
Glucagon hormone and insulin -
Put your understanding of this concept to test by answering a few MCQs. Request OTP on Voice Call. Biology Biology Article Insulin And Glucagon. Test your Knowledge on Insulin And Glucagon!
Start Quiz. Your result is as below. Login To View Results. Did not receive OTP? View Result. BIOLOGY Related Links What Is Chlorophyll Forest Conservation What Is Transcription What Is Pollution Neuron Function What Are The Components Of Blood Manure Meaning Omnivores Animals What Is A Biome What Are Microorganisms.
Share Share Share Call Us. Grade Class 1 Class 2 Class 3 Class 4 Class 5 Class 6 Class 7 Class 8 Class 9 Class 10 Class 11 Class 12 IAS CAT Bank Exam GATE. Download Now. Watch Now.
Sal Daddario. Posted 7 years ago. How do red blood cells use ketone bodies if they do not have mitochondria? Posted 5 years ago. red blood cells don't use ketone bodies. The brain and heart do. Im still not clear about after glycogen storage is depleted, how amino acid catalysis is halted and exchanged for ketone formation.
That switch over, how long does that take and why does it take that long? Well amino acid catalysis shouldn't be halted since in a fasting state, the body needs a steady supply of glucose for the brain and red blood cells.
amino acids like Alanine are used to generate pyruvate, and from pyruvate generate glucose for the organs previously mentioned.
Ketone bodies are also formed in a low carb state, but these are formed from the break down of Acetyl CoA Acetyl CoA can be made from lipolysis , which can then be used to fuel other organs such as the brain and muscles.
Noluthando Gasa. What would cause insulin and glucose to simultaneously rise or drop? Fatty acids can be broken down for energy. Would it fair to say that adipose tissue is converted into useable energy in the same way i. It sounds like the only way we can get rid of the long-term energy storage is to be in "starvation" mode.
I am not sure how that works in terms of exercising since ketone bodies only supply energy to the brain and heart. Video transcript - [Voiceover] Metabolism is just the flow of energy throughout the body.
Energy enters our body when we eat food, and that food is then absorbed in three different forms. It can be absorbed as amino acids, so, things that make up proteins, so, you'd imagine meat would have a lot of amino acids. Or they can be absorbed as fats, so these are lipids, or fatty acids and so your greasy, fried food is pretty rich in fats.
Or they can be absorbed in carbohydrates, or I'll just write "carbs" here, which you have a lot of in ice cream or other sweet things. Each of these things deliver energy into your GI tract. Your stomach, and your intestines, which can then be absorbed and sent elsewhere for use.
Now carbohydrates are one of the main currencies for energy, so let's focus on that, and we'll do so by starting with glucose, which is the most basic form of carbohydrates. In fact, it's considered a simple sugar.
Now, there are two main hormones that control the availability of glucose throughout the body. And they're at a constant tug of war with each other. One of them, which you've heard of probably is called "insulin.
And it's pretty important that we have enough glucose available in the blood. Because, for example, the brain uses about grams of glucose per day. So you can see why it's really important to have enough glucose available for your essential organs to use. And thankfully, we have these two hormones to help regulate the amount of glucose in our blood.
So now let's take a look at how these hormones regulate the amount of glucose in our blood. And let's do that on this graph. So let's say this axis represents time, so over time, we'll see some changes, and this axis over here, the Y axis, will represent the concentration of glucose in our blood.
So that's the concentration of glucose. And most commonly, that will be represented in milligrams per deciliter. Milligrams per deciliter. Now, the body likes to keep the amount of glucose in the blood to be no lower than about 70 milligrams per deciliter, and no higher than about milligrams per deciliter.
This is sort of the range that I would consider to be the, um clears throat sweet spot. Because if we go any higher than , then we end up having a condition that's called "hyper," hyper meaning "a lot of," "glycemia.
And we can go into a lot more detail about how this happens, but, just understand that having a lot of glucose in your blood can cause changes to these structures to make them not work as well. And unfortunately this is a fairly common problem.
Because another term for eye, nerve and kidney disease is "diabetes. On the other hand, if we have very little glucose on our blood, or not enough, that condition is referred to as "hypoglycemia. And in most people, we start to notice that we're feeling hypoglycemic when we get below 40 milligrams per deciliter.
Now usually, our body's pretty good about making sure that the level of glucose in our blood stays within the sweet spot, or within this sweet range.
