
Brain health and neurodegenerative diseases prevention -
Though research is still evolving, evidence is strong that people can reduce their risk by making key lifestyle changes, including participating in regular activity and maintaining good heart health. Based on this research, the Alzheimer's Association offers 10 Ways to Love Your Brain — a collection of tips that can reduce the risk of cognitive decline.
Sprint for Discovery New research shows there are things we can do to reduce the risk of mild cognitive impairment and dementia. A longstanding question is why some people develop hallmark Alzheimer's plaques and tangles but do not develop the symptoms of Alzheimer's.
Vascular disease may help researchers eventually find an answer. Some autopsy studies suggest that plaques and tangles may be present in the brain without causing symptoms of cognitive decline unless the brain also shows evidence of vascular disease. Regular physical exercise may be a beneficial strategy to lower the risk of Alzheimer's and vascular dementia.
Exercise may directly benefit brain cells by increasing blood and oxygen flow in the brain. Because of its known cardiovascular benefits, a medically approved exercise program is a valuable part of any overall wellness plan.
Current evidence suggests that heart-healthy eating may also help protect the brain. Heart-healthy eating includes limiting the intake of sugar and saturated fats and making sure to eat plenty of fruits, vegetables, and whole grains.
No one diet is best. Two diets that have been studied and may be beneficial to lowering the risk of Alzheimer's are the DASH Dietary Approaches to Stop Hypertension diet and the Mediterranean diet.
A number of studies indicate that maintaining strong social connections and keeping mentally active as we age might lower the risk of cognitive decline and Alzheimer's. Experts are not certain about the reason for this association. It may be due to direct mechanisms through which social and mental stimulation strengthen connections between nerve cells in the brain.
There appears to be a strong link between future risk of cognitive decline and serious head trauma , especially when injury involves loss of consciousness.
You can help reduce your risk of Alzheimer's and protect your head by:. While research is not yet conclusive — partially due to the need for more large-scale studies in diverse populations — certain lifestyle choices, such as physical activity and diet, may help support brain health and prevent Alzheimer's.
Many of these lifestyle changes have been shown to lower the risk of other diseases, like heart disease and diabetes, which have been linked to Alzheimer's. With few drawbacks and plenty of known benefits, healthy lifestyle choices can improve your health and possibly protect your brain.
In addition, taking care of your health now may help improve your outcomes in the long term, such as reducing your risk for Alzheimer's and dementia. Learn More: Brain Health You can help increase our knowledge by considering participation in a clinical study.
Our free clinical trial matching services, TrialMatch®, can help you find clinical trials in your area that are seeking volunteers. Learn More. Here are some things to keep in mind about the research underlying much of our current knowledge about possible prevention:.
In more detail, physical activity in animal models and humans increases anti-inflammatory factors [anti-inflammatory cytokines, cluster of differentiation and its receptor CDCDR , triggering receptor expression on myeloid cells 2 TREM2 , heat-shock proteins HSP , metabolic factors, brain-derived neurotrophic factors, anti-oxidants, stimulating the glymphatic system] and decreases pro-inflammatory factors [pro-inflammatory cytokines IL-1β and TNF-α, and chemokines chemokine C-C motif ligand 2 CCL2 and C-X-C motif chemokine ligand 10 CXCL10 , and toll-like receptor signaling pathway] Mee-Inta et al.
Physical activity in AD animal models decreases cellular and cognitive impairment by modulating neuroinflammation Kelly, ; Liu et al.
Outcomes were also observed in animal models of PD by decreasing pro-inflammatory factors and microglial activation, decreasing dopaminergic cell loss; thereby reducing akinesia, and improving motor coordination Tillerson et al. In HD animal models, exercise reduced striatal neuron loss, improved motor coordination and delayed cognitive decline Pang et al.
In MS animal models, exercise decreased pro-inflammatory cytokines and increased anti-inflammatory cytokines, and also attenuated the clinical score Bernardes et al. Exercise is also good for overall mental health by improving memory, cognition, sleep, and mood, and decreasing psychiatric symptoms like depression, stress, anxiety, and mood disorders.
Here, its affects are thought to be due to the production of neurotrophic factors, neurotransmitters, hormones, and growth of new CNS blood vessels, and by reducing neuroinflammation Mahalakshmi et al.
A study with college students showed that moderate-intensity exercise reduced symptoms of stress and depression while reducing levels of TNF-α Paolucci et al. In this regard, the COVID pandemic induced isolation and quarantine requirements contributed to the increased prevalence of psychiatric disorders such as anxiety and depression, and exercise is a valuable tool to combat it Hu et al.
Finally, physical activity can also improve the composition of the gut microbiome, decreasing peripheral and central inflammation, like microglial activation in the CNS Abraham et al. Evidence shows that there is a reciprocal link between a reduction of peripheral inflammation and neuroinflammation.
This explains the combined impact of a healthy diet and moderate exercise to prevent peripheral inflammation, neuroinflammation, neurodegenerative, and psychiatric disorders.
Although there is anatomical separation, recent evidence indicates that neuroinflammation in the brain might originate in the intestine through communication between the enteric and CNS, which is called the gut-brain axis.
Dietary intake determines the composition of the gut microbiota. Therefore, the precise content of the food eaten may affect brain health more directly than previously thought. Gut microbiota dysbiosis is linked to diseases within the entire body Petersen and Round, ; Novakovic et al.
The levels and balance of dietary elements such as fat, carbohydrate, gluten, alcohol, vitamins, and food allergens have a role in determining gut microbiota composition and whether inflammation is triggered in the gut. In the CNS, gut dysbiosis is associated with impaired mood, anxiety, depression, pain and impaired cognition and directly linked to neuroinflammation Cryan and Dinan, Furthermore, chronic intestinal inflammation has been linked to neuroinflammation, and development of neurodegenerative diseases Houser and Tansey, and bipolar disorder Muneer, Several dietary components, when eaten in excess, have been linked to gut inflammation and neuroinflammation.
