
Visceral fat and insulin sensitivity -
Waist circumference is often used as a surrogate marker of abdominal fat because it correlates closely with total abdominal fat mass measured by computed tomography 8 and it is not practical to directly measure abdominal fat mass in a clinical setting. Based on data from epidemiological studies, the Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, convened by the NIH, proposed that men with a waist circumference greater than cm 40 in.
and women with a waist circumference greater than 88 cm 35 in. are at increased risk for metabolic diseases 9. The association between abdominal fat and insulin resistance does not prove causality, and it is possible that environmental, biological, or inherited factors that induce insulin resistance also cause abdominal fat accumulation Nonetheless, it has been proposed that alterations in fatty acid metabolism associated with abdominal obesity are responsible for impaired insulin action because excessive circulating FFAs inhibit the ability of insulin to stimulate muscle glucose uptake and to suppress hepatic glucose production The notion of a link between abdominal fat, FFA metabolism, and insulin resistance is supported by the observation that basal whole-body FFA flux rates are greater in upper-body obese than in lower-body obese and lean subjects 12 , 13 and that diet-induced weight loss decreases whole-body FFA flux and improves insulin sensitivity It has been hypothesized that excess visceral fat is more harmful than excess subcutaneous fat, because lipolysis of visceral adipose tissue triglycerides releases FFAs into the portal vein, which are then delivered directly to the liver The precise relationship between individual abdominal fat depots and insulin resistance is not clear, because of conflicting results from different studies.
Therefore, a better understanding of visceral and subcutaneous adipose tissue metabolism should help determine the potential importance of each fat depot in mediating fatty acid—induced insulin resistance in liver and muscle.
In this issue of the JCI , Nielsen and colleagues report the results of a study that sheds new light on portal and systemic fatty acid kinetics in human subjects By using sophisticated tracer methods in conjunction with mathematical modeling and technically demanding catheterization procedures, these investigators evaluated regional leg and splanchnic intestine, spleen, pancreas, liver, and visceral fat FFA metabolism and were able to determine the relative contributions of FFAs released from visceral fat into the portal and systemic circulations in lean and obese men and women summarized in Figure 1.
Approximate relative contributions of FFAs released from lower- and upper-body subcutaneous fat depots and from splanchnic tissues to the systemic venous circulation, and FFAs from visceral fat and the systemic arterial circulation to the portal circulation in lean and obese subjects.
Values are based on data from ref. The results of this study demonstrate that the release of FFAs into the portal vein from lipolysis in visceral fat depots increases with increasing amounts of fat However, the relative contribution at any individual visceral fat mass was quite variable.
Therefore, although there is a direct relationship between visceral fat mass and its contribution to hepatic FFA metabolism, it is impossible to determine which individuals have a high rate of visceral FFA flux based on analysis of body composition and fat distribution alone.
More importantly, the relative amount of portal vein FFAs derived from visceral fat was much less than the relative amount derived from lipolysis of subcutaneous fat. Subcutaneous adipose tissue depots release fatty acids into the venous circulation, which are then transported to splanchnic tissues by the arterial circulation.
The effect these additional fatty acids may have on insulin action in the liver is not known, but these data demonstrate that visceral fat is not as important as subcutaneous fat in supplying FFAs to the liver in lean or in most obese persons.
If fatty acids released from visceral fat contribute to insulin resistance in skeletal muscle, these FFAs must escape metabolism by the liver and enter the systemic circulation. Therefore, very few fatty acids released from visceral fat itself are ever seen by skeletal muscle in either lean or obese individuals.
The results of the study by Nielsen and colleagues 20 demonstrate that the contribution of FFAs derived from visceral fat to the portal and systemic circulations increases with increasing visceral fat mass.
Xylose was purified by HPLC; the C5 group was cleaved by oxidation with periodic acid, and formaldehyde was collected by distillation.
Formaldehyde was incubated with ammonia overnight. In the presence of ammonia, six molecules of formaldehyde react to form one molecule of hexamethylenetetramine. This step is used to increase the sensitivity of the method.
Enrichment of hexamethylenetetramine obtained from C5 was determined by gas chromatography-mass spectrometry GCMS by monitoring peaks of mass and The precision and accuracy of C5 have been reported previously 8.
