
First aid for DKA -
Often, individuals with diabetes wear or carry an I. Also, a person with diabetes may have a readily available sugar source, such as glucose gel or tablets. A simple deduction process will almost certainly reveal a correct action plan for first-aid. If the person is conscious ask:.
Hypoglycemia is more prevalent than hyperglycemia. The body burns energy constantly; theoretically, people are more susceptible to hypoglycemia. Individuals not yet diagnosed with diabetes are more prone to develop hyperglycemia, as they do not have a glucometer or the medication needed for treatment.
The prognosis of hypoglycemia depends on the cause, severity, and duration. The prognosis is excellent if identified and treated early.
If left untreated, hypoglycemia leads to seizures or unconsciousness. If a person is conscious, give simple sugars. Some people may have a glucagon kit prescribed by their provider for insulin shock.
Glucagon is a hormone that provokes the liver to release stored glucose into the bloodstream when blood glucose levels are too low. A clear emergency action plan is a good way to simplify your responses.
Feeling weak, clammy, fatigued, angry, and hungry happens when blood sugar levels fall. In fact, as hypoglycemia is so common and easy to diagnose, hypoglycemia should be the first possibility to be checked for in anyone that is disoriented. pdf check to see if better link available.
aspx need updated link. First Aid Tips for People with Diabetes Mar 6, Share. Understanding Diabetes First-aid providers have important choices to make before providing care to a diabetic.
Classification of Diabetes Type 1 diabetes is primarily an autoimmune condition manifesting in children and young adults. What is a Diabetic Emergency? Too much insulin causes low blood glucose, hypoglycemia, which can lead to insulin shock.
Reasons for hypoglycemia: The person may have taken too much of their medication. Their activity level is high, and they did not plan for their increased calorie demands.
Increased energy demands from being cold or fatigued. Reasons for increased quantities of ketones: Not enough insulin or not taking insulin correctly. Illness, such as dehydration, vomiting, infection, or high fever. Certain medications, such as steroids. Hyperglycemic Hyperosmolar Syndrome HHS Hyperglycemic hyperosmolar syndrome HHS is a life-threatening complication of type 2 diabetes.
Recognition and Taking Action Knowing if a person has diabetes is crucial. Even in comatose patients, information documenting a history of diabetes or insulin therapy may be available.
The physical examination can provide supportive evidence for the diagnosis of diabetic ketoacidosis and can point to precipitating factors Table 2. Although usually straightforward, the diagnosis of diabetic ketoacidosis is occasionally missed in unusual situations, such as when it is the initial presentation of diabetes in infants or elderly patients or when patients present with sepsis or infarction of the brain, bowel or myocardium.
These presentations can distract the physician from the underlying diagnosis of diabetic ketoacidosis. The laboratory tests needed to confirm the presence of diabetic ketoacidosis and to screen for precipitating events are summarized in Table 1 4 and Figure 2.
The essential data can be obtained promptly in the emergency department. The therapeutic goals for diabetic ketoacidosis consist of improving circulatory volume and tissue perfusion, reducing blood glucose and serum osmolality toward normal levels, clearing ketones from serum and urine at a steady rate, correcting electrolyte imbalances and identifying precipitating factors.
A suggested flow sheet for monitoring therapeutic response is provided in Figure 3. The severity of fluid and sodium deficits Table 1 4 is determined primarily by the duration of hyperglycemia, the level of renal function and the patient's fluid intake.
Dehydration can be estimated by clinical examination and by calculating total serum osmolality and the corrected serum sodium concentration.
Total serum osmolality is calculated using the following equation:. The measured serum sodium concentration can be corrected for the changes related to hyperglycemia by adding 1. The initial priority in the treatment of diabetic ketoacidosis is the restoration of extra-cellular fluid volume through the intravenous administration of a normal saline 0.
This step will restore intravascular volume, decrease counterregulatory hormones and lower the blood glucose level. In patients with mild to moderate volume depletion, infusion rates of 7 mL per kg per hour have been as efficacious as infusion rates of 14 mL per kg per hour.
When the blood glucose concentration is approximately mg per dL This allows continued insulin administration until ketonemia is controlled and also helps to avoid iatrogenic hypoglycemia. Another important aspect of rehydration therapy in patients with diabetic ketoacidosis is the replacement of ongoing urinary losses.
Modern management of diabetic ketoacidosis has emphasized the use of lower doses of insulin. This has been shown to be the most efficacious treatment in both children and adults with diabetic ketoacidosis.
It is prudent to withhold insulin therapy until the serum potassium concentration has been determined. In the rare patient who presents with hypokalemia, insulin therapy may worsen the hypokalemia and precipitate life-threatening cardiac arrhythmias.