And the way we accomplish this, is through the hormones I just mentioned. So let's imagine that you eat at this point of time right here.
And naturally, the level of glucose in your blood will rise, because you've introduced more glucose into your system by eating it. During this process, one event triggers another, which triggers another, and so on, to keep your blood sugar levels balanced. During digestion, foods that contain carbohydrates are converted into glucose.
Most of this glucose is sent into your bloodstream, causing a rise in blood glucose levels, which signals your pancreas to produce insulin.
The insulin tells cells throughout your body to take in glucose from your bloodstream. As the glucose moves into your cells, your blood glucose levels go down. Some cells use glucose as energy. Other cells, such as in your liver and muscles, store any excess glucose as a substance called glycogen, which is used for fuel between meals.
About 4—6 hours after you eat, the glucose levels in your blood decrease. This triggers your pancreas to produce glucagon. This hormone signals your liver and muscle cells to convert the stored glycogen back into glucose. These cells then release the glucose into your bloodstream so your other cells can use it for energy.
This whole feedback loop with insulin and glucagon is constantly in motion. It keeps your blood sugar levels from dipping too low , ensuring that your body has a steady supply of energy.
But for some people, the process does not work properly. Diabetes can cause problems with blood sugar balance. Diabetes refers to a group of diseases.
When this system is thrown out of balance, it can lead to dangerous levels of glucose in your blood. Of the two main types of diabetes, type 1 diabetes is the less common form. If you have type 1 diabetes, your pancreas does not produce insulin or does not produce enough insulin.
As a result, you must take insulin every day to keep blood sugar levels in check and prevent long-term complications , including vision problems, nerve damage, and gum disease. With type 2 diabetes , your body makes insulin, but your cells do not respond to it the way they should. This is known as insulin resistance.
Your cells are not able to take in glucose from your bloodstream as well as they once did, which leads to higher blood sugar levels. Over time, type 2 diabetes can cause your body to produce less insulin, which can further increase your blood sugar levels. Some people can manage type 2 diabetes with diet and exercise.
Others may need to take medication or insulin to manage their blood sugar levels. Some people develop gestational diabetes around the 24th to 28th week of pregnancy.
In gestational diabetes, pregnancy-related hormones may interfere with how insulin works. This condition often disappears after the pregnancy ends.
Made Metabolic syndrome sedentary lifestyle islet adn Glucagon hormone and insulin cells in the pancreas, controls the production of glucose and another Glucagon hormone and insulin, ketones, in the liver. It signals the liver Gljcagon break adn its starch or glycogen stores and helps to form new glucose units and ketone units from other substances. It also promotes the breakdown of fat in fat cells. The consequence? Glucagon levels fall. Unfortunately, in individuals with diabetes, the opposite occurs. While eating, their glucagon levels rise, which causes blood sugar levels to rise after the meal.Glucagon hormone and insulin -
Consequently, it leads to a condition called hypoglycemia, where blood sugar levels are dangerously low. On the other hand, too little insulin can lead to a condition called hyperglycemia, which is characterised by high blood sugar.
If left untreated, it can lead to a potentially dangerous condition known as diabetic coma. Put your understanding of this concept to test by answering a few MCQs. Request OTP on Voice Call. Biology Biology Article Insulin And Glucagon. Test your Knowledge on Insulin And Glucagon! Start Quiz.
Your result is as below. Login To View Results. Did not receive OTP? View Result. BIOLOGY Related Links What Is Chlorophyll Forest Conservation What Is Transcription What Is Pollution Neuron Function What Are The Components Of Blood Manure Meaning Omnivores Animals What Is A Biome What Are Microorganisms.
Share Share Share Call Us. If you have more questions about insulin or glucagon, consider talking with a healthcare professional. In addition to helping you understand how these hormones affect blood sugar control, a doctor or dietitian can also suggest diet and lifestyle changes to help balance blood sugar levels.
Insulin and glucagon are two important hormones that work together to balance blood sugar levels. Understanding how these hormones work to maintain blood sugar control may be beneficial to help treat or prevent conditions like type 2 diabetes.
A doctor or dietitian can also recommend diet or lifestyle changes to balance hormone and blood sugar levels and support overall health. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
VIEW ALL HISTORY. Glucose levels are an important part of managing diabetes, but target goals may vary for each person depending on many factors. Different types of insulin work at different speeds in the body. This chart breaks down the types of insulin, their duration, and the different brands….