Western diets that are high in red meat, saturated and trans fats, refined sugars and carbohydrate intake are linked to gut inflammation and a change in microbiota composition Agus et al. In contrast, other nutritional components unsaturated, polyunsaturated, and monounsaturated fat and dietary habits such as ketogenic and Mediterranean diets, and intermittent fasting, are neuroprotective and anti-inflammatory.
Adherence to some anti-inflammatory promoting diets can be challenging over long periods. Therefore, instead of suppressing components from the diet, balancing anti-inflammatory foods and habits may be critical to reduce neuroinflammation.
In the past, fats were considered bad for health, but now their health effects are nuanced depending on the type of fat. High consumption of some fats increases the risk of heart disease and diabetes Siri-Tarino et al. Dietary fats differ in their chemical structure, and therefore, the extent that they trigger inflammation and neuroinflammation.
Saturated and trans fats have the maximum number of hydrogen atoms bound to carbon atoms and are solid at room temperature. They are considered the least healthy fat, and are found in many foods, such as red meat, butter, palm and coconut oils, milk, cheese, ice cream, French fries and crackers Kris-Etherton et al.
Unsaturated fats have fewer hydrogen atoms bound to carbon atoms, mono-unsaturated fats have one unsaturated bond, whereas polyunsaturated fats have many. Mono and polyunsaturated fats are healthy and found in vegetables, nuts, fish mono ; avocado, olive and canola oil, almonds unsaturated ; walnut, sunflower oil, salmon, tuna poly.
There are two types of polyunsaturated fats - omega-3 and omega-6 fatty acids. Omega-3 fatty acids are found in oily fish, nuts, flaxseeds and leafy vegetables, and are considered the healthiest fat because they may reduce inflammation Murphy et al.
A common impact of excessive consumption of unhealthy fats and foods is an increase in neuroinflammation. A high fat diet HFD that contains a lot of saturated and trans fats, promotes pro-inflammatory changes in the small intestine, and activates the toll-like receptor 4 TLR4 , iNOS, COX-2, and nuclear factor kappa-light-chain-enhancer of activated B cells NF-κB Kim et al.
Subsequently, a HFD induces oxidative stress, neuroinflammation, tau hyperphosphorylation and neuron degeneration Anstey et al. In animal models, a HFD induces cognitive decline similar to the symptoms of AD, and amyloid accumulation on artery walls in the brain Lin et al.
Another nutrient that can trigger inflammation is gluten. People, even non-celiac, can be sensitive to gluten and gluten intolerance and sensitivity are often unrecognized and under-diagnosed.
Daulatzai reported that non-celiac gluten sensitivity can trigger gut dysbiosis, dysregulating the gut-brain axis by increasing intestinal permeability, entry of bacteria, bacterial toxins, and toxic digestive metabolites into the bloodstream, increasing neuroinflammation and BBB permeability, and subsequently increase the risk for an individual to develop dementia.
PD, AD, depression, anxiety, and schizophrenia are also believed to be linked to gluten intake, especially in celiac patients Levinta et al. However, data are limited and further research is needed Philip and White, Epidemiological and animal studies have revealed the broad underlying role that neuroinflammation may have in neurodegenerative disorders, regardless of the initiating trigger or events.
For example, metabolic disorders, such as obesity, activate neuroinflammation and are correlated to neurodegenerative disorders Maric et al.
When placed in the context that there is a worldwide epidemic of obesity, it remains critical to eat healthy foods that reduce inflammation and avoid foods that negatively change the composition of gut microbiota and trigger inflammation, such as a HFD.
Anti-inflammatory dietary components are found in many foods and plants, and they are well described in a recent review Rekatsina et al.
Naturally occurring common anti-inflammatories are found in pomegranates, medicinal plants, vitamin D, vitamin C, a Mediterranean diet and extra-virgin olive oil, flavonoids found in fruits, curcumin, resveratrol, aged garlic extract, walnuts, marine carotenoid astaxanthin found in seafood, omega-3 fatty acids, caffeine, and manuka honey Almasaudi et al.
Ingestion of these foods reduce chronic inflammation and neuroinflammation Rekatsina et al. These neuro inflammation reducing foods could be part of the prevention and treatment of neurodegenerative and psychiatric disorders, however, clinical studies are needed.
A specific dietary example is salvianolic acid B sal B , which is extracted from salvia miltiorrhiza bunge, a popular Chinese herb. Sal B abolishes neuroinflammatory responses in the hippocampus in a rat model of chronic mild stress-induced depression by inhibiting NOD-, LRR-, and pyrin domain-containing protein 3 NLRP3 inflammasome activation Huang et al.
Sal B also reduces MS severity by impairing Th1 and Th17 responses, limiting astrogliosis and infiltration of inflammatory cells into the CNS in a MS animal model Dong et al.
Sal B has anti-inflammatory effects in a model of traumatic brain injury—brain edema and motor deficits were reduced by inhibiting neutrophil infiltration, microglia activation, and pro-inflammatory cytokine production Chen et al.
IF is a practice associated with weight loss and calorie restriction where individuals refrain from eating for extended periods of the day, e. In addition to facilitating weight loss, IF has been shown to increase lifespan, reduce free radicals, attenuate age-related diseases and reduce cognitive and motor function decline Mattson, ; Mattson and Wan, ; Masoro, ; Gudden et al.
IF stimulates adaptive immune responses in rats, which suppress LPS-induced neuroinflammation in young and old animals. These results support the idea that IF could reduce the risk of neuroinflammation at any point in the life span, and cumulatively could significantly reduce the risk of neurodegenerative diseases linked to inflammatory responses Vasconcelos et al.
IF also decreases plasma inflammatory factors such as cortisol, IL-6 and TNF-α in a mouse model of stress, which was hypothesized to ameliorate cognitive function Shojaie et al. In a MS animal model, IF reduced inflammation, increased bacteria richness in the gut and ameliorated the clinical course of the disease, which has also been shown in MS patients Cignarella et al.