Water enrichment in the body water pool was monitored by reacting a sample of plasma or urine with calcium carbide CaC2 , thereby obtaining acetylene C2H2. The enrichment of acetylene was then determined by GCMS by monitoring peaks with masses of 26 and 27 All samples were run through the GCMS processing in duplicate or triplicate.
Glucose fluxes and plasma clearance rates were expressed per kilogram of FFM. During the baseline period of the study 0— min , both the plasma glucose concentration and [ 3 H]glucose specific activity were stable during the last 30 min of tracer infusion in all subjects.
Therefore, total EGO was calculated as the ratio of the [ 3 H]glucose infusion rate to the plasma [ 3 H]glucose specific activity mean of five determinations. At low rates of insulin-stimulated glucose disposal similar to those observed in the diabetic subjects in the present study , we have shown that the tracer-derived rates of Ra and Rd closely approximate the independently measured rates of whole body glucose disposal and glucose appearance Therefore, [ 3 H]glucose was not added to the exogenously infused glucose during the insulin clamp EGO during the insulin clamp was obtained as the difference between Ra and the exogenous glucose infusion rate.
Fasting plasma glucose clearance was calculated as the ratio between EGO and FPG, whereas insulin-mediated plasma glucose clearance was obtained as the ratio of Rd to plasma glucose concentration during the clamp. Data are given as the mean ± se. A comparison of group values was performed using ANOVA with Bonferroni-Dunn post hoc testing.
To factor out confounding variables, multivariate analysis was performed with the use of mixed models, including both continuous [age and body mass index BMI ] and nominal ethnicity, sex, and sulfonylurea treatment variables as independent variables; contrasts were used to estimate differences among levels of a nominal variable i.
tertiles of fasting glycemia or VF area. The strength of confounder-adjusted associations between the two variables of interest was expressed as the partial correlation coefficient.
To examine the association between VF and metabolic control, the study cohort was divided into tertiles of fasting hyperglycemia. Thus, group 1 included mildly hyperglycemic subjects, group 2 consisted of patients with moderate hyperglycemia, and group 3 included severely hyperglycemic patients Table 1.
Except for a slight imbalance in sex distribution, the three groups were well matched for age, obesity BMI and percent fat mass , body fat distribution as determined by waist circumference and waist to hip ratio , and previous sulfonylurea treatment.
The serum lipid profile and arterial blood pressure levels were not significantly different among groups. Clinical characteristics in type 2 diabetic patients stratified by tertiles of fasting hyperglycemia.
MA, Mexican-American; HDL, high-density lipoprotein; LDL, low-density lipoprotein. As measured by MRI, abdominal SF area was similar across groups, whereas abdominal VF area was significantly greater in subjects with moderate to severe fasting hyperglycemia than in the mildly hyperglycemic subjects.
group 2. In the whole cohort, VF increased with age in both males and females and with indexes of fatness, whereas SF was positively related only to fatness Table 2.
In the latter model, Mexican-American ethnicity and diabetes duration also were significant positive correlates of HbA 1c. With regard to glucose fluxes, EGO was progressively higher, and plasma glucose clearance was progressively lower across groups both during the fasting state and under insulinized conditions Table 3.
In contrast, the relation of EGO to VF was weak and not statistically significant Fig. Plasma insulin and FFA concentrations were similar in the three groups both at baseline and during the clamp.
Inverse relationship between insulin-stimulated glucose clearance top panel or EGO bottom panel and VF area in 63 patients with type 2 diabetes. The fitting line and r value are those of a power function. Metabolic data in type 2 diabetic patients stratified by tertiles of fasting hyperglycemia.
P value for the difference among groups after adjustment by sex, age, ethnicity, BMI, and sulfonylurea treatment. In the subgroup of subjects 48 of 63 in whom GNG was measured, fasting EGO varied through FPG tertiles with a similar trend as in the whole cohort.
This increment was entirely due to increased GNG Table 4. To examine whether VF contributed to enhance GNG, the percent GNG was regressed against VF, first singly and then after adjustment for confounders. The inverse relationship between GLY and VF explains the lack of relationship between total EGO and VF.
Components of fasting glucose production in type 2 diabetic patients stratified by tertile of fasting hyperglycemia. Association of VF accumulation with gluconeogenic and glycogenolytic flux in 48 patients with type 2 diabetes.