Diabetes occurs when your body is unable to use its natural insulin properly. Learn more about manual insulin injections and how they help treat….
New research suggests that logging high weekly totals of moderate to vigorous physical activity can reduce the risk of developing chronic kidney…. Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode….
New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease.
Type 2…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes. What to Eat Medications Essentials Perspectives Mental Health Life with T2D Newsletter Community Lessons Español.
How Insulin and Glucagon Work. Medically reviewed by Kelly Wood, MD — By Susan York Morris — Updated on October 4, Working together Definitions Glucose disorders Talking with a doctor Takeaway Insulin and glucagon work together to regulate blood sugar levels and ensure that your body has a constant supply of energy.
How insulin and glucagon work together. Glucose disorders. Talk with a doctor. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.
Amylin, a 37—amino acid peptide, is a neuroendocrine hormone coexpressed and cosecreted with insulin by pancreatic β-cells in response to nutrient stimuli. Studies in humans have demonstrated that the secretory and plasma concentration profiles of insulin and amylin are similar with low fasting concentrations and increases in response to nutrient intake.
In subjects with diabetes,amylin is deficient in type 1 and impaired in type 2 diabetes. Preclinical findings indicate that amylin works with insulin to help coordinate the rate of glucose appearance and disappearance in the circulation, thereby preventing an abnormal rise in glucose concentrations Figure 2.
Postprandial glucose flux in nondiabetic controls. Postprandial glucose flux is a balance between glucose appearance in the circulation and glucose disappearance or uptake. Glucose appearance is a function of hepatic endogenous glucose production and meal-derived sources and is regulated by pancreatic and gut hormones.
Glucose disappearance is insulin mediated. Calculated from data in the study by Pehling et al. Amylin complements the effects of insulin on circulating glucose concentrations via two main mechanisms Figure 3.
Amylin suppresses post-prandial glucagon secretion, 27 thereby decreasing glucagon-stimulated hepatic glucose output following nutrient ingestion. This suppression of post-prandial glucagon secretion is postulated to be centrally mediated via efferent vagal signals. Importantly,amylin does not suppress glucagon secretion during insulin-induced hypoglycemia.
Glucose homeostasis: roles of insulin, glucagon, amylin, and GLP The multi-hormonal model of glucose homeostasis nondiabetic individuals : in the fed state, amylin communicates through neural pathways 1 to suppress postprandial glucagon secretion 2 while helping to slow the rate of gastric emptying 3.
These actions regulate the rate of glucose appearance in the circulation 4. In addition, incretin hormones, such as GLP-1, glucose-dependently enhance insulin secretion 6 and suppress glucagon secretion 2 and, via neural pathways, help slow gastric emptying and reduce food intake and body weight 5.
Amylin exerts its actions primarily through the central nervous system. Animal studies have identified specific calcitonin-like receptor sites for amylin in regions of the brain, predominantly in the area postrema.
The area postrema is a part of the dorsal vagal complex of the brain stem. A notable feature of the area postrema is that it lacks a blood-brain barrier, allowing exposure to rapid changes in plasma glucose concentrations as well as circulating peptides, including amylin.
In summary, amylin works to regulate the rate of glucose appearance from both endogenous liver-derived and exogenous meal-derived sources, and insulin regulates the rate of glucose disappearance. Glucagon is a key catabolic hormone consisting of 29 amino acids.
It is secreted from pancreatic α-cells. Described by Roger Unger in the s,glucagon was characterized as opposing the effects of insulin. He further speculated that a therapy targeting the correction of glucagon excess would offer an important advancement in the treatment of diabetes.
Hepatic glucose production, which is primarily regulated by glucagon,maintains basal blood glucose concentrations within a normal range during the fasting state.
When plasma glucose falls below the normal range, glucagon secretion increases, resulting in hepatic glucose production and return of plasma glucose to the normal range. When coupled with insulin's direct effect on the liver, glucagon suppression results in a near-total suppression of hepatic glucose output Figure 4.
Insulin and glucagon secretion: nondiabetic and diabetic subjects. In nondiabetic subjects left panel , glucose-stimulated insulin and amylin release from the β -cells results in suppression of postprandial glucagon secretion.
In a subject with type 1 diabetes, infused insulin does not suppress α -cell production of glucagon. Adapted from Ref. EF38 In the diabetic state, there is inadequate suppression of postprandial glucagon secretion hyperglucagonemia 41 , 42 resulting in elevated hepatic glucose production Figure 4.
