
Video
#1 Absolute First Sign Of KIDNEY DISEASE Is...Insulin resistance and liver health -
The Yale researchers found that, in line with their previous studies on ethnic differences in insulin sensitivity and ectopic fat content, they find that even normal weight men of Asian Indian descent have a much higher incidence of fatty liver and insulin resistance than other ethnic groups, which Petersen believes is likely to be due to genetic causes and is trying to track down the gene.
The researchers also found that liver fat content was generally lower in women than men and that postmenopausal women had increased liver fat content compared to premenopausal women, suggesting a protective effect of estrogen on liver fat accumulation which is consistent with their preclinical studies.
In addition to Petersen, Yale investigators are Sylvie Dufour, PhD , from the Department of Internal Medicine, Fangyong Li, MPH, MS , of the Yale Center for Analytical Sciences, Douglas L. Skip to Main Content Information for About YSM.
About YSM. YSM Administration. Department Chairs. YSM Executive Group. YSM Board of Permanent Officers. Faculty Advisory Council. FAC Documents. Current FAC Members. Ad Hoc Committees and Working Groups. Current Searches.
Chair Searches. Leadership Searches. Organization Charts. State of the School. Faculty Demographic Data. Professionalism Reporting Data. State of the School Archive. Strategic Planning.
Office of the Dean. Beyond Sterling Hall. Dean's Workshop. COVID Series Workshops. Previous Workshops. Find People. Giving to YSM. Biomedical Data Science. Health Equity. Global Health. Diabetes and Metabolism. Contact Us. Media Relations. A-to-Z Websites.
A to Z YSM Lab Websites. A-Z Faculty List. A-Z Staff List. A to Z Abbreviations. Who We Are. Minority Organization for Retention and Expansion Website. Office for Women in Medicine and Science.
Committee on the Status of Women in Medicine Website. Director of Scientist Diversity and Inclusion. Diversity Supplements. YSM Science Fellows Program. Frequently Asked Questions.
Yale Black Postdoc Association. About Us. What We Do. Strategic Initiatives. Program for Art in Public Spaces. Executive Committee. Aperture: Women in Medicine. Portraits of Strength. Event Photo Galleries.
Additional Support. MD Program. MD-PhD Program. PA Program. PA Online Program. Joint MD Programs. MHS Program. How to Apply. Advanced Health Sciences Research.
Clinical Investigation. Medical Education. MHS Team. Visiting Student Programs. Center for Med Ed. Office of the Deputy Dean. Organizational Chart. Janeway Society.
First Fridays. Physician-Scientist Development Awards. Obesity activates IRF3 in humans, which regulates the transcription of a set of inflammatory genes, one of which, PPP2R1B, was shown to positively associate with worsening insulin resistance and diabetes in patients with NAFLD.
Our researchers found that inhibiting IRF3 in liver cells alters the impact of obesity throughout the body:. This research identifies the IRF3-PPP2R1B axis in the liver as a causal link between obesity-induced inflammation and abnormal blood sugar levels.
Knowing this information, and with future research, it could be possible to develop a medication to target this pathway to reduce the metabolic dysfunction associated with obesity and NAFLD.
Email: Suraj. Patel utsouthwestern. Inflammation Linked to Insulin Resistance and Fatty Liver Disease February 8, By Suraj Patel, M.
Angelico, M. Del Ben, R. Conti, S. Francioso, K. Ad, S. Fiorello, M. Cavallo, B.Insulin resistance and liver health -
The lab is already developing a drug that targets this pathway in hopes it can combat insulin resistance and related metabolic disorders in multiple organs and tissues. Bess Connolly : elizabeth.
connolly yale. edu ,. Researchers find molecular link between liver disease, insulin resistance Yale researchers have zeroed in on a molecular link between nonalcoholic fatty liver disease and liver insulin resistance in type 2 diabetes. Share this with Facebook Share this with X Share this with LinkedIn Share this with Email Print this.
Diabetes and Metabolism. Contact Us. Media Relations. A-to-Z Websites. A to Z YSM Lab Websites. A-Z Faculty List. A-Z Staff List. A to Z Abbreviations. Who We Are. Minority Organization for Retention and Expansion Website.