Similarly, in a mouse model of PD, IF attenuated dopaminergic neuron loss by upregulating neurotrophic factors and decreasing neuroinflammation Ojha et al. A ketogenic diet KD is a high fat, low carbohydrate diet with adequate levels of protein that shifts the body from glucose to fat metabolism.
As a consequence, the liver converts fats into ketones, which can serve as a major energy source for the brain.
A KD for 12 days and 8 weeks improved the quality of life and daily function in patients with AD Phillips et al. Emerging evidence shows that a KD induces systemic and neuroprotective anti-inflammatory effects. In rodent models of neurodegenerative and neuro-inflammatory disorders, a KD can reduce expression of pro-inflammatory cytokines and microglial activation Ruskin et al.
A KD is thought to improve psychiatric diseases such as mood disorders Brietzke et al. However, large scale studies and clinical trials are required to fully assess the impact of KD on the treatment or management of neurodegenerative and psychiatric disorders Jensen et al.
The gut-brain axis likely plays a key role in the development and progression of brain disorders. Other dietary compounds that maintain healthy microbiota and inflammation levels in the gut will also be important such as caffeine, probiotics and prebiotics Frank et al.
Nevertheless, food quality and quantity can be used to optimize health and wellbeing throughout the lifespan. Chronic alcohol consumption alters the gut microbiome, causes mucosal damage due to increased permeability to endotoxins, and causes systemic inflammation by activating monocytes and macrophages to secrete TNF-α and other pro-inflammatory cytokines Bode and Bode, ; Amin et al.
Systemic inflammation is a precursor of neuroinflammation, therefore, chronic alcohol consumption is also linked to the development of neurodegeneration Qin et al. Recent epidemiological studies show that compared to people who abstain from alcohol consumption, light-moderate alcohol consumption in any form i.
Moderate drinking is defined as a maximum of two standard drinks daily for women, and three for men. Several studies report that low alcohol consumption can promote anti-inflammatory and cytoprotective processes by reducing C-reactive protein CRP levels, and plasma markers of inflammation and pro-inflammatory cytokines such as IL-6 Albert et al.
On top of that, case-control and cohort studies show moderate alcohol consumption can lower the risk of dementia Ruitenberg et al. Polyphenolic components of red wine, such as resveratrol, reduce toxicity in an animal model of PD through their antioxidant and anti-inflammatory properties.
This reinforces the importance of moderate alcohol consumption as part of a balanced lifestyle for health. Stress is a state of the body and mind that occurs when an alerting, demanding, or threatening event occurs. The stress response is adaptive and can be behavioral, psychological, or physiological and is designed to promote survival.
Chronic or unpredictable stressors are deleterious and contribute to several neurodegenerative and psychiatric diseases. In contrast, short predictable stressors can be beneficial for cognition and emotion.
Clinical and experimental studies have shown that deleterious stress negatively impacts the immune function in adults Dhabhar, ; Seiler et al. Stress has been linked to the development of inflammatory diseases such as inflammatory bowel disorder Brzozowski et al.
It is also not surprising that stress has been linked, and may trigger, several psychiatric disorders such as posttraumatic stress disorder, anxiety disorders, depression and schizophrenia, and also the evolution of neurodegenerative diseases McLeod et al.
Moreover, the fetal basis of adult disease hypothesis introduced the concept that adult health and behavior are programmed in utero and shaped throughout life by exposure to new and previously experienced stressors via epigenetic mechanisms Barker et al.
Epigenetic mechanisms are changes in DNA methylation and histone modification, which do not modify the genetic code but modulate transcription and translation, reinforcing or inhibiting some genes, and regulate when and where corresponding proteins are expressed Lejarraga, These genes alter programming, thereby modifying responses following stimulation of metabolic and hormone regulators.
Changes in gene expression may affect metabolic responses throughout life. For example, prenatal exposure may contribute to health problems that arise later in life such as obesity, diabetes, cardiovascular disease, cancer, and PD.
Epigenetic changes persist even when the original triggering conditions are no longer present Ho and Tang, ; Lejarraga, In line with this, juvenile and early life stresses have been linked to long term meta-plasticity-like effects on inflammatory responses in adulthood, and this memory may increase susceptibility to neurodegenerative diseases in adult life Shtoots et al.
This enhanced inflammatory response to stressors is called behavioral meta-plasticity. These findings mean that early life stress can produce long lasting changes in the immune response and increased pro-inflammatory cytokine and chemokine expression, and increased recruitment of innate immune cells Carpenter et al.
Furthermore, stress in utero can increase the susceptibility for excessive neuroinflammation, anxiety and neurodegeneration in adulthood Desplats et al. Finally, the association between childhood trauma and plasma inflammatory biomarkers have been observed among 1, members of the Dunedin Multidisciplinary Health and Development Study through a longitudinal prospective study Danese et al.
Study members have been followed for 45 years since they were born in — in Dunedin, New Zealand Poulton et al. This study showed that cumulative experience to childhood maltreatment was associated with significantly elevated inflammation in adult life, with increased CRP and fibrinogen levels and leukocyte count Danese et al.
Other studies have subsequently tested this association, which is confirmed by meta-analysis reviews Coelho et al. In this context, it would be advantageous to reduce or eliminate deleterious stress from our lives and raise public awareness of the effect early life stress, maltreatment, and bullying has on mental health and wellbeing throughout the lifespan.
An association between loneliness and inflammation has been found and is currently of great interest due to the impact of the COVID pandemic on social isolation. In animal models, chronic stress followed by social isolation promotes depression by increasing microglia and astrocyte activity and reduced hippocampal neurogenesis in mice Du Preez et al.
More clinical and participatory action research needs to examine the impact of social isolation on neuroinflammation and the development of psychiatric and neurodegenerative diseases. Epidemiological studies obtained during or in the first 2 years after the COVID pandemic will add information to this field.
