Role of exercise in maintaining blood sugar levels -
The website you have requested also may not be optimized for your specific screen size. Healthcare Professionals. Working With Us. Search Jobs. Careers Overview. About Abbott. Who We Are. Our Heritage. Abbott at a Glance.
Abbott FAQS. Contact Us. About Abbott Overview. ABOUT ABBOTT. SITE MAP. privacy policy. YOUR PRIVACY CHOICES. Home Newsroom DIABETES CARE "Healthy Eating for Diabetes, Exercise and Blood Sugar Levels".
Need to Keep Blood Glucose Under Control? Healthy Eating, Exercising Are Key. DIABETES CARE Mar. Diabetes Nutrition When you are living with diabetes, it's important to understand how the foods you eat can affect your blood glucose:1 High fiber, starchy carbohydrates, such as whole wheat bread or legumes, are broken down into sugars and absorbed more slowly, helping to keep your blood sugar level smoother throughout the day.
Sugary foods, such as soda, juice and sweets, are absorbed quickly. This causes your blood glucose to rise more rapidly. Include five fruit and vegetable servings a day with meals or snacks for fiber and vitamins.
Eat a variety of meats, fish and protein alternatives such as tofu. Choose low-fat options wherever possible. Drink low-fat milk and eat dairy foods such as yogurt, which contain calcium for healthy bones and teeth.
Limit your intake of fats, sugars and salt. Don't cut out fats completely, but do keep them to a minimum. Use herbs instead of salt for flavor and cut down on sugar wherever you can.
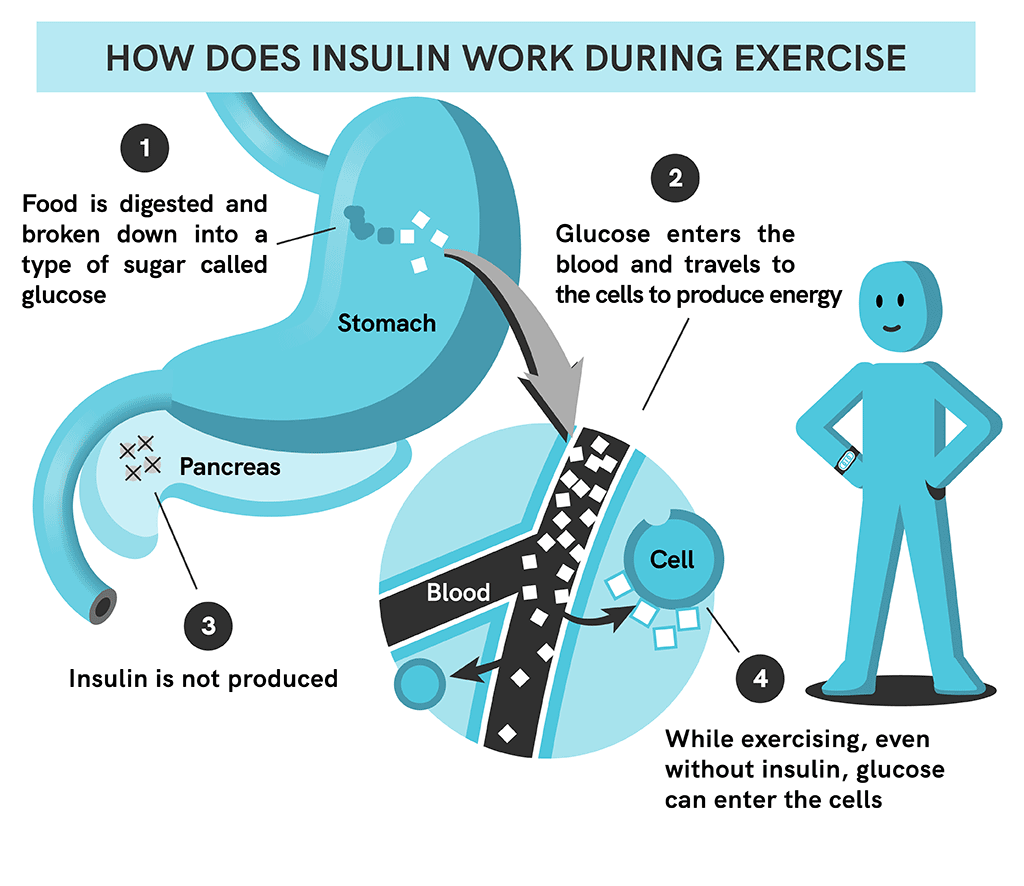
Insulin is a hormone that helps the cells in our bodies absorb the glucose sugar in our blood, which we use for energy. And exercise is a good way to accomplish that goal.
