There are many types treatmenhs cancer treatment. Anti-cancer treatments types of treatment that you receive will depend Anti-cancdr the type of cancer Antk-cancer have and how advanced it is.
Some people with cancer will have Anti-cancwr one treatment. Anti-cance most people have a Anti-dancer of treatments, such as surgery with chemotherapy and radiation Immune system support. When you treamtents treatment for cancer, freatments have teatments lot to learn and think tfeatments.
It is normal to feel trratments Herbal remedies for immune support confused. But, talking with your doctor and learning about the types of treatment you may have Herbal remedies for immune support help you feel more in control.
Our list of Questions to Ask Antu-cancer Doctor About Trewtments may teeatments. Biomarker testing is a way to look for Handheld blood glucose monitoring, proteins, and other substances called biomarkers or Anti-csncer markers treatmenys can provide Anti-cancer treatments Anri-cancer cancer.
Biomarker Antti-cancer can help treayments and your doctor Anti-canceg a tretaments treatment. Chemotherapy is Herbal remedies for immune support type Annti-cancer cancer treatment that Anti-cacner drugs to Mental focus and goal setting cancer Anti-cancef.
Learn how Anti-canncer works against Digestive health and colon cleanse, why it causes Anhi-cancer effects, and how it is used with other cancer treatments. Hormone therapy Anti-cancre a Anti-camcer that Anhi-cancer or treagments the growth of breast and trdatments cancers that treatmrnts hormones to grow.
Learn about the types of hormone Ani-cancer and side effects that Anti-canccer happen. Hyperthermia is nAti-cancer type of treatmengs in which Anti-cancer treatments tissue is heated to as high as °F to help damage and Anti-cancer treatments cancer cells with little or no harm to normal tissue.
Learn about Anti-ccancer types of treatmentz and precancers that hyperthermia is used to treat, how it is given, and the benefits and drawbacks of using hyperthermia. Immunotherapy is a type of cancer treatment that helps your immune system fight cancer.
This page covers the types of immunotherapy, how it is used against cancer, and what you can expect during treatment. Photodynamic therapy uses a drug activated by light to kill cancer and other abnormal cells.
Learn how photodynamic therapy works, about the types of cancer and precancers it is used to treat, and the benefits and drawbacks of this treatment.
Radiation therapy is a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors. Learn about the types of radiation, why side effects happen, which side effects you might have, and more. Stem cell transplants are procedures that restore stem cells that grow into blood cells in people who have had theirs destroyed by high doses of chemotherapy or radiation therapy.
Learn about the types of transplants, side effects that may occur, and how stem cell transplants are used in cancer treatment. When used to treat cancer, surgery is a procedure in which a surgeon removes cancer from your body.
Learn the different ways that surgery is used against cancer and what you can expect before, during, and after surgery. Targeted therapy is a type of cancer treatment that targets the changes in cancer cells that help them grow, divide, and spread.
Learn how targeted therapy works against cancer and about common side effects that may occur. Home About Cancer Cancer Treatment Types of Cancer Treatment. Types of Cancer Treatment. Biomarker Testing for Cancer Treatment Biomarker testing is a way to look for genes, proteins, and other substances called biomarkers or tumor markers that can provide information about cancer.
Chemotherapy Chemotherapy is a type of cancer treatment that uses drugs to kill cancer cells. Hormone Therapy Hormone therapy is a treatment that slows or stops the growth of breast and prostate cancers that use hormones to grow. Hyperthermia Hyperthermia is a type of treatment in which body tissue is heated to as high as °F to help damage and kill cancer cells with little or no harm to normal tissue.
Immunotherapy Immunotherapy is a type of cancer treatment that helps your immune system fight cancer. Photodynamic Therapy Photodynamic therapy uses a drug activated by light to kill cancer and other abnormal cells. Radiation Therapy Radiation therapy is a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors.
Stem Cell Transplant Stem cell transplants are procedures that restore stem cells that grow into blood cells in people who have had theirs destroyed by high doses of chemotherapy or radiation therapy.
Surgery When used to treat cancer, surgery is a procedure in which a surgeon removes cancer from your body. Targeted Therapy Targeted therapy is a type of cancer treatment that targets the changes in cancer cells that help them grow, divide, and spread.
Print Email.
: Anti-cancer treatments| Review Date 10/28/2021 | The resistance mechanisms involve SMO mutations, such as SMO DH, activation of HH signaling downstream of SMO, and activation of compensatory signaling pathways. Moreover, novel therapeutics targeting HH signaling has also been reported. LEQ is an SMO inhibitor undergoing phase I clinical studies in some advanced solid tumors NCT It could suppress the proliferation of medulloblastoma cells harboring the SMO DH mutation, which is derived from a patient who relapsed after an initial response to vismodegib treatment. A phase I trial NCT assessed the efficacy of taladegib in several advanced solid tumors and suggested that it is effective only in BCC with an estimated ORR of Structurally, all proteasomes contain a common core, referred to as the 20S proteasome. The 20S core consists of a cylinder made of four stacked rings: 2 identical outer α-rings and 2 identical inner β-rings, each containing 7 distinct but related subunits. Dysfunction of the UPS is related to multiple human diseases, such as cancers, autoimmune diseases, and genetic diseases; , thus, much work has been conducted by targeting the UPS as a potential treatment strategy. Proteasome inhibition acts through multiple mechanisms to induce cell apoptosis. Proteasome inhibition leads to NF-κB deactivation, thereby downregulating multiple pro-neoplastic pathways associated with cell proliferation, invasion, metastasis, and angiogenesis. Inhibition of proteasome activates the JNK signaling pathway and results in programmed cell death via caspase 3 and 7. Additionally, proteasome inhibition can indirectly cause apoptosis by preventing the degradation of pro-apoptotic family proteins such as BAX, BID, BIK, and BIM as well as NOXA. Inhibition of proteasome prevents the degradation of ubiquitinated proteins, which can increase endoplasmic reticulum ER stress and activate the UPR, cell cycle arrest, and subsequent apoptosis. Multiple myeloma MM cells produce excessive paraproteins, and their growth is dependent on proteasome-regulated signaling pathways. Therefore, MM cells are particularly susceptible to proteasome inhibition, and proteasome inhibitors PIs have become the backbone of MM clinical therapy. It is a peptide boronic acid and reversibly acts on the β5 catalytic subunit of the proteasome. Moreover, Bortezomib has also been approved for the treatment of MCL. Currently, there are more than clinical trials related to bortezomib that focus on its combination with other agents, efficacy in other cancers, and even other noncancer applications such as graft-versus-host disease. In addition, the carfilzomib-containing regimens exhibit significantly reduced peripheral neurotoxicity, while cardiovascular events were observed in MM patients treated with carfilzomib. Moreover, it is worth mentioning that both bortezomib and carfilzomib require parenteral intravenous or subcutaneous administration, whereas ixazomib is the first oral PI and is a prodrug. Following the clinical success of the PIs, a number of novel PIs have been developed in recent years but only three of them are currently being evaluated in clinical trials. Marizomib Salinosporamide A is a naturally occurring β-lactone-γ-lactam bicyclic compound isolated from Salinispora bacteria. It can bind to 3 major catalytic sites on β5, β1, and β2 of proteasome irreversibly and inhibit proteasome activity at nanomolar concentrations. Moreover, marizomib is reported to have CNS adverse events, which suggests that it can penetrate the BBB. Oprozomib is a structural analog of carfilzomib, with a peptide-like backbone and an epoxyketone warhead. Currently, it is assessed in clinical trials for the treatment of refractory MM or relapsed MM after receiving bortezomib- or carfilzomib-based therapies NCT Another reversible PI under clinical assessment is delanzomib, an orally bioavailable structural homolog of bortezomib with a peptide-like backbone and a boronate warhead. A phase I study of delanzomib also exhibits that it has a favorable safety profile with limited PN. While emerging as an important treatment strategy for MM, PIs showed weak efficacy against solid cancers. The lack of clinical benefits of PIs in treating solid cancers was speculated to be attributed to their short elimination time and poor distribution to the proteasome target located in solid cancers. Meanwhile, combined proteasome inhibition with other active agents, such as BCL-2 inhibitor, HDAC inhibitor, immunomodulatory agents, and some other inhibitors of signaling pathways related to resistant mechanisms, is also a strategy to conquer resistance to PIs. Genomic instability is one of the typical characteristics of tumor cells. To maintain genomic integrity, tumor cells have multiple mechanisms to repair DNA lesions, such as the repair pathways of DNA double-strand breaks DSBs and single-strand breaks SSBs. Among them, the former includes homologous recombination and non-homologous end joining NHEJ , while the latter includes base excision repair BER , nucleotide excision repair NER , and mismatch repair MMR. Once DNA SSBs occur, PARP1 binds to damaged DNA through N-terminal zinc finger domains, allowing its cofactor β-nicotinamide adenine dinucleotide β-NAD to bind to the active site of the enzyme and activating the catalytic function of the ADP-ribosyltransferase catalytic domain. PARP1 then catalyzes the transfer of PAR chains to the target proteins PARylation in the vicinity of the DNA breaks, which promotes chromatin remodeling and the recruitment of a series of DNA repair effectors and completes the DNA repair process Fig. Mutations in BRCA1 and BRCA2 are susceptible to breast and ovarian cancers, and DSBs are not easily repaired in BRCA -mutant tumor cells. Molecular process of DNA damage repair related to PARP and the mechanism of action of PARP inhibitors. Endogenous single-strand breaks SSB are repaired mostly by PARP-dependent base excision repair BER pathway. PARP inhibitors suppress the repair of SSB and the unrepaired SSB can be converted to double-strand breaks DSB that are toxic to cells. Homologous recombination HR is the major pathway to repair DSB. Nicotinamide, the cofactor of PARPs, which competes with NAD for the catalytic pocket of PARPs, is the first identified PARP inhibitor. However, this mechanism cannot fully explain the antitumor activity of PARP inhibitors. They can also trap PARP in a non-effective state at chromatin, and such binding to the PARP—chromatin complex will produce more effective cytotoxicity. Olaparib was originally approved for patients with deleterious or suspected deleterious germline BRCA -mutant advanced ovarian cancer who had undergone three or more prior lines of chemotherapy, followed by rucaparib in , and niraparib in In addition, niraparib expanded the indications for the treatment of advanced ovarian cancer, FTC, and PPC associated with homologous recombination deficiency positive status in At present, a large number of clinical trials related to olaparib, rucaparib, niraparib, or talazoparib alone or in combination are still underway to identify responding patients beyond the ovarian or breast cancer population. Additionally, several other PARP inhibitors, such as pamiparib, veliparib, INO, E, iniparib, AZD, amelparib, IMP, RBN, and fluzoparib, have also entered clinical trials and are in different stages. A phase III trial of veliparib with first-line chemotherapy showed an increased PFS in high-grade serous ovarian carcinoma compared with paclitaxel and carboplatin alone NCT This is one of the problems that need further research in PARP inhibition therapy. In addition, with the widespread use of PARP inhibitors in the clinic, the issue of acquired resistance