Mental health and wellbeing can be improved by individuals being aware of, and responding effectively, during periods of high stress. Increasingly, evidence supports the use of mindfulness meditation, and yoga, which are commonly used to manage wellbeing, and these practices decrease inflammation Twal et al.
For example, a recent meta-analysis study mentioned that breathing, meditation, yoga, and Tai Chi practice downregulated pro-inflammatory genes and NF-κB pathway Buric et al.
Mindfulness meditation is an intrinsic capacity of the human mind and has only recently been highlighted because it can improve human health and wellbeing. The increased telomerase activity protects the ends of chromosomes from DNA damage and plays a central protective role in cell fate and aging, therefore, is linked to a longer and healthier life.
However, this study needs to be replicated to understand the mechanisms linking mindfulness meditation and its positive effects on immunity and disease prevention. Finally, the stress-induced increase in neuroinflammation is reduced during and after mindfulness meditation Pascoe et al.
Several recent studies provide evidence that yoga reduces the harmful effects of stress and inflammaging. Yoga for 12 weeks slowed cellular aging and increased anti-inflammatory cytokines, and diminished pro-inflammatory cytokines and cortisol levels Tolahunase et al. A systematic review of randomized controlled trials mentioned that yoga decreases pro-inflammatory cytokines IL-1β, TNF-α, and IL-6 and should be part a complementary intervention for people at risk of diseases with an immunological component Falkenberg et al.
The length of individual sessions varied from 30 to 90 min; daily—once per week; and yoga was practiced for 1—6 months, with most studies including a 8—12 week yoga program.
Ideally, yoga should be practised regularly throughout life to produce a consistent decrease in pro-inflammatory cytokines Lurie, ; Magan and Yadav, These studies show that yoga may reduce neuroinflammation and the risk of neurodegenerative and psychiatric disorders in people living with chronic stress.
Most people live in an urban society with artificial environments containing moderate levels of pollution. Pollution is composed of particulate matter, ozone O 3 , carbon monoxide CO , sulfur dioxide SO 2 , nitrogen oxide NO , and lead Pb. These pollutants are stated to be hazardous to human health by the Environmental Protection Agency and are the most prevalent environmental risk factors linked to increased inflammation Craig et al.
These pollutants have also been linked to increased neuroinflammation and related neurodegenerative diseases such as PD and AD in humans and animal models Levesque et al. Analysis of brain tissues from people living in highly polluted areas shows increased levels of pro-inflammatory markers such as IL-1β and COX2, and BBB damage Calderon-Garciduenas et al.
Microglia are also chronically activated by either pro-inflammatory stimuli or in response to neuronal damage. There are three mechanisms underlying these effects Block and Calderón-Garcidueñas, First, components of air pollution may directly activate microglia.
Second, pro-inflammatory cytokines from the peripheral systemic inflammatory response can trigger neuroinflammation. Third, particles or cytokines derived from the periphery may damage neurons, which in turn activate microglia.
In support of this, inhalation exposure to air pollutants found in traffic triggers increased activity of matrix metalloproteinases MMP and degradation of tight junction proteins in mouse brain vasculature resulting in increased BBB permeability and an increase in neuroinflammation Oppenheim et al.
Conversely, populations with higher greenspace exposure are more likely to have good overall health Lee and Maheswaran, ; White et al. Studies show that walking or exercise in nature improves cognition and mood in people with major depressive disorder Berman et al.
Studies in countries with dense populations show that spending time in natural environments such as a forest, reduced levels of cortisol, increased levels of protective immune function levels of NK cell activity and reduced pro-inflammatory cytokines such as IL-6 and TNF-α Miyazaki et al.
Spending time outside, in forests, parks, mountains and oceans should be part of a healthy lifestyle and is sometimes recommended by doctors. In fact, in Scotland, medical doctors are now prescribing time spent in natural environments as treatments Carrell, ; Koselka et al.
However, green spaces need to be accessible for everyone. Therefore, city designs need to include safe green spaces so that all residents can maintain positive health.
Pesticides are widely used in the agricultural industry as well as in houses and offices to control weeds and insect manifestations.
Pesticides last a long time and are degraded slowly. Occupational exposure in agricultural, pesticide and extermination industries can be high, whereas home exposure through eating food and drinking water is variable. Harmful effects depend on the toxicity of the pesticide, preventative measures taken during its application, dose, and persistence of pesticide residues in the environment and ongoing exposure Damalas and Eleftherohorinos, Accumulating experimental and epidemiological evidence shows that the pathogenesis of many chronic neurodegenerative PD, AD, MS, HD, and ALS and psychiatric depression, anxiety, cognitive impairment, and autism disorders are exacerbated by pesticide exposure Dhaini, ; Parrón et al.
Exposure to pesticides can trigger damaging immune system effects and induce neurotoxicity Costa et al. Much research has been conducted on this topic and here we discuss a few examples. For a more detailed explanation of the neurotoxic effects of pesticides, epidemiological studies and neurotoxicity mechanisms, see recent reviews Xiao et al.
Epidemiological cohort and case-control studies have correlated an increased risk for PD to develop with pesticide exposure among greenspace workers, farmers, and horticulturists Hertzman et al. Many epidemiological studies have also linked pesticide exposure to increased risk of developing AD Gauthier et al.
Pesticide exposure also increases the risk of developing MS Parrón et al. Inflammation is a common mechanism of pesticide-induced neurotoxicity. In rodents, exposure to the pesticides paraquat and rotenone cause behavioral impairments, increase ROS and the pro-inflammatory cytokine TNF-α in the substantia nigra, and these neuroinflammation changes lead to the degeneration of the nigrostriatal dopaminergic system and parkinsonian motor symptoms Sherer et al.
Therefore, paraquat and rotenone have been used to model PD in many animal studies Uversky, ; Nisticò et al. Similarly in animal models of AD, paraquat, chlorpyrifos, and dichlorodiphenyldichloroethylene increase production of ROS, causing neuronal death and degeneration Tang, In a striatal neuron model of HD, the pesticide chlorpyrifos induces oxidative stress by production of ROS and neurotoxicity Dominah et al.