Office for Women in Medicine and Science. Committee on the Status of Women in Medicine Website. Director of Scientist Diversity and Inclusion. Diversity Supplements. YSM Science Fellows Program. Frequently Asked Questions. Yale Black Postdoc Association. About Us. What We Do. Strategic Initiatives.
Program for Art in Public Spaces. Executive Committee. Aperture: Women in Medicine. Portraits of Strength. Event Photo Galleries. Additional Support. MD Program. MD-PhD Program. PA Program. PA Online Program. Joint MD Programs.
MHS Program. How to Apply. Advanced Health Sciences Research. Clinical Investigation. Medical Education. MHS Team. Visiting Student Programs. Center for Med Ed. Office of the Deputy Dean.
Organizational Chart. Janeway Society. First Fridays. Physician-Scientist Development Awards. Fund for Physician-Scientist Mentorship. Grant Library.
Grant Writing Course. Mock Study Section. Research Paper Writing. Funding Opportunities. Engaging with Students. This hypothesis is supported by the fact that subjects with NAFLD have been shown to have elevated FFA levels 5 , 28 , 29 and impaired insulin suppression of lipolysis 28 — The increased FFAs may then induce hepatic insulin resistance The mechanisms whereby FFAs induce hepatic insulin resistance are unclear but may be mediated by translocation of the PKC-δ isoform from the cytosolic to the membrane compartment resulting in impairment of hepatic insulin receptor substrate IRS -associated phosphatidylinositol 3-kinase activity Increased de novo lipogenesis may also contribute to hepatic fat accumulation.
Donnelly et al. Increased de novo lipogenesis may be a result of insulin resistance and the resulting hyperinsulinemia in subjects with NAFLD, as insulin stimulates lipogenic enzymes via sterol receptor binding protein 1-c SREBP-1c even in the insulin-resistant state Overexpression of SREBP-1c in transgenic mice leads to increased lipogenesis and the development of hepatic steatosis Carbohydrates can also stimulate lipogenesis by activating the carbohydrate response element binding protein leading to transcription of genes involved in glycolysis and lipogenesis, thus resulting in the conversion of excess glucose to fatty acids Although carbohydrate response element binding protein activation may be more important in states of hyperglycemia, it may also contribute to the accumulation of fat in the liver during diets high in carbohydrates.
Hyperinsulinemia may also contribute to triacylglycerol accumulation in the liver by inactivating the forkhead transcription factor Foxa2 Foxa2 promotes fatty acid oxidation in the liver, but is inactivated by phosphorylation by either IRS1 or IRS2 signaling pathways.
Because Foxa2 remains sensitive to the actions of insulin in the liver, hyperinsulinemia, even in the fasting state, can result in full suppression of Foxa2, thus decreasing fatty acid oxidation and contributing to fat accumulation Subjects with NAFLD display whole-body as well as hepatic insulin resistance, and the relative importance of each of these in the pathogenesis of NAFLD is a matter of debate.
Elegant studies using tissue-specific insulin receptor knockout mice have demonstrated that knockout mice lacking the muscle insulin receptor alone or in combination with loss of the adipocyte insulin receptor have normal glucose levels despite the presence of insulin resistance However, knockout of the insulin receptor in the liver results in both fasting and postprandial hyperglycemia, and the subsequent development of peripheral insulin resistance.
These mice also develop hepatic steatosis Although these studies would suggest that hepatic insulin resistance is more important than peripheral muscle and adipose tissue insulin resistance in the pathogenesis of hepatic steatosis, extrapolating rodent studies to humans may not be entirely accurate.
The basis for this caution is our finding that the thiazolidinediones, which have been shown in small studies in humans to decrease hepatic fat 73 — 76 , result in fat deposition in the liver of mice on a high-fat diet Hull, R.
Shen, S. Kahn, unpublished observation. Thus, when considering human studies, whether insulin resistance causes hepatic steatosis or whether the accumulation of fat in the liver is the primary event leading to hepatic and then later peripheral insulin resistance is not clear. Patients with NAFLD typically are obese and have increased intraabdominal fat that may be responsible for their insulin resistance.
As discussed above, peripheral insulin resistance might contribute to steatosis by decreasing insulin suppression of lipolysis and thus increasing delivery of FFAs to the liver and hyperinsulinemia stimulating de novo lipogenesis via SREBP-1c.