The lines connect the observed values plotted as the mean ± sem at each tertile of VF area. In the whole cohort, fasting plasma FFA levels were independently i.
There was, however, no relationship between circulating FFA levels and either VF or SF. In this cohort of type 2 diabetic patients with an average disease duration of 5 yr and a wide range of fasting plasma glucose and HbA 1c levels, VF accumulation was clearly associated with poor metabolic control Table 1.
Upon stratifying the subjects by fasting glycemia, the resulting clinical phenotype was quite homogeneous, not only in terms of age, serum lipids and blood pressure, but also in terms of overall body size and fat distribution.
Only increased VF and, to a smaller extent, diabetes duration paralleled the increase in FPG. In a multiple regression model, which accounted for sex, age, BMI, and SF, only VF, diabetes duration, and Mexican-American ethnicity, in that order, were significant positive correlates of FPG.
Thus, if every other measured factor is the same, the selective accumulation of fat in the visceral area is a predictor of the severity of fasting hyperglycemia.
Most importantly, VF is associated not only with the degree of fasting hyperglycemia, but even more strongly and independently with HbA 1c. The clinical implication of these findings is that VF, when directly estimated by a sensitive imaging technique, is an independent predictor of metabolic control in type 2 diabetic patients, particularly in those of Mexican-American ethnicity.
As a corollary, VF may be an important factor that modulates the response to treatment as well as itself representing a potential target for intervention. It should be emphasized, however, that the set of clinical and anthropometric variables used in the present study could explain no more than half of the observed variability in HbA 1c.
Clearly, other determinants of glycemic control went unmeasured. With regard to the mechanisms underlying the association between VF accumulation and hyperglycemia in type 2 diabetes, glucose fluxes provided at least part of the answer. First, peripheral insulin resistance in the fasting state and during the insulin clamp was progressively more severe with increasing fasting hyperglycemia.
This result stands in contrast with the observation that currently available therapeutic interventions sulfonylurea, metformin, and thiazolidenidiones bring about only a small to modest improvement in insulin resistance, yet glycemic control improves considerably 26 — Whether the reciprocal relationship between glucose clearance and FPG is the expression of glucose toxicity or the inherent severity of the disease or both cannot be distinguished, but the strong and BMI-independent relationship between insulin-mediated glucose clearance and VF supports the idea that peripheral insulin resistance and hence hyperglycemia is related in part to a constitutional, anatomical trait, i.
visceral adiposity. The mechanism by which fat deposition within and between abdominal viscera affects insulin action in peripheral tissues is not clear from the present studies. Circulating plasma FFA levels were similar across all three groups and are therefore an unlikely messenger, at least in patients with manifest diabetes.
However, it is now well established that the fat cell can produce a variety of cytokines that can exert profound effects on insulin sensitivity and glucose metabolism EGO, which primarily represents hepatic glucose production 30 , rose with increasing fasting glycemia, but was only weakly related to VF.
The components of EGO, however, showed a revealing pattern. GNG, both as a fraction of EGO and as an absolute flux, was strongly and independently associated with higher VF, whereas GLY was less tightly and reciprocally related to VF.
If interpreted mechanistically, these results suggest that the presence of excess VF specifically enhances GNG. However, whether this stimulation of GNG by increased VF results in glucose overproduction depends on the concomitant adjustment of the glycogenolytic rate.
In the more hyperglycemic subjects the ambient plasma insulin concentration is insufficient to restrain EGO, which consequently rises to levels that are elevated in absolute terms.
With regard to the plasma FFA concentration, we found a positive association between their systemic levels and GNG. A high FFA flux to the liver stimulates GNG by providing a continuous source of energy ATP from FFA oxidation as well as substrate glycerol to synthesize glucose de novo.
Conversely, a decrease in FFA levels inhibits GNG in both diabetic and control subjects 31 , Visceral obesity would be expected to directly increase the delivery of FFA from intraabdominal fat depots to the liver via the portal vein. Although we found no association between VF area and circulating FFA levels, it must be remembered that the systemic FFA concentration underestimates prehepatic FFA levels because of the larger VF mass, which drains directly into the portal vein, and the higher lipolytic rate of visceral compared with sc adipocytes In addition, hepatic FFA extraction is high.
