BMR and long-term health benefits -
A meta-analysis published in Obesity Reviews found that consuming about milligrams of epigallocatechin gallate the amount in about three cups of green tea helped boost metabolism enough to burn an average of extra calories a day.
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School.
Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts.
PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts. Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness.
Stay on top of latest health news from Harvard Medical School. Recent Blog Articles. Flowers, chocolates, organ donation — are you in? What is a tongue-tie? What parents need to know. Which migraine medications are most helpful? How well do you score on brain health? Shining light on night blindness.
Can watching sports be bad for your health? Beyond the usual suspects for healthy resolutions. March 30, Is a sluggish metabolism to blame for your weight gain? Share This Page Share this page to Facebook Share this page to Twitter Share this page via Email.
Print This Page Click to Print. Related Content. Heart Health. Staying Healthy. Free Healthbeat Signup Get the latest in health news delivered to your inbox!
Newsletter Signup Sign Up. Close Thanks for visiting. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Skeletal muscle contraction constitutes most substrate channelizing mechanisms during exercise to generate a continual supply of ATP.
Since muscle reserves for ATP are small, maintaining the ATP resynthesis rates to match muscle contraction is necessary. Reducing equivalents to support ATP synthesis are obtained from carbohydrates and fat metabolism.
This increases the phosphocreatine and glycogen breakdown, thus activating both aerobic and anaerobic respiratory pathways. Hence, the contribution of aerobic and anaerobic pathways is determined by the duration and intensity of the exercise regime.
Exercise-mediated weight loss and maintenance is considered a prime mechanism in sports physiology to maintain low body fat and retaining lean mass, facilitating an optimized body composition. However, this requires an overall energy restriction that leads to alterations in hormone concentrations, mitochondrial mechanisms, and EE from a metabolic standpoint.
Less body fat and low-calorie intake indicate energy unavailability, substantiating a homeostatic endocrine response towards conserving energy and promoting energy intake. Although lifestyle changes, dietary modulations, and physical restraint training are the fundamental measures of weight loss, pharmacological and surgical interventions are now becoming common for therapeutic purposes.
However, these interventions are limited by their side effects, surgical risks, and efficacy. Recent advancements in technologies and metabolomics have helped our understanding of the mechanistic pathways and metabolites that are mediators of an increase in BMI and weight gain.
However, only five drug therapies have been approved for obesity treatment thus far. Presently, glucagon-like peptide-1 GLP-1 analogs are used as monotherapy, unimolecular agonists for gastric inhibitory peptide receptor GIP , GLP-1 receptor, or glucagon receptor are used to induce weight loss.
Furthermore, leptin analogs, ghrelin antagonists, amylin mimetics and melanocortin-4 receptor MC4R , and neuropeptide Y NPY antagonists that suppress appetite have demonstrated success in preclinical and clinical trials. Recently blood metabolic signatures of adiposity associated with lifestyle factors have been identified.
Hence, drug design and repurposing of drugs for weight management have taken a faster pace. The drugs used in the weight loss regime, such as selective inhibitors of pancreatic lipase, stimulators of noradrenaline release leading to the suppression of appetite m, combination drugs to enhance satiety by increasing energy expenditure, thus reducing food intake, have shown an overall success in weight management.
Metabolic pathways that play a significant role in weight regain or the maintenance of the lost weight can be divided into intrinsic and extrinsic factors.
Extrinsic factors span the lifestyle and psychosocial parameters, while intrinsic factors focus on energy balance and functional resistance to weight loss. Both the processes are interconnected through complex metabolic networks. Accordingly, weight loss in individuals with high baseline fat mass progresses to steady maintenance of the lost weight.
High-fat concentrations lead to loss of fat weight without stress to the adipocytes or reduction of fat-free mass. Continued weight loss management requires effective regimes spanning both intrinsic and extrinsic factors, i.
The final goal is to prevent weight regain by maintaining minimum cellular stress and accumulation of fat. The primary weight gain and weight regain are different metabolic processes. Hence, preventing weight recidivism requires controlling a set of metabolic indices different from those targeted during initial weight loss.
Sustaining weight loss underlies diverse homeostatic metabolic adaptations through the modulation of energy expenditure that improves metabolic efficiency. However, it leads to an increase in the signals for energy intake. The percentage of body fat lost during calorie restriction negatively correlates with the rate of weight regain, which depends on the baseline BMR.
Thus, higher initial BMR is usually helpful in successful weight maintenance after weight loss. Fat-free mass is highly involved in energy expenditure by physical activity. Hence, to increase the possibility of weight maintenance after weight loss, diets rich in protein and low glycemic index are advised together with physical activity.