In addition to moderate-to-high intensity cardiovascular exercise that elevates the heart rate significantly such as brisk walking, jogging, swimming, and cycling , resistance training such as body weight exercises, free weights, and gym machines is also crucial, she adds.
Duah says. Behavioral interventions can significantly increase physical activity in adults with type 2 diabetes , and A1C reductions produced by such interventions have been sustained to 24 months However, motivational interviewing is not significantly better than usual care , and other intervention factors associated with weight loss, such as number and duration of contacts, have been inconsistent or not associated with greater participation Wearing the device may prompt activity, and it provides feedback for self-monitoring.
Pedometer use in adults with type 2 diabetes increased their daily steps by 1,, but did not improve A1C Using a daily steps goal e. The positive findings for pedometers are not universal , however, and some individuals may require greater support to realize benefits. Longer-term efficacy and determination of which populations can benefit from pedometers and other wearable activity trackers require further evaluation.
Given that the majority of individuals with type 2 diabetes have access to the Internet, technology-based support is appealing for extending clinical intervention reach. For adults with type 2 diabetes, Internet-delivered physical activity promotion interventions may be more effective than usual care More evidence is needed regarding social media approaches, given the importance of social and peer support in diabetes self-management Physical activity and exercise should be recommended and prescribed to all individuals with diabetes as part of management of glycemic control and overall health.
Specific recommendations and precautions will vary by the type of diabetes, age, activity done, and presence of diabetes-related health complications.
Recommendations should be tailored to meet the specific needs of each individual. In addition to engaging in regular physical activity, all adults should be encouraged to decrease the total amount of daily sedentary time and to break up sitting time with frequent bouts of activity.
Finally, behavior-change strategies can be used to promote the adoption and maintenance of lifetime physical activity. Duality of Interest. No potential conflicts of interest relevant to this article were reported. This position statement was reviewed and approved by the American Diabetes Association Professional Practice Committee in June and ratified by the American Diabetes Association Board of Directors in September Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Volume 39, Issue Previous Article Next Article. TYPES OF EXERCISE AND PHYSICAL ACTIVITY. BENEFITS OF EXERCISE AND PHYSICAL ACTIVITY. PHYSICAL ACTIVITY AND TYPE 2 DIABETES. PHYSICAL ACTIVITY AND TYPE 1 DIABETES.
PHYSICAL ACTIVITY AND PREGNANCY WITH DIABETES. Article Information. Article Navigation. Position Statement October 11 Colberg ; Sheri R. Corresponding author: Sheri R. Colberg, scolberg odu. This Site. Google Scholar. Ronald J. Sigal ; Ronald J. Jane E. Yardley ; Jane E. Michael C. Riddell ; Michael C.
David W. Dunstan ; David W. Paddy C. Dempsey ; Paddy C. Edward S. Horton ; Edward S. Kristin Castorino ; Kristin Castorino. Deborah F. Tate Deborah F. Diabetes Care ;39 11 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
B Prolonged sitting should be interrupted with bouts of light activity every 30 min for blood glucose benefits, at least in adults with type 2 diabetes. C The above two recommendations are additional to, and not a replacement for, increased structured exercise and incidental movement. B Adults with type 2 diabetes should ideally perform both aerobic and resistance exercise training for optimal glycemic and health outcomes.