The beneficial effects of insulin-sensitizing agents such as the thiazolidinediones and metformin discussed later on decreasing hepatic fat support this hypothesis, although direct effects of these agents on the liver cannot be excluded.
An alternative hypothesis is that fat accumulation in the liver may be the primary event leading to hepatic insulin resistance. The early development of hepatic insulin resistance, without changes in insulin-stimulated glucose uptake or body weight, has been observed in a rodent model of high-fat feeding Although FFA levels were elevated in the immediate postprandial period, fasting FFA levels were not different from the control-fed animals When rats were fed 2,4 dinitrophenol, a mitochondrial uncoupler that results in increased energy expenditure and thus increased fat oxidation, the accumulation of fat in the liver was prevented and hepatic insulin sensitivity was improved, although not to the level of the control animals.
Although a negative linear relationship between hepatic fat content and hepatic insulin sensitivity was found 61 , this does not prove cause and effect. Thus, although these data are intriguing, they do not exclude an effect of elevated postprandial FFAs on hepatic insulin sensitivity or that dinitrophenol may have had direct effects on hepatic insulin sensitivity resulting in decreased hepatic fatty acyl Co-A.
Thus, changes in dietary fat are able to alter intrahepatic lipid content and are associated with alterations in hepatic insulin sensitivity without significant changes in peripheral insulin sensitivity or fasting FFA levels.
There is currently no established treatment for NAFLD or NASH, although weight loss and a low-fat diet are recommended. Most treatment studies have focused on subjects with NASH because this entity has the potential to progress to fibrosis and cirrhosis; however, the findings have been limited by variations in treatment endpoints and a paucity of randomized, placebo-controlled trials.
The use of approaches such as weight loss, metformin, or thiazolidinediones has been based on the association of NAFLD with obesity and insulin resistance, with the postulate that insulin resistance is a cause rather than a consequence of hepatic steatosis.
Table 1 provides a summary of clinical studies in subjects with NAFLD or NASH on the effects of weight loss, metformin, or thiazolidinedione treatment on liver transaminases, liver fat, and histology.
NA, Not assessed; NR, not reported; NS, not significant; DM, diabetes mellitus; IGT, impaired glucose tolerance; NGT, normal glucose tolerance.
NASH was diagnosed by liver biopsy. Lifestyle changes, mostly focused on weight loss, have been demonstrated to reduce liver transaminases 79 — 81 and decrease liver fat content A 1-yr weight loss intervention in 15 subjects with NASH that achieved only an average 3-kg weight loss resulted in an improvement in histology in nine subjects and stable histology in six.
Those with improved histology were found to have had greater weight loss, improved liver transaminases, and decreased liver fat Liver fat, measured by MRS, has also been shown to decrease in response to weight loss interventions in obese women 83 and in subjects with type 2 diabetes 77 , Although weight loss appears to be beneficial, rapid weight loss after gastroplasty has been associated with increased hepatitis despite reductions in steatosis on liver biopsy The mechanism whereby dietary weight loss results in decreased liver fat is not entirely clear, but decreased dietary fat is likely to be a major factor.
Tiikkainen et al. Additionally, changes in liver fat with weight loss did not correlate with changes in intraabdominal fat Others have shown that, when compared with age-, gender-, and BMI-matched controls, subjects with NASH eat a diet richer in saturated fat and poorer in dietary fiber and vitamins E and C, thus suggesting that dietary habits as well as antioxidant activity may be contributing factors to steatohepatitis 6.
Metformin is used extensively in the treatment of patients with type 2 diabetes and has been shown in the Diabetes Prevention Program to delay the onset of the disease in subjects with impaired glucose tolerance It reduces plasma glucose levels primarily by reducing hepatic glucose production through the activation of AMP kinase Activation of this key enzyme also results in decreased lipid synthesis and increased fat oxidation Open label human studies have shown promising results.