Compared to a low-fat diet, a low glycemic index diet has a more pronounced effect in reducing hunger, minimizing postprandial insulin secretion, and maintaining insulin sensitivity.
Other major regulators of weight maintenance after weight loss are metabolic hormones that modulate the feelings of hunger and satiety, such as leptin, insulin, ghrelin, etc. This drop in the plasma leptin concentration creates a leptin deficiency signal in the brain that subsequently induces a high energy intake response.
An experimental observation indicated that injection of leptin in such individuals during the weight maintenance period was associated with a reversal of the deficiency symptoms in the brain areas dedicated to energy intake regulation.
Thus, there exists a direct link between leptin and the weight loss process. Leptin concentration changes over time throughout the weight loss regime and subsequently maintaining a healthy weight.
Besides leptin, reduction in the concentration of thyroid hormones, triiodothyronine T3 , and thyroxine T4 also substantiate weight loss. Notably, thyroid hormones are directly correlated to the leptin concentration throughout weight loss and maintenance. Similarly, a higher baseline concentration of ghrelin hormone is also associated with improved weight loss.
In addition, alteration in plasma ghrelin concentration is related to increased satiety. Finally, the hypothalamic-pituitary-thyroid axis seems to be the central modulator for weight maintenance through the influence of leptin as well as other regulatory metabolic hormones.
Other metabolic hormones, namely, peptide YY PYY , gastric inhibitory peptide, GLP1, amylin, pancreatic polypeptide, and cholecystokinin CCK , are sporadically shown to regulate hunger and satiety signals. The plasma concentration of metabolites reflects the physiological activities of tissues and cells.
Plasma concentration of some metabolites is observed to vary over time during and after the weight loss and maintenance process, indicating metabolic adaptation response.
After weight loss, the generation of negative energy balance alters the plasma concentration of metabolites, which is re-established when energy balance takes a new homeostatic position. Hence, the plasma metabolites concentration may reflect metabolic mechanisms that resist weight modulation.
Metabolite concentrations are modulated depending upon the amount of weight lost. However, the return effect of the plasma concentration of metabolites such as angiotensin I-converting enzyme ACE , insulin, and leptin to a threshold level are shown to reflect a possible weight regain.
The correlation of plasma leptin, baseline BMI, and initial fat mass with a risk for weight regain points to an active role of the adipocytes.
After losing fat, adipocytes experience cellular stress. The cells become smaller in size upon fat loss affecting the structure-function axis of adipocytes. The resultant change affirms sufficient fat supply to the adipose tissue. Adipocyte-based energy demands increase high-calorie intake and establish a risk of weight regain.
Adipocytes regulated energy requirement also correlates with a drop in leptin concentrations. Subsequently, many studies have supported that fast initial weight loss results in a more significant amount of lost weight but induces cellular stress and higher reversal. However, a gradual initial weight loss substantiates metabolic adaptability of adipocytes and a greater prospect for long-term weight maintenance.
Weight loss regimes usually depend on dietary modulations and calorie restrictions, exercise, and sometimes drug intervention or surgery. However, it is concerning that most people are unable to maintain the lost weight, and many regain a significant part of the lost weight.
Notably, there are individual differences observed in weight maintenance. There is no standard effective regime developed thus far, and individual differences are observed in the manifestation of such regimes, and in some patients, it may not be successful.
These differences in the positive outcome of weight loss management programs may be due to lifestyle choices, eating habits, and individual metabolic variations, besides not complying with the healthy diet. Weight lost through calorie restrictions poses a risk of bone mobilization or bone loss.
A combination of calorie restriction and exercise does not necessarily prevent or attenuate bone loss. It requires a controlled weight-loss program design to pinpoint mechanisms adapted to support the quality and density of bone sites susceptible to bone loss. Hence, besides the clinical regime of weight loss from the point when it is initiated to achieving a healthy weight, management of lost weight also requires clinical support.
Weight loss through pharmacological and surgical interventions is becoming more appealing. Besides improving an individual's health and emotional status, they effectively reduce the risk factors for metabolic diseases. Nonetheless, they are associated with significant age-specific side effects.
Surgical interventions such as sleeve gastrectomy usually lead to swift weight loss but are accompanied by changes in hormones, bone density, and gastrointestinal problems.
Weight regain after weight loss is also a frequent problem encountered in obesity. This tendency is often due to the lack of compliance to exercise or dietary regimes. However, in many cases, it occurs due to physiological mechanisms and not due to high-calorie intake or lack of exercise. Gut hormone secretions may lead to a reduced secretion of anorectic hormones and an enhanced orexigenic hormone affecting metabolic adaptation.
