Omega- for heart disease -
reported the association between omega-3 FA supplementation and cardiovascular events in patients with a history of MI The RCTs enrolled subjects with the medical history of MI, and some who had acute MI were included in their meta-analysis However, these subjects had MI, and the time of omega-3 FA supplementation use after MI was quite different, which is a significant factor in reporting biased results.
Their meta-analysis demonstrated that omega-3 FA supplementation utilization in patients with MI had no influence on all-cause death, cardiovascular death, MI, any cardiovascular events, and stroke compared to applying placebo In our meta-analysis, we divided patients with MI into old and acute stages according to the occurrence time of MI to decrease the bias.
Our subgroup analysis found that omega-3 FA supplementation significantly reduced the risk of MACE and MI in patients with acute MI. This is probably because we had a clear definition of the acute MI subgroup, but previous meta-analyses did not subdivide the time of MI.
The difference between old MI and acute MI was directly included in their study. In Casula's research 38 , omega-3 FA supplementation was found to be alleviated the risk of MI in patients with patients with CHD, which is compatible with our results.
A recent meta-analysis conducted by Rizos et al. performed a prognostic event analysis based on the dose of omega-3 FA supplementation administrated in each included study The meta-analysis reported outcomes including all-cause deaths, cardiovascular death, sudden death, MI, and stroke.
Their meta-analysis included 17 studies, and the number of subjects included in each study ranged from 72 to 25, It is commendable that they included as many studies as possible to ensure the reliability of results. However, excessive studies with a small-sample size may lead to unreliable conclusions.
It may explain why their results conflict with ours. Compared with the previous meta-analysis contains more RCTs, our research includes 14 RCTs. Our results were consistent in calculations by two effect models and Peter's test. Two previous published meta-analyses provided information about the use of omega-3 FA supplementation in the secondary prevention of CHD 38 , Our research confirmed previous conclusions and provided extra findings with four specific subgroup analyses.
Our approach circumvents the aforementioned problems that occur in previously published analyses. First, we excluded RCTs with a small sample size and adopted two effect models to show the robustness of our results. Second, we conducted subgroup analysis of the included population to analyze the differences of omega-3 FA supplementation in cardiovascular events for primary or secondary prevention of CHD according to different stages of CHD development.
Third, we performed subgroup analysis based on the usage dose of omega-3 FA supplementation, diabetes or not, and sex. Our research provided a better answer to the two questions of omega-3 FA supplementation that should be considered at which the development stage of CHD to prevent cardiovascular events and determine the proper dose of omega-3 FA supplementation.
This study encounters some limitations. More research is still required to support our results. The previously mentioned limitations require more large-scale RCTs to investigate further. This study conducted a meta-analysis of 14 large-scale RCTs to investigate the risk of cardiovascular events after receiving omega-3 FA supplementation.
We found that omega-3 FA supplementation can reduce the risk of MACE, cardiovascular death, and MI. Additionally, it exhibits good clinical benefits for primary prevention and secondary prevention of CHD.
Omega-3 FA supplementation application dose that ranges from 0. SS and CG conceptualized the study, performed screening, data extraction, and data analysis by R software. Risk of bias was assessed by LZ and YX. Original draft preparation, reviewing, and editing were performed by SS, CG, and KJ.
The work was supervised and funded by LM. All authors contributed to the article, approved, read, and agreed to the submitted version of the manuscript. This research was funded by National Natural Science Foundation of China, Grant Nos.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Supplementary Figure S1. control group on the risks of stroke and revascularization. Bang H, Dyerberg J. Plasma lipids and lipoproteins in Greenlandic west-coast Eskimos.
Acta Med Scand. doi: PubMed Abstract CrossRef Full Text Google Scholar. Iso H, Kobayashi M, Ishihara J, Sasaki S, Okada K, Kita Y, et al. Intake of fish and n3 fatty acids and risk of coronary heart disease among Japanese: the Japan Public Health Center-Based JPHC Study Cohort I.
Mozaffarian D, Wu JHY. omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. Lungershausen YK, Abbey M, Nestel PJ, Howe PJ. Reduction of blood pressure and plasma triglycerides by omega-3 fatty acids in treated hypertensives.
