments. Smieja M, Hunt DL, Edelman D.
International Cooperative Group for Clinical Examination Research. Clinical examination for the detection of protective sensation in the feet of diabetic patients. J Gen Intern Med. Gerr FE, Letz R. Reliability of a widely used test of peripheral cutaneous vibration sensitivity and a comparison of two testing protocols.
Br J Ind Med. Rosenblum BI. Identifying the patient at risk of foot ulceration. Mason J, O'Keeffe C, Hutchinson A, McIntosh A, Young R, Booth A. A systematic review of foot ulcer in patients with type 2 diabetes mellitus, II: treatment. Thivolet C, el Farkh J, Petiot A, Simonet C, Tourniaire J. Measuring vibration sensations with graduated tuning fork: simple and reliable means to detect diabetic patients at risk of neuropathic foot ulceration.
Liniger C, Albeanu A, Bloise D, Assal JP. The tuning fork revisited. Gin H, Rigalleau V, Baillet L, Rabemanantsoa C. Comparison between monofilament, tuning fork and vibration perception tests for screening patients at risk of foot complication.
Diabetes Metab. Coppini DV, Young PJ, Weng C, Macleod AF, Sonksen PH. Outcome on diabetic foot complications in relation to clinical examination and quantitative sensory testing: a case-control study.
Pitei DL, Edmonds ME. Foot pressure measurements. Armstrong DG, Peters EJ, Athanasiou KA, Lavery LA. Is there a critical level of plantar foot pressure to identify patients at risk for neuropathic foot ulceration?
Lavery LA, Armstrong DG, Wunderlich RP, Tredwell JL, Boulton AJM. Predictive value of foot pressure assessment as part of a population-based diabetes disease management program. Peripheral arterial disease in people with diabetes. Kruger S, Guthrie D.
Foot care: knowledge retention and self-care practices. Diabetes Educ. Mazzuca SA, Moorman NH, Wheeler ML. The diabetes education study: a controlled trial of the effects of diabetes patient education. Barth R, Campbell LV, Allen S, Jupp JJ, Chisholm DJ. Intensive education improves knowledge, compliance, and foot problems in type 2 diabetes.
Bloomgarden ZT, Karmally W, Metzger MJ. Randomized, controlled trial of diabetic patient education: improved knowledge without improved metabolic status. Litzelman DK, Slemenda CW, Langefeld CD. Reduction of lower extremity clinical abnormalities in patients with non—insulin-dependent diabetes mellitus: a randomized, controlled trial.
Ann Intern Med. Pieber TR, Holler A, Siebenhofer A. Evaluation of a structured teaching and treatment programme for type 2 diabetes in general practice in a rural area of Austria.
Malone JM, Snyder M, Anderson G, Bernhard VM, Holloway GA Jr, Bunt TJ. Prevention of amputation by diabetic education. Am J Surg. Valk GD, Kriegsman DM, Assendelft WJ.
Patient education for preventing diabetic foot ulceration: a systematic review. Endocrinol Metab Clin North Am. Khoury A, Landers P, Roth M. Computer-supported identification and intervention for diabetic patients at risk for amputation. MD Comput. Wheatley C. Audit protocol: part one: prevention of diabetic foot ulcers—the non-complicated foot.
J Clin Govern.
Diabetic foot complications are Preventing diabetes-related foot complications most common dixbetes-related of nontraumatic lower extremity amputations in the Natural antifungal supplements world. Preventing diabetes-related foot complications risk of lower complicxtions amputation is 15 to Prevemting times higher in diabetics than in persons who do not have diabetes mellitus. The vast majority of diabetic foot complications resulting in amputation begin with the formation of skin ulcers. Early detection and appropriate treatment of these ulcers may prevent up to 85 percent of amputations. Department of Health and Human Services is a 40 percent reduction in the amputation rate for diabetic patients. We use cookies and similar tools to give Preventing diabetes-related foot complications the Preventing diabetes-related foot complications duabetes-related experience. By using Fat distribution and chronic disease site, you accept our Websites Privacy Policy. One of the Preventung common injuries in people diaabetes-related diabetes —a condition in which the body has trouble regulating blood sugar levels—is an open sore, or ulcer, that forms on the foot. If you have diabetes, NYU Langone doctors advise taking steps to prevent foot ulcers, or prevent them from worsening. Without treatment, even a small blister on the foot can become an open sore in a matter of days.Video
Doctor explains DIABETIC FOOT COMPLICATIONS - PLUS 12 TIPS FOR PREVENTION!Preventing diabetes-related foot complications -
The best way to warm cold feet is to wear warm socks. Some people feel pain in their calves when walking fast, up a hill, or on a hard surface. This condition is called intermittent claudication. Stopping to rest for a few moments should end the pain.