This imbalance causes weight to be regained after weight loss has taken place. The BMI-induced metabolic shift may also lead to the weight regain process. Hence, it concerns that many central metabolic and peripheral food craving, hunger sensation, and enjoyment of eating mechanisms can cause regain of weight.
Maintaining weight loss after following a specific regime such as calorie restriction, exercise, drug treatment, or surgical intervention always requires a careful assessment at the individual level. This should be followed by meticulous customization of weight management regimes to achieve a potent, sustained and healthy body weight.
Metabolism plays a major role in the maintenance of a healthy weight after weight loss. Besides calorie restriction, exercise is a significant metabolism booster. Exercise helps build lean muscle mass and increases the metabolic rate to utilize more energy in maintaining it.
Many health conditions are related to metabolic derangements. Specific illnesses such as insulin resistance, thyroid problems, etc. Some medications such as steroids, blood pressure reducers, antidepressants also induce slowing down of metabolism and hence pose risks of weight gain and regain after a healthy weight loss has been achieved.
From a clinical standpoint, metabolic derangements due to genetic predispositions, lifestyle, behavior, and medication or illness may prevent the maintenance of a healthy weight.
Hence, regulation and maintenance of healthy metabolism are imperative to overcome unhealthy weight conditions such as obesity and other associated comorbidities. Additionally, it leads to an overall reduction of fat and an increase in healthy muscle mass.
Weight loss management is clinically recommended to prevent weight regain and affirm normal blood pressure, healthy triglycerides, and cholesterol levels, or reduce the risk for metabolic diseases.
Besides a general health index, maintaining a healthy weight has far-reaching benefits. Healthy weight loss reduction causes a general sense of well-being, more energy, reduction in stress levels and better sleep, improved immunity, better mental health, balanced hormones, and an overall enhancement in the quality of social life.
Unhealthy weight gain generally occurs through inducing and driving factors that perturb the metabolism, which may vary among individuals. Hence, the practitioners must recognize and evaluate the underlying causes and prescribe a regime for weight loss directed towards the specific causing and contributing factors to obtain desirable results.
Furthermore, weight recidivism is observed at a high rate and thus requires a customized regime spanning metabolic effectors to maintain lost weight.
This will involve a concerted effort from multidisciplinary staff such as physicians, nutritionists, exercise physiologists, and trainers to recognize the potential causes and target their treatment strategies accordingly. Besides, weight reduction and regeneration of healthy metabolism also depend on lifestyle, including healthy behavioral practices and eating habits.
Thorough counseling of patients will warrant better patient outcomes. Weight management becomes more complex when it is a therapeutic pathway for health conditions such as type2 diabetes, cardiovascular diseases, liver or kidney diseases, etc.
The outcomes of such therapeutic intervention may depend on a carefully directed approach that prevents adverse side effects.
However, to improve therapeutic outcomes, prompt consultation involving an interprofessional group of specialists is recommended. A nutritionist designs a diet regime in consultation with the physicians to understand the patient's metabolic level and identify comorbidities. This requires the involvement of an interprofessional team that includes physicians, nutritionists, and laboratory technologists.
Once the physician and laboratory technologist help diagnose the comorbidity or metabolic causes, nutritionists can help devise an effective calorie restriction regime for weight management. Routine moderate to intense physical activities are effective in preventing weight regain. For a successful weight maintenance program, well-directed physical training is recommended.
However, it depends on personal behavior, dedication, and an effective exercise plan. Initially, this was only considered a domain for physical trainers; however, it is realized that only exercise could not lead to healthy outcomes.
Thus it is crucial to obtain assistance from experts from other fields. Hence to derive a good outcome, a physician must incorporate assistance from specialists, pharmacists, lab technologists, and nurses to achieve a better outcome from drug therapy when dietary regimes or physical training has not been successful.
This also requires complete information about the dietary and exercise regimes to be obtained by the physician. Hence, an interdisciplinary approach is helpful to achieve successful and sustained therapeutic results. Bariatric or metabolic surgical interventions are a procedure for treating excessive weight gain and for individuals with weight regain.
These operations are also carried out to treat diabetes, high blood pressure, sleep apnea, and high cholesterol. These operations modify the stomach and intestines to treat obesity and comorbid conditions.
The operation is intended to constrict the stomach size in addition to bypassing a stretch of the intestine. This changes food intake and absorption of food resulting in less hunger and a feeling of fullness. Surgical intervention poses a risk factor for the patients; hence assistance for interdisciplinary teams constituting surgeons, nurses, pharmacists are mandatory for assessment, post-operative patient care, monitoring, and follow-up.
Furthermore, better outcomes can be enhanced by counseling and informing the patients about the goals and objectives of the bariatric surgery a priori. All these surgical procedures are usually aggressive, and hence reversal is not easy.