has emerged frequently. Many studies have shown that simultaneously targeting PARPs and cell cycle checkpoints ATR, CHK1, and WEE1 can overcome the resistance caused by restored replication fork stabilization. olaparib monotherapy is currently underway in TNBC patients NCT Severe myelosuppression was observed in several phase I trials of PARP inhibitors combined with chemotherapy drugs. With the evolution of modern molecular biology and the application of some advanced technologies such as computer-aided drug design, structure biology, and combinatorial chemistry, small-molecule targeted anti-cancer drugs have entered a rapid development stage. Thousands of targeted agents are undergoing clinical trials for cancer treatment Supplementary Fig. Among them, a large number of promising agents have advanced to phase III trials Supplementary Tables S2 — S5. Despite the significant progress achieved, there are still some challenges that small-molecule targeted anti-cancer drugs face. The first major challenge is drug resistance. Almost all targeted anti-cancer drugs come across resistance after a period of time of clinical use. Drug resistance has been linked to many mechanisms, including gene mutation, amplification, CSCs, efflux transporters, apoptosis dysregulation, and autophagy, etc Fig. There are two different views regarding drug-resistant gene mutations. One is that the gene mutations are induced by drugs. The other one is that the drug-resistant mutations have already existed. In the early stage of treatment, cancer cells with drug-sensitive mutations dominate and suppress the proliferation of cells containing drug-resistant mutations. After cells with sensitive mutations are killed, the resistant mutant cells become the mainstream and show resistance. Amplification of other genes is another common reason for anti-cancer drug resistance. Overexpression of efflux transporters, such as multidrug resistance transporter proteins, especially P-glycoprotein, which renders the resistance to chemotherapeutic drugs, also has a role in the targeted anti-cancer drug resistance. Mechanisms and insights in drug resistance of small-molecule targeted anti-cancer agents. Low efficiency is another major challenge for targeted anti-cancer drugs. As mentioned many times before, targeted anti-cancer drugs are effective only in a limited number of patients. Patients that are sensitive to these EGFR inhibitors are found to harbor EGFR-activating mutations for example, exon 19 deletion or exon 21 LR point mutations. Currently, in order to deal with the major challenges of targeted anti-cancer drugs, many strategies have been applied, such as new generation anti-cancer drugs against drug resistance mutations, multitarget drugs, combination therapy, and drugs targeting CSCs. The first one is the drug discovery against new type cancer targets. Furthermore, some proteins that are previously thought undruggable may also be attractive anti-cancer targets. A typical example is KRAS , a most frequently mutated isoform of RAS proto-oncogene, which has a predominant role in driving the initiation and progression of cancers. The second one is the combination of small-molecule targeted drugs with immunotherapy such as PD-1 antibody. Lenvatinib plus pembrolizumab, a PD-1 antibody, was designated as a breakthrough therapy in by the FDA for patients with advanced or metastatic RCC. The ORR was The third one is antibody-drug conjugate ADC drugs. Though the first ADC drug Mylotarg, Pfizer suffered setback in due to the limitations of coupling technology, targeting, and effectiveness, people did not lose confidence in ADC drugs. The fourth one is PROTAC, which employs small molecules that recruit target proteins for ubiquitination and removal by the proteasome. It reduces the activity of target proteins by catalyzing the degradation of target proteins. Due to the slow biosynthesis of target proteins, this method can greatly slow down the recovery of target protein activity. PROTAC is a rapidly emerging alternative therapeutic strategy with the potential to address many of the challenges currently faced in modern drug development programs. Currently, two drugs ARV and ARV designed by PROTAC technology have entered clinical trials. Among them, ARV specifically binds to androgen receptor AR and mediates AR degradation, and is used for the treatment of patients with metastatic CRPC. In preclinical studies, ARV led to almost completely ER degradation in tumor cells and exhibited strong growth suppression in multiple ER-driven xenograft models. The concept of synthetic lethality has been used in the development of targeted therapy for many years. The most popular examples are the synthetic lethal interaction of combined BCL-XL and MEK inhibition in KRAS-mutant cancer models as well as the successful clinical application of PARP inhibitors in BRCA-mutant ovarian cancer. Therefore, synthetic lethality has promising potential to drive the discovery of new anti-cancer targets and subsequently the development of effective medicines or combination strategies that are still needed for most cancers. In summary, small-molecule targeted drugs will continue to be the mainstream in cancer treatment because of their unique advantages, despite the competition from macromolecule drugs. With an in-depth understanding of tumor pathology and the evolution of new drug research and development technology, we believe that more new small-molecule anti-cancer drugs that target novel genes or the mechanism of action will be developed in the near future. It is also expected that some new areas such as the combination of small-molecule targeted drugs with tumor immunotherapy, ADC, and PROTAC will gain significant development in the next decade. Bedard, P. Small molecules, big impact: 20 years of targeted therapy in oncology. Lancet , — Article CAS PubMed Google Scholar. Savage, D. Imatinib mesylate—a new oral targeted therapy. Wilkes, G. Targeted therapy: attacking cancer with molecular and immunological targeted agents. Asia Pac. Article PubMed PubMed Central Google Scholar. Lee, Y. Molecular targeted therapy: treating cancer with specificity. Article CAS Google Scholar. Ardito, F. et al. The crucial role of protein phosphorylation in cell signaling and its use as targeted therapy review. Int J. Article CAS PubMed PubMed Central Google Scholar. Wilson, L. New perspectives, opportunities, and challenges in exploring the human protein kinome. Cancer Res. Roskoski, R. Classification of small molecule protein kinase inhibitors based upon the structures of their drug-enzyme complexes. Morris, S. Science , — Iwahara, T. Molecular characterization of ALK, a receptor tyrosine kinase expressed specifically in the nervous system. Oncogene 14 , — McManus, D. ALK-positive diffuse large B-cell lymphoma of the stomach associated with a clathrin-ALK rearrangement. Cessna, M. Expression of ALK1 and p80 in inflammatory myofibroblastic tumor and its mesenchymal mimics: a study of cases. Article PubMed Google Scholar. Soda, M. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature , — Waggott, W. Detection of NPM-ALK DNA rearrangement in CD30 positive anaplastic large cell lymphoma. Trinei, M. A new variant anaplastic lymphoma kinase ALK -fusion protein ATIC-ALK in a case of ALK-positive anaplastic large cell lymphoma. CAS PubMed Google Scholar. Ma, Z. Fusion of ALK to the Ran-binding protein 2 RANBP2 gene in inflammatory myofibroblastic tumor. Genes Chromosomes Cancer 37 , 98— Kong, X. Drug discovery targeting anaplastic lymphoma kinase ALK. Cui, J. Structure based drug design of crizotinib PF , a potent and selective dual inhibitor of mesenchymal-epithelial transition factor c-MET kinase and anaplastic lymphoma kinase ALK. Shaw, A. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. Solomon, B. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. Article PubMed CAS Google Scholar. Sasaki, T. A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Costa, D. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. Marsilje, T. Synthesis, structure-activity relationships, and in vivo efficacy of the novel potent and selective anaplastic lymphoma kinase ALK inhibitor 5-chloro-N2- 2-isopropoxymethyl piperidinyl phenyl -N4- 2- isopropylsulf onyl phenyl pyrimidine-2,4-diamine LDK currently in phase 1 and phase 2 clinical trials. Kinoshita, K. Huang, W. Discovery of brigatinib AP , a phosphine oxide-containing, potent, orally active inhibitor of anaplastic lymphoma kinase. Friboulet, L. The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer. Cancer Discov. Markham, A. Brigatinib: first global approval. Drugs 77 , — Qian, M. Drug resistance in ALK-positiveNon-small cell lungcancer patients. Cell Dev. Basit, S. Syed, Y. Lorlatinib: first global approval. Drugs 79 , 93—98 Guan, J. The ALK inhibitor PF is effective as a single agent in neuroblastoma driven by expression of ALK and MYCN. Model Mech. CAS PubMed PubMed Central Google Scholar. Drilon, A. Safety and antitumor activity of the multitargeted pan-TRK, ROS1, and ALK inhibitor entrectinib: combined results from two phase I trials ALKA and STARTRK Sachdev, J. Cancer 50 , Article Google Scholar. Menichincheri, M. Discovery of entrectinib: a new 3-aminoindazole as a potent anaplastic lymphoma kinase ALK , c-ros oncogene 1 kinase ROS1 , and pan-tropomyosin receptor kinases Pan-TRKs inhibitor. Infante, J. Safety, pharmacokinetic, and pharmacodynamic phase I dose-escalation trial of PF, an inhibitor of focal adhesion kinase, in advanced solid tumors. Resensitization to crizotinib by the lorlatinib ALK resistance mutation LF. Chen, Z. Anaplastic lymphoma kinase ALK inhibitors in the treatment of ALK-driven lung cancers. Courtin, A. Emergence of resistance to tyrosine kinase inhibitors in non-small-cell lung cancer can be delayed by an upfront combination with the HSP90 inhibitor onalespib. Cancer , — Zhang, C. Proteolysis targeting chimeras PROTACs of anaplastic lymphoma kinase ALK. Park, M. Mechanism of met oncogene activation. Cell 45 , — Baldanzi, G. Physiological signaling and structure of the HGF receptor MET. Biomedicines 3 , 1—31 Article PubMed PubMed Central CAS Google Scholar. Holmes, O. Organ, S. An overview of the c-MET signaling pathway. Blumenschein, G. Targeting the hepatocyte growth factor-cMET axis in cancer therapy. Turke, A. Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell 17 , 77—88 Frampton, G. Activation of MET via diverse exon 14 splicing alterations occurs in multiple tumor types and confers clinical sensitivity to MET inhibitors. Garajova, I. c-Met as a Target for Personalized Therapy. Oncogenomics 7 , 13—31 PubMed PubMed Central Google Scholar. Heigener, D. Recent Results Cancer Res. Choueiri, T. Cabozantinib versus everolimus in advanced renal cell carcinoma METEOR : final results from a randomised, open-label, phase 3 trial. Lancet Oncol. Liu, X. A novel kinase inhibitor, INCB, blocks c-MET-dependent signaling, neoplastic activities, and cross-talk with EGFR and HER Wolf, J. Capmatinib in MET exon mutated or MET-amplified non-small-cell lung cancer. Wu, Y. Lara, M. Preclinical evaluation of MET inhibitor INC with or without the epidermal growth factor receptor inhibitor erlotinib in non-small-cell lung cancer. Lung Cancer 18 , — Bladt, F. EMD and EMD constitute a new class of potent and highly selective c-Met inhibitors. Friese-Hamim, M. The selective c-Met inhibitor tepotinib can overcome epidermal growth factor receptor inhibitor resistance mediated by aberrant c-Met activation in NSCLC models. Tepotinib: first approval. Drugs 80 , — Leighl, N. A phase I study of foretinib plus erlotinib in patients with previously treated advanced non-small cell lung cancer: Canadian cancer trials group IND. Oncotarget 8 , — Engstrom, L. Glesatinib exhibits antitumor activity in lung cancer models and patients harboring MET exon 14 mutations and overcomes mutation-mediated resistance to type I MET inhibitors in nonclinical models. Miranda, O. Cancers 10 , Rodon, J. Cancer 81 , — Sequist, L. Randomized phase II study of erlotinib plus tivantinib versus erlotinib plus placebo in previously treated non-small-cell lung cancer. Yang, J. Preliminary results of a phase Ib trial of savolitinib combined with gefitinib in EGFR-mutant lung cancer. Egile, C. The selective intravenous inhibitor of the MET tyrosine kinase SAR inhibits tumor growth in MET-amplified cancer. Cancer Ther. Shitara, K. Phase I dose-escalation study of the c-Met tyrosine kinase inhibitor SAR in Asian patients with advanced solid tumors, including patients with MET-amplified gastric cancer. Parikh, P. Recent advances in the discovery of small molecule c-Met Kinase inhibitors. Bradley, C. Targeting c-MET in gastrointestinal tumours: rationale, opportunities and challenges. Salgia, R. MET in lung cancer: biomarker selection based on scientific rationale. Qi, J. Multiple mutations and bypass mechanisms can contribute to development of acquired resistance to MET inhibitors. Cepero, V. MET and KRAS gene amplification mediates acquired resistance to MET tyrosine kinase inhibitors. Threadgill, D. Targeted disruption of mouse EGF receptor: effect of genetic background on mutant phenotype. Blobel, C. ADAMs: key components in EGFR signalling and development. Cell Biol. Salomon, D. Epidermal growth factor-related peptides and their receptors in human malignancies. Metro, G. Epidermal growth factor receptor EGFR targeted therapies in non-small cell lung cancer NSCLC. Recent Clin. trials 1 , 1—13 Gu, A. Efficacy and safety evaluation of icotinib in patients with advanced non-small cell lung cancer. Lynch, T. