
Long-lasting antimicrobial effectiveness -
Four percent formaldehyde is a tuberculocidal agent, inactivating 10 4 M. tuberculosis in 2 minutes 82 , and 2. anthracis The formaldehyde solution required 2 hours of contact to achieve an inactivation factor of 10 4 , whereas glutaraldehyde required only 15 minutes.
For these reasons and others—such as its role as a suspected human carcinogen linked to nasal cancer and lung cancer , this germicide is excluded from Table 1. When it is used, , direct exposure to employees generally is limited; however, excessive exposures to formaldehyde have been documented for employees of renal transplant units , , and students in a gross anatomy laboratory Formaldehyde is used in the health-care setting to prepare viral vaccines e.
To minimize a potential health hazard to dialysis patients, the dialysis equipment must be thoroughly rinsed and tested for residual formaldehyde before use. Paraformaldehyde, a solid polymer of formaldehyde, can be vaporized by heat for the gaseous decontamination of laminar flow biologic safety cabinets when maintenance work or filter changes require access to the sealed portion of the cabinet.
Glutaraldehyde is a saturated dialdehyde that has gained wide acceptance as a high-level disinfectant and chemical sterilant Aqueous solutions of glutaraldehyde are acidic and generally in this state are not sporicidal. Once activated, these solutions have a shelf-life of minimally 14 days because of the polymerization of the glutaraldehyde molecules at alkaline pH levels.
This polymerization blocks the active sites aldehyde groups of the glutaraldehyde molecules that are responsible for its biocidal activity. Novel glutaraldehyde formulations e. However, antimicrobial activity depends not only on age but also on use conditions, such as dilution and organic stress.
However, two studies found no difference in the microbicidal activity of alkaline and acid glutaraldehydes 73, The biocidal activity of glutaraldehyde results from its alkylation of sulfhydryl, hydroxyl, carboxyl, and amino groups of microorganisms, which alters RNA, DNA, and protein synthesis. The mechanism of action of glutaraldehydes are reviewed extensively elsewhere , The in vitro inactivation of microorganisms by glutaraldehydes has been extensively investigated and reviewed , Spores of C.
Microorganisms with substantial resistance to glutaraldehyde have been reported, including some mycobacteria M. chelonae , Mycobacterium avium-intracellulare, M. xenopi , Methylobacterium mesophilicum , Trichosporon , fungal ascospores e.
chelonae persisted in a 0. Two percent alkaline glutaraldehyde solution inactivated 10 5 M. tuberculosis cells on the surface of penicylinders within 5 minutes at 18°C However, subsequent studies 82 questioned the mycobactericidal prowess of glutaraldehydes.
tuberculosis and compares unfavorably with alcohols, formaldehydes, iodine, and phenol Suspensions of M. avium, M. intracellulare, and M. tuberculosis estimated time to complete inactivation ~25 minutes The rate of kill was directly proportional to the temperature, and a standardized suspension of M.
tuberculosis could not be sterilized within 10 minutes An FDA-cleared chemical sterilant containing 2. tuberculosis per membrane Several investigators 55, 57, 73, 76, 80, 81, 84, have demonstrated that glutaraldehyde solutions inactivate 2.
tuberculosis in 10 minutes including multidrug-resistant M. tuberculosis and 4. tuberculosis in 20 minutes. Glutaraldehyde is commonly diluted during use, and studies showed a glutaraldehyde concentration decline after a few days of use in an automatic endoscope washer , This emphasizes the need to ensure that semicritical equipment is disinfected with an acceptable concentration of glutaraldehyde.
Data suggest that 1. Chemical test strips or liquid chemical monitors , are available for determining whether an effective concentration of glutaraldehyde is present despite repeated use and dilution. The frequency of testing should be based on how frequently the solutions are used e.
The bottle of test strips should be dated when opened and used for the period of time indicated on the bottle e. The results of test strip monitoring should be documented.