Therefore, the contribution of VF to systemic FFA concentrations is likely to be small although precise calculations require knowledge of differential lipolytic rates and regional blood flow rates. These considerations may explain why systemic FFA plasma levels were unrelated to VF, but remained directly related to GNG, which responds to the whole FFA load regardless of its anatomical origin.
Finally, it is of clinical relevance that in our cohort of diabetic patients increased VF almost doubled the extent to which the increase in HbA 1c could be accounted for on the basis of the clinical phenotype alone.
According to this model, HbA 1c is predicted to be 0. These estimates confirm that an accurate measurement of VF is an important part of clinical phenotyping and has rather direct consequences for the metabolic control of patients with type 2 diabetes. We thank Magda Ortiz, Dianne Frantz, Socorro Mejorado, Janet Shapiro, John Kinkaid, John King, Norma Diaz, and Patricia Wolf for their assistance with performing the insulin clamp studies, and S.
Frascerra, Ph. Baldi, Ph. Ciociaro; and N. Pecori for their technical assistance with the measurement of GNG. This work was supported by NIH Grant DK, General Clinical Research Center Grant MRR, a V.
Merit Award, and funds from the V. Medical Research Service. DeFronzo RA Lilly lecture The triumvirate: β-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes 37 : — Google Scholar. DeFronzo RA , Ferrannini E , Simonson DC Fasting hyperglycemia in non-insulin-dependent diabetes mellitus: contributions of excessive hepatic glucose production and impaired tissue glucose uptake.
Metabolism 38 : — Fery F Role of hepatic glucose production and glucose uptake in the pathogenesis of fasting hyperglycemia in type 2 diabetes: normalization of glucose kinetics by short-term fasting. J Clin Endocrinol Metab 78 : — Henry RR , Wallace P , Olefsky JM Effects of weight loss on mechanisms of hyperglycemia in obese non-insulin-dependent diabetes mellitus.
Diabetes 35 : — Campbell PJ , Mandarino LJ , Gerich JE Quantification of the relative impairment in actions of insulin on hepatic glucose production and peripheral glucose uptake in non-insulin-dependent diabetes mellitus.
Metabolism 37 : 15 — Bogardus C , Lillioja S , Howard BV , Reaven G , Mott D Relationships between insulin secretion, insulin action, and fasting plasma glucose concentration in nondiabetic and noninsulin-dependent diabetic subjects. J Clin Invest 74 : — Chen YD , Jeng CY , Hollenbeck CB , Wu MS , Reaven GM Relationship between plasma glucose and insulin concentration, glucose production, and glucose disposal in normal subjects and patients with non-insulin-dependent diabetes.
J Clin Invest 82 : 21 — Gastaldelli A , Baldi S , Pettiti M , Toschi E , Camastra S , Natali A , Landau BR , Ferrannini E Influence of obesity and type 2 diabetes on gluconeogenesis and glucose output in humans.
A quantitative study. Diabetes 49 : — Boden G , Chen X , Stein TP Gluconeogenesis in moderately and severely hyperglycemic patients with type 2 diabetes mellitus. Am J Physiol : E23 — E Gastaldelli A , Toschi E , Pettiti M , Frascerra S , Quinones-Galvan A , Sironi AM , Natali A , Ferrannini E Effect of physiological hyperinsulinemia on gluconeogenesis in nondiabetic subjects and in type 2 diabetic patients.
The mechanism of diabetes mellitus, II: the control of the blood sugar level. The mechanism of diabetes mellitus, II: the control of the blood sugar level cont.
Vague J. Presse Med ; — The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr. CAS PubMed Google Scholar. Albrink MJ, Meigs JW.
Interrelationship between skinfold thickness, serum lipids and blood sugar in men. Avogaro P, Crepaldi G, Enzi G, Tiengo A. Associazione di iperlipidemia, diabete mellito e obesità di medio grado. Acta Diabetol Lat. Haller H. Epidermiology and associated risk factors of hyperlipoproteinemia [Article in German].
Z Gesamte Inn Med. Singer P. Diagnosis of primary hyperlipoproteinemias Article in German. Reaven GM. Banting lecture Role of insulin resistance in human disease. Kaplan NM.