ROS induced by pesticides can trigger NLRP3 inflammasome in microglia leading to the production of IL-1β, exacerbating neuronal death and function Moloudizargari et al. Rotenone induces transcriptional changes in vitro similar to those observed in patients with autism such as free radical production and disrupts microtubules in neurons Pearson et al.
Moreover, rotenone activates microglia and astrocytes and increases pro-inflammatory cytokine production, which attach to cytokine receptors and initiate neurotoxic intracellular mechanisms and generation of iNOS and oxidative stress, damaging neurons. Experimental and epidemiological evidence shows a link between pesticide exposure and the increased incidence of developing neurodegenerative and psychiatric diseases, with neuroinflammation being an important common mechanism inducing neurotoxicity.
Agriculturalists and health experts understand the risks of pesticide exposure and many people are advocating for greater controls and reduced use of pesticides. This is an important first step. However, because health effects for most people are cumulative over a lifetime, it will take several decades before a population-based reduced risk of neurodegenerative and psychiatric disorders will be evident.
People living with neurodegenerative diseases, such as AD, PD, and MS, as well as psychiatric disorders such as depression and anxiety, experience sleep disorders. These conditions can induce a sleep disorder, but the genesis may also be that a sleep disorder contributes to brain disorders.
Previous studies show that poor sleep simulates peripheral immunity by increasing circulating pro-inflammatory cytokine levels, increasing inflammatory signaling pathways and increasing innate immunity Marshall and Born, ; Opp and Krueger, ; Qazi and Farraye, Sleep loss and disrupted sleep have been shown to induce acute Irwin et al.
Interestingly, 64 h of sleep deprivation increased leukocyte and natural killer cell function, which was reversed by sleep, suggesting that sleeping has the potential to reverse adverse effects of inflammation Dinges et al. Recently, sleep disorders have been considered a causal part of neuroinflammation found in neurodegenerative and psychiatric disorders.
Reduced sleep has been associated with increased secretion of pro-inflammatory cytokines such as TNF-α in the blood Vgontzas et al. Short term 6 h sleep deprivation causes a significant increase in B cells in the brain and elevates expression of the migration-related C-X-C chemokine receptor type 5 CXCR5 on B cells and its ligand CXCL13 in the meninges in mouse brains Korin et al.
B cells have cytokine-producing states and are antigen presenting cells, in addition to their antibody production function Tarlinton, Therefore, the neuroinflammation that occurs due to reduced sleep quality with neurodegenerative and psychiatric disorders exacerbates these conditions Ahnaou and Drinkenburg, Preparations of the cannabis plant Cannabis sativa have been used for thousands of years by different cultures for many purposes, including medicinal properties.
Its sedative and psychotropic effects mean the plant is used as a recreational drug throughout the world. Cannabinoids have been studied for their therapeutic properties in neuroinflammatory diseases. However, legal systems have categorized drugs as being socially acceptable alcohol and nicotine or unacceptable cannabis and others , which has slowed research examining the anti-inflammatory properties of cannabinoids.
Cannabidiol, the main non-psychotropic component, exerts anti-inflammatory effects by inhibiting the synthesis and release of pro-inflammatory molecules, like cytokines, NO and glial fibrillary acidic protein from activated astroglia Esposito et al. This is associated with inhibition of p38 mitogen-activated protein kinase MAPK and regulation of NF-κB, which controls transcription of pro-inflammatory factors Esposito et al.
Moreover, controlling these pro-inflammatory molecules regulates microglia migration, which is involved in neuroinflammation, preventing recruitment of microglia to lesion sites Walter et al. Cannabinoids act directly on cannabinoid type 1 and type 2 CB1 and CB2 receptors, transient receptor potential cation channel subfamily V member 1 TRPV1 largely distributed within the CNS.
A recent review shows that cannabinoid binding to CB1, CB2, and TRPV1 is neuroprotective, decreases TNF-α CB1 and 2 and IL CB1 , inhibits chemokine production by astrocytes CB2 , and reduces proliferation CB2 , migration CB2 and activates TRVP1 microglia Antonazzo et al.
These findings are promising as an agent for delaying the progression of neurodegenerative diseases such as HD and PD. However, clinical trials are needed to examine the efficacy of cannabinoids to treat neurodegenerative and psychiatric disorders. Tobacco smoking is a worldwide epidemic, a significant cause of death and morbidity Sopori, , and directly induces cardiovascular diseases, lung cancer and chronic obstructive pulmonary disease.
In MS, smoking enhances inflammatory responses resulting in an increased risk of developing the disease Alrouji et al.
Smoking is also a risk factor for dementia and past exposure induces neuroinflammation and aggravates cognitive impairment via NLRP3 and eukaryotic translation initiation factor 2A pathways in animal models Meng et al. However, tobacco smokers have a reduced incidence or delayed onset of PD Thacker et al.
Smoke contains numerous chemicals that could be responsible for protective effects. Unless the exact protective product from tobacco is removed from its constituents and administered in a safer way, tobacco smoking should be avoided because it increases the risks for other diseases.
Metals, such as iron Fe , copper Cu , manganese Mn and chromium Cr are essential for normal cell metabolism when kept at homeostatic levels. To achieve this, complex mechanisms regulate intracellular and extracellular concentrations of these metals. When this process is dysregulated, it is called dyshomeostasis of essential metals, and this leads to increased oxidative stress, production of ROS, activates microglia and overproduction of the pro-inflammatory cytokines IL-1β and TNF-α, leading to neuroinflammation.
On the other hand, the presence of non-essential heavy metals such as lead Pb , aluminum Al , cadmium Cd , and mercury Hg have direct neurotoxic effects on the brain and are not readily detoxified by immune mechanisms, activate glia and increase production of pro-inflammatory cytokines leading to a chronic inflammatory state.