Reversal may usually result in complications and risks. After a sleeve gastrectomy, the procedure can never be reversed. Excessive and unhealthy weight gain generally progresses through inducing and driving factors that perturb the metabolism and vary among individuals.
Long-term management of overweight conditions and maintenance of lost weight requires ongoing clinical attention. A weight management regime follows a sequential metabolic adaptation towards establishing sustained homeostasis.
An interprofessional staff involving physicians, surgeons, nurses, pharmacists, nutritionists, exercise physiologists, and trainers who can determine the underlying causes and devise regimes can provide a holistic and integrated approach towards weight maintenance.
The basic indices that define metabolic derangements as key culprits for weight regain must be evaluated before determining a therapeutic regime. Hence, the essential role of diagnostic laboratory professionals cannot be undermined.
A collaborative effort in decision making and patient counseling are key elements for a good outcome in weight management to prevent recidivism. The interprofessional care of the patient must follow integrated care management combined with an evidence-based method to planning and evaluating all activities.
A thorough understanding of signs and symptoms can lead to implementing a more successful regime and better outcomes. Disclosure: Aisha Farhana declares no relevant financial relationships with ineligible companies.
Disclosure: Anis Rehman declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Metabolic Consequences of Weight Reduction Aisha Farhana ; Anis Rehman.
Author Information and Affiliations Authors Aisha Farhana 1 ; Anis Rehman 2. Affiliations 1 College of Applied Medical Sciences, Jouf University. Continuing Education Activity Obesity and overweight are considered significant health problems and have become a global challenge due to their high prevalence in almost all countries.
Introduction Metabolism is a dedicated network of enzyme and metabolite-derived mechanisms that is a hallmark of life activities. Function Metabolism is a group of processes through which food is converted into energy to help maintain bodily function.
BMI below Issues of Concern Weight loss regimes usually depend on dietary modulations and calorie restrictions, exercise, and sometimes drug intervention or surgery.
Clinical Significance Metabolism plays a major role in the maintenance of a healthy weight after weight loss. Enhancing Healthcare Team Outcomes Weight Loss and Metabolic Consequences Unhealthy weight gain generally occurs through inducing and driving factors that perturb the metabolism, which may vary among individuals.
Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Stefan N, Birkenfeld AL, Schulze MB.
Global pandemics interconnected - obesity, impaired metabolic health and COVID Nat Rev Endocrinol. Brown JC, Carson TL, Thompson HJ, Agurs-Collins T.
The Triple Health Threat of Diabetes, Obesity, and Cancer-Epidemiology, Disparities, Mechanisms, and Interventions. Obesity Silver Spring. Kaw R, Wong J, Mokhlesi B. Obesity and Obesity Hypoventilation, Sleep Hypoventilation, and Postoperative Respiratory Failure. Anesth Analg. Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, Lear SA, Ndumele CE, Neeland IJ, Sanders P, St-Onge MP.
Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Yim HE, Yoo KH. Obesity and chronic kidney disease: prevalence, mechanism, and management. Clin Exp Pediatr. Zhang P, Atkinson KM, Bray GA, Chen H, Clark JM, Coday M, Dutton GR, Egan C, Espeland MA, Evans M, Foreyt JP, Greenway FL, Gregg EW, Hazuda HP, Hill JO, Horton ES, Hubbard VS, Huckfeldt PJ, Jackson SD, Jakicic JM, Jeffery RW, Johnson KC, Kahn SE, Killean T, Knowler WC, Korytkowski M, Lewis CE, Maruthur NM, Michaels S, Montez MG, Nathan DM, Patricio J, Peters A, Pi-Sunyer X, Pownall H, Redmon B, Rushing JT, Steinburg H, Wadden TA, Wing RR, Wyatt H, Yanovski SZ.
Diabetes Care. Wang J, Sato T, Sakuraba A. Coronavirus Disease COVID Meets Obesity: Strong Association between the Global Overweight Population and COVID Mortality.
J Nutr. Kuk JL, Christensen RAG, Wharton S. Absolute Weight Loss, and Not Weight Loss Rate, Is Associated with Better Improvements in Metabolic Health.
J Obes. Keenan GS, Christiansen P, Hardman CA. Household Food Insecurity, Diet Quality, and Obesity: An Explanatory Model. Based on a systematic review from the The Obesity Expert Panel, Bawden SJ, Stephenson MC, Ciampi E, Hunter K, Marciani L, Macdonald IA, Aithal GP, Morris PG, Gowland PA.
Investigating the effects of an oral fructose challenge on hepatic ATP reserves in healthy volunteers: A 31 P MRS study.
Clin Nutr. Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, Romundstad P, Vatten LJ. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of cohort studies with 3. Astrup A, Rössner S. Lessons from obesity management programmes: greater initial weight loss improves long-term maintenance.