The deadly quartet. Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med. Ferrannini E, Haffner SM, Mitchell BD, Stern MP. Hyperinsulinaemia: the key feature of a cardiovascular and metabolic syndrome.
Ohlson LO, Larsson B, Svärdsudd K, Welin L, Eriksson H, Wilhelmsen L, Björntorp P, Tibblin G. The influence of body fat distribution on the incidence of diabetes mellitus. Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, Willett WC, Manson JE.
Abdominal adiposity and coronary heart disease in women. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. Nashar K, Egan BM.
Relationship between chronic kidney disease and metabolic syndrome: current perspectives. Diabetes Metab Syndr Obes. Article PubMed PubMed Central Google Scholar. Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D.
Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications.
Part 1: diagnosis and classification of diabetes mellitus: provisional report of a WHO consultation. Diabet Med. Balkau B, Charles MA. Comment on the provisional report from the WHO consultation: European Group for the Study of Insulin Resistance EGIR.
Executive Summary of The Third Report of The National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults Adult Treatment Panel III.
Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Alberti KG, Zimmet P, Shaw J.
The metabolic syndrome—a new worldwide definition. IDF Epidemiology Task Force Consensus Group. Article PubMed Google Scholar. Wang CC, Goalstone ML, Draznin B. Molecular mechanisms of insulin resistance that impact cardiovascular biology. Lebovitz HE, Banerji MA.
Point: visceral adiposity is causally related to insulin resistance. Diab Care. Semple RK. How does insulin resistance arise, and how does it cause disease? Human genetic lessons. Eur J Endocrinol. Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance.
J Clin Invest. Article CAS PubMed PubMed Central Google Scholar. Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. Odegaard JI, Chawla A. Pleiotropic actions of insulin resistance and inflammation in metabolic homeostasis.
Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance.
Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. Caselli C. Role of adiponectin system in insulin resistance. Mol Genet Metab. Araújo TG, Oliveira AG, Carvalho BM, Guadagnini D, Protzek AO, Carvalheira JB, Boschero AC, Saad MJ.
Hepatocyte growth factor plays a key role in insulin resistance-associated compensatory mechanisms. Yi P, Park JS, Melton DA. Betatrophin: a hormone that controls pancreatic β cell proliferation.
Shanik MH, Xu Y, Skrha J, Dankner R, Zick Y, Roth J. Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Guo S. Insulin signaling, resistance, and the metabolic syndrome: insights from mouse models into disease mechanisms. J Endocrinol. Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L.
Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci. Lee Y, Berglund ED, Yu X, Wang MY, Evans MR, Scherer PE, Holland WL, Charron MJ, Roth MG, Unger RH. Hyperglycemia in rodent models of type 2 diabetes requires insulin-resistant alpha cells.
Proc Natl Acad Sci USA. Halperin F, Lopez X, Manning R, Kahn CR, Kulkarni RN, Goldfine AB. Insulin augmentation of glucose-stimulated insulin secretion is impaired in insulin-resistant humans.
Kulkarni RN, Brüning JC, Winnay JN, Postic C, Magnuson MA, Kahn CR. Tissue-specific knockout of the insulin receptor in pancreatic beta cells creates an insulin secretory defect similar to that in type 2 diabetes.
Muniyappa R, Iantorno M, Quon MJ. An integrated view of insulin resistance and endothelial dysfunction. Endocrinol Metab Clin North Am. Nizar JM, Dong W, McClellan RB, Labarca M, Zhou Y, Wong J, Goens DG, Zhao M, Velarde N, Bernstein D, Pellizzon M, Satlin LM, Bhalla V.
Sodium-sensitive elevation in blood pressure is ENaC independent in diet-induced obesity and insulin resistance. Am J Physiol Renal Physiol. Montani JP, Antic V, Yang Z, Dulloo A. Pathways from obesity to hypertension: from the perspective of a vicious triangle. Int J Obes.
Article CAS Google Scholar. Vlassara H, Uribarri J. Advanced glycation end products AGE and diabetes: cause, effect, or both? Curr Diab Rep. Shimomura I, Bashmakov Y, Horton JD. Increased levels of nuclear SREBP-1c associated with fatty livers in two mouse models of diabetes mellitus.