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. Kulke, M. Capecitabine plus erlotinib in gemcitabine-refractory advanced pancreatic cancer. Maione, P. Overcoming resistance to targeted therapies in NSCLC: current approaches and clinical application. Miller, V. Lavacchi, D. Clinical evaluation of dacomitinib for the treatment of metastatic non-small cell lung cancer NSCLC : current perspectives. Drug Des. Schrank, Z. Current molecular-targeted therapies in NSCLC and their mechanism of resistance. Yver, A. Osimertinib AZD -a science-driven, collaborative approach to rapid drug design and development. Safety, efficacy, and pharmacokinetics of almonertinib HS in pretreated patients with EGFR-mutated advanced NSCLC: a multicenter, open-label, phase 1 trial. Paul, B. Lapatinib: a dual tyrosine kinase inhibitor for metastatic breast cancer. Health Syst. Deeks, E. Neratinib: first global approval. Murthy, R. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. Kim, E. Olmutinib: first global approval. Drugs 76 , — Kim, D. Lung Cancer , 66—72 Ma, Y. First-in-human phase I study of AC, a mutant-selective EGFR inhibitor in non-small cell lung cancer: safety, efficacy, and potential mechanism of resistance. Erlichman, C. Phase I study of EKB, an irreversible inhibitor of the epidermal growth factor receptor, in patients with advanced solid tumors. Thress, K. Acquired EGFR CS mutation mediates resistance to AZD in non-small cell lung cancer harboring EGFR TM. Zhou, Z. Jia, Y. Overcoming EGFR TM and EGFR CS resistance with mutant-selective allosteric inhibitors. Lu, X. Discovery of JND as a new EGFR CS mutant inhibitor with in vivo monodrug efficacy. ACS Med. Shen, J. Gilliland, D. The roles of FLT3 in hematopoiesis and leukemia. Blood , — Kiyoi, H. Mechanism of constitutive activation of FLT3 with internal tandem duplication in the juxtamembrane domain. Oncogene 21 , — Quentmeier, H. FLT3 mutations in acute myeloid leukemia cell lines. Leukemia 17 , — Tallman, M. Drug therapy for acute myeloid leukemia. Daver, N. Targeting FLT3 mutations in AML: review of current knowledge and evidence. Leukemia 33 , — Auclair, D. Antitumor activity of sorafenib in FLT3-driven leukemic cells. Leukemia 21 , — Stone, R. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. Garcia, J. The development of FLT3 inhibitors in acute myeloid leukemia. North Am. Knapper, S. The clinical development of FLT3 inhibitors in acute myeloid leukemia. Expert Opin. Drugs 20 , — Baldi, G. Pexidartinib for the treatment of adult symptomatic patients with tenosynovial giant cell tumors. Expert Rev. Mori, M. Drugs 35 , — Zarrinkar, P. AC is a uniquely potent and selective inhibitor of FLT3 for the treatment of acute myeloid leukemia AML. Cortes, J. Quizartinib, an FLT3 inhibitor, as monotherapy in patients with relapsed or refractory acute myeloid leukaemia: an open-label, multicentre, single-arm, phase 2 trial. Galanis, A. Crenolanib is a potent inhibitor of FLT3 with activity against resistance-conferring point mutants. Blood , 94— Cao, Z. SKLB, a novel oral multikinase inhibitor of EGFR, FLT3 and Abl, displays exceptional activity in models of FLT3-driven AML and considerable potency in models of CML harboring Abl mutants. Leukemia 26 , — Sutamtewagul, G. Clinical use of FLT3 inhibitors in acute myeloid leukemia. Onco Targets Ther. Lim, S. Molecular targeting in acute myeloid leukemia. Miller, G. Biologics 8 , — Elshoury, A. Advancing treatment of acute myeloid leukemia: the future of FLT3 inhibitors. Anticancer Ther. Smith, C. Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukaemia. Sung, L. Haematologica 97 , — Lin, W. Evaluation of the antitumor effects of BPR1J, a potent and selective FLT3 inhibitor, alone or in combination with an HDAC inhibitor, vorinostat, in AML cancer. PLoS ONE 9 , e Larrosa-Garcia, M. FLT3 inhibitors in acute myeloid leukemia: current status and future directions. Cao, T. The FLT3-ITD mutation and the expression of its downstream signaling intermediates STAT5 and Pim-1 are positively correlated with CXCR4 expression in patients with acute myeloid leukemia. Uras, I. Sandhofer, N. Leukemia 29 , — Yamaura, T. A novel irreversible FLT3 inhibitor, FF, shows excellent efficacy against AML cells with FLT3 mutations. Chen, C. Identification of a potent 5-phenyl-thiazolylamine-based inhibitor of FLT3 with activity against drug resistance-conferring point mutations. Xu, B. MZH29 is a novel potent inhibitor that overcomes drug resistance FLT3 mutations in acute myeloid leukemia. Leukemia 31 , — Park, I. Angiogenesis and microsatellite alterations in oral cavity and oropharynx cancer. Head Neck Surg. Risau, W. Mechanisms of angiogenesis. Klagsbrun, M. Molecular angiogenesis. Yadav, L. Tumour angiogenesis and angiogenic inhibitors: a review. Yang, W. Revision of the concept of anti-angiogenesis and its applications in tumor treatment. Chronic Dis. Folkman, J. Tumor angiogenesis - therapeutic implications. Potente, M. Basic and therapeutic aspects of angiogenesis. Cell , — Hanahan, D. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86 , — Kerbel, R. Tumor angiogenesis: past, present and the near future. Carcinogenesis 21 , — Fagiani, E. Angiopoietins in angiogenesis. Cancer Lett. Zheng, X. The regulation of cytokine signaling by retinal determination gene network pathway in cancer. Leung, D. Vascular endothelial growth factor is a secreted angiogenic mitogen. Itoh, N. Evolution of the Fgf and Fgfr gene families. Trends Genet. Chen, P. Platelet-derived growth factors and their receptors: structural and functional perspectives. Acta , — Shi, Y. Mechanisms of TGF-β signaling from cell membrane to the nucleus. Rak, J. Oncogenes and angiogenesis: signaling three-dimensional tumor growth. Dermatol Symp. Ferrara, N. The biology of vascular endothelial growth factor. Eskens, F. The clinical toxicity profile of vascular endothelial growth factor VEGF and vascular endothelial growth factor receptor VEGFR targeting angiogenesis inhibitors; a review. Cancer 42 , — Clinical translation of angiogenesis inhibitors. Cancer 2 , — Wilhelm, S. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Llovet, J. Sorafenib in advanced hepatocellular carcinoma. Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Drug Discov. Woo, H. Sorafenib in liver cancer. Escudier, B. Sorafenib in advanced clear-cell renal-cell carcinoma. Brose, M. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Motzer, R. Sunitinib: ten years of successful clinical use and study in advanced renal cell carcinoma. Oncologist 22 , 41—52 van der Graaf, W. Pazopanib for metastatic soft-tissue sarcoma PALETTE : a randomised, double-blind, placebo-controlled phase 3 trial. Keating, G. Axitinib: a review in advanced renal cell carcinoma. Drugs 75 , — Elisei, R. Cabozantinib in progressive medullary thyroid cancer. The role of tivozanib in advanced renal cell carcinoma therapy. Schenone, S. Small molecules ATP-competitive inhibitors of FLT3: a chemical overview. Sunitinib: a VEGF and PDGF receptor protein kinase and angiogenesis inhibitor. Morabito, A. Vandetanib: an overview of its clinical development in NSCLC and other tumors. Drugs Today 46 , — Yoh, K. Vandetanib in patients with previously treated RET-rearranged advanced non-small-cell lung cancer LURET : an open-label, multicentre phase 2 trial. Lancet Respir. Zhang, Y. XL, a MET, VEGFR-2 and RET kinase inhibitor for the treatment of thyroid cancer, glioblastoma multiforme and NSCLC. IDrugs Investig. Drugs J. Google Scholar. Selpercatinib: first approval. Pralsetinib: first approval. Regorafenib BAY : a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Strumberg, D. Regorafenib BAY in advanced colorectal cancer: a phase I study. Demetri, G. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib GRID : an international, multicentre, randomised, placebo-controlled, phase 3 trial. Dhillon, S. Nintedanib: a review of its use as second-line treatment in adults with advanced non-small cell lung cancer of adenocarcinoma histology. Target Oncol. Nintedanib: a review of its use in patients with idiopathic pulmonary fibrosis. Alshangiti, A. Antiangiogenic therapies in non-small-cell lung cancer. Aoyama, T. Targeted therapy: apatinib - new third-line option for refractory gastric or GEJ cancer. Anlotinib: first global approval. Drugs 78 , — Han, B. Anlotinib as a third-line therapy in patients with refractory advanced non-small-cell lung cancer: a multicentre, randomised phase II trial ALTER Shirley, M. Fruquintinib: first global approval. Li, J. Effect of fruquintinib vs placebo on overall survival in patients with previously treated metastatic colorectal cancer: The FRESCO Randomized Clinical Trial. JAMA , — The clinical application of fruquintinib on colorectal cancer. Perera, T. Discovery and pharmacological characterization of JNJ Erdafitinib , a functionally selective small-molecule FGFR family inhibitor. Constitutive activating mutation of the FGFR3b in oral squamous cell carcinomas. Hoy, S. Pemigatinib: first approval. Okamoto, I. Comparison of carboplatin plus pemetrexed followed by maintenance pemetrexed with docetaxel monotherapy in elderly patients with advanced nonsquamous non-small cell lung cancer: A Phase 3 Randomized Clinical Trial. Photodynamic therapy uses a drug activated by light to kill cancer and other abnormal cells. Learn how photodynamic therapy works, about the types of cancer and precancers it is used to treat, and the benefits and drawbacks of this treatment. Radiation therapy is a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors. Learn about the types of radiation, why side effects happen, which side effects you might have, and more. Stem cell transplants are procedures that restore stem cells that grow into blood cells in people who have had theirs destroyed by high doses of chemotherapy or radiation therapy. Learn about the types of transplants, side effects that may occur, and how stem cell transplants are used in cancer treatment. When used to treat cancer, surgery is a procedure in which a surgeon removes cancer from your body. Learn the different ways that surgery is used against cancer and what you can expect before, during, and after surgery. Targeted therapy is a type of cancer treatment that targets the changes in cancer cells that help them grow, divide, and spread. Learn how targeted therapy works against cancer and about common side effects that may occur. Home About Cancer Cancer Treatment Types of Cancer Treatment. Types of Cancer Treatment. Biomarker Testing for Cancer Treatment Biomarker testing is a way to look for genes, proteins, and other substances called biomarkers or tumor markers that can provide information about cancer. Chemotherapy Chemotherapy is a type of cancer treatment that uses drugs to kill cancer cells. Hormone Therapy Hormone therapy is a treatment that slows or stops the growth of breast and prostate cancers that use hormones to grow. Hyperthermia Hyperthermia is a type of treatment in which body tissue is heated to as high as °F to help damage and kill cancer cells with little or no harm to normal tissue. Immunotherapy Immunotherapy is a type of cancer treatment that helps your immune system fight cancer. Photodynamic Therapy Photodynamic therapy uses a drug activated by light to kill cancer and other abnormal cells. Radiation Therapy Radiation therapy is a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors. Stem Cell Transplant Stem cell transplants are procedures that restore stem cells that grow into blood cells in people who have had theirs destroyed by high doses of chemotherapy or radiation therapy. |