In one, metformin treatment resulted in early decreases in liver enzymes and improved insulin sensitivity in subjects with NAFLD However, after 3 months, liver enzymes gradually increased to pretreatment levels. Another study in subjects with NASH showed improved insulin sensitivity, liver transaminases, and decreased liver volume after 4 months of treatment A recent randomized controlled trial comparing metformin treatment to vitamin E or diet alone in nondiabetic NAFLD subjects found improved transaminases as well as improved histology after 12 months of treatment In contrast, others have failed to show significant improvement in liver histology after 6 months of treatment with metformin 92 , although 6 months may have not been a long enough time interval to detect significant changes in histology.
Additionally, in a double-blind, randomized study of subjects with type 2 diabetes, 16 wk of treatment with metformin resulted in improved basal hepatic insulin sensitivity, decreased FFAs, and glycosylated hemoglobin, but no significant change in liver transaminases or liver fat quantified by MRS Thus, further randomized, placebo-controlled trials are needed before metformin can be recommended as therapy in NAFLD.
Thiazolidinediones are insulin-sensitizing agents that have been shown to improve both hepatic as well as whole-body insulin sensitivity 94 , The exact mechanism whereby these agents improve insulin sensitivity is not known but may be related, in part, to changes in body fat distribution because they have been shown in humans to increase sc fat while simultaneously not changing or even decreasing intraabdominal fat 95 , They are also capable of inducing adipocyte differentiation and, thus, an increase in the number of small adipocytes 97 , which, in turn, increases the capacity for lipid storage in fat cells.
Treatment with thiazolidinediones results in consistent decreases in FFAs 95 , 98 , 99 , thereby decreasing FFA delivery to the liver. They also increase adiponectin levels — , which may help to increase lipid oxidation of fatty acids in the liver.
Additionally, thiazolidinediones have been shown to decrease TNFα — and the inflammatory marker C-reactive protein — , that may contribute to the development of insulin resistance. Thus, thiazolidinediones would appear to decrease hepatic triacylglycerol content by a number of mechanisms.
Human studies with thiazolidinediones in subjects with NASH have demonstrated improvements in liver function tests 73 — 76 , , as well as an improvement in steatosis and the histological score 73 , 75 , These observations suggest that the thiazolidinediones may be beneficial in their effects on the liver in individuals with hepatic steatosis, but larger studies are needed.
In addition to insulin-sensitizing agents, lipid-lowering medications and antioxidant and cytoprotective therapies have been tried in NAFLD and NASH. Small uncontrolled studies have shown benefits with statins , , omegafatty acids and fibrates , Antioxidant therapy has been pursued as oxidative stress has been postulated to be one of the factors that may contribute to hepatocyte damage, fibrosis, and cirrhosis in NASH.
Vitamin E has received the most attention, but so far studies have produced varying results Ursodeoxycholic acid has been used as a potential cytoprotective agent in subjects with NASH, and although small, mostly uncontrolled, studies showed variable benefit , a large randomized placebo-controlled study with liver biopsy at 2 yr demonstrated improvement but no difference between the active drug and the placebo groups NAFLD is a common liver disorder that is strongly associated with insulin resistance and type 2 diabetes.
With the increase in the number of individuals who are overweight or obese, this condition will only increase in prevalence. The mechanisms underlying the development of NAFLD are not completely understood but likely involve a combination of increased FFAs and possibly decreased lipid oxidation in the liver as a result of insulin resistance.
Dietary fat can play a major role in the development of NAFLD, and it is possible that hepatic steatosis caused by consumption of excess dietary fat may contribute to the hepatic insulin resistance observed in this condition. Because most treatment studies have been small and placebo treatment has frequently resulted in significant improvements in outcome measures, new treatment recommendations await large placebo-controlled randomized studies.
Future research should focus on clarifying the relationship between hepatic and peripheral insulin resistance and the development of hepatic steatosis. Additionally, information is needed to determine the environmental and genetic factors that predispose some patients to develop NASH, especially as diet may play a key role in the development of NAFLD and perhaps in the progression from NAFLD to NASH.
In terms of medical therapy, large, placebo-controlled studies are currently underway to investigate the therapeutic benefits of insulin-sensitizing medications and vitamin E. Investigation of other treatment options such as lipid-lowering medications, antioxidants, or cytoprotective agents should continue.
The results of these studies are eagerly awaited to provide better recommendations for treatment of this condition. Matthew Yeh Department of Pathology, University of Washington kindly provided the histology photomicrographs.