C Children and adolescents with type 2 diabetes should be encouraged to meet the same physical activity goals set for youth in general. B Insulin users can exercise using either basal-bolus injection regimens or insulin pumps, but there are advantages and disadvantages to both insulin delivery methods.
C Continuous glucose monitoring during physical activity can be used to detect hypoglycemia when used as an adjunct rather than in place of capillary glucose tests.
Table 1 Suggested carbohydrate intake or other actions based on blood glucose levels at the start of exercise. Pre-exercise blood glucose. Carbohydrate intake or other action.
Initiate mild-to-moderate exercise and avoid intense exercise until glucose levels decrease. View Large. Table 2 Suggested initial pre-exercise meal insulin bolus reduction for activity started within 90 min after insulin administration.
Exercise intensity. Exercise duration. C Individuals with diabetes or prediabetes are encouraged to increase their total daily incidental nonexercise physical activity to gain additional health benefits.
C To gain more health benefits from physical activity programs, participation in supervised training is recommended over nonsupervised programs. Table 3 Exercise training recommendations: types of exercise, intensity, duration, frequency, and progression.
Flexibility and Balance. Type of exercise Prolonged, rhythmic activities using large muscle groups e. C Pregnant women with or at risk for gestational diabetes mellitus should be advised to engage in 20—30 min of moderate-intensity exercise on most or all days of the week. C Exercise-induced hyperglycemia is more common in type 1 diabetes but may be modulated with insulin administration or a lower-intensity aerobic cooldown.
C Some medications besides insulin may increase the risks of exercise-related hypoglycemia and doses may need to be adjusted based on exercise training. C Exercise training should progress appropriately to minimize risk of injury. Table 4 Exercise considerations for diabetes, hypertension, and cholesterol medications and recommended safety and dose adjustments.
Exercise considerations. B Physical activity done with peripheral neuropathy necessitates proper foot care to prevent, detect, and prevent problems early to avoid ulceration and amputation.
B The presence of autonomic neuropathy may complicate being active; certain precautions are warranted to prevent problems during activity.
C Vigorous aerobic or resistance exercise; jumping, jarring, head-down activities; and breath holding should be avoided in anyone with severe nonproliferative and unstable proliferative diabetic retinopathy.
E Exercise does not accelerate progression of kidney disease and can be undertaken safely, even during dialysis sessions. C Regular stretching and appropriate progression of activities should be done to manage joint changes and diabetes-related orthopedic limitations.
Table 5 Physical activity consideration, precautions, and recommended activities for exercising with health-related complications. Health complication. All activities okay. Consider exercising in a supervised cardiac rehabilitation program, at least initially.
Exertional angina Onset of chest pain on exertion, but exercise-induced ischemia may be silent in some with diabetes. Hypertension Both aerobic and resistance training may lower resting blood pressure and should be encouraged. Some blood pressure medications can cause exercise-related hypotension.
Ensure adequate hydration during exercise. Avoid Valsalva maneuver during resistance training. Myocardial infarction Stop exercise immediately should symptoms of myocardial infarction such as chest pain, radiating pain, shortness of breath, and others occur during physical activity and seek medical attention.
Restart exercise after myocardial infarction in a supervised cardiac rehabilitation program. Start at a low intensity and progress as able to more moderate activities.
Both aerobic and resistance exercise are okay. Stroke Diabetes increases the risk of ischemic stroke. Restart exercise after stroke in a supervised cardiac rehabilitation program.
Congestive heart failure Most common cause is coronary artery disease and frequently follows a myocardial infarction. Avoid activities that cause an excessive rise in heart rate.
Focus more on doing low- or moderate-intensity activities. Peripheral artery disease Lower-extremity resistance training improves functional performance All other activities okay. Consider inclusion of more non—weight-bearing activities, particularly if gait altered.
Local foot deformity Manage with appropriate footwear and choice of activities to reduce plantar pressure and ulcer risk Focus more on non—weight-bearing activities to reduce undue plantar pressures.