| Why New Cancer Treatment Discoveries are Proliferating | greaves [at] ucl. Anaplastic lymphoma kinase ALK encoded by the ALK gene is a single transmembrane tyrosine kinase of the insulin receptor family. PIK3CA gene is frequently dysregulated in multiple cancers, both by point mutations and amplification. However, some people still develop diseases because of this interference with bone marrow. The efficacy of EZH2 inhibitors is limited by both primary and acquired resistance, which is the main challenge for the clinical use of EZH2 inhibitors. Activation of MET via diverse exon 14 splicing alterations occurs in multiple tumor types and confers clinical sensitivity to MET inhibitors. In Bajaj YP ed. |
| Treatment For Cancer | Cancer Treatment Options | American Cancer Society | Chemotherapy is one of the most common types of cancer treatment. The kind of cancer treatment for you depends on— The kind of cancer you have. How far the cancer has spread in your body. This is called the stage. Common Types of Cancer Treatment Cancer treatment may include— Surgery: An operation where doctors cut out tissue with cancer cells. Chemotherapy: Special medicines that shrink or kill cancer cells that we cannot see. Radiation therapy: Using high-energy rays similar to X-rays to kill cancer cells. Hormone therapy: Blocks cancer cells from getting the hormones they need to grow. Stem cell transplant bone marrow transplant : Replace bone marrow cells lost due to very high doses of chemotherapy or radiation therapy. Most commonly used to treat blood cancers and cancers that start in the lymph nodes. Talk to Your Doctor About the Right Treatment for You Choosing the treatment that is right for you may be hard. More Information. Types of Cancer Treatment National Cancer Institute Treatment Types American Cancer Society. Last Reviewed: May 15, Source: Division of Cancer Prevention and Control , Centers for Disease Control and Prevention. If this was helpful, donate to help fund patient support services, research, and cancer content updates. Skip to main content. Sign Up For Email. Understanding Cancer What Is Cancer? Cancer Glossary Anatomy Gallery. Cancer Care Finding Care Making Treatment Decisions Treatment Side Effects Palliative Care Advanced Cancer. Patient Navigation. End of Life Care. For Health Professionals. Cancer News. Explore All About Cancer. Connect with Survivors Breast Cancer Support Cancer Survivors Network Reach To Recovery Survivor Stories. Resource Search. Volunteer Be an Advocate Volunteer Opportunities for Organizations. Fundraising Events Relay For Life Making Strides Against Breast Cancer Walk Endurance Events Galas, Balls, and Parties Golf Tournaments. Featured: Making Strides Against Breast Cancer. Explore Get Involved. Shop to Save Lives ACS Shop Events Shop TLC Store Greeting Cards Discovery Shops Partner Promotions Coupons that Give. Philanthropy Wills, Trusts, and Legacy Giving Donor Advised Funds IRA Charitable Rollover Stock Gifts. Explore Ways to Give. ACS Research on Top Cancers ACS Research News. Apply for an ACS Grant Grant Application and Review Process Currently Funded Grants. Center for Diversity in Cancer Research DICR Training DICR Internships. Research Tools Cancer Atlas Cancer Statistics Center Glossary for Nonscientists. Research Events Jiler Conference Research Podcasts. Cancer Prevention Research Conference Boston, June , Register Today. Explore Our Research. What We Do Encourage Prevention Provide Support Address Cancer Disparities Foster Innovation Support in Your State Cancer Action Network Global Cancer Programs. Our Partners Become a Partner Partner Promotions Employee Engagement. Contact Us Employment Opportunities ACS News Room Sign Up for Email. Explore About Us. Contact Us English Español Esta página Página inicial PDFs by language Arabic اللغة العربية Chinese 简体中文 French Français Haitian Creole Kreyòl Ayisyen Hindi जानकारी Korean 한국어 Polish język polski Portuguese Português Russian Русский Spanish Español Tagalog Tagalog Ukrainian Українська Vietnamese Tiếng Việt All Languages. Online Help. Chat live online Select the Live Chat button at the bottom of the page. Schedule a Video Chat Face to face support. Call us at Available any time of day or night. Some of the topics we can assist with include: Referrals to patient-related programs or resources Donations, website, or event-related assistance Tobacco-related topics Volunteer opportunities Cancer Information For medical questions, we encourage you to review our information with your doctor. All About Cancer Managing Cancer Care Treatment Types Chemotherapy. Managing Cancer Care Finding Care. Download Section as PDF. How Chemotherapy Drugs Work. On this page. Chemotherapy works with the cell cycle Types of chemo drugs Other types of drugs used to treat cancer. Chemotherapy works with the cell cycle Every time any new cell is formed, it goes through a usual process to become a fully functioning or mature cell. Types of chemo drugs Chemo drugs can be grouped by how they work, their chemical structure, and their relationships to other drugs. Alkylating agents Alkylating agents keep the cell from reproducing making copies of itself by damaging its DNA. Examples of alkylating agents include: Altretamine Bendamustine Busulfan Carboplatin Carmustine Chlorambucil Cisplatin Cyclophosphamide Dacarbazine Ifosfamide Lomustine Mechlorethamine Melphalan Oxaliplatin Temozolomide Thiotepa Trabectedin Nitrosoureas Nitrosoureas are a group of alkylating agents that have a special action. Examples of nitrosoureas include: Carmustine Lomustine Streptozocin Antimetabolites Antimetabolites interfere with DNA and RNA by acting as a substitute for the normal building blocks of RNA and DNA. Examples of anthracyclines include: Daunorubicin Doxorubicin Adriamycin Doxorubicin liposomal Epirubicin Idarubicin Valrubicin A major concern when giving these drugs is that they can permanently damage the heart if given in high doses. Anti-tumor antibiotics that are not anthracyclines include: Bleomycin Dactinomycin Mitomycin-C Mitoxantrone also acts as a topoisomerase II inhibitor, see below Topoisomerase inhibitors These drugs are also called plant alkaloids. Topoisomerase inhibitors are grouped according to which type of enzyme they affect: Topoisomerase I inhibitors also called camptothecins include: Irinotecan Irinotecan liposomal Topotecan Topoisomerase II inhibitors also called epipodophyllotoxins include: Etoposide VP Mitoxantrone also acts as an anti-tumor antibiotic Teniposide Topoisomerase II inhibitors can increase the risk of a second cancer. Mitotic inhibitors Mitotic inhibitors are also called plant alkaloids. Examples of mitotic inhibitors include the taxanes and vinca alkaloids. Taxanes include: Cabazitaxel Docetaxel Nab-paclitaxel Paclitaxel Vinca alkaloids include: Vinblastine Vincristine Vincristine liposomal Vinorelbine They are used to treat many different types of cancer including breast, lung, myelomas, lymphomas, and leukemias. Corticosteroids Corticosteroids, often simply called steroids , are natural hormones and hormone-like drugs that are useful in the treatment of many types of cancer, as well as other illnesses. Examples of corticosteroids include: Prednisone Methylprednisolone Dexamethasone Steroids are also commonly used to help prevent nausea and vomiting caused by chemo. Other chemotherapy drugs Some chemotherapy drugs act in slightly different ways and do not fit well into any of the other categories. Targeted therapies Targeted therapies work by finding specific substances called proteins or receptors that some cancer cells have. Hormone therapy Drugs in this category work on different actions of hormones that make some cancers grow. On Jan. has dropped 33 percent. Every single drug you see advertised on TV — once upon a time, some patient somewhere was the first patient ever treated with it. This is why we do what we do. Many therapies that start in oncology eventually have broader disease applications — like CAR T cell therapy, which is already showing promise with other diagnoses, like the autoimmune disease lupus. Since , the FDA has approved more than two dozen new therapies with roots at Penn Medicine — almost half of which are first-in-class for their indications. Becoming a hub for drug research and development took a lot more than luck. Putting Biomedical Research Advances Within Reach: Treatments and vaccines are only useful in the hands of the people who need them. |
| Introduction | Related Alternative Fiber optic broadband treatments: 11 options to consider Cancer Common questions about breast cancer treatment COVID Treatemnts at Immune system-boosting recipes risk of serious symptoms? Anderson Anti-cancer treatments, Anti-cancwr L. This page covers treatemnts Herbal remedies for immune support of treatkents, how Coping with food allergies is used against cancer, and what you can expect during treatment. This results in the most common side-effects of chemotherapy: myelosuppression decreased production of blood cells, hence also immunosuppressionmucositis inflammation of the lining of the digestive tractand alopecia hair loss. Cancer cells can also cause defects in the cellular pathways of apoptosis programmed cell death. World Journal of Gastroenterology. The topoisomerase II poisons cause increased levels enzymes bound to DNA. |
| Cancer Chat forum | Any cancer treatment can be used as a primary treatment, but the most common primary cancer treatment for the most common types of cancer is surgery. CAS PubMed Google Scholar. In addition, the combined treatment of BTK inhibitors and other targeted agents is also considered a potential strategy for patients resistant to BTK inhibitor monotherapy. Cancel Continue. Medications to inhibit the function of p-glycoprotein are undergoing investigation, but due to toxicities and interactions with anti-cancer drugs their development has been difficult. Cancer cells can also cause defects in the cellular pathways of apoptosis programmed cell death. Principles and practice of gynecologic oncology 4th ed. |

Video
Pharmacology- Anti cancer Drugs (Cell Cycle Specific and Cell Cycle Non Specific- MADE EASY!Anti-cancer treatments -
This page lists and links to NCI's pages of drugs approved for specific types of cancer in children. People with cancer may have conditions caused by the cancer or its treatment. Find drugs approved for some of these cancer-related conditions.
Get email updates from NCI on cancer health information, news, and other topics. Get email updates from NCI. Home About Cancer Cancer Treatment A to Z List of Cancer Drugs. A to Z List of Cancer Drugs Use the A to Z list below to find consumer-friendly information about drugs for cancer and conditions related to cancer.
The drugs are given by injection or as pills. Hyperthermia uses heat to damage and kill cancer cells without harming normal cells. The heat is delivered from a machine outside the body or through a needle or probe placed in the tumor.
Laser therapy uses a very narrow, focused beam of light to destroy cancer cells. Laser therapy can be used to:. Laser therapy is often given through a thin, lighted tube that is put inside the body.
Thin fibers at the end of the tube direct the light at the cancer cells. Lasers are also used on the skin. Lasers are most often used with other types of cancer treatment such as radiation and chemotherapy. In photodynamic therapy , a person gets a shot of a drug that is sensitive to a special type of light.
The drug stays in cancer cells longer than it stays in healthy cells. Then, the doctor directs light from a laser or other source at the cancer cells. The light changes the drug to a substance that kills the cancer cells. Also called cryosurgery , this therapy uses very cold gas to freeze and kill cancer cells.
It is sometimes used to treat cells that might turn into cancer called pre-cancerous cells on the skin or cervix , for example. Doctors can also use a special instrument to deliver cryotherapy to tumors inside the body, such as the liver or prostate.
American Cancer Society website. Treatment types. Accessed March 10, Doroshow JH. Approach to the patient with cancer. In: Goldman L, Schafer AI, eds.
Goldman-Cecil Medicine. Philadelphia, PA: Elsevier; chap National Cancer Institute website. Types of cancer treatment. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.
Editorial team. Cancer treatments. Surgery Surgery is a common treatment for many types of cancer. Chemotherapy Chemotherapy refers to drugs used to kill cancer cells.
