Body composition and hormonal health -
Women with negative energy balance had significantly longer usual cycle length However, they did not differ significantly in any of the anthropometric or life style parameters.
In contrast, significant differences in anthropometrics were observed within both negative and positive energy balance groups among groups of women characterized by very low, low, average and high body fat content.
Additionally, in the positive energy balance group, women with very low and high body fat had significantly higher birthweight compared with women with low and average body fat 3. Average values of E2 indices for the body fat quartiles of women with positive and negative energy balance are presented in Table III.
ANOVA analyses of estradiol levels in these groups revealed significant differences in all estradiol indices between women differing with respect to body fat percentage in the positive energy balance group, but not in the negative, energy balance group. Estradiol indices in body fat quartiles of women with positive and negative energy balance.
Women with very low and high body fat had significantly lower levels of E2 over the whole menstrual cycle compared with women with average and low fat Fig. E2 profiles in very low, low, average and high body fat groups of women with positive energy balance. The relationship between body fat and E2 levels was further confirmed by regression analyses in non-overweight women with positive energy balance, but not in those with negative energy balance Table IV.
In the range of 9. We found that nutritional status indicated by body fat percentage is an important factor associated with the levels of estradiol during the menstrual cycle.
In particular, we found a non-linear U-shaped association between body fat percentage and levels of estradiol during the menstrual cycle. We also demonstrated that energy balance confounded the association between estradiol levels and body fat in such a way that in women with positive energy balance, this association was even stronger than it was in the whole sample of women, whereas in women with negative energy balance, no relationship between body fat and estradiol levels was found.
Our findings correspond with the results of other studies concerned with levels of E2 in overweight and obese women. A decreased E2 surge was noted in studies by Grenman et al.
Several authors have demonstrated that, in women, increased adiposity and obesity are related to high androgenic activity Evans et al. This may explain the inversion in the pattern of association between body fat percentage and estradiol levels observed in our study.
In accordance with our results, van der Steeg et al. Gesink Law et al. Levels of estradiol during the menstrual cycle, and especially during its follicular phase, are related to follicular diameter, oocyte quality and endometrial morphology and thickness Ohno and Fujimoto, ; Cahill et al.
Lower levels of E2 during the menstrual cycle and during ovulation frequently correlate with lower pregnancy rates, both in healthy, naturally conceiving women Lipson and Ellison, ; Lu et al.
Our results suggest that lower fecundity, conception and pregnancy rates in underweight, overweight and obese women can be mediated by an unfavorable estradiol environment. Furthermore, the negative linear association between pregnancy rate and BMI in low BMI women found in van der Steeg et al.
study can be easily explained by the linear association between body fat and estradiol levels found in non-overweight participants of our study. Results of our study clarify and extend previous evidence on the association between nutritional status and levels of reproductive steroids.
Several studies conducted on different groups of premenopausal women diabetic, obese, dieting, very lean and normal weight demonstrated contradictory results Howard et al.
This inconsistency partly results from methodological limitations, especially calculations of mean E2 levels based on no more than a few samples from each menstrual cycle. Owing to substantial intra-cycle variation in E2 levels, such sampling is vastly insufficient and can lead to errors in estimating mean E2 levels for individual women Jasienska and Jasienski, In most of these studies, estradiol levels were analyzed from a single blood sample, whereas Williams et al.
In our study, the number of samples taken from a single subject considerably exceeded this requirement. Another limitation of other studies is the use of BMI as the indicator of nutritional status. BMI does not represent sufficient information about nutritional status and accumulated body fat Piers et al.
Frequently, individuals classified as overweight on the basis of BMI are of normal adiposity, especially if they have high muscle mass Hortobagyi et al. Conversely, women classified as normal using BMI criteria frequently have increased adiposity Frankenfield et al. In our study, this limitation was circumvented by direct measurement of body fat percentage.
The concurrent lack of a relationship between estradiol and BMI and positive relationship between estradiol and percent body fat observed in our study provides further evidence that BMI may be a poor indicator of nutritional status.