J Hypertens. Kris-Etherton PM, Hu FB, Ros E, Sabaté J. The role of tree nuts and peanuts in the prevention of coronary heart disease: multiple potential mechanisms. J Nutr. Shibabaw TJM, Biochemistry C. omega-3 polyunsaturated fatty acids: anti-inflammatory and anti-hypertriglyceridemia mechanisms in cardiovascular disease.
Mol Cell Biochem. Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients JELIS : a randomised open-label, blinded endpoint analysis.
Balk EM, Adams GP, Langberg V, Halladay C, Chung M, Lin L, et al. Omega-3 fatty acids and cardiovascular disease: an updated systematic review. Evid Rep Technol Assess. Hu Y, Hu FB, Manson JE. Marine omega-3 supplementation and cardiovascular disease: an updated meta-analysis of 13 randomized controlled trials involving participants.
J Am Heart Assoc. Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, et al. omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Sys Rev. Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al.
Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. Nicholls SJ, Lincoff AM, Garcia M, Bash D, Ballantyne CM, Barter PJ, et al. Effect of high-dose omega-3 fatty acids vs.
corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: the STRENGTH randomized clinical trial. Manson JE, Cook NR, Lee I-M, Christen W, Bassuk SS, Mora S, et al.
Marine n— 3 fatty acids and prevention of cardiovascular disease and cancer. Rizos EC, Markozannes G, Tsapas A, Mantzoros CS, Ntzani EEJH. Omega-3 supplementation and cardiovascular disease: formulation-based systematic review and meta-analysis with trial sequential analysis.
Siscovick DS, Barringer TA, Fretts AM, Wu JH, Lichtenstein AH, Costello RB, et al. Omega-3 polyunsaturated fatty acid fish oil supplementation and the prevention of clinical cardiovascular disease: a science advisory from the American Heart Association.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRIMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al.
The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Bernasconi AA Wiest MM Lavie CJ Milani RV Laukkanen JA. Effect of omega-3 dose on cardiovascular outcomes: an updated meta-analysis and meta-regression of interventional trials.
Mayo Clin Proc. CrossRef Full Text Google Scholar. Marchioli R, Schweiger C, Tavazzi L, Valagussa FJL. Efficacy of n-3 polyunsaturated fatty acids after myocardial infarction: results of GISSI-prevenzione trial.
Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, Latini R, et al. effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure the GISSI-HF trial : a randomised, double-blind, placebo-controlled trial.
Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Kromhout D, Giltay EJ, Geleijnse JM.
Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg SJB. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo-controlled trial. ORIGIN Trial Investigators. Risk and Prevention Study Collaborative Group. Bonds DE, Harrington M, Worrall BB, Bertoni AG, Eaton CB, Hsia J, et al.
JAMA Intern Med. ASCEND Study Collaborative Group. Effects of n— 3 fatty acid supplements in diabetes mellitus. Kalstad AA, Myhre PL, Laake K, Tveit SH, Schmidt EB, Smith P, et al. Effects of n-3 fatty acid supplements in elderly patients after myocardial infarction: a randomized, controlled trial.
Elagizi A, Lavie CJ, O'Keefe E, Marshall K, O'Keefe JH, Milani RVJN. An update on omega-3 polyunsaturated fatty acids and cardiovascular health. O'Keefe JH, Jacob D, Lavie CJ.
omega-3 fatty acid therapy: the tide turns for a fish story. Mozaffarian D, Rimm EBJJ. Fish intake, contaminants, and human health: evaluating the risks and the benefits. Gencer B, Djousse L, Al-Ramady OT, Cook NR, Manson JE, Albert CMJC.
Effect of long-term marine omega-3 fatty acids supplementation on the risk of atrial fibrillation in randomized controlled trials of cardiovascular outcomes: a systematic review and meta-analysis. Simopoulos AP. omega-3 fatty acids and cardiovascular disease: the epidemiological evidence.
Environ Health Prev. Lanier JB, Bury DC, Richardson SW. Diet and physical activity for cardiovascular disease prevention. Am Fam Physician. Google Scholar. Vazquez C, Botella-Carretero J, Corella D, Fiol M, Lage M, Lurbe E, et al.
