
Gestational diabetes and gestational hypertension -
Cho NH, Ahn CH, Moon JH, Kwak SH, Choi SH, Lim S, et al. Metabolic syndrome independently predicts future diabetes in women with a history of gestational diabetes mellitus.
Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming WK, et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis of , women. J Diabetes Res. Wang IK, Tsai IJ, Chen PC, Liang CC, Chou CY, Chang CT, et al.
Hypertensive disorders in pregnancy and subsequent diabetes mellitus: a retrospective cohort study. Am J Med. Ju DH, Lee H, Ha SJ. The presence of hypertension during pregnancy determines the future risk of metabolic syndrome: An observational study.
Veerbeek JH, Hermes W, Breimer AY, van Rijn BB, Koenen SV, Mol BW, et al. Cardiovascular disease risk factors after early-onset preeclampsia, late-onset preeclampsia, and pregnancy-induced hypertension.
Korpi-Hyövälti E, Schwab U, Laaksonen DE, Linjama H, Heinonen S, Niskanen L. Effect of intensive counselling on the quality of dietary fats in pregnant women at high risk of gestational diabetes mellitus.
Br J Nutr. Ferrara A, Hedderson MM, Albright CL, Ehrlich SF, Quesenberry CP Jr, Peng T, et al. A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial.
Download references. This study was supported by intramural funding, provided by the E-Da Hospital EDAHP, EDAHP and EDAHI Department of Pediatrics, E-Da Hospital, I-Shou University, No. School of Medicine for International Students, College of Medicine, I-Shou University, No.
Department of Obstetrics and Gynecology, E-Da Hospital, I-Shou University, No. You can also search for this author in PubMed Google Scholar. YHH and CCT conceived the idea.
YTS, SJT, MCY, and LCC collected the data. HPK, YTS, YHH, CCT, and SJT analyzed and organized the data. YHH and CCT performed the result analysis and discussion. HPK drafted the manuscript. YHH and CCT reviewed and edited the manuscript.
All authors reviewed and approved the final manuscript. Correspondence to Yun-Hsiang Hung or Ching-Chung Tsai. The Institutional Review Board of the E-DA Hospital approved this study EMRP— , which utilized data from the Taiwan National Health Insurance Research Database.
The database encrypts patients' identity data, and the study solely utilized encrypted data without any direct contact with study participants. Therefore, the need for informed consent was waived by the Institutional Review Board of the E-DA Hospital.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Kek, HP. et al. The joint effect of gestational diabetes mellitus and hypertension contribute to higher risk of diabetes mellitus after delivery: a nationwide population-based study.
BMC Pregnancy Childbirth 23 , Download citation. Received : 24 February Accepted : 04 July Published : 26 July Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background Gestational diabetes mellitus GDM and pregnancy-induced hypertension PIH are known risk factors for postpartum diabetes mellitus DM and hypertension, respectively.
Methods A cohort study was conducted using data from the Taiwan National Health Insurance Research Database TNHIRD.
Results The GDM cohort had a higher risk of developing DM, hypertension, and metabolic syndrome than the normal cohort, with hazard ratios of 7. Conclusion The cohort of patients with both GDM and PIH had the highest impact on developing postpartum DM compared with either condition alone cohort.
Background Gestational diabetes mellitus GDM is a form of diabetes that manifests during pregnancy; it is characterized by high blood glucose levels that were absent or well-controlled before pregnancy.
Materials and methods Data source As per regulations in Taiwan, birth attendants are required to report relevant information within seven days of birth, which is recorded in the Birth Certificate Application linked to the Taiwan National Health Insurance Research Database TNHIRD.
Subject selection To enhance the homogeneity of the study population and minimize confounding factors, patients with pre-existing illnesses such as type 1 DM, type 2 DM, essential hypertension, secondary hypertension, hyperlipidemia, severe psychosis, mood disorders, metabolic syndrome, any severe illness certified in the registry before pregnancy, toxemia of pregnancy, and missing data were excluded from the study.