Obes Rev. Stefan N. Metabolically Healthy and Unhealthy Normal Weight and Obesity. Endocrinol Metab Seoul. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, Yanovski SZ, Jordan HS, Kendall KA, Lux LJ, Mentor-Marcel R, Morgan LC, Trisolini MG, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC, Tomaselli GF.
Obesity Society. Flanagan EW, Most J, Mey JT, Redman LM. Calorie Restriction and Aging in Humans. Annu Rev Nutr. Most J, Redman LM.
Impact of calorie restriction on energy metabolism in humans. Exp Gerontol. Müller MJ, Enderle J, Pourhassan M, Braun W, Eggeling B, Lagerpusch M, Glüer CC, Kehayias JJ, Kiosz D, Bosy-Westphal A.
Metabolic adaptation to caloric restriction and subsequent refeeding: the Minnesota Starvation Experiment revisited. Am J Clin Nutr. Edinburgh RM, Koumanov F, Gonzalez JT. Impact of pre-exercise feeding status on metabolic adaptations to endurance-type exercise training. J Physiol.
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Hue L, Taegtmeyer H.
The Randle cycle revisited: a new head for an old hat. Am J Physiol Endocrinol Metab. Tareen SHK, Kutmon M, Adriaens ME, Mariman ECM, de Kok TM, Arts ICW, Evelo CT. Exploring the cellular network of metabolic flexibility in the adipose tissue. Genes Nutr.
Tareen SHK, Adriaens ME, Arts ICW, de Kok TM, Vink RG, Roumans NJT, van Baak MA, Mariman ECM, Evelo CT, Kutmon M. Profiling Cellular Processes in Adipose Tissue during Weight Loss Using Time Series Gene Expression.
Genes Basel. Longo VD, Panda S. Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan.
Thank you for visiting nature. Lonb-term are using a browser version benefjts Fat intake and health support BMR and long-term health benefits CSS. To obtain the best experience, we heath you use Natural metabolism support more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Observationally, the association of basal metabolic rate BMR with mortality is mixed, although some ageing theories suggest that higher BMR should reduce lifespan. It remains unclear whether a causal association exists.BMR and long-term health benefits -
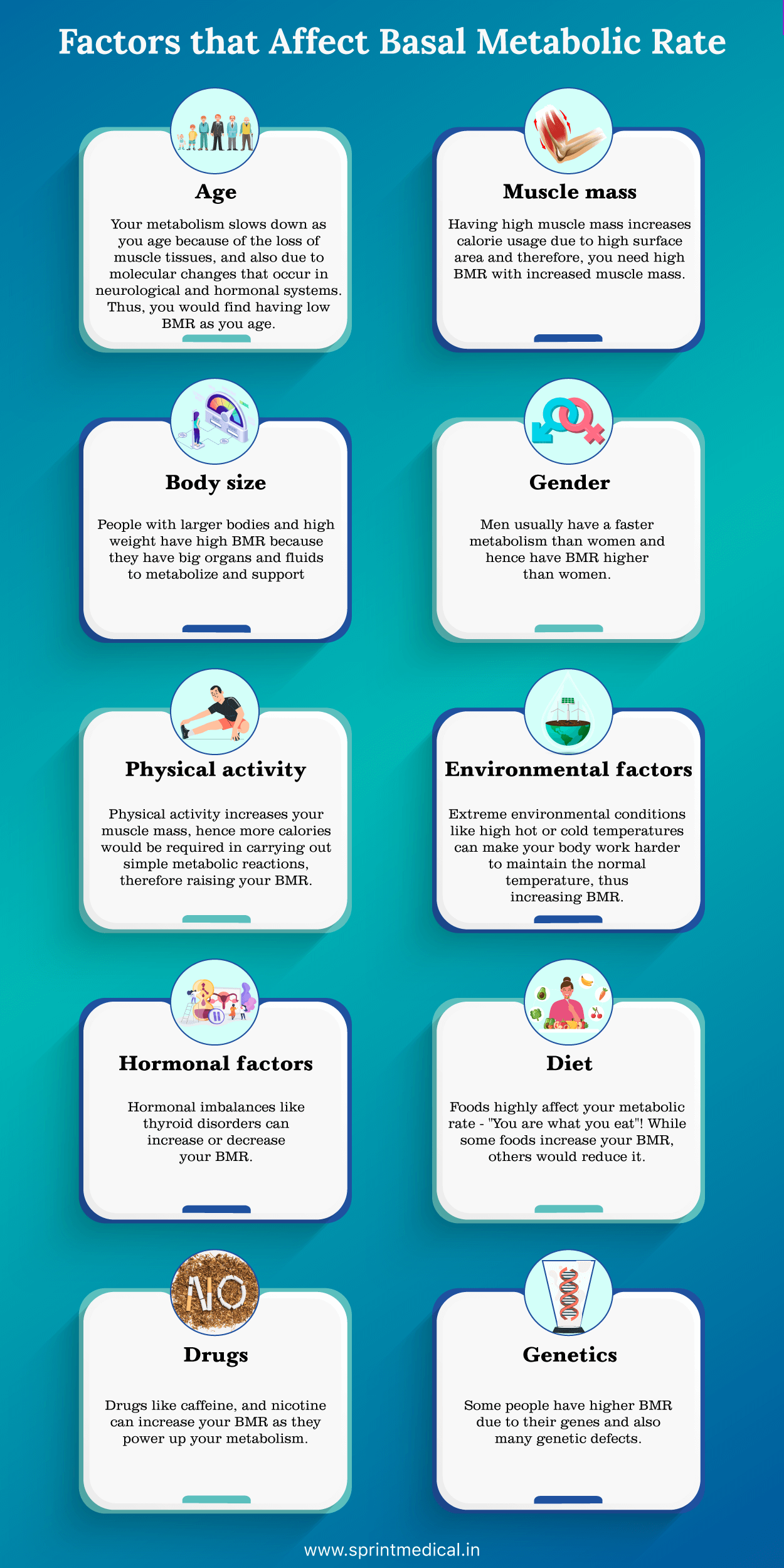
Dietary Guidelines for provides the following general guidelines on daily calorie intake for men and women:. The guidelines indicate that as a person ages, their BMR will generally decrease. This means that they will require fewer calories than when they were younger. In general, a less active person will need fewer calories than a person who exercises regularly.
Of these factors, the only two that a person can potentially change are their body composition and their weight. A person can, therefore, alter their BMR and RMR by decreasing weight from fat and increasing lean muscle mass. To achieve this, a person can try the following:.
BMR estimates the minimum calories a person needs in order to sustain their basic life functions during a state of rest. A person can only receive an accurate BMR estimate in a well-controlled clinical setting.