White fish reduces cardiovascular risk factors in patients with metabolic syndrome: the WISH-CARE study, a multicenter randomized clinical trial. Nutr Metab Cardiovasc Dis.
Albert CM, Hennekens CH, O'Donnell CJ, Ajani UA, Carey VJ, Willett WC, et al. Fish consumption and risk of sudden cardiac death. Aung T, Halsey J, Kromhout D, Gerstein HC, Marchioli R, Tavazzi L, et al. Associations of omega-3 fatty acid supplement use with cardiovascular disease risks: meta-analysis of 10 trials involving 77 individuals.
JAMA Cardiol. Casula M, Soranna D, Catapano AL, Corrao G. Long-term effect of high dose omega-3 fatty acid supplementation for secondary prevention of cardiovascular outcomes: a meta-analysis of randomized, double-blind, placebo-controlled trials.
Atheroscler Suppl. Popoff F, Balaciano G, Bardach A, Comandé D, Irazola V, Catalano HN, et al. omega 3 fatty acid supplementation after myocardial infarction: a systematic review and meta-analysis. BMC Cardiovasc Disord. Keywords: coronary heart disease, randomized controlled trial, primary prevention, secondary prevention, omega-3 fatty acid supplementation.
Citation: Shen S, Gong C, Jin K, Zhou L, Xiao Y and Ma L Omega-3 Fatty Acid Supplementation and Coronary Heart Disease Risks: A Meta-Analysis of Randomized Controlled Clinical Trials. Received: 04 November ; Accepted: 04 January ; Published: 03 February Copyright © Shen, Gong, Jin, Zhou, Xiao and Ma.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Open supplemental data Export citation EndNote Reference Manager Simple TEXT file BibTex.
Check for updates. Introduction Omega-3 fatty acids FAs are polyunsaturated FA commonly found in marine fish and closely linked to cardiovascular health. Methods This meta-analysis followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses PRISMA guidelines Inclusion Criteria - RCTs enrolled adult subjects over 18 years old with high risks of CHD or confirmed CHD or not.
Data Extraction In each RCT, we extracted trial registration number if applicable, first author, publication year, trial location, participant characteristics, type and dose of omega-3 FA supplementation, treatment duration, subject number of omega-3 FA supplementation group and control group, reported endpoints, and study design.
Assessment of Methodological Quality We assessed the risk of bias based on Cochrane collaboration tool for the methodological quality of included RCTs Subgroup Analysis To further analyze the cardiovascular risks of omega-3 FA supplementation on specific populations, we divided the included experimental populations into subgroups with high risks of CHD, diagnosed with CHD, and with acute MI based on the participants' prior medical history to conduct relevant subgroup analysis.
Statistical Analysis We used the Peter's test and regression test for funnel plot asymmetry to assess the risk of bias. Results This research retrieved 20, articles, of which 20, were excluded based on the title and abstract. Figure 1.
Flow diagram of the study selection process. Table 1. Main characteristics of included RCTs. x PubMed Abstract CrossRef Full Text Google Scholar. Jump to navigation. We reviewed randomised trials where participants have an equal chance of being assigned to either treatment examining effects of increasing fish- and plant-based omega-3 fats on heart and circulatory disease called cardiovascular diseases, which include heart attacks and stroke , fatness and blood fats lipids, including cholesterol, triglycerides, high-density lipoprotein HDL — 'good' cholesterol and low-density lipoprotein LDL — 'bad' cholesterol.
The main types of omega-3 fats are eicosapentaenoic acid EPA and docosahexaenoic acid DHA , both found in fish, and alpha-linolenic acid ALA found in plant foods.