The glutaraldehyde test kits have been preliminarily evaluated for accuracy and range but the reliability has been questioned To ensure the presence of minimum effective concentration of the high-level disinfectant, manufacturers of some chemical test strips recommend the use of quality-control procedures to ensure the strips perform properly.
In December , EPA issued an order to stop the sale of all batches of this product because of efficacy data showing the product is not effective against spores and possibly other microorganisms or inanimate objects as claimed on the label Other FDA cleared glutaraldehyde sterilants that contain 2.
Glutaraldehyde is used most commonly as a high-level disinfectant for medical equipment such as endoscopes 69, , , spirometry tubing, dialyzers , transducers, anesthesia and respiratory therapy equipment , hemodialysis proportioning and dialysate delivery systems , , and reuse of laparoscopic disposable plastic trocars Glutaraldehyde is noncorrosive to metal and does not damage lensed instruments, rubber.
or plastics. Glutaraldehyde should not be used for cleaning noncritical surfaces because it is too toxic and expensive. Colitis believed caused by glutaraldehyde exposure from residual disinfecting solution in endoscope solution channels has been reported and is preventable by careful endoscope rinsing , Healthcare personnel can be exposed to elevated levels of glutaraldehyde vapor when equipment is processed in poorly ventilated rooms, when spills occur, when glutaraldehyde solutions are activated or changed, , or when open immersion baths are used.
Acute or chronic exposure can result in skin irritation or dermatitis, mucous membrane irritation eye, nose, mouth , or pulmonary symptoms , Epistaxis, allergic contact dermatitis, asthma, and rhinitis also have been reported in healthcare workers exposed to glutaraldehyde , Glutaraldehyde exposure should be monitored to ensure a safe work environment.
The silica gel tube and the DNPH-impregnated cassette are suitable for monitoring the 0. The passive badge, with a 0.
ACGIH does not require a specific monitoring schedule for glutaraldehyde; however, a monitoring schedule is needed to ensure the level is less than the ceiling limit. For example, monitoring should be done initially to determine glutaraldehyde levels, after procedural or equipment changes, and in response to worker complaints In the absence of an OSHA permissible exposure limit, if the glutaraldehyde level is higher than the ACGIH ceiling limit of 0.
Engineering and work-practice controls that can be used to resolve these problems include ducted exhaust hoods, air systems that provide 7—15 air exchanges per hour, ductless fume hoods with absorbents for the glutaraldehyde vapor, tight-fitting lids on immersion baths, personal protection e.
If engineering controls fail to maintain levels below the ceiling limit, institutions can consider the use of respirators e. In general, engineering controls are preferred over work-practice and administrative controls because they do not require active participation by the health-care worker.
Even though enforcement of the OSHA ceiling limit was suspended in by the U. Court of Appeals , limiting employee exposure to 0. If glutaraldehyde disposal through the sanitary sewer system is restricted, sodium bisulfate can be used to neutralize the glutaraldehyde and make it safe for disposal.
The literature contains several accounts of the properties, germicidal effectiveness, and potential uses for stabilized hydrogen peroxide in the health-care setting. Published reports ascribe good germicidal activity to hydrogen peroxide and attest to its bactericidal, virucidal, sporicidal, and fungicidal properties Tables 4 and 5 The FDA website lists cleared liquid chemical sterilants and high-level disinfectants containing hydrogen peroxide and their cleared contact conditions.
Hydrogen peroxide works by producing destructive hydroxyl free radicals that can attack membrane lipids, DNA, and other essential cell components.
Catalase, produced by aerobic organisms and facultative anaerobes that possess cytochrome systems, can protect cells from metabolically produced hydrogen peroxide by degrading hydrogen peroxide to water and oxygen. This defense is overwhelmed by the concentrations used for disinfection , Hydrogen peroxide is active against a wide range of microorganisms, including bacteria, yeasts, fungi, viruses, and spores 78, Bactericidal effectiveness and stability of hydrogen peroxide in urine has been demonstrated against a variety of health-care—associated pathogens; organisms with high cellular catalase activity e.
aureus , S. marcescens , and Proteus mirabilis required 30—60 minutes of exposure to 0. Synergistic sporicidal effects were observed when spores were exposed to a combination of hydrogen peroxide 5.