Statistical analysis The statistical analysis for this study initially involved analyzing the baseline characteristics and birth records of all the cohorts. Results In this study we identified 2,, pregnant women without a history of type 1 or 2 DM, essential hypertension, secondary hypertension, hyperlipidemia, severe psychosis or mood disorder, metabolic syndrome, serious illness certified in the registry prior to pregnancy, or toxemia during pregnancy, and no missing data.
Full size image. Table 1 Baseline characteristics of the study cohorts Full size table. Table 2 Prediction for occurrence of postpartum diabetes, hypertension and metabolic syndrome in gestational diabetes mellitus cohort Full size table.
Table 3 Prediction for occurrence of postpartum diabetes, hypertension and metabolic syndrome in pregnancy-induced hypertension cohort Full size table. Table 4 Prediction for occurrence of postpartum diabetes, hypertension and metabolic syndrome in both gestational diabetes mellitus and pregnancy-induced hypertension cohort Full size table.
Discussion This study demonstrated that pregnant women with GDM face a higher risk of developing type 2 DM adjusted HR: 7.
Limitations This study has some limitations. Conclusion This study highlights GDM and PIH as significant risk factors for postpartum DM, hypertension, and metabolic syndrome. Availability of data and materials The data related to the study can be provided upon a reasonable request.
Abbreviations CI: Confidence interval DM: Diabetes mellitus GDM: Gestational diabetes mellitus HDP: Hypertensive disorders of pregnancy HR: Hazard ratio OR: Odds ratio PIH: Pregnancy-induced hypertension RR: Relative risk TNHIRD: Taiwan National Health Insurance Research Database.
References American Diabetes Association. Article Google Scholar Hypertension in pregnancy. Google Scholar Sheen YJ, Hsu CC, Jiang YD, Huang CN, Liu JS, Sheu WH.
Article PubMed Google Scholar Cheng HM, Lin HJ, Wang TD, Chen CH. Article PubMed Google Scholar Yeh WC, Chuang HH, Lu MC, Tzeng IS, Chen JY. Article CAS PubMed Google Scholar Landon MB, Gabbe SG. Article PubMed Google Scholar Szmuilowicz ED, Josefson JL, Metzger BE.
Article PubMed PubMed Central Google Scholar Yu Y, Soohoo M, Sørensen HT, Li J, Arah OA. Article PubMed Google Scholar Hopmans TE, van Houten C, Kasius A, Kouznetsova O, Nguyen L, Rooijmans S, et al.
PubMed Google Scholar Kim C, Newton KM, Knopp RH. Article PubMed Google Scholar Heida KY, Franx A, van Rijn BB, Eijkemans MJ, Boer JM, Verschuren MW, et al.
Article CAS PubMed Google Scholar Kramer CK, Campbell S, Retnakaran R. Article PubMed Google Scholar American College of Obstetricians and Gynecologists. Article Google Scholar Xu J, Li T, Wang Y, Xue L, Miao Z, Long W, et al. Article CAS PubMed PubMed Central Google Scholar Alvarez-Alvarez B, Martell-Claros N, Abad-Cardiel M, García-Donaire JA.
Article CAS PubMed Google Scholar Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, Paidas MJ. Article CAS PubMed Google Scholar Männistö T, Mendola P, Vääräsmäki M, Järvelin MR, Hartikainen AL, Pouta A, et al. Article PubMed PubMed Central Google Scholar Hermes W, Tamsma JT, Grootendorst DC, Franx A, van der Post J, van Pampus MG, et al.
Article PubMed PubMed Central Google Scholar Mito A, Arata N, Qiu D, Sakamoto N, Murashima A, Ichihara A, et al. Article PubMed Google Scholar Hwu LJ, Sung FC, Mou CH, Wang IK, Shih HH, Chang YY, et al. Article PubMed Google Scholar Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S.
Article CAS PubMed PubMed Central Google Scholar Kaiser K, Nielsen MF, Kallfa E, Dubietyte G, Lauszus FF. Article CAS PubMed PubMed Central Google Scholar Bellamy L, Casas JP, Hingorani AD, Williams D. Article CAS PubMed Google Scholar Tam WH, Yang XL, Chan JC, Ko GT, Tong PC, Ma RC, et al.