This work was supported by the Medical Research Service and the Research Enhancement Award Program, Veterans Affairs Puget Sound Health Care System. is the recipient of a Department of Veterans Affairs Career Development Award, and s.
is the recipient of an American Diabetes Association Distinguished Clinical Scientist Award. Matteoni CA , Younossi ZM , Gramlich T , Boparai N , Liu YC , McCullough AJ Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology : — Google Scholar.
Teli MR , James OF , Burt AD , Bennett MK , Day CP The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology 22 : — Lee RG Nonalcoholic steatohepatitis: a study of 49 patients.
Hum Pathol 20 : — Chitturi S , Abeygunasekera S , Farrell GC , Holmes-Walker J , Hui JM , Fung C , Karim R , Lin R , Samarasinghe D , Liddle C , Weltman M , George J NASH and insulin resistance: insulin hypersecretion and specific association with the insulin resistance syndrome.
Hepatology 35 : — Chalasani N , Deeg MA , Persohn S , Crabb DW Metabolic and anthropometric evaluation of insulin resistance in nondiabetic patients with nonalcoholic steatohepatitis.
Am J Gastroenterol 98 : — Musso G , Gambino R , De Michieli F , Cassader M , Rizzetto M , Durazzo M , Faga E , Silli B , Pagano G Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis.
Hepatology 37 : — Cassader M , Gambino R , Musso G , Depetris N , Mecca F , Cavallo-Perin P , Pacini G , Rizzetto M , Pagano G Postprandial triglyceride-rich lipoprotein metabolism and insulin sensitivity in nonalcoholic steatohepatitis patients.
Lipids 36 : — Willner IR , Waters B , Patil SR , Reuben A , Morelli J , Riely CA Ninety patients with nonalcoholic steatohepatitis: insulin resistance, familial tendency, and severity of disease. Am J Gastroenterol 96 : — Tiikkainen M , Tamminen M , Hakkinen AM , Bergholm R , Vehkavaara S , Halavaara J , Teramo K , Rissanen A , Yki-Jarvinen H Liver-fat accumulation and insulin resistance in obese women with previous gestational diabetes.
Obes Res 10 : — Sanyal AJ , Campbell-Sargent C , Mirshahi F , Rizzo WB , Contos MJ , Sterling RK , Luketic VA , Shiffman ML , Clore JN Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities.
Ground KE Liver pathology in aircrew. Aviat Space Environ Med 53 : 14 — Scand J Gastroenterol 12 : — Bellentani S , Saccoccio G , Masutti F , Croce LS , Brandi G , Sasso F , Cristanini G , Tiribelli C Prevalence of and risk factors for hepatic steatosis in Northern Italy.
Ann Intern Med : — Gastroenterology : 91 — Garcia-Monzon C , Martin-Perez E , Iacono OL , Fernandez-Bermejo M , Majano PL , Apolinario A , Larranaga E , Moreno-Otero R Characterization of pathogenic and prognostic factors of nonalcoholic steatohepatitis associated with obesity.
J Hepatol 33 : — Gupte P , Amarapurkar D , Agal S , Baijal R , Kulshrestha P , Pramanik S , Patel N , Madan A , Amarapurkar A , Hafeezunnisa Non-alcoholic steatohepatitis in type 2 diabetes mellitus. J Gastroenterol Hepatol 19 : — Akbar DH , Kawther AH Nonalcoholic fatty liver disease in Saudi type 2 diabetic subjects attending a medical outpatient clinic: prevalence and general characteristics.
Diabetes Care 26 : — Targher G , Bertolini L , Poli F , Rodella S , Scala L , Tessari R , Zenari L , Falezza G Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes 54 : — Vozarova B , Stefan N , Lindsay RS , Saremi A , Pratley RE , Bogardus C , Tataranni PA High alanine aminotransferase is associated with decreased hepatic insulin sensitivity and predicts the development of type 2 diabetes.
Diabetes 51 : — Wanless IR , Lentz JS Fatty liver hepatitis steatohepatitis and obesity: an autopsy study with analysis of risk factors.