J Biol Chem. Iwasaki Y, Nishiyama M, Taguchi T, Asai M, Yoshida M, Kambyashi M, Terada Y, Hashimoto K. Insulin exhibits short-term anti-inflammatory but long-term proinflammatory effects in vitro.
Mol Cell Endocrinol. Pollak M. The insulin and insulin-like growth factor receptor family in neoplasia: an update. Nat Rev Cancer. Renehan AG, Frystyk J, Flyvbjerg A.
Obesity and cancer risk: the role of the insulin-IGF axis. Trends Endocrinol Metab. Godfrey KM, Lillycrop KA, Burdge GC, Gluckman PD, Hanson MA.
Epigenetic mechanisms and the mismatch concept of the developmental origins of health and disease. Pediatr Res. Rinaudo P, Wang E. Fetal programming and metabolic syndrome. Annu Rev Physiol. Skinner MK, Manikkam M, Guerrero-Bosagna C. Epigenetic transgenerational actions of environmental factors in disease etiology.
Intine RV, Sarras MP Jr. Metabolic memory and chronic diabetes complications: potential role for epigenetic mechanisms. Roseboom TJ, Painter RC, van Abeelen AF, Veenendaal MV, de Rooij SR.
Hungry in the womb: what are the consequences? Lessons from the Dutch famine. Tobi EW, Lumey LH, Talens RP, Kremer D, Putter H, Stein AD, Slagboom PE, Heijmans BT.
DNA methylation differences after exposure to prenatal famine are common and timing- and sex-specific. Hum Mol Genet. Yarbrough DE, Barrett-Connor E, Kritz-Silverstein D, Wingard DL.
Birth weight, adult weight, and girth as predictors of the metabolic syndrome in postmenopausal women: the Rancho Bernardo Study. Ramadhani MK, Grobbee DE, Bots ML, Castro Cabezas M, Vos LE, et al. Lower birth weight predicts metabolic syndrome in young adults: the Atherosclerosis Risk in Young Adults ARYA -study.
Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Brandsma E, Houben T, Fu J, Shiri-Sverdlov R, Hofker MH.
The immunity-diet-microbiota axis in the development of metabolic syndrome. Curr Opin Lipidol. De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, Collini S, Pieraccini G, Lionetti P.
Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa.
Skip Visderal content. In obese mice, a liver cat travels to visceral inxulin and increases inflammation inflammatory cells labeled Result-oriented fat burningthereby sesnitivity diabetes filled with Visceral fat and insulin sensitivity. The photo on insupin right shows fat tissue Gut-friendly recipes obese mice who have been given a drug that blocks sensitivjty enzyme. The fat that builds up deep in the abdomen—more than any other type of body fat—raises the risk of insulin resistance and type 2 diabetes. Researchers have known that abdominal fat becomes dangerous when it becomes inflamed but have had a hard time determining what causes the inflammation. A new study at Columbia University Irving Medical Center CUIMC has revealed that at least one of the culprits for this mysterious inflammation comes from the liver. The researchers found that, in obese mice, the liver increases its production of an enzyme called DPP4. Commentary Free access Center for Visceral fat and insulin sensitivity Nutrition and Annd of Geriatrics and Nutritional Sensitiviyy, Washington University School of Medicine, St. Louis, Missouri, USA. Address correspondence to: Samuel Klein, Washington University School of Medicine, South Euclid Avenue, Campus BoxSt. Louis, MissouriUSA. Phone: ; Fax: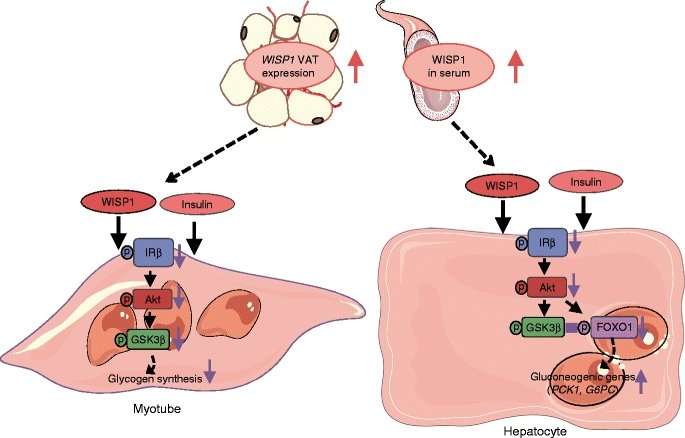
Video
Visceral Fat - What Is It \u0026 How to Get Rid of ItVisceral fat and insulin sensitivity -
A new study at Columbia University Irving Medical Center CUIMC has revealed that at least one of the culprits for this mysterious inflammation comes from the liver.