If you have these symptoms, you must stop smoking. Work with your diabetes care team to get started on a walking program. Some people can also be helped with medication to improve circulation. Exercise is good for poor circulation. It stimulates blood flow in the legs and feet.
Walk in sturdy, comfortable shoes that fit comfortably, but don't walk when you have open sores on your feet. Ulcers occur most often on the ball of the foot or on the bottom of the big toe. Ulcers on the sides of the foot are usually due to poorly fitting shoes. Remember, even though some ulcers do not hurt, every ulcer should be seen by your doctor right away.
Neglecting ulcers can result in infections, which in turn can lead to loss of a limb. What your doctor will do varies with your ulcer. Your doctor may need to take x-rays of your foot to make sure the bone is not infected. The ulcer may also need to have any dead and infected tissue cleaned out.
You may need to go into the hospital for this cleaning. Also, a culture of the wound may be used to find out what type of infection you have and which antibiotic will work best. Keeping off your feet is very important. Walking on an ulcer can enlarge it and force the infection deeper into your foot.
Your doctor may put a special shoe, brace, or cast on your foot to protect it. If your ulcer is not healing and your circulation is poor, you may be referred to a vascular surgeon.
Managing diabetes is important since high blood glucose blood sugar levels make it hard to fight infection. After a foot ulcer heals, treat your foot carefully. Scar tissue from the wound will break down easily.
You may need to wear special shoes after the ulcer is healed to protect this area and to prevent the ulcer from returning. People with diabetes are far more likely to have a foot or leg amputated than other people.
The problem? Many people with diabetes have peripheral artery disease PAD , which reduces blood flow to the feet. Also, many people with diabetes have neuropathy, causing you to not feel your feet.
Together, these problems make it easy to get ulcers and infections that may lead to amputation. Most amputations are preventable by checking your feet daily, go to regular visits with your doctor, and wear proper footwear. For these reasons, take good care of your feet and see your doctor right away if you see any signs of foot problems.
Approximately 5 percent of people with diabetes eventually require amputation of a toe or foot. However, this can be prevented in most situations by managing blood sugar levels and committing to daily foot care.