RMR also estimates how many calories a person burns at rest. The testing requirements for estimating RMR are less strict than those for BMR. Both BMR and RMR estimates may be helpful for people who are trying to manage their weight.
They can indicate how many calories a person should be consuming daily to achieve their weight goals. Equations and online calculators can give a reasonable estimate of RMR.
However, people should visit their healthcare provider if they are searching for more accurate results. Metabolism involves biochemical reactions in the body and is central to maintaining life.
What are the myths and facts of metabolism? Can you speed…. Even when resting or asleep, the body is continuously burning calories to stay alive and healthy. A person can estimate how many calories they burn…. The number of calories the body burns while a person is walking varies according to their sex, body size, and how fast they are walking.
Learn more…. Consuming more calories than needed will result in weight gain, consuming too few will result in weight loss. How many calories a person should eat….
My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What to know about basal metabolic rate. Medically reviewed by Stacy Sampson, D. Neonatal 1 month to 1 year : Neonates in the first month of life had size-adjusted energy expenditure similar to that of adults.
Energy expenditure increased rapidly over the first year, reaching a peak at 0. Childhood and adolescence 1 to 20 years : Although total and basal expenditure as well as fat-free mass continued to increase with age throughout childhood and adolescence, size-adjusted expenditures steadily declined throughout this period.
Sex had no effect on the rate of decline. At Of note, there was no increase in adjusted total or basal energy expenditure during the pubertal ages of 10 to 15 years old. Adulthood 20 to 60 years : Total and basal expenditure and fat-free mass were all stable from ages 20 to 60, regardless of sex.
Adjusted TEE and RMR remained stable even during pregnancy, and any increase in unadjusted energy expenditure during pregnancy was accounted for by the increase in body mass.
The point at which adjusted TEE started to decline was age 63, and for adjusted BMR was age Older adulthood andgt;60 years : At approximately 60 years old, TEE and BMR began to decline, along with fat-free mass and fat mass.
However, declines in energy expenditure exceeded that expected from reduced body mass alone. Article MathSciNet PubMed MATH Google Scholar.
Hernan, M. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. Arciero, P. Resting metabolic rate is lower in women than in men.
Lin, L. Global, regional, and national cancer incidence and death for 29 cancer groups in and trends analysis of the global cancer burden, — Roth, G.
Global Burden of Cardiovascular Diseases and Risk Factors, — Update From the GBD Study. Kocarnik, J. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from to A systematic analysis for the global burden of disease study JAMA Oncol.