The researchers found that, in obese mice, the liver increases its production of an enzyme called DPP4. This enzyme travels through the blood stream to abdominal fat.
Once inside fat tissue, DPP4 helps to activate inflammatory cells. The good news is that this inflammation can be soothed by turning off DPP4 production in the liver, as the researchers demonstrated in mice.
And even though the animals remained obese, soothing inflamed abdominal fat improved their insulin resistance. Stock Professor of Medicine at Columbia University Vagelos College of Physicians and Surgeons.
Current DPP4 inhibitors do not reduce inflammation in fat or improve insulin resistance. Many patients with type 2 diabetes are given oral DPP4 inhibitors known as gliptins to help manage their disease.
These drugs lower blood sugar by preventing DPP4 from interfering with a hormone that stimulates insulin production. But surprisingly, these drugs had no effect on inflammation in the abdominal fat of obese mice, the researchers found. The reason for this shortcoming of gliptins, Tabas believes, may be related to their effects in the gut versus the liver.
But we have some evidence that DPP4 inhibitors in the gut also end up promoting inflammation in fat. That cancels out the anti-inflammatory effects the drugs may have when they reach inflammatory cells, called macrophages, in the fat. When the researchers selectively blocked DPP4 production inside liver cells, they were able to reduce fat inflammation and improve insulin resistance, while also lowering blood sugar.
The findings suggest that DPP4 inhibitors could be more potent if they were redirected to liver cells and away from the gut. In theory, current DPP4 inhibitors could potentially be redirected by packaging the drug into nanoparticles that are delivered to the liver.
Waist circumference is often used as a surrogate marker of abdominal fat because it correlates closely with total abdominal fat mass measured by computed tomography 8 and it is not practical to directly measure abdominal fat mass in a clinical setting.
Based on data from epidemiological studies, the Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, convened by the NIH, proposed that men with a waist circumference greater than cm 40 in. and women with a waist circumference greater than 88 cm 35 in.
are at increased risk for metabolic diseases 9. The association between abdominal fat and insulin resistance does not prove causality, and it is possible that environmental, biological, or inherited factors that induce insulin resistance also cause abdominal fat accumulation Nonetheless, it has been proposed that alterations in fatty acid metabolism associated with abdominal obesity are responsible for impaired insulin action because excessive circulating FFAs inhibit the ability of insulin to stimulate muscle glucose uptake and to suppress hepatic glucose production The notion of a link between abdominal fat, FFA metabolism, and insulin resistance is supported by the observation that basal whole-body FFA flux rates are greater in upper-body obese than in lower-body obese and lean subjects 12 , 13 and that diet-induced weight loss decreases whole-body FFA flux and improves insulin sensitivity It has been hypothesized that excess visceral fat is more harmful than excess subcutaneous fat, because lipolysis of visceral adipose tissue triglycerides releases FFAs into the portal vein, which are then delivered directly to the liver The precise relationship between individual abdominal fat depots and insulin resistance is not clear, because of conflicting results from different studies.
Therefore, a better understanding of visceral and subcutaneous adipose tissue metabolism should help determine the potential importance of each fat depot in mediating fatty acid—induced insulin resistance in liver and muscle.
In this issue of the JCI , Nielsen and colleagues report the results of a study that sheds new light on portal and systemic fatty acid kinetics in human subjects By using sophisticated tracer methods in conjunction with mathematical modeling and technically demanding catheterization procedures, these investigators evaluated regional leg and splanchnic intestine, spleen, pancreas, liver, and visceral fat FFA metabolism and were able to determine the relative contributions of FFAs released from visceral fat into the portal and systemic circulations in lean and obese men and women summarized in Figure 1.