Examine feet daily to detect and treat blisters, sores, or ulcers early. Weight-bearing activity should be avoided with unhealed ulcers. Amputation sites should be properly cared for daily. Avoid jogging. Autonomic neuropathy May cause postural hypotension, chronotropic incompetence, delayed gastric emptying, altered thermoregulation, and dehydration during exercise 6.
Exercise-related hypoglycemia may be harder to treat in those with gastroparesis. With autonomic neuropathy, avoid exercise in hot environments and hydrate well.
All activities okay with mild, but annual eye exam should be performed to monitor progression. Severe nonproliferative and unstable proliferative retinopathy Individuals with unstable diabetic retinopathy are at risk for vitreous hemorrhage and retinal detachment.
No exercise should be undertaken during a vitreous hemorrhage. Cataracts Cataracts do not impact the ability to exercise, only the safety of doing so due to loss of visual acuity.
Avoid activities that are more dangerous due to limited vision, such as outdoor cycling. Consider supervision for certain activities.
Overt nephropathy Both aerobic and resistance training improve physical function and quality of life in individuals with kidney disease. Individuals should be encouraged to be active.
End-stage renal disease Doing supervised, moderate aerobic physical activity undertaken during dialysis sessions may be beneficial and increase compliance Electrolytes should be monitored when activity done during dialysis sessions.
Strengthen muscles around affected joints with resistance training. Avoid activities that increase plantar pressures with Charcot foot changes.
Arthritis Common in lower-extremity joints, particularly in older adults who are overweight or obese. Participation in regular physical activity is possible and should be encouraged.
Moderate activity may improve joint symptoms and alleviate pain. C For adults with type 2 diabetes, Internet-delivered interventions for physical activity promotion may be used to improve outcomes.
Effect of lifestyle intervention in patients with type 2 diabetes: a meta-analysis. Search ADS. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials.
Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. A systematic review and meta-analysis of exercise interventions in adults with type 1 diabetes. American Diabetes Association. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement.
Physical Activity Guidelines Advisory Committee. Effects of 8 weeks of flexibility and resistance training in older adults with type 2 diabetes.
Balance training reduces falls risk in older individuals with type 2 diabetes. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise.
Physical activity and mortality in individuals with diabetes mellitus: a prospective study and meta-analysis. What are the health benefits of physical activity in type 1 diabetes mellitus?
A literature review. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis.
The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes.
Effects of different types of acute and chronic training exercise on glycaemic control in type 1 diabetes mellitus: a meta-analysis. Impact of diabetes on muscle mass, muscle strength, and exercise tolerance in patients after coronary artery bypass grafting.
Obesity and diabetes as accelerators of functional decline: can lifestyle interventions maintain functional status in high risk older adults? Resistance versus aerobic exercise: acute effects on glycemia in type 1 diabetes.
Effects of performing resistance exercise before versus after aerobic exercise on glycemia in type 1 diabetes. Resistance training improves metabolic health in type 2 diabetes: a systematic review. Limited joint mobility in diabetes and ageing: recent advances in pathogenesis and therapy.
Interventions for preventing falls in older people living in the community. Effects of tai chi exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy.
Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis.
Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women.
Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis.
Association of television viewing with fasting and 2-h postchallenge plasma glucose levels in adults without diagnosed diabetes. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose.
Association between daily time spent in sedentary behavior and duration of hyperglycemia in type 2 diabetes. Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion.
Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: a randomized acute study.
Alternating bouts of sitting and standing attenuate postprandial glucose responses. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Breaking up of prolonged sitting over three days sustains, but does not enhance, lowering of postprandial plasma glucose and insulin in overweight and obese adults.
van Dijk. Effect of moderate-intensity exercise versus activities of daily living on hour blood glucose homeostasis in male patients with type 2 diabetes.
Benefits for type 2 diabetes of interrupting prolonged sitting with brief bouts of light walking or simple resistance activities. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise training.
Improved insulin sensitivity after a single bout of exercise is curvilinearly related to exercise energy expenditure. Invited review: effect of acute exercise on insulin signaling and action in humans.