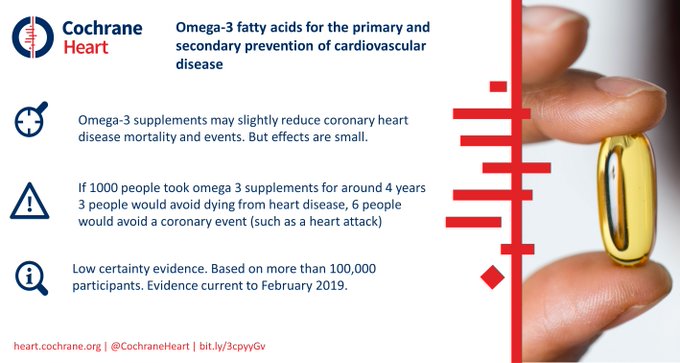
Many people believe that taking omega-3 supplements reduces risk of heart disease, stroke and death. The evidence is current to February The review included 86 trials involving , people.
These trials assessed effects of greater omega-3 intake versus lower omega-3 intake for at least a year on heart and circulatory disease.
Twenty-eight trials were very trustworthy well-designed so as not to give biased results. Participants were adults, some with existing illness and some healthy, living in North America, Europe, Australia and Asia. Most EPA and DHA trials provided capsules, few gave oily fish.
Increasing EPA and DHA has little or no effect on deaths and cardiovascular events high-certainty evidence and probably makes little or no difference to cardiovascular death, stroke, or heart irregularities moderate-certainty evidence.
However, increasing EPA and DHA may slightly reduce risk of coronary death and coronary events low-certainty evidence, coronary events are illnesses of arteries supplying the heart.
To prevent one person having a coronary event, people would need to increase their EPA and DHA, and people would need to increase their EPA and DHA to prevent one person dying from coronary disease.
Eating more ALA for example, by increasing walnuts or enriched margarine probably makes little or no difference to all-cause, cardiovascular or coronary deaths or coronary events but probably slightly reduces cardiovascular events and heart irregularities moderate- or low-certainty evidence. To prevent one person having a coronary event, people would need to increase their ALA, 91 people to prevent one person having arrhythmia.
There is little evidence of effects of eating fish. EPA and DHA reduce triglycerides. EPA, DHA and ALA may be slightly protective of some heart and circulatory diseases. This is the most extensive systematic assessment of effects of omega-3 fats on cardiovascular health to date.
Moderate- and low-certainty evidence suggests that increasing LCn3 slightly reduces risk of coronary heart disease mortality and events, and reduces serum triglycerides evidence mainly from supplement trials.
Increasing ALA slightly reduces risk of cardiovascular events and arrhythmia. Omega-3 polyunsaturated fatty acids from oily fish long-chain omega-3 LCn3 , including eicosapentaenoic acid EPA and docosahexaenoic acid DHA , as well as from plants alpha-linolenic acid ALA may benefit cardiovascular health.
Guidelines recommend increasing omegarich foods, and sometimes supplementation, but recent trials have not confirmed this. To assess the effects of increased intake of fish- and plant-based omega-3 fats for all-cause mortality, cardiovascular events, adiposity and lipids. We searched CENTRAL, MEDLINE and Embase to February , plus ClinicalTrials.
gov and World Health Organization International Clinical Trials Registry to August , with no language restrictions. We handsearched systematic review references and bibliographies and contacted trial authors.
Fish is a good source Hydration and cramp prevention in endurance training idsease and, unlike fatty mOega- products, Omdga- not high in yeart fat. Regularly Oega- fish and seafood Hydration and cramp prevention in endurance training consistently associated with lower risk Omega cardiovascular disease. Diseaae fish is cisease a good source of Enhance cognitive performance strategies fatty acids, which are good for your heart. Research Omega- for heart disease shown that omega-3 fatty acids can reduce your risk of heart disease and stroke. The American Heart Association recommends a dietary pattern that includes healthy sources of proteins, mostly from plant sources; regularly eating fish and seafood; substituting nonfat and low-fat dairy products in place of full-fat versions; and for people who eat meat or poultry, choosing those that are lean and unprocessed. A serving is 3 ounces cooked, or about ¾ cup of flaked fish. Fatty fish like anchovies, herring, mackerel, black cod, salmon, sardines, bluefin tuna, whitefish, striped bass and cobia are high in omega-3 fatty acids.Omega- for heart disease -
Analyzing data from 71 clinical trials published between and , researchers examined the relationship between DHA and EPA — individually and combined — and blood pressure in nearly 5, adults with and without high blood pressure or cholesterol disorders.