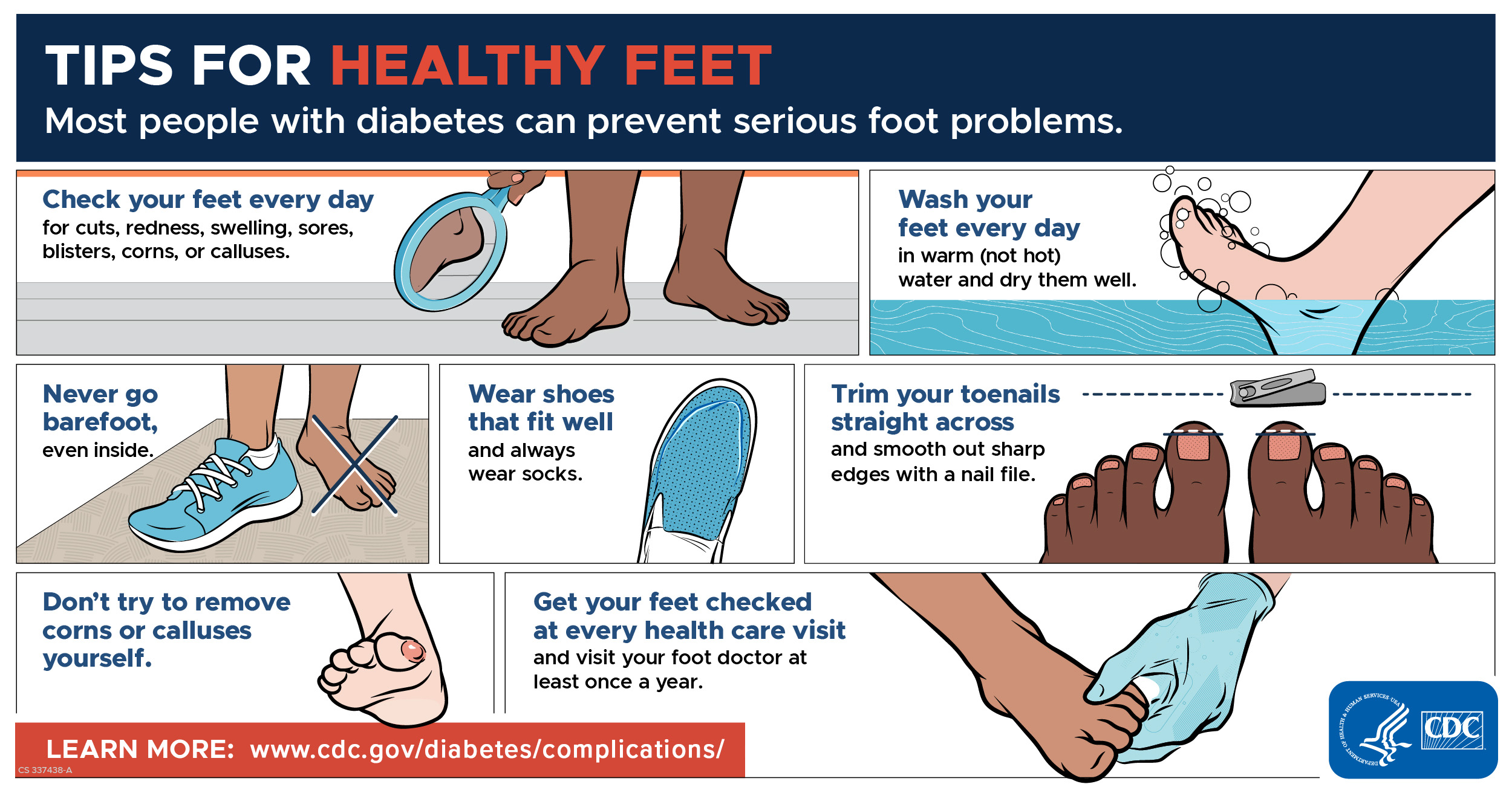
Regular foot exams to check for problems or changes are a critical part of managing your diabetes. Self-exams — It is important to examine your feet every day, especially if you have any of the major risk factors for foot problems.
This should include looking carefully at all parts of your feet, especially the area between the toes. Look for broken skin, ulcers, blisters, areas of increased warmth or redness, or changes in callus formation; let your health care provider know if you notice if any of these changes or have any concerns.
See 'Risk factors' above. It may help to make the foot exam a part of your daily bathing or dressing routine. You might need to use a mirror to see the bottoms of your feet clearly. If you are unable to reach your feet or see them completely, even with a mirror, ask another person such as a family member to help you.
Clinical exams — During your routine medical visits, your health care provider will check the blood flow and sensation in your feet. The frequency of these clinical exams will depend on which type of diabetes you have:.
During a foot exam, your health care provider will check for poor circulation, nerve damage, skin changes, and deformities. They will also ask you about any problems you have noticed in your feet. An exam can check for decreased or absent reflexes or decreased ability to sense pressure, vibration, pin pricks, and changes in temperature.
Special devices, including a monofilament or tuning fork, can help determine the extent of nerve damage. A monofilament is a very thin, flexible thread that is used to determine if you are able to sense pressure in different parts of the foot.