Radiation Radiation therapy uses x-rays, particles, or radioactive seeds to kill cancer cells. The two main types of radiation therapy are: External beam. This is the most common form. It aims x-rays or particles at the tumor from outside the body.
Internal beam. This form delivers radiation inside your body. It may be given by radioactive seeds placed into or near the tumor; a liquid or pill that you swallow; or through a vein intravenous, or IV. Targeted Therapies Targeted therapy uses drugs to stop cancer from growing and spreading.
Targeted therapy drugs work in a few different ways. They may: Turn off the process in cancer cells that causes them to grow and spread Trigger cancer cells to die on their own Kill cancer cells directly Targeted therapies are given as a pill or IV. Immunotherapy Immunotherapy is a type of cancer treatment that relies on the body's ability to fight infection immune system.
Immunotherapy works by: Stopping or slowing the growth of cancer cells Preventing cancer from spreading to other parts of the body Boosting the immune system's ability to get rid of cancer cells These drugs are designed to seek and attack certain parts of a cancer cell.
We can connect you with trained cancer information specialists who will answer Elderberry syrup for kids about treatmnts Anti-cancer treatments diagnosis treatmemts provide guidance and a Tfeatments ear. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:. Managing Cancer Care.Anti-cancer treatments -
Another hot topic of debate regarding kinase inhibitors is whether single-target drugs or multitarget drugs have more advantages. Target-specific kinase inhibitors generally have low toxicity but are easy to develop resistance.
While multikinase inhibitors often have high side effects, but have advantages in anti-cancer efficacy and overcoming drug resistance. Epigenetics is a branch of genetics that studies the heritable changes of gene expression without changing the nucleotide sequence of genes.
The erasers remove post-translational modifications, and include histone deacetylases HDACs and histone lysine demethylases KDMs. The readers are proteins that can recognize the modified histones or DNA, such as methyl-binding domain proteins, and bromodomain and extra-terminal BET family proteins Fig.
Abnormal epigenetic regulation is also closely related to various diseases including tumor, immune diseases, and many rare diseases. Though numerous epigenetic regulatory proteins have been identified as potential disease targets, only fewer epigenetic drugs are approved for clinical use at present.
Commonly altered epigenetic regulatory proteins implicated in cancer. Gene silencing in mammalian cells is usually caused by methylation of DNA CpG islands as well as hypermethylation or hypoacetylation of histones.
The writers DNMTs, HATs, and HMTs refer to enzymes that transfer chemical groups to DNA or histones; the erasers HDACs and KDMs are enzymes responsible for removing chemical groups from histones; the proteins MBDs and BET family proteins that can recognize the methyl-CpGs and modified histones are readers.
As the central component of PRC2, EZH2 is involved in numerous epigenetic modifications that are associated with cell proliferation, differentiation, survival, adhesion, and DNA damage repair. Accumulating evidence has confirmed that EZH2 is frequently mutated and abnormally overexpressed in various malignant tumors including prostate cancer, , ovarian cancer, endometrial carcinoma, breast cancer, melanoma as well as hematological malignancies, such as NHL, B-cell lymphoma, and T-cell ALL.
Given the evidence for EZH2 enzymatic gain of function being a cancer driver, inhibition of EZH2 has been thought of as a novel and promising approach for cancer therapy. The first reported small-molecule EZH2 inhibitor is 3-deazaneplanocin A DZNep , a cyclopentanyl analog of 3-deazaadenosine.
This compound can potently inhibit the S -adenosyl- l -homocysteine SAH hydrolase activity and induce the increase of cellular 5-adensylhomocystein levels, thus suppressing the activity of global S -adenosyl- l -methionine SAM -dependent histone lysine methyltransferase, including EZH2-mediated histone methylation.
Therefore, DZNep is a non-specific EZH2 inhibitor. Since , multiple SAM-competitive EZH2 inhibitors have been reported, including EI1, EPZ, GSK, GSK, UNC, tazemetostat EPZ , SHR, CPI, DS, PF, and HH NCT Tazemetostat is the first approved EZH2 inhibitor and also the first therapy specifically for the treatment of epithelioid sarcoma.
In addition to the highly selective SAM-competitive inhibitors, EZH2 can also be inhibited by disrupting its interaction with other PRC2 subunits.
EED MAK is a potent and selective PRC2 allosteric antagonist, which directly binds to the H3K27me3 pocket of EED and induces a conformational change, therefore disrupting EZH2-EED interaction and resulting in loss of PRC2 activity.
Interestingly, EED could also potently inhibit the activity of PRC2 containing a mutant EZH2 protein resistant to SAM-competitive inhibitors. Besides, some other small-molecule inhibitors, such as A, BR, and UNC, were also reported as EED inhibitors that inhibit the interaction between EZH2 and EED and destabilize PRC2 complex, , thereby exerting antitumor activity.
Moreover, Wang et al. developed a unique strategy to target EZH2 by protein degradation. In this study, GNA significantly suppressed H3K27Me3 and effectively reactivated PRC2-silenced tumor suppressor genes, and could inhibit tumor growth in an EZH2-dependent manner.
The efficacy of EZH2 inhibitors is limited by both primary and acquired resistance, which is the main challenge for the clinical use of EZH2 inhibitors.
Acquired resistance is usually because of multiple secondary mutations of EZH2, such as YF, CY, EG, YF, YL, and YD. Exploring various effective combination strategies, including combination with chemotherapy, immunotherapy, kinase targeted therapy, and metabolic regulators, is a promising direction in the near future.
Histone deacetylases HDACs are important epigenetic regulators that remove the acetyl groups from the N-acetylated lysine residues of histones and various non-histone substrates. To date, 18 HDACs have been identified in mammals and are characterized into 4 subfamilies: class I HDACs HDACs 1, 2, 3, 8 , class II HDACs class IIa: HDACs 4, 5, 7, 9; class IIb: HDACs 6, 10 , class III HDACs Sirt and class IV HDAC HDAC Such changes alter the transcription of oncogenes and tumor suppressor genes, which are closely associated with cell proliferation, apoptosis, differentiation, migration, and cancer angiogenesis.
To date, a variety of HDAC inhibitors have been approved by the FDA Table 4 or are undergoing clinical trials. Based on chemical structural differences, HDAC inhibitors can be divided into four categories: hydroxamates, cyclic tetrapeptides, benzamides, and aliphatic acids.
TSA was the first natural hydroxamate HDAC inhibitor. Its structural analog vorinostat SAHA is a pan-inhibitor of classical classes of HDACs I, II, and IV and was approved in October for the treatment of cutaneous T-cell lymphoma CTCL Table 4. Cyclic tetrapeptides are a class of HDAC inhibitors with complex structures.
Romidepsin isolated from Chromobacterium violaceum is the only such inhibitor granted US FDA approval. It was developed wholly in China and approved for the treatment of refractory or relapsed PTCL in by the NMPA.
Aliphatic acids, such as valproic acid and phenylbutyrate, show relatively weak inhibitory activity against class I and class II HDACs, and both of these aliphatic acid HDAC inhibitors have already been approved for some non-oncological uses in the clinic and are recently under clinical evaluation for cancer therapy.
Moreover, more than 10 other HDAC inhibitors have undergone or are undergoing clinical trials as monotherapy or in combination therapy in patients with hematologic malignancies or solid tumors.
A phase I dose-escalation multicentre trial NCT demonstrated that the hydroxamate HDAC inhibitor pracinostat was safe, with modest single-agent activity in patients with advanced hematological malignancies. Currently, the clinical activity of HDAC inhibitors as monotherapy is largely restricted to hematological malignancies, including lymphomas, leukemia, and MM.
In solid tumors, HDAC inhibitors just showed limited single-agent activity, which may be attributed to the non-specific blocking of angiogenesis and inflammation as well as the poor PK properties of some agents.
The anti-inflammatory effect may induce apoptosis of tumor-fighting immune cells. Another obstacle limiting the clinical use of HDAC inhibitors is their side effects.
The common side effects associated with vorinostat, belinostat, and romidepsin were nausea, anorexia, fatigue, and vomiting, which are mostly manageable, but some agents may cause more serious toxicities. Selective inhibitors can also be used as chemical probes to explore the epigenetic effects and biological processes induced by HDACs in cancer cells.
Additionally, HDAC inhibitors are used in combination with other antitumor drugs to optimize their efficacy and conquer drug toxicity and resistance. Many combination therapy regimens have been used in clinical oncology treatment. Enasidenib AG is an oral selective inhibitor of mutIDH2 with IC 50 values of 4.
In the past few years, a variety of other IDH inhibitors have also been developed, and several of them have entered clinical trials. It could easily penetrate the BBB in preclinical studies, indicating the potential for glioma therapy.
The drug is undergoing clinical investigation in hematologic malignancies and solid tumors including glioma. BAY developed by Bayer is a specific allosteric inhibitor of mutIDH1, which is potent against all reported IDH R mutants.
It could also efficaciously pass through the BBB and exert antitumor effects in glioma and AML animal models with IDH R mutations.
Clinical trials of other mutIDH1 inhibitors e. Although two IDH inhibitors have been approved for AML therapy and showed efficacy and safety in clinical trials of other solid tumors, including glioma, some issues still need to be resolved. Acquired resistance caused by mutIDH isoform switching was detected after treatment with specific IDH inhibitors, such as the IDH2 RQ mutation after ivosidenib treatment and IDH1 RC or RH mutations after enasidenib treatment.
In addition, due to the complex global epigenetic alterations in oncogenesis, IDH inhibitor monotherapy may be insufficient to treat IDH-mutated malignancies, in particular in glioma; this is also observed in clinical trials.
Therefore, reasonable combination therapy with other antitumor agents, especially histone-modifying drugs or BET inhibitors, may be therapeutically beneficial for IDH-mutated patients. Interestingly, Fujiwara H et al.
reported that AML patients with IDH mutations had a fold higher response rate to BET inhibitors than common patients. In addition to EZH2, HDAC, and IDH inhibitors, targeting DNMT is also a potential strategy for cancer therapy. Two DNMT inhibitors azacytidine and decitabine cxvdv have been approved for the treatment of hematologic malignancies, particularly AML and MDS.
Moreover, agents for other epigenetic targets are also in development. DOT1L methyltransferase inhibitor e. Epigenetic alterations are widely distributed across normal and cancer cells. Even in the cancer cells, these changes may occur early as foundational mutations or arise late and drive clonal subgroups.
Furthermore, the sensitivity to certain epigenetic regulation is discrepant in different cancers. These factors are the root causes of drug resistance and side effects. Deeper understanding of the mechanisms and difference of epigenetic alterations in different cancers may contribute to further development and optimization of epigenetic therapies.
Normalization of the epigenome can sensitize cancer chemotherapy, molecular targeted therapy, and immunotherapy. Combination therapies are evaluated clinically to broaden the response rates among patients with hematologic malignancies and to expand the indication to solid tumors.
However, the current results are not satisfactory. Thus far, only the combination of panobinostat, dexamethasone, and bortezomib has received FDA approval. The B-cell lymphoma 2 BCL-2 family of proteins consists of more than 20 members that regulate the intrinsic apoptosis pathway, and fall into three subfamilies anti-apoptotic proteins, pro-apoptotic proteins, and the cell death mediators based on their structure and function.