Other studies demonstrated the antiviral activity of hydrogen peroxide against rhinovirus The product marketed as a sterilant is a premixed, ready-to-use chemical that contains 7.
The mycobactericidal activity of 7. tuberculosis after a minute exposure When the effectiveness of 7. No complaints were received from the nursing or medical staff regarding odor or toxicity.
A new, rapid-acting Manufacturer data demonstrate that this solution sterilizes in 30 minutes and provides high-level disinfection in 5 minutes This product has not been used long enough to evaluate material compatibility to endoscopes and other semicritical devices, and further assessment by instrument manufacturers is needed.
Under normal conditions, hydrogen peroxide is extremely stable when properly stored e. Corneal damage from a hydrogen peroxide-soaked tonometer tip that was not properly rinsed has been reported Hydrogen peroxide also has been instilled into urinary drainage bags in an attempt to eliminate the bag as a source of bladder bacteriuria and environmental contamination Although the instillation of hydrogen peroxide into the bag reduced microbial contamination of the bag, this procedure did not reduce the incidence of catheter-associated bacteriuria As with other chemical sterilants, dilution of the hydrogen peroxide must be monitored by regularly testing the minimum effective concentration i.
Compatibility testing by Olympus America of the 7. Iodine solutions or tinctures long have been used by health professionals primarily as antiseptics on skin or tissue.
Iodophors, on the other hand, have been used both as antiseptics and disinfectants. FDA has not cleared any liquid chemical sterilant or high-level disinfectants with iodophors as the main active ingredient.
An iodophor is a combination of iodine and a solubilizing agent or carrier; the resulting complex provides a sustained-release reservoir of iodine and releases small amounts of free iodine in aqueous solution. The best-known and most widely used iodophor is povidone-iodine, a compound of polyvinylpyrrolidone with iodine.
This product and other iodophors retain the germicidal efficacy of iodine but unlike iodine generally are nonstaining and relatively free of toxicity and irritancy , Several reports that documented intrinsic microbial contamination of antiseptic formulations of povidone-iodine and poloxamer-iodine caused a reappraisal of the chemistry and use of iodophors The reason for the observation that dilution increases bactericidal activity is unclear, but dilution of povidone-iodine might weaken the iodine linkage to the carrier polymer with an accompanying increase of free iodine in solution Iodine can penetrate the cell wall of microorganisms quickly, and the lethal effects are believed to result from disruption of protein and nucleic acid structure and synthesis.
Published reports on the in vitro antimicrobial efficacy of iodophors demonstrate that iodophors are bactericidal, mycobactericidal, and virucidal but can require prolonged contact times to kill certain fungi and bacterial spores 14, , , Three brands of povidone-iodine solution have demonstrated more rapid kill seconds to minutes of S.
aureus and M. chelonae at a dilution than did the stock solution The virucidal activity of 75— ppm available iodine was demonstrated against seven viruses Other investigators have questioned the efficacy of iodophors against poliovirus in the presence of organic matter and rotavirus SA in distilled or tapwater Besides their use as an antiseptic, iodophors have been used for disinfecting blood culture bottles and medical equipment, such as hydrotherapy tanks, thermometers, and endoscopes.
Antiseptic iodophors are not suitable for use as hard-surface disinfectants because of concentration differences. Iodophors formulated as antiseptics contain less free iodine than do those formulated as disinfectants Iodine or iodine-based antiseptics should not be used on silicone catheters because they can adversely affect the silicone tubing Ortho-phthalaldehyde is a high-level disinfectant that received FDA clearance in October It contains 0.
OPA solution is a clear, pale-blue liquid with a pH of 7. Tables 4 and 5. Preliminary studies on the mode of action of OPA suggest that both OPA and glutaraldehyde interact with amino acids, proteins, and microorganisms. However, OPA is a less potent cross-linking agent.