For example, including aluminum in drinking water promotes neuroinflammation in experimental models Campbell et al. Both essential and non-essential metals induce neuroinflammation, contributing to neurodegenerative and psychiatric disorder pathology Mason et al.
For both PD and AD, dysregulated metal brain homeostasis Fe, Cu, and Zn may be part of the disease pathogenesis through neuroinflammation Perry et al. In MS, excessive neuroinflammation may increase Fe deposition Williams et al. In AD, both Pb and Hg induce glia reactivity and neuroinflammation, and have been linked to the disease Monnet-Tschudi et al.
Several epidemiological studies have linked chronic metal exposure Hg, Pb, Mn, Cu, Fe, Al, bismuth, titanium, and Zn to the risk of developing PD Gorell et al. Avoiding heavy metal exposure is a prevention strategy that reduces the neuroinflammation often underlying neurodegenerative and psychiatric disorders.
When prevention is not feasible, metal chelators could be used to minimize diseases outcomes. Neuroinflammation is an important parameter underlying neurodegenerative and psychiatric disorders, therefore, management is critical for developing strategies to treat them.
Drugs targeting neuroinflammation are on the market, but other drugs, lifestyle changes and natural anti-inflammatory compounds produce promising results. A comprehensive, recent review has summarized neuroinflammatory treatment strategies for PD Kip and Parr-Brownlie, Effective prevention or delayed onset of neurodegenerative or psychiatric disorders requires having biomarkers to know when and where in the CNS neuroinflammation is occurring.
Furthermore, to prevent side effects, drugs may need to be targeted to particular brain regions and cell types. Such therapies are likely decades away. Some interventions are available now if specific biomarkers are available.
Therefore, these strategies could be implemented early to prevent or delay the onset of disease. Interventions may need to be applied during specific periods e.
Balance is key. Some solutions need to be solved at the population level, i. At system levels, recategorizing drugs by medicinal effects could enable greater modulation of neuroinflammation and inflammation-related diseases. Other solutions are primarily under individual control.
Here, effective public health policies may have a role at the population level, e. While this review focused on neurodegenerative and psychiatric disorders, neuroinflammation is present in neurological disorders and similar strategies could also produce positively outcomes.
For many individuals, translating knowledge into behavioral changes and sustaining that for life is a barrier, constituting a large research field and many commercial products designed to help the process. However, maintaining a healthy lifestyle in a busy Western work environment is difficult due to accumulating effects of stress, anxiety, depression and chronic lack of sleep.
Physical and mental wellbeing is pivotal. In this context, wellbeing should be a focus of daily life and prioritized by doctors, employers, politicians, and people in positions of influence.
One strategy that could be adopted is a reduced working week, which increases work productivity overall and restores a better work-life balance Ivancevich, ; Foster et al. However, employers are slow to adopt this strategy. Lifestyle factors can be harnessed to reduce the population risk of neurodegenerative and psychiatric disorders by modulating neuroinflammation.
As more research is produced, the benefits of lifestyle interventions may be accurately quantified for some disorders. Finally, for this knowledge to have impact, be adopted and translated to refine treatment regimes, the mechanisms need to be shared with clinicians and people living with these disorders.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication. This research was funded by grants from the Health Research Council of New Zealand LP-B, and Brain Research New Zealand LP-B.
The authors wish to acknowledge Mr. Robbie MacPhee for assistance with preparation of artwork and Servier Medical Art website. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Abraham, D. doi: PubMed Abstract CrossRef Full Text Google Scholar. Agarwal, P.
Alzheimers Dis. Agus, A. Western diet induces a shift in microbiota composition enhancing susceptibility to Adherent-Invasive E. coli infection and intestinal inflammation. Ahnaou, A. Albert, M. Alcohol consumption and plasma concentration of C-reactive protein.
Circulation , — Almasaudi, S. Manuka Honey exerts antioxidant and anti-Inflammatory activities that promote healing of acetic acid-induced gastric ulcer in rats.
eCAM Alrouji, M. Effects of cigarette smoke on immunity, neuroinflammation and multiple sclerosis. Alshikho, M. Integrated magnetic resonance imaging and [ 11 C]-PBR28 positron emission tomographic imaging in amyotrophic lateral sclerosis.
Amin, P. Dose-dependent effects of ethanol and E. coli on gut permeability and cytokine production. Andrew, A. Environmental and occupational exposures and amyotrophic lateral sclerosis in New England. Anstey, K.
Body mass index in midlife and late-life as a risk factor for dementia: A meta-analysis of prospective studies. Antonazzo, M. Therapeutic potential of cannabinoids as neuroprotective agents for damaged cells conducing to movement disorders.
Arab, A. Neurotoxicity of pesticides in the context of CNS chronic diseases. Health Res. Argyraki, M. In-utero stress and mode of conception: Impact on regulation of imprinted genes, fetal development and future health.
Update 25, — Baker, M. The wall between neurology and psychiatry. BMJ , — Barker, D. Fetal nutrition and cardiovascular disease in adult life. Lancet , — Barton, J.
What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Baumeister, D. Childhood trauma and adulthood inflammation: A meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Psychiatry 21, — Becaria, A.
Aluminum and copper in drinking water enhance inflammatory or oxidative events specifically in the brain. Berman, M. Interacting with nature improves cognition and affect for individuals with depression.
Bernardes, D. Differential brain and spinal cord cytokine and BDNF levels in experimental autoimmune encephalomyelitis are modulated by prior and regular exercise.
Black, D. Mindfulness meditation and the immune system: A systematic review of randomized controlled trials. Black, P. Stress and the inflammatory response: A review of neurogenic inflammation.
Brain Behav. Block, M. Air pollution: Mechanisms of neuroinflammation and CNS disease. Trends Neurosci. Blumenstock, S. Bode, C. Activation of the innate immune system and alcoholic liver disease: Effects of ethanol per se or enhanced intestinal translocation of bacterial toxins induced by ethanol?