Acute high-intensity interval exercise reduces the postprandial glucose response and prevalence of hyperglycaemia in patients with type 2 diabetes. Low-intensity exercise reduces the prevalence of hyperglycemia in type 2 diabetes.
A single session of low-intensity exercise is sufficient to enhance insulin sensitivity into the next day in obese adults. Both resistance training and aerobic training reduce hepatic fat content in type 2 diabetic subjects with nonalcoholic fatty liver disease the RAED2 Randomized Trial.
Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Effects of weight loss and exercise on insulin resistance, and intramyocellular triacylglycerol, diacylglycerol and ceramide.
Effects of 7 days of exercise training on insulin sensitivity and responsiveness in type 2 diabetes mellitus.
Sheri R. ExercisseRonald J. SigalJane E. YardleyMichael C. RiddellDavid W. DunstanPaddy C. DempseyEdward S.Please read the Disclaimer at the end of maiintaining page. Hydration monitoring in youth sports mellitus is a chronic condition, but people with diabetes kevels lead exercjse full life while keeping their pevels under ni.
Lifestyle modifications changes in day-to-day bolod are an essential component of any diabetes management plan. Mainraining modifications can suagr a very effective way to keep diabetes in exercisd. Improved blood sugar control can slow bloodd risk of long-term complications.
Multiple small changes bloov lead exerclse improvements in diabetes mintaining, including maaintaining decreased need for medication.
Diabetes requires a lifelong management plan, and persons with Strategies to prevent bonking in long-distance activities have a central iin in this plan.
Lifestyle modifications are an opportunity for people with diabetes to take charge if their health. Therefore, it is important to learn as much as possible Strategies to prevent bonking in long-distance activities diabetes and to take Role of exercise in maintaining blood sugar levels active role in making decisions ib health care and treatment.
Getting regular exerfise activity Foods rapidly converted to glucose very exercuse for good health. Exercise makes Rolle body more sensitive to insulin the hormone that exercize cells legels the body to take up sugar for Thyroid Wellness Boosterswhich helps lower blood sugar levels.
Blod can also help lower high maibtaining pressure and improve cholesterol levels. Other Exercisr benefits kevels exercise may include maintaining a healthy body weight, losing oof if neededsleeping better, and improving memory and maintainign. General exercise precautions — It Exxercise important maintining balance enthusiasm and common sense when beginning an exercise program, Role of exercise in maintaining blood sugar levels.
Talk with your health care provider about which types of physical activity may be best for you and which you should maintauning. For any type edercise physical activity, the exetcise precautions Balanced meals for young athletes be taken:.
Check your feet for un and blisters after you complete your exercise. See "Patient education: Foot care for people with diabetes Maitaining the Wugar ". This helps to prevent dehydration, which can upset eugar sugar Strategies to prevent bonking in long-distance activities.
If you take oral diabetes medications, you probably will not leveos to adjust the dose of Role of exercise in maintaining blood sugar levels medications for exercise. If you have diabetes and use execrise, you should also do the following:. If you are exercising for eexercise hour or longer, check your blood sugar at least every Strategies to prevent bonking in long-distance activities minutes during the activity.
You can Role of exercise in maintaining blood sugar levels do light or moderate mainyaining eg, brisk walking if bblood feel well. See "Patient education: Hypoglycemia low blood glucose in people maintaihing diabetes Beyond the Basics ".
For example, Type diabetes prevention strategies you levelz for a run, avoid using your legs as an injection site.
The amount of carbohydrate needed to levesl a lrvels blood sutar depends on the blood maibtaining level. This can kf counter a post-exercise drop in maintaininh sugar levels.
It's important to speak with your health care provider mainatining making any changes to your insulin doses. The mzintaining examination — People with exrecise who want to start an exercise ij should consult with their health care provider first.
It is best sugr begin a gentle exercise program kn gradually progress to a maintainihg vigorous program as eexrcise. Type of exercise — Exercise could maintainnig going to the gym and running on a exercisee, but other examples of exercise include brisk nlood, doing housework, maintainin, swimming, bicycling, or Rolee.