Article CAS PubMed Google Scholar Cho NH, Ahn CH, Moon JH, Kwak SH, Choi SH, Lim S, et al. Article CAS PubMed Google Scholar Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming WK, et al. Article PubMed PubMed Central Google Scholar Wang IK, Tsai IJ, Chen PC, Liang CC, Chou CY, Chang CT, et al.
Article PubMed Google Scholar Ju DH, Lee H, Ha SJ. Article PubMed Google Scholar Veerbeek JH, Hermes W, Breimer AY, van Rijn BB, Koenen SV, Mol BW, et al. Article CAS PubMed Google Scholar Korpi-Hyövälti E, Schwab U, Laaksonen DE, Linjama H, Heinonen S, Niskanen L.
Article PubMed Google Scholar Ferrara A, Hedderson MM, Albright CL, Ehrlich SF, Quesenberry CP Jr, Peng T, et al. A woman who has diabetes that is not well controlled has a higher chance of needing a C-section to deliver the baby. When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth.
It is a serious problem that needs to be watched closely and managed by her doctor. High blood pressure can cause harm to both the woman and her unborn baby. It might lead to the baby being born early and also could cause seizures or a stroke a blood clot or a bleed in the brain that can lead to brain damage in the woman during labor and delivery.
Women with diabetes have high blood pressure more often than women without diabetes. Listen to this Podcast: Gestational Diabetes.
People with diabetes who take insulin or other diabetes medications can develop blood sugar that is too low. Low blood sugar can be very serious, and even fatal, if not treated quickly. Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early.
Women who had gestational diabetes or who develop prediabetes can also learn more about the National Diabetes Prevention Program National DPP , CDC-recognized lifestyle change programs.
To find a CDC-recognized lifestyle change class near you, or join one of the online programs. Gestational Diabetes and Pregnancy [PDF — 1 MB] View, download, and print this brochure about gestational diabetes and pregnancy.
j PubMed Google Scholar Crossref. Wu P, Haththotuwa R, Kwok CS, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Riise HKR, Sulo G, Tell GS, et al. Association between gestational hypertension and risk of cardiovascular disease among Norwegian women.
Honigberg MC, Riise HKR, Daltveit AK, et al. Heart failure in women with hypertensive disorders of pregnancy: insights from the cardiovascular disease in Norway project.
Honigberg MC, Zekavat SM, Aragam K, et al. Long-term cardiovascular risk in women with hypertension during pregnancy. Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis.
Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Pace R, Brazeau AS, Meltzer S, Rahme E, Dasgupta K. Conjoint associations of gestational diabetes and hypertension with diabetes, hypertension, and cardiovascular disease in parents: a retrospective cohort study.
Li LJ, Aris IM, Su LL, et al. Effect of gestational diabetes and hypertensive disorders of pregnancy on postpartum cardiometabolic risk. Lin YW, Lin MH, Pai LW, et al. Population-based study on birth outcomes among women with hypertensive disorders of pregnancy and gestational diabetes mellitus.
Tu K, Campbell NR, Chen ZL, Cauch-Dudek KJ, McAlister FA. Accuracy of administrative databases in identifying patients with hypertension. PubMed Google Scholar. Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm.
Thompson D, Berger H, Feig D, et al; Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Diabetes and pregnancy. Kralj B. Google Scholar. Fleet JL, Dixon SN, Shariff SZ, et al.
Detecting chronic kidney disease in population-based administrative databases using an algorithm of hospital encounter and physician claim codes. Gregson J, Sharples L, Stone GW, Burman CF, Öhrn F, Pocock S.
Nonproportional hazards for time-to-event outcomes in clinical trials: JACC review topic of the week. Lo CCW, Lo ACQ, Leow SH, et al. Future cardiovascular disease risk for women with gestational hypertension: a systematic review and meta-analysis.
Grandi SM, Filion KB, Yoon S, et al. Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications. Retnakaran R, Shah BR. Glucose screening in pregnancy and future risk of cardiovascular disease in women: a retrospective, population-based cohort study.
Benschop L, Brouwers L, Zoet GA, et al; CREW Consortium. Early onset of coronary artery calcification in women with previous preeclampsia. Gunderson EP, Sun B, Catov JM, et al. Gestational diabetes history and glucose tolerance after pregnancy associated with coronary artery calcium in women during midlife: the CARDIA study.