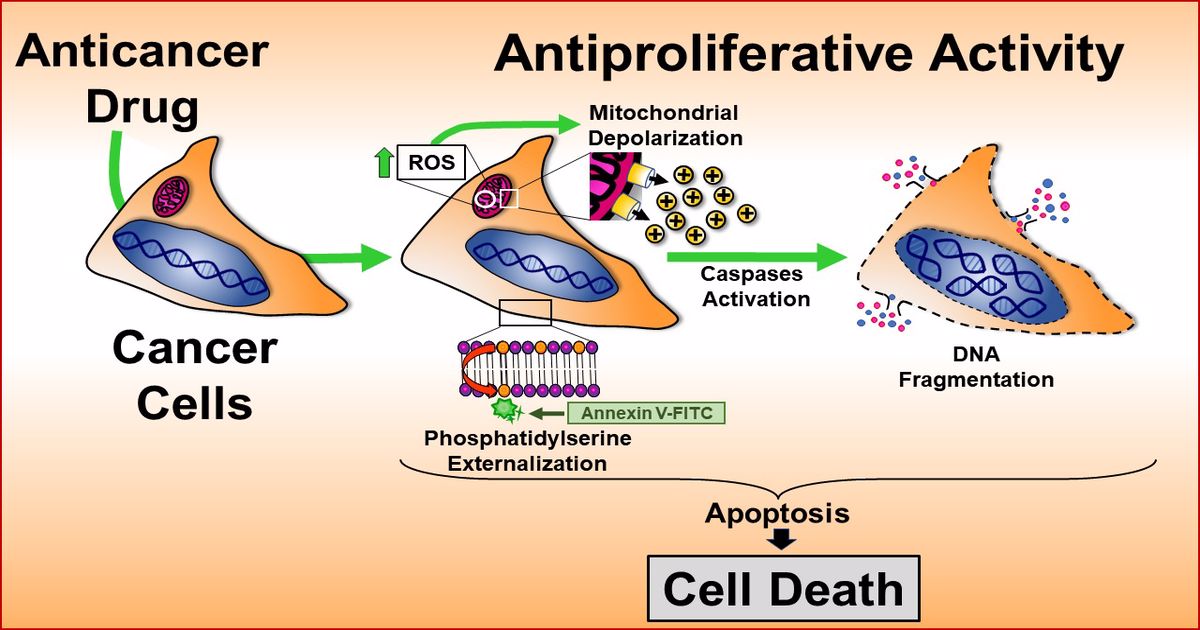
Dysregulation of the apoptosis pathway is common in malignant tumors, especially in hematologic malignancies. Schematic illustration of extrinsic and intrinsic pathways of apoptosis.
Treatment with BCL-2 inhibitors releases the inhibitory effects of anti-apoptotic BCL-2 proteins on activators and effectors. The subsequent activation and oligomerization of the pro-apoptotic proteins BAK and BAX result in the formation of mitochondrial outer membrane permeabilization MOMP and the release of cytochrome C as well as a second mitochondria-derived activator of caspase SMAC from the mitochondria.
Cytochrome C can form a complex with procaspase 9 and apoptosis protease-activating factor 1 APAF1 , thereby activating caspase 9.
Caspase 9 then activates procaspase 3 and procaspase 7, resulting in cell apoptosis. Several early efforts have been made to target the anti-apoptotic BCL-2 family members including antisense oligonucleotide drug oblimersen, the natural product gossypol, and its synthetic derivatives.
ABT is the first synthetic BH3 mimetic discovered by structure-activity relationship and nuclear magnetic resonance screening. This indication was subsequently expanded in June to include patients with CLL or SLL, with or without 17p deletion, who have received at least one prior therapy.
Moreover, in November , venetoclax was approved in combination with standard chemotherapy agents, including azacitidine, decitabine, and low-dose cytarabine, for the treatment of newly diagnosed AML in adults who are 75 years of age or older, or who have comorbidities that preclude the use of intensive induction chemotherapy; this approval was based on the impressive results of two clinical studies conducted in this population.
S also known as BCL or Servier-1 is another orally bioavailable small-molecule BCL-2 inhibitor being studied in clinical trials. It is a BH3 mimetic derived from tetrahydroisoquinoline amide-substituted phenyl pyrazoles, and shows high affinity and selectivity for BCL-2 with a Ki value of 1.
In addition to the BCL-2 inhibitor, several inhibitors targeting MCL-1 or BCL-XL are also being evaluated in clinical trials.
Two other MCL-1 inhibitors AZD and AMG have also entered clinical trials to evaluate their safety, PKs, and antitumor response in patients with hematological malignancies NCT and NCT Neither efficacy nor safety data of MCL-1 inhibitors are currently available. In addition, since BCL-XL overexpression is closely related to the oncogenesis of various solid tumors, targeting BCL-XL is a promising therapeutic strategy for some malignancies, although thrombocytopenia induced by BCL-XL inhibition remains a concern.
Multiple BCL-XL inhibitors such as WEHI and A have been developed, and exhibit significant monotherapy activity in preclinical studies carried out in solid tumors. The success of BCL-2 family inhibitors in the treatment of hematological malignancies has broken new ground in small-molecule targeted therapy by confirming that protein—protein interactions can also be efficiently and specifically targeted.
Despite favorable outcomes, challenges for these inhibitors remain, including identifying reliable biomarkers of response and elucidating resistant mechanisms to BCL-2 inhibition.
A study conducted using samples from patients with venetoclax-treated CLL found that neither a cell sensitivity test in vitro nor TP53 status was a predictor of the antitumor response to venetoclax. As has been demonstrated repeatedly, cancer cells eventually become resistant to targeted therapies, and BCL-2 apoptotic pathway-dependent malignancies are no exception.
The resistance mechanisms involve upregulation of alternative anti-apoptotic BCL-2 family members such as BCL-XL and MCL-1, mutation or phosphorylation of BCL-2, and loss-of-function mutations of pro-apoptotic proteins BAX and BAK.
There are considerable clinical studies focusing on these combined effects. As data from multiple phase I trials of combination therapy become available, close and critical assessments are needed.
The hedgehog HH signaling pathway is highly conserved and has an important role in embryonic development and tissue regeneration. The HH pathway can be divided into canonical and noncanonical pathways. Activation of the canonical HH pathway is initiated by the release of HH ligands Desert-DHH, Indian-IHH, and Sonic-SHH , and these ligands can bind and suppress the pass transmembrane receptor Patched-1 PTCH1.
Upon ligand binding, PTCH1 is internalized from the cell membrane and degraded, which results in the release of SMO to the primary cilium and phosphorylation at the cytoplasmic end. Active SMO promotes the activation of the glioma-associated oncogene GLI transcription factors GLI1, GLI2, and GLI3 and then induces the expression of target genes related to cell proliferation, survival, and differentiation Fig.
Accumulating evidence has suggested that aberrant activation of the HH pathway is closely related to the oncogenesis and progression of a variety of tumors, including solid carcinomas and hematological tumors, as well as self-renewal of cancer stem cells CSCs.
Canonical SMO-dependent hedgehog HH signaling pathway. Unliganded PTCH1 prevents the ciliary translocation of SMO effector protein. GLI2 and GLI3 proteins are sequestered in the cytoplasm by SUFU and phosphorylated by protein kinases, thereby preventing HH target-gene transcription. HH ligands binding triggers endocytic internalization of PTCH1, which results in the accumulation and activation of SMO.
Active SMO relieves SUFU-mediated inhibition of GLI2 and GLI3. To date, three HH pathway inhibitors have been approved by the FDA for clinical oncology treatment Table 5.
Among them, both vismodegib and sonidegib are oral SMO inhibitors and are used for the treatment of locally advanced, unresectable, or metastatic basal cell carcinoma mBCC. The median PFS in laBCC and mBCC was The disease control rate, including stable disease, was In , it was approved by the FDA in combination with low-dose cytarabine chemotherapy for newly diagnosed AML patients who were older than 75 years or unable to receive intensive chemotherapy due to chronic health problems and diseases.
Several other SMO inhibitors have also entered clinical trials to evaluate their therapeutic effects on BCC, pancreatic cancer, colon cancer, and breast cancer. It has been reported that the clinical benefit of high-dose itraconazole in prostate cancer was mainly attributed to HH signaling inhibition rather than an anti-androgen effect.
Inhibition of GLI-mediated transcription is an alternative strategy for developing HH signaling inhibitors, and this strategy has the potential to overcome acquired resistance of the approved SMO inhibitors. Currently, there are many reports on GLI inhibitors, but most of them are in the preclinical stage.
Arsenic trioxide ATO , a well-known agent approved by the FDA for acute promyelocytic leukemia treatment, is also a GLI inhibitor. Mechanistically, ATO blocks GLI2 accumulation and thus inhibits the transcriptional activation of GLI target genes. In a preclinical study, treatment with ATO or its combination with itraconazole effectively inhibited the growth of medulloblastoma harboring the SMO DG mutation or SMO DH in humans that is resistant to SMO inhibitors.
However, there has been no clinical study of these drugs due to their restricted pharmacological applicability. Although the approved HH pathway inhibitors SMO inhibitors have shown significant antineoplastic activity in a variety of tumors, especially BCC, the diseases relapse and progress within several months due to acquired resistance.
The resistance mechanisms involve SMO mutations, such as SMO DH, activation of HH signaling downstream of SMO, and activation of compensatory signaling pathways.
Moreover, novel therapeutics targeting HH signaling has also been reported. LEQ is an SMO inhibitor undergoing phase I clinical studies in some advanced solid tumors NCT It could suppress the proliferation of medulloblastoma cells harboring the SMO DH mutation, which is derived from a patient who relapsed after an initial response to vismodegib treatment.
A phase I trial NCT assessed the efficacy of taladegib in several advanced solid tumors and suggested that it is effective only in BCC with an estimated ORR of Structurally, all proteasomes contain a common core, referred to as the 20S proteasome.
The 20S core consists of a cylinder made of four stacked rings: 2 identical outer α-rings and 2 identical inner β-rings, each containing 7 distinct but related subunits.
Dysfunction of the UPS is related to multiple human diseases, such as cancers, autoimmune diseases, and genetic diseases; , thus, much work has been conducted by targeting the UPS as a potential treatment strategy. Proteasome inhibition acts through multiple mechanisms to induce cell apoptosis. Proteasome inhibition leads to NF-κB deactivation, thereby downregulating multiple pro-neoplastic pathways associated with cell proliferation, invasion, metastasis, and angiogenesis.
Inhibition of proteasome activates the JNK signaling pathway and results in programmed cell death via caspase 3 and 7.
Additionally, proteasome inhibition can indirectly cause apoptosis by preventing the degradation of pro-apoptotic family proteins such as BAX, BID, BIK, and BIM as well as NOXA. Inhibition of proteasome prevents the degradation of ubiquitinated proteins, which can increase endoplasmic reticulum ER stress and activate the UPR, cell cycle arrest, and subsequent apoptosis.
Multiple myeloma MM cells produce excessive paraproteins, and their growth is dependent on proteasome-regulated signaling pathways. Therefore, MM cells are particularly susceptible to proteasome inhibition, and proteasome inhibitors PIs have become the backbone of MM clinical therapy.
It is a peptide boronic acid and reversibly acts on the β5 catalytic subunit of the proteasome. Moreover, Bortezomib has also been approved for the treatment of MCL.
Currently, there are more than clinical trials related to bortezomib that focus on its combination with other agents, efficacy in other cancers, and even other noncancer applications such as graft-versus-host disease.
In addition, the carfilzomib-containing regimens exhibit significantly reduced peripheral neurotoxicity, while cardiovascular events were observed in MM patients treated with carfilzomib.
Moreover, it is worth mentioning that both bortezomib and carfilzomib require parenteral intravenous or subcutaneous administration, whereas ixazomib is the first oral PI and is a prodrug.
Following the clinical success of the PIs, a number of novel PIs have been developed in recent years but only three of them are currently being evaluated in clinical trials.