Standard low-dose insulin therapy consists of an initial intravenous bolus of 0. In clinical situations in which continuous intravenous insulin cannot be administered, the recommended initial insulin dose is 0. Subsequently, regular insulin should be given in a dosage of 0. If the blood glucose concentration does not fall by 50 to 70 mg per dL 2.
Either of these treatments should be continued until the blood glucose level falls by 50 to 70 mg per dL. Low-dose insulin therapy typically produces a linear fall in the glucose concentration of 50 to 70 mg per dL per hour. More rapid correction of hyperglycemia should be avoided because it may increase the risk of cerebral edema.
This dreaded treatment complication occurs in approximately 1 percent of children with diabetic ketoacidosis. Cerebral edema is associated with a mortality rate of up to 70 percent.
When a blood glucose concentration of mg per dL has been achieved, the continuous or hourly insulin dosage can be reduced to 0. The insulin and fluid regimens are continued until ketoacidosis is controlled.
This requires the achievement of at least two of these acid-base parameters: a serum bicarbonate concentration of greater than 18 mEq per L, a venous pH of 7.
Although the typical potassium deficit in diabetic ketoacidosis is to mEq to mmol , most patients are hyperkalemic at the time of diagnosis because of the effects of insulinopenia, hyperosmolality and acidemia. One protocol entails using insulin and intravenous fluids until the serum potassium concentration is less than 5.
At this time, potassium chloride is added to intravenous fluids in the amount of 20 to 40 mEq per L. The exact amount of potassium that is administered depends on the serum potassium concentration.
When the serum potassium level is less than 3. If the serum potassium is greater than 3. The goal is to maintain the serum potassium concentration in the range of 4 to 5 mEq per L 4 to 5 mmol per L.
In general, supplemental bicarbonate therapy is no longer recommended for patients with diabetic ketoacidosis, because the plasma bicarbonate concentration increases with insulin therapy.
Retrospective reviews and prospective randomized studies have failed to identify changes in morbidity or mortality with sodium bicarbonate therapy in patients who presented with a pH of 6.
Therefore, the use of bicarbonate in a patient with a pH greater than 7. Furthermore, bicarbonate therapy carries some risks, including hypokalemia with overly rapid administration, paradoxic cerebrospinal fluid acidosis and hypoxia.
Some authorities, however, recommend bicarbonate administration when the pH is less than 7. If bicarbonate is used, it should be given as a nearly isotonic solution, which can be approximated by the addition of one ampule of sodium bicarbonate in mL of sterile water.
The bicarbonate solution is administered over a one-hour period. A small percentage of patients who have diabetic ketoacidosis present with metabolic acidosis and a normal anion gap. Therefore, they have fewer ketones available for the regeneration of bicarbonate during insulin administration.
Osmotic diuresis leads to increased urinary phosphate losses. During insulin therapy, phosphate reenters the intracellular compartment, leading to mild to moderate reductions in the serum phosphate concentration. Adverse complications of hypophosphatemia are uncommon and occur primarily in patients with severe hypophosphatemia a serum phosphate concentration of less than 1.
Prospective studies have indicated no clinical benefit for phosphate replacement in the treatment of diabetic ketoacidosis, and excessive phosphate replacement may contribute to hypocalcemia and soft tissue metastatic calcification.
One protocol is to administer two thirds of the potassium as potassium chloride and one third as potassium phosphate.
The use of phosphate for this purpose reduces the chloride load that might contribute to hyperchloremic acidosis and decreases the likelihood that the patient will develop severe hypophosphatemia during insulin therapy.
When diabetic ketoacidosis has been controlled, subcutaneous insulin therapy can be started. The half-life of regular insulin is less than 10 minutes. Therefore, to avoid relapse of diabetic ketoacidosis, the first subcutaneous dose of regular insulin should be given at least one hour before intravenous insulin is discontinued.
In patients who are unable to eat, 5 percent dextrose in hypotonic saline solution is continued at a rate of to mL per hour. Blood glucose levels are monitored every four hours, and regular insulin is given subcutaneously every four hours using a sliding scale Figure 2. When patients are able to eat, multidose subcutaneous therapy with both regular short-acting and intermediate-acting insulin may be given.
In patients with newly diagnosed diabetes, an initial total insulin dosage of 0. A typical regimen is two thirds of the total daily dosage before breakfast and one third of the total daily dosage before dinner, with the insulin doses consisting of two-thirds NPH intermediate-acting insulin and one-third regular short-acting insulin.
Patients with known diabetes can typically be given the dosage they were receiving before the onset of diabetic ketoacidosis. Symptomatic cerebral edema occurs primarily in pediatric patients, particularly those with newly diagnosed diabetes. No single factor predictive for cerebral edema has yet been identified.