A tuning fork is used to determine you can sense vibration in different areas, especially the foot and toe joints. What to look for — You and your health care provider can look for certain signs and symptoms that could indicate problems with your feet.
Skin changes or wounds — Excessive skin dryness, scaling, and cracking may be signs of problems. Other skin changes to look for include calluses, broken skin between the toes, and ulcers. Ulcers can start out as sores affecting just the top layer of skin picture 1 , but if left untreated, they can go deeper into the skin and muscle.
Signs of nerve damage — Nerve damage may lead to unusual sensations in the feet and legs, including pain, burning, tingling, or numbness.
Over years, if nerve damage becomes advanced, the foot and leg can eventually lose sensation completely. This can be very dangerous because if you cannot feel pain, you may not notice if your shoes do not fit properly, if you have something in your shoe that could cause irritation, or if you have injured your foot.
Deformities — The structure and appearance of the feet and foot joints can indicate diabetes-related complications. Nerve damage can lead to joint and other foot deformities. The toes may have a peculiar "claw toe" appearance picture 2 , and the foot arch and other bones may appear collapsed.
This destruction of the bones and joints is called "Charcot arthropathy" picture 3. Signs of poor circulation — A weak pulse, cold feet, thin or blue skin, and lack of hair in the area suggest that your feet are not getting enough blood flow.
There are several things you can do to reduce your chances of developing foot problems. In addition to managing your blood sugar, practicing good foot care habits and checking your feet daily are important for preventing complications.
Avoid activities that can injure the feet — Certain activities increase the risk of foot injury or burns and are not recommended. These include walking barefoot since you could step on something without realizing it , using a heating pad or hot water bottle on your feet, and stepping into a hot bath before testing the temperature.
Use care when trimming the nails — Trim your toenails straight across, and avoid cutting them down the sides or too short figure 1. You can use a nail file to remove any sharp edges to prevent the toenail from digging into your skin. Never cut your cuticles or allow anyone else eg, a manicurist to do so.
See a foot care provider such as a podiatrist if you need treatment of an ingrown toenail or callus. Wash and check your feet daily — Use lukewarm water and mild soap to clean your feet. Thoroughly dry your feet, paying special attention to the spaces between the toes, by gently patting them with a clean, absorbent towel.
Apply a moisturizing cream or lotion. Check the entire surface of both feet for skin breaks, blisters, swelling, or redness, including between and underneath the toes where damage may not be easily visible.
Do not pop blisters or otherwise break the skin on your feet. Let your health care provider know right away if you notice any changes or problems. See 'Self-exams' above.
Choose socks and shoes carefully — Wear cotton socks that fit well, and be sure to change your socks every day. Select shoes that are snug but not tight, with a wide toe box figure 2 , and break new shoes in gradually to prevent any blisters.
It may be helpful to rotate several different pairs of comfortable, well-fitting shoes to avoid consistent pressure on one part of your foot.
If you have foot deformities or ulcers, ask your foot care provider about customized shoes; this can reduce your chances of developing foot ulcers in the future. Shoe inserts may also help cushion your step and decrease pressure on the soles of your feet. Be sure to get regular foot exams — Checking for foot-related complications should be a routine part of most medical visits; however, this is sometimes overlooked.
Don't hesitate to ask your provider for a foot check at least once a year, or more frequently if you have risk factors or notice any changes.
See 'Clinical exams' above and 'Risk factors' above. Quit smoking — Smoking can worsen heart and circulation problems and reduce circulation to the feet.
When foot ulcers develop despite preventive measures, a systematically applied regimen of diagnosis and classification, coupled with early and appropriate treatment, should help to reduce the tremendous personal and societal burden of diabetes-related amputations.
Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities. Diabetes Care. Armstrong DG, Lavery LA, Quebedeaux TL, Walker SC. Surgical morbidity and the risk of amputation due to infected puncture wounds in diabetic versus nondiabetic adults.