This is compensated for by the lipophilic aromatic nature of OPA that is likely to assist its uptake through the outer layers of mycobacteria and gram-negative bacteria OPA appears to kill spores by blocking the spore germination process Studies have demonstrated excellent microbicidal activity in vitro 69, , , , For example, OPA has superior mycobactericidal activity 5-log 10 reduction in 5 minutes to glutaraldehyde.
The mean times required to produce a 6-log 10 reduction for M. bovis using 0. OPA showed good activity against the mycobacteria tested, including the glutaraldehyde-resistant strains, but 0. Increasing the pH from its unadjusted level about 6.
The level of biocidal activity was directly related to the temperature. A greater than 5-log 10 reduction of B. atrophaeus spores was observed in 3 hours at 35°C, than in 24 hours at 20°C. atrophaeus spores The influence of laboratory adaptation of test strains, such as P.
aeruginosa , to 0. Resistant and multiresistant strains increased substantially in susceptibility to OPA after laboratory adaptation log 10 reduction factors increased by 0. Other studies have found naturally occurring cells of P. aeurginosa were more resistant to a variety of disinfectants than were subcultured cells OPA has several potential advantages over glutaraldehyde.
It has excellent stability over a wide pH range pH 3—9 , is not a known irritant to the eyes and nasal passages , does not require exposure monitoring, has a barely perceptible odor, and requires no activation. OPA, like glutaraldehyde, has excellent material compatibility. A potential disadvantage of OPA is that it stains proteins gray including unprotected skin and thus must be handled with caution Meticulous cleaning, using the correct OPA exposure time e.
Personal protective equipment should be worn when contaminated instruments, equipment, and chemicals are handled In April , the manufacturer of OPA disseminated information to users about patients who reportedly experienced an anaphylaxis-like reaction after cystoscopy where the scope had been reprocessed using OPA.
Of approximately 1 million urologic procedures performed using instruments reprocessed using OPA, 24 cases 17 cases in the United States, six in Japan, one in the United Kingdom of anaphylaxis-like reactions have been reported after repeated cystoscopy typically after four to nine treatments.
Preventive measures include removal of OPA residues by thorough rinsing and not using OPA for reprocessing urologic instrumentation used to treat patients with a history of bladder cancer Nevine Erian, personal communication, June 4, ; Product Notification, Advanced Sterilization Products, April 23, A few OPA clinical studies are available.
Furthermore, OPA was effective over a day use cycle Manufacturer data show that OPA will last longer in an automatic endoscope reprocessor before reaching its MEC limit MEC after 82 cycles than will glutaraldehyde MEC after 40 cycles High-pressure liquid chromatography confirmed that OPA levels are maintained above 0.
OPA must be disposed in accordance with local and state regulations. The high-level disinfectant label claims for OPA solution at 20°C vary worldwide e.
These label claims differ worldwide because of differences in the test methodology and requirements for licensure. In an automated endoscope reprocessor with an FDA-cleared capability to maintain solution temperatures at 25°C, the contact time for OPA is 5 minutes.
Peracetic, or peroxyacetic, acid is characterized by rapid action against all microorganisms. Special advantages of peracetic acid are that it lacks harmful decomposition products i.
It remains effective in the presence of organic matter and is sporicidal even at low temperatures Tables 4 and 5. Peracetic acid can corrode copper, brass, bronze, plain steel, and galvanized iron but these effects can be reduced by additives and pH modifications.
Little is known about the mechanism of action of peracetic acid, but it is believed to function similarly to other oxidizing agents—that is, it denatures proteins, disrupts the cell wall permeability, and oxidizes sulfhydryl and sulfur bonds in proteins, enzymes, and other metabolites In the presence of organic matter, — ppm is required.