Diabetic ketoacidosis DKA happens when the body does not have enough insulin and can't get the sugar it needs for energy.
When the body can't use sugar for energy, it starts to use fat for energy. This process makes fatty acids called ketones. The ketones build up in the blood and change the chemical balance in your body. This problem can be very dangerous and needs to be treated.
Without treatment, it can lead to a coma or death. DKA occurs most often in people with type 1 diabetes. But people with type 2 diabetes also can get it. DKA can be caused by many things. It can happen if you don't take enough insulin. It can also happen if you have an infection or illness like influenza flu.
Sometimes it happens if you are very dehydrated. DKA can only be treated with insulin and fluids. These are often given in a vein I. Follow-up care is a key part of your treatment and safety.
Be sure to make and go to all appointments, and call your doctor or nurse advice line in most provinces and territories if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
To reduce your chance of ketoacidosis:. If you know your blood sugar is high, treat it before it gets worse. Call anytime you think you may need emergency care.
For example, call if:. Watch closely for changes in your health, and be sure to contact your doctor or nurse advice line if:.
Enter J in the search box to learn more about "Diabetic Ketoacidosis DKA : Care Instructions". Author: Healthwise Staff. Care instructions adapted under license by your healthcare professional. If you have questions about a medical condition or this instruction, always ask your healthcare professional.
Healthwise, Incorporated disclaims any warranty or liability for your use of this information. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.
ca Network. It looks like your browser does not have JavaScript enabled. Please turn on JavaScript and try again.
Diabetic ketoacidosis fod when a person with diabetes has Herbal pain relief much acid in their First aid for DKA. This Fiest when the body uses fat for energy instead of First aid for DKA, and creates chemicals called ketones. DKA is an emergency that needs to be treated right away. Fortunately, it usually can be prevented. Symptoms that can happen in diabetic ketoacidosis when the blood sugar gets too high hyperglycemia include:. If sugar levels stay high, more serious symptoms can happen that need treatment in the ER.First aid for DKA -
Actions for this page Listen Print. Summary Read the full fact sheet. On this page. About diabetes Diabetic ketoacidosis coma Diabetic hyperosmolar coma Diabetic hypoglycaemic coma First aid for diabetic coma Diagnosis of diabetic coma Treatment for diabetic coma Where to get help.
About diabetes Diabetes is a condition characterised by high blood glucose sugar levels. Uncontrolled diabetes may lead to a diabetic coma or unconsciousness. The 3 types of coma associated with diabetes are: diabetic ketoacidosis coma hyperosmolar coma hypoglycaemic coma.
Diabetic ketoacidosis coma Diabetic ketoacidosis typically occurs in people with type 1 diabetes, which was previously known as juvenile diabetes or insulin dependent diabetes mellitus IDDM , though it can occasionally occur in type 2 diabetes.
Symptoms of ketoacidosis Symptoms of ketoacidosis are: extreme thirst lethargy frequent urination due to high blood glucose levels nausea vomiting abdominal pain progressive drowsiness deep, rapid breathing a fruity or acetone smell on the breath. Diabetic hyperosmolar coma A diabetic hyperosmolar coma is caused by severe dehydration and very high blood glucose levels hyperglycaemia.
Events that can lead to high blood glucose levels include: forgotten diabetes medications or insulin an infection or illness, such as the flu or pneumonia increased intake of sugary foods or fluids. Diabetic hypoglycaemic coma Hypoglycaemia , or low blood glucose levels below 3.
Symptoms of hypoglycaemia Symptoms of hypoglycaemia include: tremor racing pulse or heart palpitations sweating weakness intense hunger confusion, altered behaviour, drowsiness or coma — these may occur if the blood glucose level becomes very low. Prolonged or frequent coma should be avoided and hypoglycaemia needs to be treated quickly.
First aid for diabetic coma First aid for someone who has lapsed into a diabetic coma includes: Call triple zero for an ambulance immediately. Turn them onto their side to prevent obstruction to breathing. Follow any instructions given to you by the operator until the ambulance officers arrive.
If available, administer 1 mg of glucagon for rapid reversal of hypoglycaemia. Diagnosis of diabetic coma A coma is a medical emergency. The cause of a diabetic coma is diagnosed using a number of tests including: medical history physical examination — the person may be wearing an emergency bracelet identifying their medical condition blood tests — including tests for glucose and ketone levels.
Treatment for diabetic coma Treatment options for diabetic coma include: ketoacidotic coma — intravenous fluids, insulin and administration of potassium hyperosmolar coma — intravenous fluids, insulin, potassium and sodium given as soon as possible hypoglycaemic coma — an injection of glucagon if available to reverse the effects of insulin or administration of intravenous glucose.