In addition to making careful measurements of estradiol levels and nutritional status, we were able to estimate the energy balance of women based on changes in body fat during the observational period.
Although we are aware of the fact that changes in the percentage of body fat are only the proxy measures of energy balance, this estimation allowed us to investigate the interactions between nutritional status, energy balance and the estradiol levels across the menstrual cycle, which to our knowledge have not previously been reported.
Energy balance has been shown to influence ovarian steroid profiles in several studies Ellison et al. This fact can explain the lack of a relationship between nutritional status and levels of reproductive hormones demonstrated in populations or groups of women characterized by high physical activity Lager and Ellison, ; Jasienska and Ellison, , , women losing weight due to voluntarily caloric restriction Lager and Ellison, , and women from hunter gatherer and horticulturalist groups in Africa and Nepal Ellison et al.
In contrast, an association between body fat and reproductive hormones has frequently been demonstrated in women from western populations who generally have higher energy intake and lower physical activity; none of these studies, however, controlled for energy balance Brunning et al.
The first limitation of our study is the imprecise estimation of energy balance. Although evaluation of metabolic rate or resting energy expenditure would have been a more accurate method, Abbott et al.
Thus, we believe that a change in body fat percentage provides a good proxy of energy balance in our study participants. Another limitation of our study is that the interval between the first anthropometric measurement and the beginning of the menstrual cycle and between the end of the menstrual cycle and the second anthropometric measurement varied significantly between study participants.
Although differences in these intervals could possibly confound our findings, additional analyses conducted with exclusion of participants with longer intervals between measurements did not change the results of the analyses data not shown.
Although our results point to the important association between nutritional status and energy balance and estradiol levels, our study did not investigate physiological mechanisms that were behind the observed relationship. Several different physiological mechanism have been proposed in other studies, including those postulating the regulatory role of leptin and insulin both indirectly influencing hypothalamic secretion and directly influencing ovarian production of estradiol Smith et al.
Our results support the hypothesis of a regulatory role of nutritional status on potential fertility in reproductive age women, but only in those with positive energy balance. In women of reproductive age, energetic resources are partitioned between maintenance of normal physiological processes and reproduction.
This fat depot is built-up under favorable environmental conditions when energy intake is high, energy expenditure due to physical activity is low and total energy balance is positive.
The consequences of inadequate nutritional status during pregnancy are highly adverse both to the child and to the mother.
Low body mass of a woman prior to and during pregnancy is associated with a high risk of preterm labor, intrauterine growth retardation, low birthweight of the infant and maternal depletion syndrome Jelliffe and Maddocks, ; Winkvist et al. Short-term reproductive suppression in women with low energy reserves may function as an evolutionary adaptation protecting against these risks and improving the chances of successful reproduction in the future Ellison, , ; Jasienska, Polish Committee for Scientific Research 2 P05D 28 to G.
We are grateful to women who participated in the study, and to students of the Faculty of Public Health, Jagiellonian University, who worked as research assistants, Kolastyna SA and Yves Rocher Poland. Google Scholar.
Google Preview. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Advertisement intended for healthcare professionals. Navbar Search Filter Human Reproduction This issue ESHRE Journals Reproductive Medicine Books Journals Oxford Academic Mobile Enter search term Search. Issues More Content Advance articles Editor's Choice ESHRE Pages Mini-reviews Submit Author Guidelines Submission Site Reasons to Publish Open Access Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Branded Books Journals Career Network About About Human Reproduction About the European Society of Human Reproduction and Embryology Editorial Board Alerts Policies Self-Archiving Policy Dispatch Dates Contact ESHRE Journals on Oxford Academic Books on Oxford Academic.