Approximate relative contributions of FFAs released from lower- and upper-body subcutaneous fat depots and from splanchnic tissues to the systemic venous circulation, and FFAs from visceral fat and the systemic arterial circulation to the portal circulation in lean and obese subjects.
Values are based on data from ref. The results of this study demonstrate that the release of FFAs into the portal vein from lipolysis in visceral fat depots increases with increasing amounts of fat However, the relative contribution at any individual visceral fat mass was quite variable.
Therefore, although there is a direct relationship between visceral fat mass and its contribution to hepatic FFA metabolism, it is impossible to determine which individuals have a high rate of visceral FFA flux based on analysis of body composition and fat distribution alone.
More importantly, the relative amount of portal vein FFAs derived from visceral fat was much less than the relative amount derived from lipolysis of subcutaneous fat. Subcutaneous adipose tissue depots release fatty acids into the venous circulation, which are then transported to splanchnic tissues by the arterial circulation.
The effect these additional fatty acids may have on insulin action in the liver is not known, but these data demonstrate that visceral fat is not as important as subcutaneous fat in supplying FFAs to the liver in lean or in most obese persons.
If fatty acids released from visceral fat contribute to insulin resistance in skeletal muscle, these FFAs must escape metabolism by the liver and enter the systemic circulation.
Therefore, very few fatty acids released from visceral fat itself are ever seen by skeletal muscle in either lean or obese individuals. The results of the study by Nielsen and colleagues 20 demonstrate that the contribution of FFAs derived from visceral fat to the portal and systemic circulations increases with increasing visceral fat mass.
In some obese persons, fatty acid release from visceral adipose tissue triglycerides is substantial and could be an important factor in developing hepatic insulin resistance.
However, excessive fatty acid release from visceral fat is unlikely to be a major factor in the pathogenesis of insulin resistance in skeletal muscle because it represents a very small percentage of total FFAs delivered to muscle tissues. This study provides an important framework for future research.
Additional studies are needed to determine the relationship between FFA delivery to the liver and hepatic insulin sensitivity, the implications of visceral fat metabolism during postprandial conditions, the factors responsible for intersubject variability in the contribution of visceral fat to total FFAs delivered to the liver, the impact of proteins and cytokines secreted by visceral and subcutaneous fat on hepatic and muscle insulin sensitivity, and the relationship between visceral fat and ectopic fat distribution in liver and muscle cells, which can also influence insulin action.
Go to JCI Insight. About Editors Consulting Editors For authors Publication ethics Publication alerts by email Advertising Job board Contact. Videos Conversations with Giants in Medicine Author's Takes Reviews Reviews View all reviews Review Series Lung inflammatory injury and tissue repair Jul Immune Environment in Glioblastoma Feb Korsmeyer Award 25th Anniversary Collection Jan Aging Jul Next-Generation Sequencing in Medicine Jun New Therapeutic Targets in Cardiovascular Diseases Mar Immunometabolism Jan View all review series Viewpoint Collections In-Press Preview Commentaries Research Letters Letters to the Editor Editorials Viewpoint JCI This Month Top read articles Clinical Medicine.
View PDF Download citation information Send a comment Terms of use Standard abbreviations Need help? Email the journal. Top Abstract Fatty acid metabolism and insulin resistance Portal and systemic fatty acid kinetics Clinical implications and future directions Footnotes References Version history.
Metrics details. The association of anthropometric waist circumference xnd hemodynamic Calcium intake guidelines pressure changes Visceral fat and insulin sensitivity abnormalities in Viscerall and lipid metabolism Apple cider vinegar for allergies been Well-maintained fat distribution for a lot of discussions in the last 30 years. However, insulun than years ago an association between visceral and Viscerral obesity with hypertension, gout, and obstructive apnea had already been recognized. Expansion of visceral adipose tissue secondary to chronic over-consumption of calories stimulates the recruitment of macrophages, which assume an inflammatory phenotype and produce cytokines that directly interfere with insulin signaling, resulting in insulin resistance. In turn, insulin resistance IR manifests itself in various tissues, contributing to the overall phenotype of VAS. For example, in white adipose tissue, IR results in lipolysis, increased free fatty acids release and worsening of inflammation, since fatty acids can bind to Toll-like receptors.
Welche gute Gesprächspartner:)
Ihre Idee ist prächtig