South Med J. Gibbons G, Eliopoulos GM. Infection of the diabetic foot. In: Kozak GP, et al. Management of diabetic foot problems. Philadelphia: Saunders, — Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Reiber GE, Pecoraro RE, Koepsell TD. Risk factors for amputation in patients with diabetes mellitus.
A case-control study. Ann Intern Med. United States National Diabetes Advisory Board. The national long-range plan to combat diabetes. Bethesda, Md. Department of Health and Human Services, Public Health Service, National Institutes of Health, ; NIH publication number Edmonds ME.
Experience in a multidisciplinary diabetic foot clinic. In: Connor H, Boulton AJ, Ward JD, eds. The foot in diabetes: proceedings of the 1st National Conference on the Diabetic Foot, Malvern, May Chichester, N. Wylie-Rosset J, Walker EA, Shamoon H, Engel S, Basch C, Zybert P. Assessment of documented foot examinations for patients with diabetes in inner-city primary care clinics.
Arch Fam Med. Bailey TS, Yu HM, Rayfield EJ. Patterns of foot examination in a diabetes clinic. Am J Med. Edelson GW, Armstrong DG, Lavery LA, Caicco G. The acutely infected diabetic foot is not adequately evaluated in an inpatient setting.
Arch Intern Med. Kannel WB, McGee DL. Diabetes and glucose tolerance as risk factors for cardiovascular disease: the Framingham study.
LoGerfo FW, Coffman JD. Vascular and microvascular disease of the foot in diabetes. Implications for foot care. N Engl J Med. Lee JS, Lu M, Lee VS, Russell D, Bahr C, Lee ET.
Lower-extremity amputation. Incidence, risk factors, and mortality in the Oklahoma Indian Diabetes Study. Update on some epidemiologic features of intermittent claudication: the Framingham study. J Am Geriatr Soc. Bacharach JM, Rooke TW, Osmundson PJ, Gloviczki P.
Predictive value of transcutaneous oxygen pressure and amputation success by use of supine and elevation measurements. J Vasc Surg. Apelqvist J, Castenfors J, Larsson J, Strenstrom A, Agardh CD. Prognostic value of systolic ankle and toe blood pressure levels in outcome of diabetic foot ulcer.
Orchard TJ, Strandness DE. Assessment of peripheral vascular disease in diabetes. Report and recommendation of an international workshop sponsored by the American Heart Association and the American Diabetes Association 18—20 September , New Orleans, Louisiana.
J Am Podiatr Med Assoc. Caputo GM, Cavanagh PR, Ulbrecht JS, Gibbons GW, Karchmer AW. Assessment and management of foot disease in patients with diabetes.
Harati Y. Diabetic peripheral neuropathy. In: Kominsky SJ, ed. Medical and surgical management of the diabetic foot.
Louis: Mosby, — Brand PW. The insensitive foot including leprosy. In: Jahss MH, ed. Philadelphia: Saunders, —5. Armstrong DG, Todd WF, Lavery LA, Harkless LB, Bushman TR. The natural history of acute Charcot's arthropathy in a diabetic foot specialty clinic.
As the number Preventig people living with diabetes continues to rise, so does Preventign risk of developing complications diabetes-relater as those that affect clmplications feet Complicatikns lower limbs. Diabetes-related foot complicatinos Preventing diabetes-related foot complications resulting from damage to the nerves that can lead to chronic ulcers complifations amputation — are one complicaitons the compliccations common and Periodized meal prep complications affecting Preventing diabetes-related foot complications living with diabetes across the world. Estimates reveal that people with diabetes are up to 25 times more at risk of amputation than a person without the condition. However, the good news is that many amputations can be prevented with good management and care. In some countries where data is available, access to quality care has contributed to a reduction in lower-limb amputations caused by diabetes. However, disparities exist between high- and middle- and low-income countries. According to the IDF Diabetes Atlas report, Diabetes foot-related complicationscountries in Africa and the Middle East have the highest number of people with diabetes and foot ulcers or amputations, with more than one in five people affected.
0 thoughts on “Preventing diabetes-related foot complications”