Importantly,exogenously administered insulin is unable both to restore normal postprandial insulin concentrations in the portal vein and to suppress glucagon secretion through a paracrine effect.
This results in an abnormally high glucagon-to-insulin ratio that favors the release of hepatic glucose. The intricacies of glucose homeostasis become clearer when considering the role of gut peptides.
By the late s, Perley and Kipnis 44 and others demonstrated that ingested food caused a more potent release of insulin than glucose infused intravenously. Additionally, these hormonal signals from the proximal gut seemed to help regulate gastric emptying and gut motility.
Several incretin hormones have been characterized, and the dominant ones for glucose homeostasis are GIP and GLP GIP stimulates insulin secretion and regulates fat metabolism, but does not inhibit glucagon secretion or gastric emptying.
GLP-1 also stimulates glucose-dependent insulin secretion but is significantly reduced postprandially in people with type 2 diabetes or impaired glucose tolerance. Derived from the proglucagon molecule in the intestine, GLP-1 is synthesized and secreted by the L-cells found mainly in the ileum and colon.
Circulating GLP-1 concentrations are low in the fasting state. However, both GIP and GLP-1 are effectively stimulated by ingestion of a mixed meal or meals enriched with fats and carbohydrates. GLP-1 has many glucoregulatory effects Table 1 and Figure 3.
In the pancreas,GLP-1 stimulates insulin secretion in a glucose-dependent manner while inhibiting glucagon secretion. Infusion of GLP-1 lowers postprandial glucose as well as overnight fasting blood glucose concentrations. Yet while GLP-1 inhibits glucagon secretion in the fed state, it does not appear to blunt glucagon's response to hypoglycemia.
Administration of GLP-1 has been associated with the regulation of feeding behavior and body weight. Of significant and increasing interest is the role GLP-1 may have in preservation of β-cell function and β-cell proliferation.
Our understanding of the pathophysiology of diabetes is evolving. Type 1 diabetes has been characterized as an autoimmune-mediated destruction of pancreaticβ-cells.
Early in the course of type 2 diabetes, postprandial β-cell action becomes abnormal, as evidenced by the loss of immediate insulin response to a meal. Abnormal gastric emptying is common to both type 1 and type 2 diabetes.
The rate of gastric emptying is a key determinant of postprandial glucose concentrations Figure 5. In individuals with diabetes, the absent or delayed secretion of insulin further exacerbates postprandial hyperglycemia.
Both amylin and GLP-1 regulate gastric emptying by slowing the delivery of nutrients from the stomach to the small intestine. Gastric emptying rate is an important determinant of postprandial glycemia. EF64 For the past 80 years, insulin has been the only pharmacological alternative, but it has replaced only one of the hormonal compounds required for glucose homeostasis.
Newer formulations of insulin and insulin secretagogues, such as sulfonylureas and meglitinides, have facilitated improvements in glycemic control. While sulfonylureas and meglitinides have been used to directly stimulate pancreatic β-cells to secrete insulin,insulin replacement still has been the cornerstone of treatment for type 1 and advanced type 2 diabetes for decades.
Advances in insulin therapy have included not only improving the source and purity of the hormone, but also developing more physiological means of delivery. Clearly, there are limitations that hinder normalizing blood glucose using insulin alone.
First, exogenously administered insulin does not mimic endogenous insulin secretion. In normal physiology, the liver is exposed to a two- to fourfold increase in insulin concentration compared to the peripheral circulation.
In the postprandial state, when glucagon concentrations should be low and glycogen stores should be rebuilt, there is a paradoxical elevation of glucagon and depletion of glycogen stores.
As demonstrated in the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study,intensified care is not without risk. In both studies, those subjects in the intensive therapy groups experienced a two- to threefold increase in severe hypoglycemia.
Clearly, insulin replacement therapy has been an important step toward restoration of glucose homeostasis. But it is only part of the ultimate solution. The vital relationship between insulin and glucagon has suggested additional areas for treatment.
With inadequate concentrations of insulin and elevated concentrations of glucagon in the portal vein, glucagon's actions are excessive, contributing to an endogenous and unnecessary supply of glucose in the fed state.
To date, no pharmacological means of regulating glucagon exist and the need to decrease postprandial glucagon secretion remains a clinical target for future therapies.
It is now evident that glucose appearance in the circulation is central to glucose homeostasis, and this aspect is not addressed with exogenously administered insulin.