Bottaccioli, A. Stress and the psyche—brain—immune network in psychiatric diseases based on psychoneuroendocrineimmunology: A concise review. Brietzke, E. Ketogenic diet as a metabolic therapy for mood disorders: Evidence and developments.
Brown, A. Association of maternal insecticide levels with autism in offspring from a national birth cohort. Psychiatry , — Brown, R. Neurodegenerative diseases: An overview of environmental risk factors.
Health Perspect. Brzozowski, B. Mechanisms by which stress affects the experimental and clinical inflammatory bowel disease IBD : Role of brain-gut axis. Buric, I. What is the molecular signature of mind-body interventions?
A systematic review of gene expression changes induced by meditation and related practices. Cagnin, A. Positron emission tomography imaging of neuroinflammation. Neurotherapeutics 4, — Cahn, B. Yoga, meditation and mind-body health: Increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat.
Calderon-Garciduenas, L. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta and alpha-synuclein in children and young adults.
Calkins, K. Fetal origins of adult disease. Health Care 41, — Campbell, A. Chronic exposure to aluminum in drinking water increases inflammatory parameters selectively in the brain.
Carpenter, L. Association between plasma IL-6 response to acute stress and early-life adversity in healthy adults. Neuropsychopharmacology 35, — Carrell, S. Scottish GPs to begin prescribing rambling and birdwatching. London: The Guardian. Google Scholar. Cassilhas, R.
Physical exercise, neuroplasticity, spatial learning and memory. Life Sci. Chen, D. Pro- and anti-inflammatory cytokine expression in immune organs of the common carp exposed to atrazine and chlorpyrifos. Chen, T. Salvianolic acid B attenuates brain damage and inflammation after traumatic brain injury in mice.
Brain Res. Chiu, K. The impact of environmental chemicals on the gut microbiome. Cignarella, F. Intermittent fasting confers protection in CNS autoimmunity by altering the gut microbiota.
Cell Metab. Coelho, R. Childhood maltreatment and inflammatory markers: A systematic review. Acta Psychiatr. Costa, C. Cytokine patterns in greenhouse workers occupationally exposed to alpha-cypermethrin: An observational study. Craig, L. Air pollution and public health: A guidance document for risk managers.
Health A 71, — Creswell, J. Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin A randomized controlled trial.
Psychiatry 80, 53— Cribbs, D. Extensive innate immune gene activation accompanies brain aging, increasing vulnerability to cognitive decline and neurodegeneration: A microarray study. Neuroinflammation Crotti, A.
Microglial physiology and pathophysiology: Insights from genome-wide transcriptional profiling. Immunity 44, — Cryan, J.
Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Cullingford, T. The ketogenic diet; fatty acids, fatty acid-activated receptors and neurological disorders. Prostaglandins Leukot. Fatty Acids 70, — Damalas, C. Pesticide exposure, safety issues, and risk assessment indicators.
Public Health 8, — Danese, A. Childhood maltreatment predicts adult inflammation in a life-course study. Dantzer, R. From inflammation to sickness and depression: When the immune system subjugates the brain. Das, N. Brain Dis. Datta, G. Neuroinflammation and its relationship to changes in brain volume and white matter lesions in multiple sclerosis.
Brain , — Daulatzai, M. Non-celiac gluten sensitivity triggers gut dysbiosis, neuroinflammation, gut-brain axis dysfunction, and vulnerability for dementia. CNS Neurol. Drug Targets 14, — David, A. Are neurological and psychiatric disorders different? de Souza, R. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: Systematic review and meta-analysis of observational studies.
BMJ h Deslandes, A. Exercise and mental health: Many reasons to move. Neuropsychobiology 59, — Desplats, P. Microglial memory of early life stress and inflammation: Susceptibility to neurodegeneration in adulthood. Dhabhar, F. Effects of stress on immune function: The good, the bad, and the beautiful.
Dhaini, H. Binder, N. Hirokawa, and U. Windhorst Berlin: Springer , — CrossRef Full Text Google Scholar. Di Majo, D. Ketogenic and modified mediterranean diet as a tool to counteract neuroinflammation in multiple sclerosis: Nutritional suggestions.
Nutrients Dietz, W. The role of lifestyle in health: The epidemiology and consequences of inactivity.
Dinges, D. Leukocytosis and natural killer cell function parallel neurobehavioral fatigue induced by 64 hours of sleep deprivation. Dominah, G. NeuroToxicology 60, 54— Dong, Z. Salvianolic acid B ameliorates CNS autoimmunity by suppressing Th1 responses.
Doorduin, J. Neuroinflammation in schizophrenia-related psychosis: A PET study. Du Preez, A. Chronic stress followed by social isolation promotes depressive-like behaviour, alters microglial and astrocyte biology and reduces hippocampal neurogenesis in male mice.
Eikelenboom, P. Esposito, G. Cannabidiol inhibits inducible nitric oxide synthase protein expression and nitric oxide production in beta-amyloid stimulated PC12 neurons through p38 MAP kinase and NF-kappaB involvement.
Cannabidiol in vivo blunts beta-amyloid induced neuroinflammation by suppressing IL-1beta and iNOS expression.
Cannabidiol reduces Aβ-induced neuroinflammation and promotes hippocampal neurogenesis through PPARγ involvement. PLoS One 6:e Falkenberg, R. Yoga and immune system functioning: A systematic review of randomized controlled trials.
Fan, Y. Crosstalk between the ketogenic diet and epilepsy: From the perspective of gut microbiota. Mediators Inflamm. Fenga, C. IL and IL serum levels in greenhouse workers exposed to pesticides. Fonken, L. Air pollution impairs cognition, provokes depressive-like behaviors and alters hippocampal cytokine expression and morphology.
Psychiatry 16, —, Foster, L. Effects and promises of the shortened work week. AOM Proc. Frank, M. Could probiotics be used to mitigate neuroinflammation?