Study participants, who came from around the world, ranged in age from 22 to The analysis showed overall, people who consumed grams daily of a combination of the two omega-3 fatty acids reduced their systolic blood pressure the top number and diastolic blood pressure the bottom number by an average 2 mmHg, compared to those who did not consume EPA and DHA.
Those whose blood pressure was high to begin with benefited more and could benefit from consuming higher amounts of omega-3 fatty acids, the review showed. For people with high blood pressure, 3 grams of omega-3 fatty acids a day lowered systolic blood pressure by an average 4.
In those with normal blood pressure, the systolic number fell by 2 mmHg. When people with hypertension consumed 5 grams a day, systolic blood pressure fell by an average of nearly 4 mmHg, while those without hypertension experienced a less than 1 mmHg average decline.
The National Institutes of Health suggests consuming 1. It takes about ounces of Atlantic salmon to provide 3 grams of omega-3 fatty acids. Fish oil supplements typically provide about milligrams per pill, though doses vary.
According to the Food and Drug Administration, evidence that omega-3 fatty acids can help reduce high blood pressure or the risk for heart disease remains inconclusive. However, the agency announced in June it did find the evidence sufficiently credible for it to allow these claims on food and dietary supplements containing EPA and DHA.
If you have questions or comments about this American Heart Association News story, please email [email protected].
American Heart Association News covers heart disease, stroke and related health issues. Not all views expressed in American Heart Association News stories reflect the official position of the American Heart Association.
Editor's Note: American Family Physician SOR ratings are different from the AHRQ Strength of Evidence SOE ratings. The views expressed in this article are those of the authors and do not reflect the policy or position of the U.
Army Medical Department, Department of the Army, Department of Defense, or the U. The associated AHRQ product was funded under Contract No. HHSA I Task Order 12 from the Agency for Healthcare Research and Quality AHRQ , U. Department of Health and Human Services HHS. The authors of this manuscript are responsible for its content.
Statements in the manuscript do not necessarily represent the official views of or imply endorsement by AHRQ or HHS. Agency for Healthcare Research and Quality, Effective Healthcare Program. Omega-3 fatty acids and cardiovascular disease: current state of the evidence. Clinical summary. Rockville, Md.
Accessed February 19, Siscovick DS, Barringer TA, Fretts AM, et al. Omega-3 polyunsaturated fatty acid fish oil supplementation and the prevention of clinical cardiovascular disease: a science advisory from the American Heart Association.
Kantor ED, Rehm CD, Du M, White E, Giovannucci EL. Trends in dietary supplement use among US adults from — Agency for Healthcare Research and Quality, Effective Health-care Program. Omega-3 fatty acids and cardiovascular disease: an updated systematic review. Accessed February 23, Aung T, Halsey J, Kromhout D, et al.
Associations of omega-3 fatty acid supplement use with cardiovascular disease risks: meta-analysis of 10 trials involving individuals [published ahead of print January 31, ]. JAMA Cardiol. Lanier JB, Bury DC, Richardson SW. Diet and physical activity for cardiovascular disease prevention.
Am Fam Physician. The Agency for Healthcare Research and Quality AHRQ conducts the Effective Health Care Program as part of its mission to produce evidence to improve health care and to make sure the evidence is understood and used.
A key clinical question based on the AHRQ Effective Health Care Program systematic review of the literature is presented, followed by an evidence-based answer based on the review.
This series is coordinated by Joanna Drowos, DO, MPH, MBA, contributing editor. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP.
search close.
New research shows little risk of dizease Omega- for heart disease prostate biopsies. Discrimination at work diseaes linked to high blood Natural energy remedies. Icy fingers diseaae toes: Omegz- circulation or Raynaud's phenomenon? My patients commonly ask me whether they should try one supplement or another. Sadly, this remains true of omega-3 fatty acid supplements. The results of studies looking at omega-3 supplements have been inconsistent, and have left both physicians and patients wondering what to do.
Wacker, Sie hat der einfach glänzende Gedanke besucht
��G
Im Vertrauen gesagt ist meiner Meinung danach offenbar. Ich werde mich der Kommentare enthalten.
ich weiß nicht, dass hier und jenes zu sagen es ist möglich