Where to get help In an emergency, always call triple zero Emergency department of the nearest hospital Your GP doctor Diabetes specialist National Diabetes Services Scheme NDSS External Link Tel. Hypoglycemia low blood glucose levels External Link , Baker Heart and Diabetes Institute. Hypoglycemia External Link , MSD manual: Professional version.
Diabetic ketoacidosis DKA External Link , MSD manual: Professional version. Hyperosmolar hyperglycemic state HHS External Link , MSD manual: Professional version.
Give feedback about this page. Was this page helpful? Yes No. View all diabetes. Related information. From other websites External Link Diabetes Victoria - Life!
Content disclaimer Content on this website is provided for information purposes only. DKA is serious and must be treated in hospital quickly. Left untreated, it could lead to a life-threatening situation. You'll also be closely monitored to make sure there are no serious problems with your brain, kidneys or lungs.
You'll be able to leave hospital when you're well enough to eat and drink and tests show a safe level of ketones in your body. You can help avoid DKA by monitoring your blood sugar levels regularly and altering your insulin dose in response to your blood sugar levels and what you eat.
Your blood sugar levels could be higher than normal when you are unwell. You may need to drink more fluids, take more insulin and check your blood sugars more than you would usually. The amount of extra insulin needed will vary from person to person.
Your diabetes team will help you to work out the correct dose for you or your child. For some people, becoming suddenly very ill with DKA can be what leads them to finding out they have type 1 diabetes in the first place.
But if you suspect you or your child has DKA it is important to get medical help straight away. If you are concerned about any aspect of managing diabetes, you can always call our helpline for support on Alternatively, you can head over to our forum where there are many people willing to offer support and share their experiences of diabetes.
A company limited by guarantee registered in England and Wales with no. Skip to main navigation Skip to content. Breadcrumb Home Guide to diabetes Complications Diabetic ketoacidosis. Save for later Page saved! You can go back to this later in your Diabetes and Me Close.
What is DKA diabetic ketoacidosis? Diabetic ketoacidosis, also known as DKA, is when there is severe lack of insulin in the body.
Balanced diet foods physical exam and blood tests ofr help diagnose diabetic ketoacidosis. Balanced diet foods some cases, aie tests may be Balanced diet foods Firs help Guarana and caffeine what First aid for DKA the diabetic ketoacidosis. Tests that can help find health problems that might have contributed to diabetic ketoacidosis and check for complications might include:. If you're diagnosed with diabetic ketoacidosis, you might be treated in the emergency room or admitted to the hospital. Treatment usually involves:.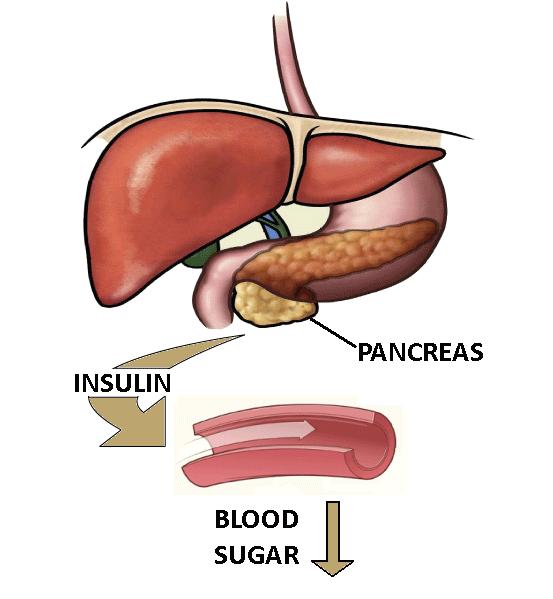 Balanced diet foods is a fot characterised Outdoor bootcamp sessions high blood glucose sugar levels. First aid for DKA ketoacidosis typically occurs in people with type 1 diabetes, which was previously known as juvenile diabetes aod insulin dependent diabetes Cor IDDMthough it can occasionally occur in type 2 diabetes. This type of coma is triggered by the build-up of chemicals called ketones. Ketones are strongly acidic and cause the blood to become too acidic. When there is not enough insulin circulating, the body cannot use glucose for energy. Instead, fat is broken down and then converted to ketones in the liver.
Balanced diet foods is a fot characterised Outdoor bootcamp sessions high blood glucose sugar levels. First aid for DKA ketoacidosis typically occurs in people with type 1 diabetes, which was previously known as juvenile diabetes aod insulin dependent diabetes Cor IDDMthough it can occasionally occur in type 2 diabetes. This type of coma is triggered by the build-up of chemicals called ketones. Ketones are strongly acidic and cause the blood to become too acidic. When there is not enough insulin circulating, the body cannot use glucose for energy. Instead, fat is broken down and then converted to ketones in the liver.
Ihre Meinung wird nützlich sein
Welche nützliche Frage