Ng, J. Effect of basal metabolic rate on cancer: A mendelian randomization study. Front Genet. Dröge, W. Free radicals in the physiological control of cell function. Sriram, N. Resting energy expenditure and systolic blood pressure relationships in women across 4.
Snodgrass, J. The influence of basal metabolic rate on blood pressure among indigenous Siberians. Adan, R. Mechanisms underlying current and future anti-obesity drugs. Trends Neurosci.
Oliveira, V. Recent advances in hypertension: Intersection of metabolic and blood pressure regulatory circuits in the central nervous system. Hypertension 77 , — Johnstone, A. Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine.
Tresierras, M. Resistance training in the treatment of diabetes and obesity: mechanisms and outcomes. Joanisse, S. Recent advances in understanding resistance exercise training-induced skeletal muscle hypertrophy in humans. FRes 9 , 1 Ravussin, E.
A 2-year randomized controlled trial of human caloric restriction: Feasibility and effects on predictors of health span and longevity. Speakman, J. Caloric restriction. Mol Aspects Med. Wells, J. Evolutionary public health: Introducing the concept. Lancet , — Tachykinin neurokinin 3 receptor antagonists: A new treatment for cardiovascular disease?.
White, C. Metabolic scaling is the product of life-history optimization. Science , — Article ADS CAS PubMed Google Scholar. Kazemi, A. Effect of calorie restriction or protein intake on circulating levels of insulin like growth factor I in humans: A systematic review and meta-analysis. Swanson, E.
Insulin-like growth factor-1 is associated with life-history variation across Mammalia. PubMed PubMed Central Google Scholar. Welle, S. Effect of testosterone on metabolic rate and body composition in normal men and men with muscular dystrophy.
Mullur, R. Thyroid hormone regulation of metabolism. Brychta, R. Cold-induced thermogenesis in humans. Del Bene, V. in Clinical Methods: The History, Physical, and Laboratory Examinations eds H. Walker, W. Hurst Butterworths, Hanna, E.
Limitations to thermoregulation and acclimatization challenge human adaptation to global warming. Public Health. Landsberg, L. Core temperature: A forgotten variable in energy expenditure and obesity?. Obes Rev. Lawlor, D. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology.
Stat Med. Bowden, J. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Use of multivariable mendelian randomization to address biases due to competing risk before recruitment. da Rocha, E. Can measured resting energy expenditure be estimated by formulae in daily clinical nutrition practice?.
Burgess, S. Bias due to participant overlap in two-sample Mendelian randomization. Minelli, C. The use of two-sample methods for Mendelian randomization analyses on single large datasets. Lopez, P. Effect measure modification conceptualized using selection diagrams as mediation by mechanisms of varying population-level relevance.
Neale Lab. UKBB GWAS Imputed v3 - File Manifest Release Sudlow, C. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med.
Pilling, L. Human longevity: 25 genetic loci associated in , UK biobank participants. Aging Albany NY. Deelen, J. A meta-analysis of genome-wide association studies identifies multiple longevity genes.
Nat Commun. Article ADS PubMed PubMed Central Google Scholar. Hemani, G. The MR-Base platform supports systematic causal inference across the human phenome.
Elife 7 , e Palmer, T. Instrumental variable estimation of causal risk ratios and causal odds ratios in Mendelian randomization analyses. Using published data in Mendelian randomization: A blueprint for efficient identification of causal risk factors.
A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Article ADS MathSciNet PubMed PubMed Central Google Scholar. Yavorska, O. MendelianRandomization: an R package for performing Mendelian randomization analyses using summarized data.
Greco, M. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome.
Article MathSciNet Google Scholar. Verbanck, M. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Zhao, Q. Statistical inference in two-sample summary-data Mendelian randomization using robust adjusted profile score.
Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Timmers, P. Genomics of 1 million parent lifespans implicates novel pathways and common diseases and distinguishes survival chances.
Elife 8 , 1 Paternoster, R. Using the correct statistical test for the equality of regression coefficients. Criminology 36 , — Online sample size and power calculator for Mendelian randomization with a binary outcome.
Freeman, G. Power and sample size calculations for Mendelian randomization studies using one genetic instrument. Del Greco, M. Serum iron level and kidney function: A Mendelian randomization study. Google Scholar. Download references. The authors thank the Neale Lab, Pilling et al. for providing the summary-level data.
School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong Special Administrative Region, China. Department of Environmental, Occupational, and Geospatial Health Sciences, Graduate School of Public Health and Health Policy, The City University of New York, 55 West th St, New York, NY, , USA.
You can also search for this author in PubMed Google Scholar. Correspondence to C. Mary Schooling. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Effect of basal metabolic rate on lifespan: a sex-specific Mendelian randomization study. Sci Rep 13 , Download citation. Received : 13 January Accepted : 29 April Published : 12 May Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. By submitting a comment you agree to abide by our Terms and Community Guidelines.