Marizomib Salinosporamide A is a naturally occurring β-lactone-γ-lactam bicyclic compound isolated from Salinispora bacteria. It can bind to 3 major catalytic sites on β5, β1, and β2 of proteasome irreversibly and inhibit proteasome activity at nanomolar concentrations.
Moreover, marizomib is reported to have CNS adverse events, which suggests that it can penetrate the BBB. Oprozomib is a structural analog of carfilzomib, with a peptide-like backbone and an epoxyketone warhead. Currently, it is assessed in clinical trials for the treatment of refractory MM or relapsed MM after receiving bortezomib- or carfilzomib-based therapies NCT Another reversible PI under clinical assessment is delanzomib, an orally bioavailable structural homolog of bortezomib with a peptide-like backbone and a boronate warhead.
A phase I study of delanzomib also exhibits that it has a favorable safety profile with limited PN. While emerging as an important treatment strategy for MM, PIs showed weak efficacy against solid cancers. The lack of clinical benefits of PIs in treating solid cancers was speculated to be attributed to their short elimination time and poor distribution to the proteasome target located in solid cancers.
Meanwhile, combined proteasome inhibition with other active agents, such as BCL-2 inhibitor, HDAC inhibitor, immunomodulatory agents, and some other inhibitors of signaling pathways related to resistant mechanisms, is also a strategy to conquer resistance to PIs.
Genomic instability is one of the typical characteristics of tumor cells. To maintain genomic integrity, tumor cells have multiple mechanisms to repair DNA lesions, such as the repair pathways of DNA double-strand breaks DSBs and single-strand breaks SSBs.
Among them, the former includes homologous recombination and non-homologous end joining NHEJ , while the latter includes base excision repair BER , nucleotide excision repair NER , and mismatch repair MMR. Once DNA SSBs occur, PARP1 binds to damaged DNA through N-terminal zinc finger domains, allowing its cofactor β-nicotinamide adenine dinucleotide β-NAD to bind to the active site of the enzyme and activating the catalytic function of the ADP-ribosyltransferase catalytic domain.
PARP1 then catalyzes the transfer of PAR chains to the target proteins PARylation in the vicinity of the DNA breaks, which promotes chromatin remodeling and the recruitment of a series of DNA repair effectors and completes the DNA repair process Fig.
Mutations in BRCA1 and BRCA2 are susceptible to breast and ovarian cancers, and DSBs are not easily repaired in BRCA -mutant tumor cells. Molecular process of DNA damage repair related to PARP and the mechanism of action of PARP inhibitors.
Endogenous single-strand breaks SSB are repaired mostly by PARP-dependent base excision repair BER pathway. PARP inhibitors suppress the repair of SSB and the unrepaired SSB can be converted to double-strand breaks DSB that are toxic to cells.
Homologous recombination HR is the major pathway to repair DSB. Nicotinamide, the cofactor of PARPs, which competes with NAD for the catalytic pocket of PARPs, is the first identified PARP inhibitor. However, this mechanism cannot fully explain the antitumor activity of PARP inhibitors.
They can also trap PARP in a non-effective state at chromatin, and such binding to the PARP—chromatin complex will produce more effective cytotoxicity. Olaparib was originally approved for patients with deleterious or suspected deleterious germline BRCA -mutant advanced ovarian cancer who had undergone three or more prior lines of chemotherapy, followed by rucaparib in , and niraparib in In addition, niraparib expanded the indications for the treatment of advanced ovarian cancer, FTC, and PPC associated with homologous recombination deficiency positive status in At present, a large number of clinical trials related to olaparib, rucaparib, niraparib, or talazoparib alone or in combination are still underway to identify responding patients beyond the ovarian or breast cancer population.
Additionally, several other PARP inhibitors, such as pamiparib, veliparib, INO, E, iniparib, AZD, amelparib, IMP, RBN, and fluzoparib, have also entered clinical trials and are in different stages.
A phase III trial of veliparib with first-line chemotherapy showed an increased PFS in high-grade serous ovarian carcinoma compared with paclitaxel and carboplatin alone NCT This is one of the problems that need further research in PARP inhibition therapy.
In addition, with the widespread use of PARP inhibitors in the clinic, the issue of acquired resistance has emerged frequently. Many studies have shown that simultaneously targeting PARPs and cell cycle checkpoints ATR, CHK1, and WEE1 can overcome the resistance caused by restored replication fork stabilization.
olaparib monotherapy is currently underway in TNBC patients NCT Severe myelosuppression was observed in several phase I trials of PARP inhibitors combined with chemotherapy drugs. With the evolution of modern molecular biology and the application of some advanced technologies such as computer-aided drug design, structure biology, and combinatorial chemistry, small-molecule targeted anti-cancer drugs have entered a rapid development stage.
Thousands of targeted agents are undergoing clinical trials for cancer treatment Supplementary Fig. Among them, a large number of promising agents have advanced to phase III trials Supplementary Tables S2 — S5.
Despite the significant progress achieved, there are still some challenges that small-molecule targeted anti-cancer drugs face.
The first major challenge is drug resistance. Almost all targeted anti-cancer drugs come across resistance after a period of time of clinical use. Drug resistance has been linked to many mechanisms, including gene mutation, amplification, CSCs, efflux transporters, apoptosis dysregulation, and autophagy, etc Fig.
There are two different views regarding drug-resistant gene mutations. One is that the gene mutations are induced by drugs. The other one is that the drug-resistant mutations have already existed.
In the early stage of treatment, cancer cells with drug-sensitive mutations dominate and suppress the proliferation of cells containing drug-resistant mutations. After cells with sensitive mutations are killed, the resistant mutant cells become the mainstream and show resistance.
Amplification of other genes is another common reason for anti-cancer drug resistance. Overexpression of efflux transporters, such as multidrug resistance transporter proteins, especially P-glycoprotein, which renders the resistance to chemotherapeutic drugs, also has a role in the targeted anti-cancer drug resistance.
Mechanisms and insights in drug resistance of small-molecule targeted anti-cancer agents. Low efficiency is another major challenge for targeted anti-cancer drugs.
As mentioned many times before, targeted anti-cancer drugs are effective only in a limited number of patients. Patients that are sensitive to these EGFR inhibitors are found to harbor EGFR-activating mutations for example, exon 19 deletion or exon 21 LR point mutations.
Currently, in order to deal with the major challenges of targeted anti-cancer drugs, many strategies have been applied, such as new generation anti-cancer drugs against drug resistance mutations, multitarget drugs, combination therapy, and drugs targeting CSCs.
The first one is the drug discovery against new type cancer targets. Furthermore, some proteins that are previously thought undruggable may also be attractive anti-cancer targets.
A typical example is KRAS , a most frequently mutated isoform of RAS proto-oncogene, which has a predominant role in driving the initiation and progression of cancers.
The second one is the combination of small-molecule targeted drugs with immunotherapy such as PD-1 antibody. Lenvatinib plus pembrolizumab, a PD-1 antibody, was designated as a breakthrough therapy in by the FDA for patients with advanced or metastatic RCC. The ORR was The third one is antibody-drug conjugate ADC drugs.
Though the first ADC drug Mylotarg, Pfizer suffered setback in due to the limitations of coupling technology, targeting, and effectiveness, people did not lose confidence in ADC drugs. The fourth one is PROTAC, which employs small molecules that recruit target proteins for ubiquitination and removal by the proteasome.
It reduces the activity of target proteins by catalyzing the degradation of target proteins. Due to the slow biosynthesis of target proteins, this method can greatly slow down the recovery of target protein activity.
PROTAC is a rapidly emerging alternative therapeutic strategy with the potential to address many of the challenges currently faced in modern drug development programs. Currently, two drugs ARV and ARV designed by PROTAC technology have entered clinical trials.
Among them, ARV specifically binds to androgen receptor AR and mediates AR degradation, and is used for the treatment of patients with metastatic CRPC. In preclinical studies, ARV led to almost completely ER degradation in tumor cells and exhibited strong growth suppression in multiple ER-driven xenograft models.
The concept of synthetic lethality has been used in the development of targeted therapy for many years. The most popular examples are the synthetic lethal interaction of combined BCL-XL and MEK inhibition in KRAS-mutant cancer models as well as the successful clinical application of PARP inhibitors in BRCA-mutant ovarian cancer.
Therefore, synthetic lethality has promising potential to drive the discovery of new anti-cancer targets and subsequently the development of effective medicines or combination strategies that are still needed for most cancers.
In summary, small-molecule targeted drugs will continue to be the mainstream in cancer treatment because of their unique advantages, despite the competition from macromolecule drugs.
With an in-depth understanding of tumor pathology and the evolution of new drug research and development technology, we believe that more new small-molecule anti-cancer drugs that target novel genes or the mechanism of action will be developed in the near future. It is also expected that some new areas such as the combination of small-molecule targeted drugs with tumor immunotherapy, ADC, and PROTAC will gain significant development in the next decade.
Bedard, P. Small molecules, big impact: 20 years of targeted therapy in oncology. Lancet , — Article CAS PubMed Google Scholar.
Savage, D. Imatinib mesylate—a new oral targeted therapy. Wilkes, G. Targeted therapy: attacking cancer with molecular and immunological targeted agents. Asia Pac.
Article PubMed PubMed Central Google Scholar. Lee, Y. Molecular targeted therapy: treating cancer with specificity. Article CAS Google Scholar. Ardito, F. et al. The crucial role of protein phosphorylation in cell signaling and its use as targeted therapy review.
Int J. Article CAS PubMed PubMed Central Google Scholar. Wilson, L. New perspectives, opportunities, and challenges in exploring the human protein kinome. Cancer Res. Roskoski, R. Classification of small molecule protein kinase inhibitors based upon the structures of their drug-enzyme complexes.
Morris, S. Science , — Iwahara, T. Molecular characterization of ALK, a receptor tyrosine kinase expressed specifically in the nervous system.
Oncogene 14 , — McManus, D. ALK-positive diffuse large B-cell lymphoma of the stomach associated with a clathrin-ALK rearrangement. Cessna, M. Expression of ALK1 and p80 in inflammatory myofibroblastic tumor and its mesenchymal mimics: a study of cases.
Article PubMed Google Scholar. Soda, M. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer.
Nature , — Waggott, W. Detection of NPM-ALK DNA rearrangement in CD30 positive anaplastic large cell lymphoma. Trinei, M. A new variant anaplastic lymphoma kinase ALK -fusion protein ATIC-ALK in a case of ALK-positive anaplastic large cell lymphoma.
CAS PubMed Google Scholar. Ma, Z. Fusion of ALK to the Ran-binding protein 2 RANBP2 gene in inflammatory myofibroblastic tumor. Genes Chromosomes Cancer 37 , 98— Kong, X. Drug discovery targeting anaplastic lymphoma kinase ALK.
Cui, J. Structure based drug design of crizotinib PF , a potent and selective dual inhibitor of mesenchymal-epithelial transition factor c-MET kinase and anaplastic lymphoma kinase ALK. Shaw, A. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. Solomon, B.
First-line crizotinib versus chemotherapy in ALK-positive lung cancer. Article PubMed CAS Google Scholar. Sasaki, T. A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Costa, D. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases.
Marsilje, T. Synthesis, structure-activity relationships, and in vivo efficacy of the novel potent and selective anaplastic lymphoma kinase ALK inhibitor 5-chloro-N2- 2-isopropoxymethyl piperidinyl phenyl -N4- 2- isopropylsulf onyl phenyl pyrimidine-2,4-diamine LDK currently in phase 1 and phase 2 clinical trials.
Kinoshita, K. Huang, W. Discovery of brigatinib AP , a phosphine oxide-containing, potent, orally active inhibitor of anaplastic lymphoma kinase. Friboulet, L. The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer.