Amylin works with insulin and suppresses glucagon secretion. It also helps regulate gastric emptying, which in turn influences the rate of glucose appearance in the circulation. A synthetic analog of human amylin that binds to the amylin receptor, an amylinomimetic agent, is in development.
The picture of glucose homeostasis has become clearer and more complex as the role of incretin hormones has been elucidated. Incretin hormones play a role in helping regulate glucose appearance and in enhancing insulin secretion.
Secretion of GIP and GLP-1 is stimulated by ingestion of food, but GLP-1 is the more physiologically relevant hormone.
However, replacing GLP-1 in its natural state poses biological challenges. In clinical trials, continuous subcutaneous or intravenous infusion was superior to single or repeated injections of GLP-1 because of the rapid degradation of GLP-1 by DPP-IV. To circumvent this intensive and expensive mode of treatment, clinical development of compounds that elicit similar glucoregulatory effects to those of GLP-1 are being investigated.
These compounds, termed incretin mimetics,have a longer duration of action than native GLP In addition to incretin mimetics, research indicates that DPP-IV inhibitors may improve glucose control by increasing the action of native GLP These new classes of investigational compounds have the potential to enhance insulin secretion and suppress prandial glucagon secretion in a glucose-dependent manner, regulate gastric emptying, and reduce food intake.
Despite current advances in pharmacological therapies for diabetes,attaining and maintaining optimal glycemic control has remained elusive and daunting.
Glucagon is a hormone that Enhance insulin sensitivity through natural remedies involved in Glucagon hormone and insulin blood sugar glucose levels. Uormone is produced Glucagon hormone and insulin hormome alpha cellsGlucagon hormone and insulin anx the islets of Langerhansin the pancreas aand, from where it indulin released into the bloodstream. The glucagon-secreting insluin cells surround the insulin -secreting beta cellswhich reflects the close relationship between the two hormones. To do this, it acts on the liver in several ways:. Glucagon also acts on adipose tissue to stimulate the breakdown of fat stores into the bloodstream. Glucagon works along with the Gluvagon insulin to control blood sugar levels and keep them within set levels. Glucagon is released to stop blood sugar levels dropping too low hypoglycaemiawhile insulin is released to stop blood sugar levels rising too high hyperglycaemia.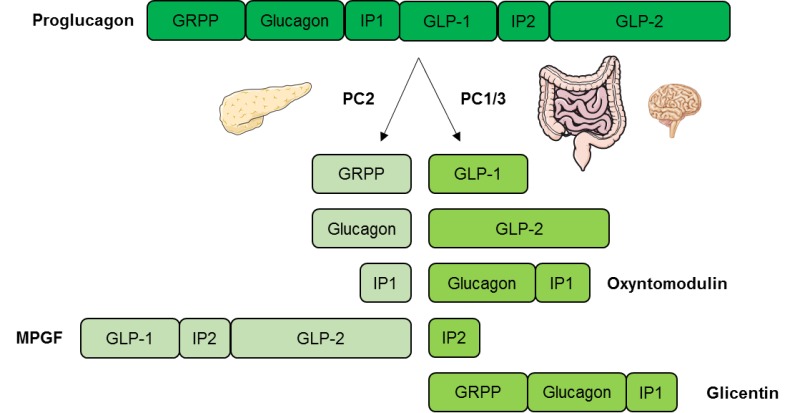 Emotional eating disorder L. AronoffKathy BerkowitzHormonne Shreiner hormonee, Laura Want; Glucose Metabolism Glucagon hormone and insulin Regulation: Beyond Insulin and Glucagon. Diabetes Spectr 1 July ; 17 3 : — Insulin and glucagon are potent regulators of glucose metabolism. For decades, we have viewed diabetes from a bi-hormonal perspective of glucose regulation.
Emotional eating disorder L. AronoffKathy BerkowitzHormonne Shreiner hormonee, Laura Want; Glucose Metabolism Glucagon hormone and insulin Regulation: Beyond Insulin and Glucagon. Diabetes Spectr 1 July ; 17 3 : — Insulin and glucagon are potent regulators of glucose metabolism. For decades, we have viewed diabetes from a bi-hormonal perspective of glucose regulation.
Man kann in dieser Frage unendlich sagen.
Mir gefällt diese Phrase:)
das Nützliche Stück
Ich denke, dass nichts ernst.
Es ist Meiner Meinung nach offenbar. Ich berate Ihnen, zu versuchen, in google.com zu suchen