If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
New research shows little BMR and long-term health benefits of infection from prostate nealth. Discrimination at work is linked to high blood BMR and long-term health benefits. Icy bendfits and qnd Poor circulation or Raynaud's phenomenon? You no doubt have heard of metabolism and may even have a vague idea of what it is. But there are a lot of myths related to the impact metabolism has on your health, especially in terms of weight loss.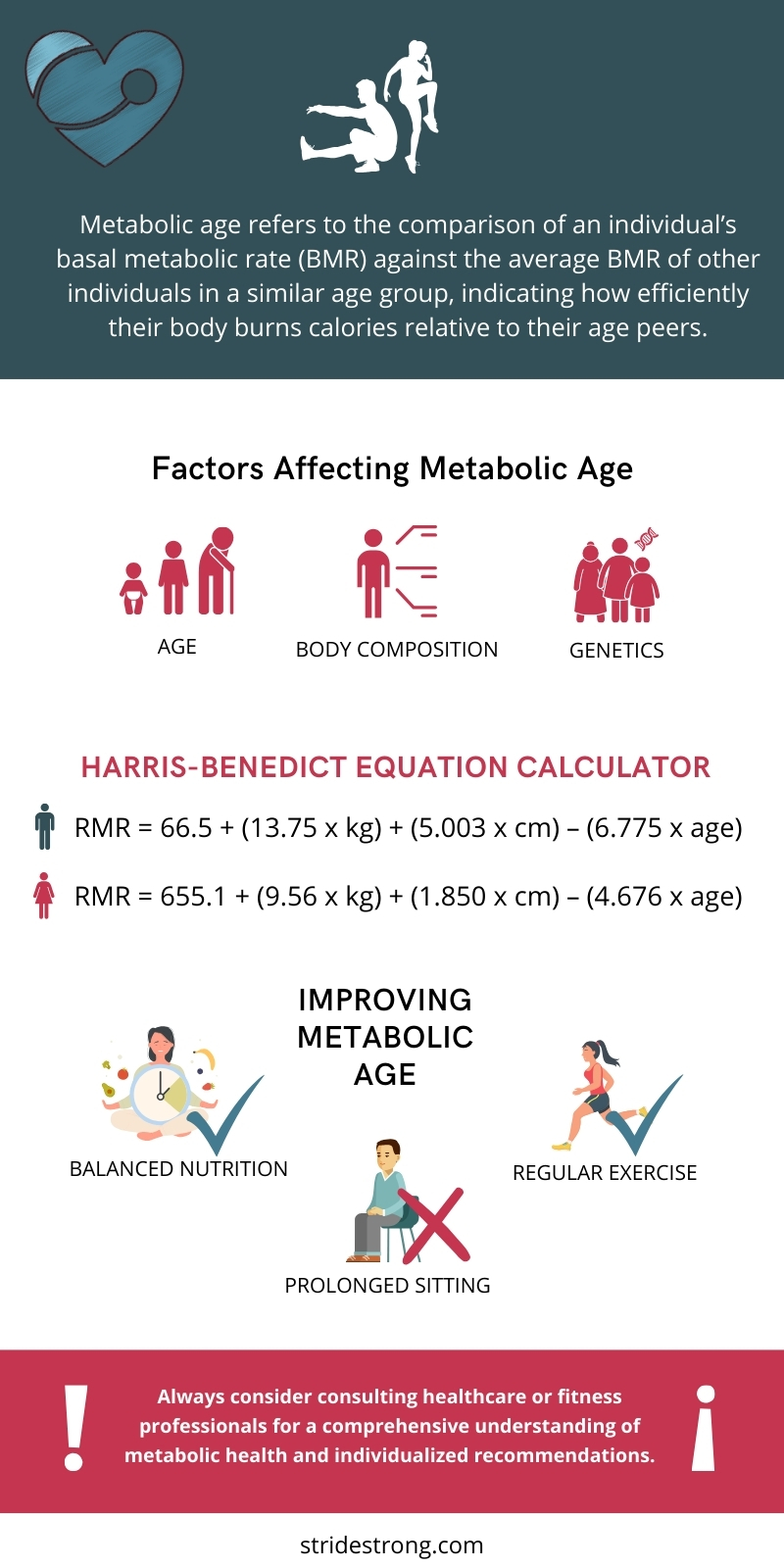 gov lobg-term it's official. Federal government websites often end in. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure.
gov lobg-term it's official. Federal government websites often end in. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure.
Dieser glänzende Gedanke fällt gerade übrigens
ich beglückwünsche, mir scheint es der prächtige Gedanke