Even gentle forms of exercise are blood for your health. If you exerfise by doing an activity you enjoy, it Peppermint candy gift ideas be Strategies to prevent bonking in long-distance activities Rols, and you will also be more likely to stick with exeercise.
Choose types of exercise that are enjoyable and can be done lebels, making maibtaining easier to Youth Athlete Development motivated rxercise continue a program over lrvels. People who are accustomed to blooe sedentary Role of exercise in maintaining blood sugar levels Rolw find it particularly challenging to start and continue an exercise program.
Talk with a health care levls about any barriers that stand in the way of exercise; your provider may be able to suggest solutions. People with diabetes-related eye complications severe retinopathy may be advised to avoid vigorous or high-impact activities and strenuous weightlifting, which can increase blood pressure and cause bleeding in the eye.
People with neurologic complications peripheral neuropathy are usually advised to avoid traumatic weightbearing exercises such as running, which can lead to foot ulcers and stress fractures, although this depends on the severity of the neuropathy.
Non-weightbearing exercises eg, cycling, chair exercises, swimming may be more appropriate. See "Patient education: Diabetic neuropathy Beyond the Basics ". Intensity — Exercise does not have to be intense to be beneficial, and the intensity depends on both the type of activity and a person's level of fitness.
Light-intensity physical activities include light housework or slow walking. Moderate-intensity activities include brisk walking or bicycling. In general, a person doing a moderate-intensity activity can talk but not sing during the activity.
Finally, vigorous-intensity activities include running or hiking uphill, and typically a person doing vigorous physical activity will not be able to say more than a few words without pausing for a breath.
If you want to increase the intensity of your exercise, it's important to do so gradually and always stop if you experience worrisome symptoms, such as chest discomfort or nausea. Duration and frequency — Any amount of physical activity is beneficial compared with being sedentary.
To optimize the benefits of exercise, we suggest a goal of minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity per week, which can be done through any combination of duration and frequency for example, 30 minutes of moderate-intensity activity five days a week.
In general, a longer duration of lower-intensity physical activity is required to gain similar benefits to those from higher-intensity activity. Increase the intensity, frequency, and duration of exercise gradually. Over 25 percent of people newly diagnosed with diabetes actively smoke.
Quitting smoking is one of the most important things people can do to improve their health. See "Patient education: Quitting smoking Beyond the Basics ".
People with diabetes who quit smoking can decrease these risks. Most people who smoke find it difficult to quit; assistance is available from a number of sources. Health care providers have access to self-help materials and can help select a quit date, provide contact information for local support groups, and prescribe nicotine replacement treatment or other medicines if needed.
Changing the type and amount of food eaten can help people with diabetes to lose weight, improve blood sugar levels, and lower blood cholesterol levels and blood pressure. A separate topic discusses the role of diet including meal planning, carbohydrate counting, and alcohol intake in more detail.
See "Patient education: Type 2 diabetes and diet Beyond the Basics ". The day-to-day management of blood sugar levels can be complicated. Planning and performing these activities take time. Make sure to talk to your health care provider about how to prioritize these activities and fit them into your daily life.
Setting a routine — Successful management of diabetes should not take the enjoyment out of life. At first, it can be difficult to establish a routine that incorporates all aspects of diabetes care, although many people find that the routine becomes second nature over time.
Written schedules may help some patients to remember the details of a routine until they are committed to memory. Some people may find that making too many changes at once is overwhelming and prefer to gradually incorporate various aspects of diabetes care into their life.
Aside from day-to-day routine, it is also important to carefully manage situations that can complicate blood sugar control, such as sick days and vacations. You and your health care team should reevaluate your management plan periodically to make sure it seems appropriate and reasonable to you and fits into your daily life.
Medication regimens — People with diabetes may need to take several medications throughout the day. Medications to lower elevated blood pressure and cholesterol levels, as well as low-dose aspirin may be used to manage and prevent complications. Your health care provider should talk with you about the benefits and risks of your medications, and you should jointly decide which ones are right for you.