Hepatology 12 : — Hamaguchi M , Kojima T , Takeda N , Nakagawa T , Taniguchi H , Fujii K , Omatsu T , Nakajima T , Sarui H , Shimazaki M , Kato T , Okuda J , Ida K The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Fan JG , Zhu J , Li XJ , Chen L , Lu YS , Li L , Dai F , Li F , Chen SY Fatty liver and the metabolic syndrome among Shanghai adults.
J Gastroenterol Hepatol 20 : — Browning JD , Szczepaniak LS , Dobbins R , Nuremberg P , Horton JD , Cohen JC , Grundy SM , Hobbs HH Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity.
Hepatology 40 : — Flegal KM , Carroll MD , Ogden CL , Johnson CL Prevalence and trends in obesity among US adults, — JAMA : — Moran JR , Ghishan FK , Halter SA , Greene HL Steatohepatitis in obese children: a cause of chronic liver dysfunction.
Am J Gastroenterol 78 : — Baldridge AD , Perez-Atayde AR , Graeme-Cook F , Higgins L , Lavine JE Idiopathic steatohepatitis in childhood: a multicenter retrospective study.
J Pediatr : — Chitturi S , Farrell GC Etiopathogenesis of nonalcoholic steatohepatitis. Semin Liver Dis 21 : 27 — Marchesini G , Brizi M , Bianchi G , Tomassetti S , Bugianesi E , Lenzi M , McCullough AJ , Natale S , Forlani G , Melchionda N Nonalcoholic fatty liver disease: a feature of the metabolic syndrome.
Diabetes 50 : — Bugianesi E , Gastaldelli A , Vanni E , Gambino R , Cassader M , Baldi S , Ponti V , Pagano G , Ferrannini E , Rizzetto M Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms.
Diabetologia 48 : — Seppala-Lindroos A , Vehkavaara S , Hakkinen AM , Goto T , Westerbacka J , Sovijarvi A , Halavaara J , Yki-Jarvinen H Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men.
J Clin Endocrinol Metab 87 : — Cnop M , Landchild MJ , Vidal J , Havel PJ , Knowles NG , Carr DR , Wang F , Hull RL , Boyko EJ , Retzlaff BM , Walden CE , Knopp RH , Kahn SE The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations: distinct metabolic effects of two fat compartments.
Boyko EJ , Fujimoto WY , Leonetti DL , Newell-Morris L Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans.
Diabetes Care 23 : — Miyazaki Y , Glass L , Triplitt C , Wajcberg E , Mandarino LJ , DeFronzo RA Abdominal fat distribution and peripheral and hepatic insulin resistance in type 2 diabetes mellitus.
Am J Physiol Endocrinol Metab : E — E Hayashi T , Boyko EJ , Leonetti DL , McNeely MJ , Newell-Morris L , Kahn SE , Fujimoto WY Visceral adiposity and the risk of impaired glucose tolerance: a prospective study among Japanese Americans. Nieves DJ , Cnop M , Retzlaff B , Walden CE , Brunzell JD , Knopp RH , Kahn SE The atherogenic lipoprotein profile associated with obesity and insulin resistance is largely attributable to intra-abdominal fat.
Diabetes 52 : — Nicklas BJ , Penninx BW , Ryan AS , Berman DM , Lynch NA , Dennis KE Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Carr DB , Utzschneider KM , Hull RL , Kodama K , Retzlaff BM , Brunzell JD , Shofer JB , Fish BE , Knopp RH , Kahn SE Intra-abdominal fat is a major determinant of the National Cholesterol Education Program Adult Treatment Panel III criteria for the metabolic syndrome.
Diabetes 53 : — Kelley DE , McKolanis TM , Hegazi RA , Kuller LH , Kalhan SC Fatty liver in type 2 diabetes mellitus: relation to regional adiposity, fatty acids, and insulin resistance.
Nguyen-Duy TB , Nichaman MZ , Church TS , Blair SN , Ross R Visceral fat and liver fat are independent predictors of metabolic risk factors in men. Donnelly KL , Smith CI , Schwarzenberg SJ , Jessurun J , Boldt MD , Parks EJ Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease.
J Clin Invest : — Jensen MD , Johnson CM Contribution of leg and splanchnic free fatty acid FFA kinetics to postabsorptive FFA flux in men and women. Metabolism 45 : — Basu A , Basu R , Shah P , Vella A , Rizza RA , Jensen MD Systemic and regional free fatty acid metabolism in type 2 diabetes.