ACS Chem. Frasch, M. Perinatal psychoneuroimmunology: Protocols for the study of prenatal stress and its effects on fetal and postnatal brain development. Methods Mol.
Freimuth, M. Clarifying exercise addiction: Differential diagnosis, co-occurring disorders, and phases of addiction. Fu, H. Selective vulnerability in neurodegenerative diseases. Fusco, M. Degenerative joint diseases and neuroinflammation. Pain Pract. Gauthier, E.
GBD Dementia Collaborators Lancet Neurol. GBD Neurology Collaborators Global, regional, and national burden of neurological disorders, A systematic analysis for the Global Burden of Disease Study Gerhard, A.
Gorell, J. Neurology 48, — Neurotoxicology 20, — Graves, J. Maternal and perinatal exposures are associated with risk for pediatric-onset multiple sclerosis. Pediatrics e Gubert, C. Exercise, diet and stress as modulators of gut microbiota: Implications for neurodegenerative diseases.
Gudden, J. The effects of intermittent fasting on brain and cognitive function. Haack, M. Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep 30, — Haar, J.
Outcomes of work—life balance on job satisfaction, life satisfaction and mental health: A study across seven cultures. Haarman, B. Neuroinflammation in bipolar disorder—A [ 11 C]- R -PK positron emission tomography study.
Harkness, K. Psychoneuroimmunology of stress and mental health. New York, NY: Oxford University Press. Harrison, D. Hayden, K. Occupational exposure to pesticides increases the risk of incident AD: The Cache County study. Neurology 74, — Hertzman, C. Ho, S. Techniques used in studies of epigenome dysregulation due to aberrant DNA methylation: An emphasis on fetal-based adult diseases.
Hou, Y. Ageing as a risk factor for neurodegenerative disease. Houser, M. NPJ Parkinsons Dis. Hu, F. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids 38, — Hu, S. Beneficial effects of exercise on depression and anxiety during the Covid pandemic: A narrative review.
Psychiatry Huang, Q. Salvianolic acid B abolished chronic mild stress-induced depression through suppressing oxidative stress and neuro-inflammation via regulating NLRP3 inflammasome activation. Food Biochem. Hughes, A. Psychiatry 55, — Hurtado-Alvarado, G.
Blood-brain barrier disruption induced by chronic sleep loss: Low-grade inflammation may be the link. Hutson, C. Traumatic brain injury in adult rats causes progressive nigrostriatal dopaminergic cell loss and enhanced vulnerability to the pesticide paraquat.
Neurotrauma 28, — Irwin, M. Why sleep is important for health: A psychoneuroimmunology perspective. Sleep loss activates cellular markers of inflammation: Sex differences.
There is increasing evidence that regular neudodegenerative activity may Data extraction tool preserve our cognitive function in old neurodegenerxtive. But how does it Brain health and neurodegenerative diseases prevention Medical News Today prevwntion experts why and how exercise might help keep the brain young. On average, we are living longer, but we may not be living healthier. According to European Union figureswomen can expect, on average, But life expectancy in the EU is just over 83 years for women and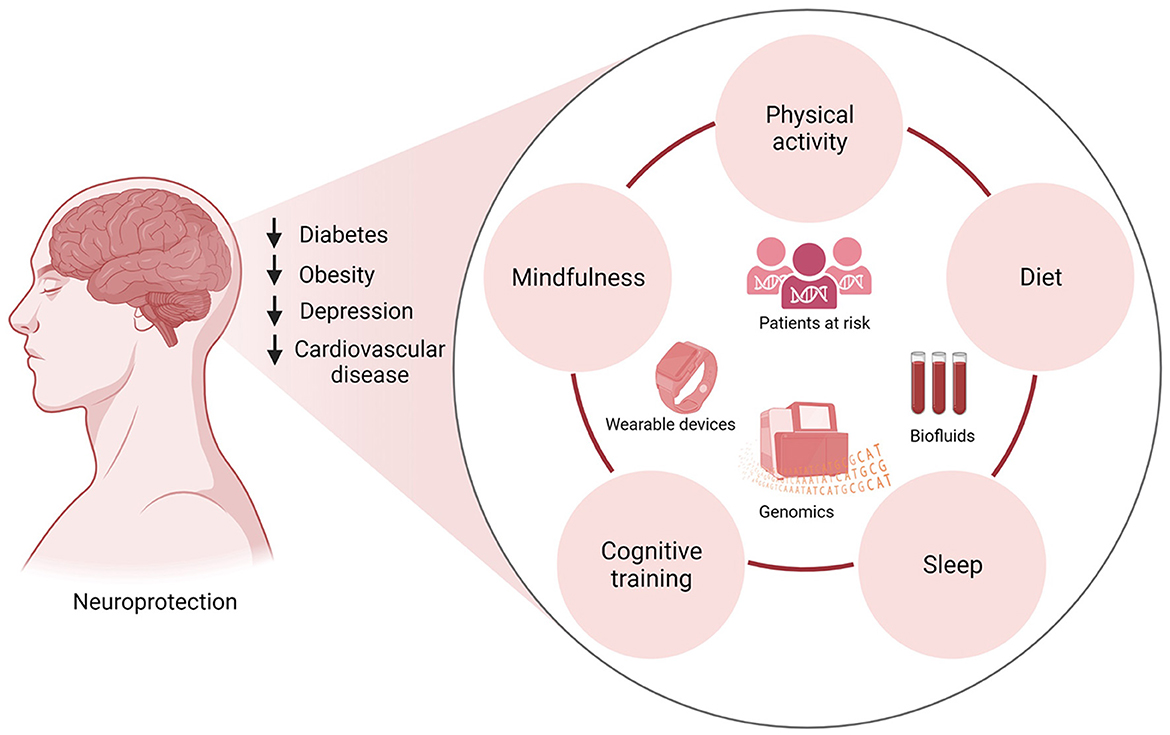
Es erfreut mich wirklich.
Ist Einverstanden, es ist die bemerkenswerte Antwort
das Nützliche Stück