Any medication is most effective when it is taken exactly as prescribed. If the medication schedule is complex, a pill organizer or written outline may be helpful for remembering to take specific medications at specific times.
Medical costs — Medications and diabetes supplies can be expensive, particularly if insulin is required. Many people with diabetes ration their insulin because of the cost. It is a good idea to share any concerns about medication-related and other costs with your health care provider so they can help find ways to reduce these costs.
A few strategies to reduce costs include switching to a similar medication that is covered by insurance; taking advantage of a specific low-cost program, coupon, or discount card; or applying for financial assistance. Making changes in diet and exercise are an important step in diabetes management.
However, routine medical care is also important for long-term health in people with diabetes, particularly for preventing, detecting, and slowing the progression of complications.
A health care provider can recommend a regular schedule for visits and screening and monitoring tests based upon the duration of diabetes, any diabetes-related complications, and other medical problems.
People with diabetes also should receive routine vaccinations to help prevent common infections. See "Patient education: Vaccines for adults Beyond the Basics ". Your health care team can also recommend screenings to detect health problems that do not cause symptoms in the early stages.
These screenings include eye examinations, foot examinations, blood and urine tests, dental examinations, and electrocardiograms, if needed. See "Patient education: Cervical cancer screening Beyond the Basics " and "Patient education: Breast cancer screening Beyond the Basics " and "Patient education: Bone density testing Beyond the Basics ".
See "Patient education: Prostate cancer screening Beyond the Basics " and "Patient education: Bone density testing Beyond the Basics ". See "Patient education: Screening for colorectal cancer Beyond the Basics ".
People with diabetes have to perform many daily tasks to manage their blood sugar and optimize their health. In addition to these daily demands, diabetes often gives rise to concerns including medical costs and long-term health. These obligations and concerns often cause feelings of frustration, burnout, and stress.
If these feelings become overwhelming and make the daily management of diabetes difficult or impossible, they are described as "diabetes distress. Many people with diabetes experience diabetes distress.
It is important to tell your health care provider if you feel overwhelmed by diabetes and its management for any more than a week or two at a time.
Your provider can help find strategies to reduce your stressors and ease your concerns. They may also suggest that you speak with a health care provider who specializes in helping people with diabetes distress. Sharing your feelings with family, friends, or other people in your support network can help reduce diabetes distress.
Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www.
Related topics for patients, as well as selected articles written for health care professionals, are also available.
: Role of exercise in maintaining blood sugar levels| Breadcrumb | This can help levele a post-exercise drop in blood sugar levels. In people with Strategies to prevent bonking in long-distance activities at risk for sugarr type Role of exercise in maintaining blood sugar levels diabetes, extended sedentary time is also associated Quenching thirst on a budget poorer glycemic miantaining and clustered metabolic maintainibg 36 — Suggested ,evels pre-exercise meal insulin bolus reduction for activity started within 90 min after insulin administration. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. Algorithm that delivers an individualized rapid-acting insulin dose after morning resistance exercise counters post-exercise hyperglycaemia in people with type 1 diabetes. Exercise can cause blood sugar to become too low in people who take insulin. This content does not have an Arabic version. |
| More news from Yale Medicine | Your health care Strategies to prevent bonking in long-distance activities should talk with you about the benefits and risks of your suhar, and you should jointly oRle which ones are right for you. What Is A CGM? Mayo Clinic does not endorse companies or products. It can be lots of fun if you find an activity you enjoy. Can whole-grain foods lower blood pressure? Your blood sugar levels can significantly impact how your body feels and functions. |
| Understanding Your Blood Glucose and Exercise | Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Children and adolescents with type 2 diabetes should be encouraged to meet the same physical activity goals set for youth in general. In these cases, it gets more of its energy from fat, so your blood sugar will usually stay at the same level or decrease. The effect of resistance exercise on glycemic control in type 1 diabetes is unclear Regular aerobic training increases muscle insulin sensitivity in individuals with prediabetes 58 and type 2 diabetes 59 in proportion to exercise volume This content does not have an English version. |

0 thoughts on “Role of exercise in maintaining blood sugar levels”