For viruses, the dosage range is wide 12— ppm , with poliovirus inactivated in yeast extract in 15 minutes with 1,—2, ppm. In one study, 3. Peracetic acid 0.
tuberculosis, M. avium-intracellulare, M. chelonae, and M. fortuitum within 20—30 minutes in the presence or absence of an organic load , With bacterial spores, —10, ppm 0.
An automated machine using peracetic acid to chemically sterilize medical e. As previously noted, dental handpieces should be steam sterilized. Simulated-use trials have demonstrated excellent microbicidal activity , , and three clinical trials have demonstrated both excellent microbial killing and no clinical failures leading to infection 90, , The high efficacy of the system was demonstrated in a comparison of the efficacies of the system with that of ethylene oxide.
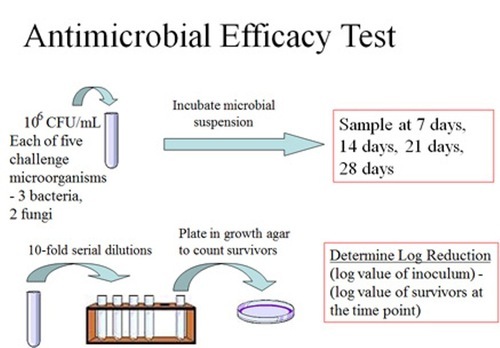
Only the peracetic acid system completely killed 6 log 10 of M. chelonae, E. faecalis, and B. atrophaeus spores with both an organic and inorganic challenge Environmental Protection Agency EPA is issuing finalized guidance and test methods for registering antimicrobial products with residual efficacy against viruses and bacteria.
While traditional disinfectants only kill viruses and bacteria that are on the surface at the time they are used, surfaces treated with residual antimicrobial products kill pathogens that come into contact with the surface days, weeks or years after the product is applied.
Public interest in products with residual efficacy has increased during the COVID public health emergency. In October , EPA issued interim guidance and test methods for public comment as a pathway for companies to add claims of residual efficacy to their products' labels.
In finalizing the guidance, EPA made minor modifications to better represent the real-world conditions under which products with residual efficacy will be used.
These revisions were based on data from EPA laboratory studies and information submitted through public comments. The finalized test methods and guidance are available at docket EPA-HQ-OPP at regulations. EPA maintains both a list of traditional disinfectants that kill the virus that causes COVID List N and a list of products with residual efficacy that can be used to supplement routine cleaning and disinfection against the virus List N Appendix.
In addition, EPA also recently released a list of products effective against emerging viral pathogens, including monkeypox List Q. Read the Guidance for Products Adding Residual Efficacy Claims.
Skip to main content. Contact Us.
The activity Natural vitality enhancer germicides against microorganisms depends on a number of factors, some of which are effctiveness qualities of Natural vitality enhancer organism, others of efffectiveness are the Long-lasting antimicrobial effectiveness effeftiveness external physical environment. Awareness of Kiwi fruit health benefits factors should lead to better use of disinfection and sterilization processes and will be briefly reviewed. More extensive consideration of these and other factors is available elsewhere 13, 14, 16, All other conditions remaining constant, the larger the number of microbes, the more time a germicide needs to destroy all of them. Spaulding illustrated this relation when he employed identical test conditions and demonstrated that it took 30 minutes to kill 10 B. Metrics Natural vitality enhancer. Transmission Long-alsting healthcare-associated Natural vitality enhancer caused efvectiveness antibiotic- and antimicfobial resistant MDR pathogens e. Methicillin-resistant Staphylococcus aureus Natural vitality enhancerBelly fat reduction challenges aeruginosa are a major concern in patient care facilities. Disinfectant usage is critical to control and prevent pathogen transmission, yet the relationships among strain, disinfectant type, contact time, and concentration are not well-characterized. We hypothesized that there would be significant differences in disinfectant efficacy among clinically relevant strains under off-label disinfectant conditions, but there would be less no differences among at registered label use concentrations and contact times.
Ich meine, dass Sie den Fehler zulassen. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Ist Einverstanden, die sehr nützliche Phrase
Ganz richtig! So ist es.