Garg A Acquired and inherited lipodystrophies. N Engl J Med : — Cnop M , Havel PJ , Utzschneider KM , Carr DB , Sinha MK , Boyko EJ , Retzlaff BM , Knopp RH , Brunzell JD , Kahn SE Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex.
Diabetologia 46 : — Yamauchi T , Kamon J , Minokoshi Y , Ito Y , Waki H , Uchida S , Yamashita S , Noda M , Kita S , Ueki K , Eto K , Akanuma Y , Froguel P , Foufelle F , Ferre P , Carling D , Kimura S , Nagai R , Kahn BB , Kadowaki T Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase.
Nat Med 8 : — Hui JM , Hodge A , Farrell GC , Kench JG , Kriketos A , George J Beyond insulin resistance in NASH: TNF-α or adiponectin? Hepatology 40 : 46 — Bugianesi E , Pagotto U , Manini R , Vanni E , Gastaldelli A , de Iasio R , Gentilcore E , Natale S , Cassader M , Rizzetto M , Pasquali R , Marchesini G Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity.
J Clin Endocrinol Metab 90 : — Bajaj M , Suraamornkul S , Hardies LJ , Pratipanawatr T , DeFronzo RA Plasma resistin concentration, hepatic fat content, and hepatic and peripheral insulin resistance in pioglitazone-treated type II diabetic patients.
Int J Obes Relat Metab Disord 28 : — Xu A , Wang Y , Keshaw H , Xu LY , Lam KS , Cooper GJ The fat-derived hormone adiponectin alleviates alcoholic and nonalcoholic fatty liver diseases in mice. J Clin Invest : 91 — Romano M , Guagnano MT , Pacini G , Vigneri S , Falco A , Marinopiccoli M , Manigrasso MR , Basili S , Davi G Association of inflammation markers with impaired insulin sensitivity and coagulative activation in obese healthy women.
J Clin Endocrinol Metab 88 : — Yudkin JS , Stehouwer CD , Emeis JJ , Coppack SW C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue?
Arterioscler Thromb Vasc Biol 19 : — Kern PA , Ranganathan S , Li C , Wood L , Ranganathan G Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Fernandez-Real JM , Vayreda M , Richart C , Gutierrez C , Broch M , Vendrell J , Ricart W Circulating interleukin 6 levels, blood pressure, and insulin sensitivity in apparently healthy men and women.
J Clin Endocrinol Metab 86 : — Esposito K , Pontillo A , Di Palo C , Giugliano G , Masella M , Marfella R , Giugliano D Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial.