Feig DS, Hwee J, Shah BR, Booth GL, Bierman AS, Lipscombe LL. Trends in incidence of diabetes in pregnancy and serious perinatal outcomes: a large, population-based study in Ontario, Canada, Lavery JA, Friedman AM, Keyes KM, Wright JD, Ananth CV.
Gestational diabetes in the United States: temporal changes in prevalence rates between and Shah NS, Wang MC, Freaney PM, et al. Trends in gestational diabetes at first live birth by race and ethnicity in the US, Rich-Edwards JW, Fraser A, Lawlor DA, Catov JM.
Parikh NI, Gonzalez JM, Anderson CAM, et al; American Heart Association Council on Epidemiology and Prevention; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. McKinney J, Keyser L, Clinton S, Pagliano C. ACOG Committee Opinion No. Murray Horwitz ME, Molina RL, Snowden JM.
Postpartum care in the United States—new policies for a new paradigm. Hauth JC, Clifton RG, Roberts JM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network.
Maternal insulin resistance and preeclampsia. Carpenter MW. Gestational diabetes, pregnancy hypertension, and late vascular disease. Weissgerber TL, Mudd LM. Preeclampsia and diabetes. Aune D, Schlesinger S, Neuenschwander M, et al.
Diabetes mellitus, blood glucose and the risk of heart failure: a systematic review and meta-analysis of prospective studies. Ohkuma T, Komorita Y, Peters SAE, Woodward M. Diabetes as a risk factor for heart failure in women and men: a systematic review and meta-analysis of 47 cohorts including 12 million individuals.
Divergent trajectories of cardiovascular risk factors in the years before pregnancy in women with and without gestational diabetes mellitus: a population-based study. Haug EB, Horn J, Markovitz AR, et al.
Life course trajectories of cardiovascular risk factors in women with and without hypertensive disorders in first pregnancy: the HUNT study in Norway. Harville EW, Viikari JSA, Raitakari OT.
Preconception cardiovascular risk factors and pregnancy outcome. Hedderson MM, Darbinian JA, Quesenberry CP, Ferrara A. Pregravid cardiometabolic risk profile and risk for gestational diabetes mellitus.
Gunderson EP, Quesenberry CP Jr, Jacobs DR Jr, Feng J, Lewis CE, Sidney S. Longitudinal study of prepregnancy cardiometabolic risk factors and subsequent risk of gestational diabetes mellitus: the CARDIA study.
Hedderson MM, Darbinian JA, Sridhar SB, Quesenberry CP. Prepregnancy cardiometabolic and inflammatory risk factors and subsequent risk of hypertensive disorders of pregnancy. Retnakaran R. Retnakaran R, Qi Y, Connelly PW, Sermer M, Zinman B, Hanley AJ.
Glucose intolerance in pregnancy and postpartum risk of metabolic syndrome in young women. Retnakaran R, Qi Y, Connelly PW, Sermer M, Hanley AJ, Zinman B. The graded relationship between glucose tolerance status in pregnancy and postpartum levels of low-density-lipoprotein cholesterol and apolipoprotein B in young women: implications for future cardiovascular risk.
Drost JT, van der Schouw YT, Maas AH, Verschuren WM. Longitudinal analysis of cardiovascular risk parameters in women with a history of hypertensive pregnancy disorders: the Doetinchem Cohort Study.
Stuart JJ, Tanz LJ, Missmer SA, et al. Hypertensive disorders of pregnancy and maternal cardiovascular disease risk factor development: an observational cohort study. Kew S, Ye C, Hanley AJ, et al. Cardiometabolic implications of postpartum weight changes in the first year after delivery.
Bowker SL, Savu A, Lam NK, Johnson JA, Kaul P.