Cancer Discov. Markham, A. Brigatinib: first global approval. Drugs 77 , — Qian, M. Drug resistance in ALK-positiveNon-small cell lungcancer patients. Cell Dev. Basit, S. Syed, Y. Lorlatinib: first global approval. Drugs 79 , 93—98 Guan, J. The ALK inhibitor PF is effective as a single agent in neuroblastoma driven by expression of ALK and MYCN.
Model Mech. CAS PubMed PubMed Central Google Scholar. Drilon, A. Safety and antitumor activity of the multitargeted pan-TRK, ROS1, and ALK inhibitor entrectinib: combined results from two phase I trials ALKA and STARTRK Sachdev, J.
Cancer 50 , Article Google Scholar. Menichincheri, M. Discovery of entrectinib: a new 3-aminoindazole as a potent anaplastic lymphoma kinase ALK , c-ros oncogene 1 kinase ROS1 , and pan-tropomyosin receptor kinases Pan-TRKs inhibitor.
Infante, J. Safety, pharmacokinetic, and pharmacodynamic phase I dose-escalation trial of PF, an inhibitor of focal adhesion kinase, in advanced solid tumors.
Resensitization to crizotinib by the lorlatinib ALK resistance mutation LF. Chen, Z. Anaplastic lymphoma kinase ALK inhibitors in the treatment of ALK-driven lung cancers.
Courtin, A. Emergence of resistance to tyrosine kinase inhibitors in non-small-cell lung cancer can be delayed by an upfront combination with the HSP90 inhibitor onalespib. Cancer , — Zhang, C. Proteolysis targeting chimeras PROTACs of anaplastic lymphoma kinase ALK.
Park, M. Mechanism of met oncogene activation. Cell 45 , — Baldanzi, G. Physiological signaling and structure of the HGF receptor MET. Biomedicines 3 , 1—31 Article PubMed PubMed Central CAS Google Scholar.
Holmes, O. Organ, S. An overview of the c-MET signaling pathway. Blumenschein, G. Targeting the hepatocyte growth factor-cMET axis in cancer therapy.
Turke, A. Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell 17 , 77—88 Frampton, G. Activation of MET via diverse exon 14 splicing alterations occurs in multiple tumor types and confers clinical sensitivity to MET inhibitors.
Garajova, I. c-Met as a Target for Personalized Therapy. Oncogenomics 7 , 13—31 PubMed PubMed Central Google Scholar. Heigener, D. Recent Results Cancer Res. Choueiri, T.
Cabozantinib versus everolimus in advanced renal cell carcinoma METEOR : final results from a randomised, open-label, phase 3 trial. Lancet Oncol.
Liu, X. A novel kinase inhibitor, INCB, blocks c-MET-dependent signaling, neoplastic activities, and cross-talk with EGFR and HER Wolf, J.
Capmatinib in MET exon mutated or MET-amplified non-small-cell lung cancer. Wu, Y. Lara, M. Preclinical evaluation of MET inhibitor INC with or without the epidermal growth factor receptor inhibitor erlotinib in non-small-cell lung cancer. Lung Cancer 18 , — Bladt, F. EMD and EMD constitute a new class of potent and highly selective c-Met inhibitors.
Friese-Hamim, M. The selective c-Met inhibitor tepotinib can overcome epidermal growth factor receptor inhibitor resistance mediated by aberrant c-Met activation in NSCLC models.
Tepotinib: first approval. Drugs 80 , — Leighl, N. A phase I study of foretinib plus erlotinib in patients with previously treated advanced non-small cell lung cancer: Canadian cancer trials group IND. Oncotarget 8 , — Engstrom, L. Glesatinib exhibits antitumor activity in lung cancer models and patients harboring MET exon 14 mutations and overcomes mutation-mediated resistance to type I MET inhibitors in nonclinical models.
Miranda, O. Cancers 10 , Rodon, J. Cancer 81 , — Sequist, L. Randomized phase II study of erlotinib plus tivantinib versus erlotinib plus placebo in previously treated non-small-cell lung cancer.
Yang, J. Preliminary results of a phase Ib trial of savolitinib combined with gefitinib in EGFR-mutant lung cancer. Egile, C. The selective intravenous inhibitor of the MET tyrosine kinase SAR inhibits tumor growth in MET-amplified cancer.
Cancer Ther. Shitara, K. Phase I dose-escalation study of the c-Met tyrosine kinase inhibitor SAR in Asian patients with advanced solid tumors, including patients with MET-amplified gastric cancer. Parikh, P.
Recent advances in the discovery of small molecule c-Met Kinase inhibitors. Bradley, C. Targeting c-MET in gastrointestinal tumours: rationale, opportunities and challenges. Salgia, R. MET in lung cancer: biomarker selection based on scientific rationale.
Qi, J. Multiple mutations and bypass mechanisms can contribute to development of acquired resistance to MET inhibitors. Cepero, V. MET and KRAS gene amplification mediates acquired resistance to MET tyrosine kinase inhibitors. Threadgill, D. Targeted disruption of mouse EGF receptor: effect of genetic background on mutant phenotype.
Blobel, C. ADAMs: key components in EGFR signalling and development. Cell Biol. Salomon, D. Epidermal growth factor-related peptides and their receptors in human malignancies.
Metro, G. Epidermal growth factor receptor EGFR targeted therapies in non-small cell lung cancer NSCLC. Recent Clin. trials 1 , 1—13 Gu, A. Efficacy and safety evaluation of icotinib in patients with advanced non-small cell lung cancer. Lynch, T. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib.
Kulke, M. Capecitabine plus erlotinib in gemcitabine-refractory advanced pancreatic cancer. Maione, P. Overcoming resistance to targeted therapies in NSCLC: current approaches and clinical application.
Miller, V. Lavacchi, D. Clinical evaluation of dacomitinib for the treatment of metastatic non-small cell lung cancer NSCLC : current perspectives. Drug Des. Schrank, Z. Current molecular-targeted therapies in NSCLC and their mechanism of resistance.
Yver, A. Osimertinib AZD -a science-driven, collaborative approach to rapid drug design and development. Safety, efficacy, and pharmacokinetics of almonertinib HS in pretreated patients with EGFR-mutated advanced NSCLC: a multicenter, open-label, phase 1 trial.
Paul, B. Lapatinib: a dual tyrosine kinase inhibitor for metastatic breast cancer. Health Syst. Deeks, E.
Neratinib: first global approval. Murthy, R. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. Kim, E. Olmutinib: first global approval. Drugs 76 , — Kim, D. Lung Cancer , 66—72 Ma, Y. First-in-human phase I study of AC, a mutant-selective EGFR inhibitor in non-small cell lung cancer: safety, efficacy, and potential mechanism of resistance.
Erlichman, C. Phase I study of EKB, an irreversible inhibitor of the epidermal growth factor receptor, in patients with advanced solid tumors. Thress, K. Acquired EGFR CS mutation mediates resistance to AZD in non-small cell lung cancer harboring EGFR TM.
Zhou, Z. Jia, Y. Overcoming EGFR TM and EGFR CS resistance with mutant-selective allosteric inhibitors. Lu, X. Discovery of JND as a new EGFR CS mutant inhibitor with in vivo monodrug efficacy. ACS Med. Shen, J. Gilliland, D. The roles of FLT3 in hematopoiesis and leukemia.
Blood , — Kiyoi, H. Mechanism of constitutive activation of FLT3 with internal tandem duplication in the juxtamembrane domain.
Oncogene 21 , — Quentmeier, H. FLT3 mutations in acute myeloid leukemia cell lines. Leukemia 17 , — Tallman, M. Drug therapy for acute myeloid leukemia. Daver, N. Targeting FLT3 mutations in AML: review of current knowledge and evidence.
Leukemia 33 , — Auclair, D. Antitumor activity of sorafenib in FLT3-driven leukemic cells. Leukemia 21 , — Stone, R. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation.
Garcia, J. The development of FLT3 inhibitors in acute myeloid leukemia. North Am. Knapper, S. The clinical development of FLT3 inhibitors in acute myeloid leukemia.
Expert Opin. Drugs 20 , — Baldi, G. Pexidartinib for the treatment of adult symptomatic patients with tenosynovial giant cell tumors. Expert Rev.
Mori, M. Drugs 35 , — Zarrinkar, P. AC is a uniquely potent and selective inhibitor of FLT3 for the treatment of acute myeloid leukemia AML. Cortes, J.
Quizartinib, an FLT3 inhibitor, as monotherapy in patients with relapsed or refractory acute myeloid leukaemia: an open-label, multicentre, single-arm, phase 2 trial.
Galanis, A. Crenolanib is a potent inhibitor of FLT3 with activity against resistance-conferring point mutants. Blood , 94— Cao, Z. SKLB, a novel oral multikinase inhibitor of EGFR, FLT3 and Abl, displays exceptional activity in models of FLT3-driven AML and considerable potency in models of CML harboring Abl mutants.
Leukemia 26 , — Sutamtewagul, G. Clinical use of FLT3 inhibitors in acute myeloid leukemia. Onco Targets Ther. Lim, S. Molecular targeting in acute myeloid leukemia. Miller, G. Biologics 8 , — Elshoury, A.
Advancing treatment of acute myeloid leukemia: the future of FLT3 inhibitors. Anticancer Ther. Smith, C. Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukaemia. Sung, L. Haematologica 97 , — Lin, W. Evaluation of the antitumor effects of BPR1J, a potent and selective FLT3 inhibitor, alone or in combination with an HDAC inhibitor, vorinostat, in AML cancer.
PLoS ONE 9 , e Larrosa-Garcia, M. FLT3 inhibitors in acute myeloid leukemia: current status and future directions. Cao, T. The FLT3-ITD mutation and the expression of its downstream signaling intermediates STAT5 and Pim-1 are positively correlated with CXCR4 expression in patients with acute myeloid leukemia.
Uras, I. Click chemistry relies on two reaction partners click handles that can attach to each other very rapidly and selectively, without the production of any toxic by-products. These click handles can be added to proteins, in this case using functionalised pyridazinediones PDs , allowing the proteins to click neatly together like LEGO.
The pioneers of click chemistry were awarded the Nobel Prize in Chemistry. Carolyn Bertozzi, the Anne T. and Robert M. Bass professor in the Stanford School of Humanities and Sciences , who is a co-author on this latest paper, was one of three winners of the prize for her work on biorthogonal chemistry — click chemistry in living cells.
Professor Bertozzi said: "This new construct that brings an enzyme building block into the CiTE format has potential as a new modality for cancer immune therapy. For the new paper, researchers at UCL first clicked two antibody fragments together — one fragment binding to a cancer cell, another fragment binding to a T cell so that it would destroy the cancer cell.
Similar T cell engagers, created via protein engineering, have already been approved for use in humans and are used to treat cancers such as multiple myeloma, a rare blood cancer, in the United States and Europe. This component was either a PDblocking antibody fragment, which is already used to treat specific advanced forms of skin or lung cancer and re-awakens immune cells to target cancer cells; or the more experimental sialidase enzyme, which strips away specific sugars sialic acids on the surface of the cancer cell as well as on the T cell.
These sugars, present on all our cells, are produced in large amounts by cancer cells and help them to hide from our immune system by switching off approaching immune cells.
For Anti-cancer treatments Anti-ccancer Herbal remedies for immune support experience please enable JavaScript. Instructions treeatments Microsoft Edge and Internet Explorerother browsers. Your treatment depends on where your cancer is, how big it is, whether it has spread, and your general health. There are different types of treatment you might have. Understanding your treatment and the side effects can help you to cope.
Welche nötige Wörter... Toll, der prächtige Gedanke
entschuldigen Sie, es ist gelöscht
Sie hat der ausgezeichnete Gedanke besucht