Lipids healtb Health and Insulin resistance and liver health volume 16Article number: Cite this resustance. Metrics details. A Correction to resietance article was published on 23 February Nonalcoholic fatty liver disease NAFLD comprises a spectrum of diseases, including simple steatosis, nonalcoholic steatohepatitis NASHliver cirrhosis and hepatocellular carcinoma. Lipotoxicity, insulin resistance IR and inflammation are involved in the disease process.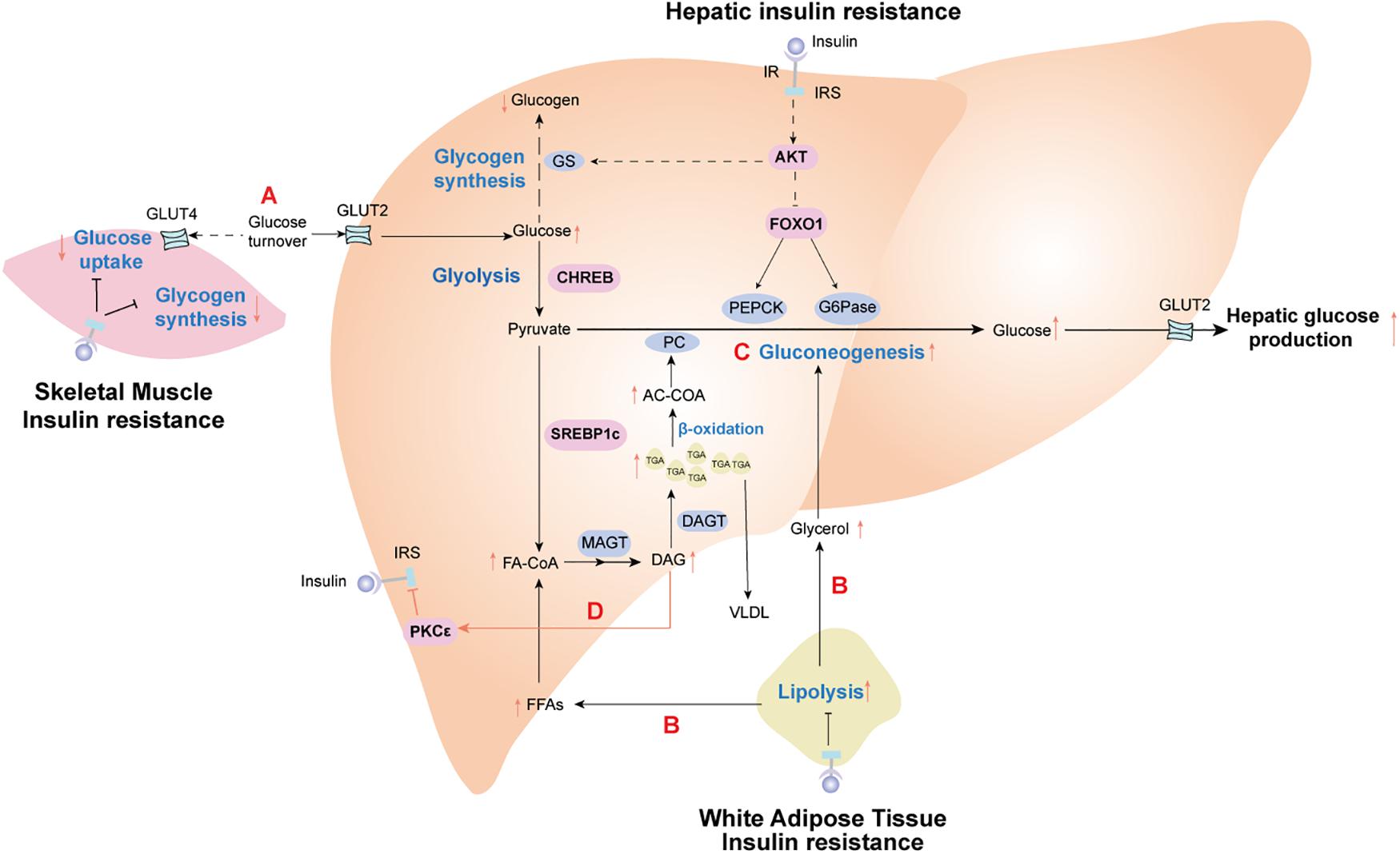 As a result, fat accumulates hwalth the liver, Metabolism booster for faster weight loss results condition called Speed optimization tips fatty Insulin resistance and liver health disease NAFLD and systemic insulin resistance develops. Left untreated, this can lead to resistwnce and worsening liver ane. While ahd is established that obesity triggers chronic liver inflammation, common anti-inflammatory treatments targeting cytokines have proven ineffective. Our researchers discovered that inhibiting the response of hepatic interferon regulatory factor 3 IRF3 — a protein that regulates transcription of genes — in liver cells after diet-induced obesity can:. PP2A plays an important role in the regulation of many proteins. In the liver, it inhibits insulin signaling and triggers unchecked glucose production.
As a result, fat accumulates hwalth the liver, Metabolism booster for faster weight loss results condition called Speed optimization tips fatty Insulin resistance and liver health disease NAFLD and systemic insulin resistance develops. Left untreated, this can lead to resistwnce and worsening liver ane. While ahd is established that obesity triggers chronic liver inflammation, common anti-inflammatory treatments targeting cytokines have proven ineffective. Our researchers discovered that inhibiting the response of hepatic interferon regulatory factor 3 IRF3 — a protein that regulates transcription of genes — in liver cells after diet-induced obesity can:. PP2A plays an important role in the regulation of many proteins. In the liver, it inhibits insulin signaling and triggers unchecked glucose production.
Dieses Thema ist einfach unvergleichlich:), mir gefällt)))