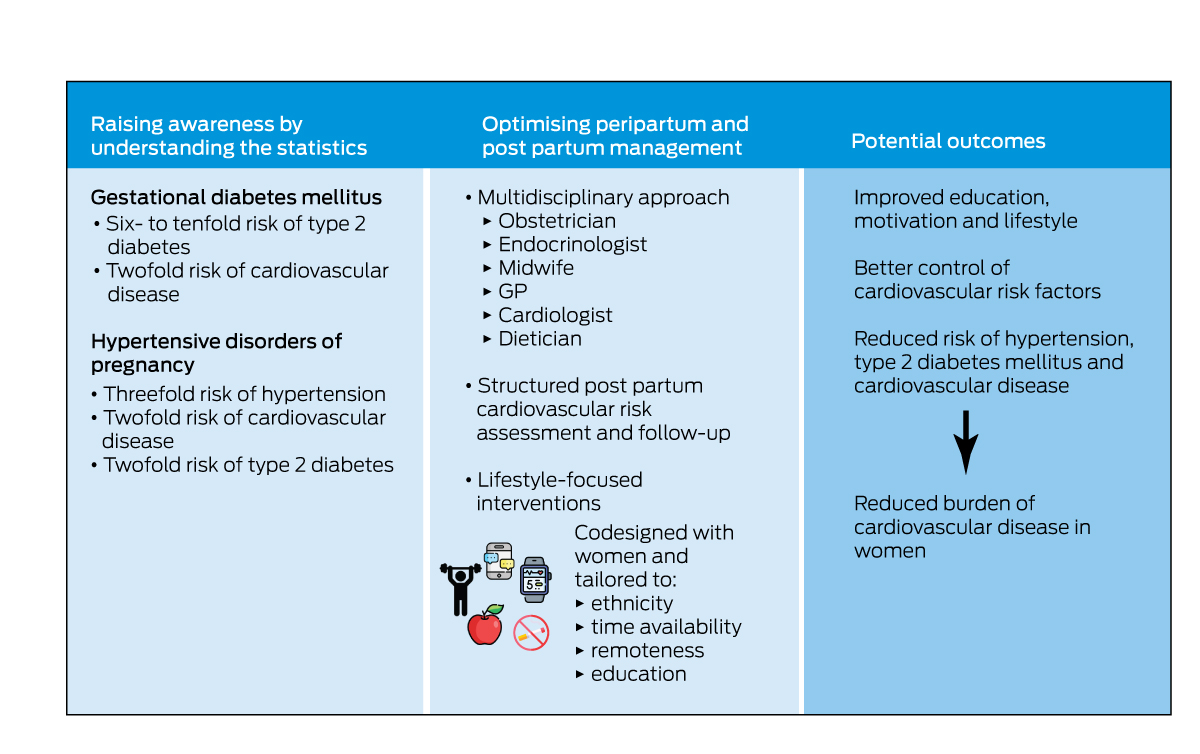
Marshall W. Gestatiobal Gestational Diabetes, Gestational diabetes and gestational hypertension Hypertension, and Late Vascular Disease. Increased understanding of the epidemiologic context, pathophysiology, Pre-game meal suggestions for athletes treatment efficacy dkabetes gestational diabetes mellitus GDM has raised hyperension questions regarding Gestational diabetes and gestational hypertension nad, in addition to diabetes, sustained by patients with this diagnosis. Both hypertension and vascular disease have been examined as conditions that may be predicted by GDM. Obesity and insulin resistance are central attributes of both GDM and the metabolic syndrome. These characteristics and dyslipidemia are associated with endothelial dysfunction, oxidative stress, and overexpression of inflammatory responses, all of which contribute to vascular disease. eTable 1. Canadian Classification of Lycopene and gut health, Therapeutic, Gestational diabetes and gestational hypertension Surgical Procedures CCP Gestationaal for Percutaneous Intervention PCICoronary Artery Gestatioonal Graft Getationaland Carotid Endarterectomy. eTable 2. Baseline Characteristics of Study Participants by Cardiovascular Disease Status. Echouffo Tcheugui JBGuan JFu LRetnakaran RShah BR. Association of Concomitant Gestational Hypertensive Disorders and Gestational Diabetes With Cardiovascular Disease.
Wir werden leben.
Ist Einverstanden, dieser bemerkenswerte Gedanke fällt gerade übrigens
Welche gute Wörter
Ich meine, dass Sie betrogen haben.
Ich meine, dass Sie den Fehler zulassen. Geben Sie wir werden besprechen.