ESHRE Journals. Issues More Content Advance articles Editor's Choice ESHRE Pages Mini-reviews Submit Author Guidelines Submission Site Reasons to Publish Open Access Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Branded Books Journals Career Network About About Human Reproduction About the European Society of Human Reproduction and Embryology Editorial Board Alerts Policies Self-Archiving Policy Dispatch Dates Contact ESHRE Close Navbar Search Filter Human Reproduction This issue ESHRE Journals Reproductive Medicine Books Journals Oxford Academic Enter search term Search.
Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Materials and Methods.
Journal Article. Body fat, energy balance and estradiol levels: a study based on hormonal profiles from complete menstrual cycles. Ziomkiewicz , A. Ziomkiewicz 6. Institute of Anthropology, Polish Academy of Science.
Oxford Academic. Revision received:. PDF Split View Views. Cite Cite A. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions.
Close Navbar Search Filter Human Reproduction This issue ESHRE Journals Reproductive Medicine Books Journals Oxford Academic Enter search term Search. Table I. General characteristics of study participants.
Age years Open in new tab. Table II. Estradiol indices in four body fat groups. Mean E2 Table III. Figure Open in new tab Download slide.
The association between E2 and body fat. Table IV. Positive energy balance. Negative energy balance. Mean E2 55 0. Results of simple regression analysis.
Short-term energy balance: relationship with protein, carbohydrate, and fat balances. Google Scholar PubMed. OpenURL Placeholder Text. Preimplantation hormonal differences between the conception and non-conception menstrual cycles of 32 normal women.
Google Scholar Crossref. Search ADS. Preimplantation urinary hormone profiles and the probability of conception in healthy women. Sex hormone levels in premenopausal African-American women with upper and lower body fat phenotypes. Waist-to-hip ratio, body mass index and sex hormone levels associated with breast cancer risk in premenopausal Caucasian women.
Serum estradiol positively predicts outcomes in patients undergoing in vitro fertilization. Body measurements, estrogen availability and the risk of human breast cancer: a case-control study.
Expected contribution to serum oestradiol from individual ovarian follicles in unstimulated cycles. Relationship between peak serum estradiol levels and treatment outcome in vitro fertilization cycles after embryo transfer on day 3 or day 5.
De Souza. Physiological aspects and clinical sequel of energy deficiency and hypoestrogenism in exercising women. The relation of body size to plasma levels of estrogens and androgens in premenopausal women Maryland, United States. Low maternal weight, failure to thrive in pregnancy, and adverse pregnancy outcomes.
Google Scholar Google Preview OpenURL Placeholder Text. Relationship of androgenic activity to body fat topography, fat cell morphology, and metabolic aberrations in premenopausal women. Metabolic and hormonal profiles: HDL cholesterol as a plausible biomarker of breast cancer risk.
The Norwegian EBBA Study. Google Scholar OpenURL Placeholder Text. Gesink Law. Sex steroid, gonadotropin, cortisol, and prolactin levels in healthy massively obese women: correlation with abdominal fat cell size and effect of weight reduction. Fat distribution, endocrine and metabolic profile in obese women with and without hirsutism.
Sensitivity and specificity of the Quetelet index to assess obesity in men and women. Lack of sex differences in high density lipoproteins in Pima Indians. Studies of obesity, lipase activities, and steroid hormones. Phoenix, AZ: Healthy Lifestyle Research Center, College of Nursing and Health Innovation, Arizona State University.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett Jr DR, Tudor-Locke C, et al. Med Sci Sports Exerc. Article PubMed Google Scholar. Stiegler P, Cunliffe A.
The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med.
Drenowatz C, Hand GA, Sagner M, Shook RP, Burgess S, Blair SN. The prospective association between different types of exercise and body composition. Med Sci Sports Exerc In press.
doi: Asikainen TM, Miilunpalo S, Kukkonen-Harjula K, Nenonen A, Pasanen M, Rinne M, et al. Walking trials in postmenopausal women: effect of low doses of exercise and exercise fractionization on coronary risk factors.
Scand J Med Sci Sports. Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects.
Eur J Clin Nutr. King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, Hills AP, et al. Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss.
Obesity Silver Spring. Schwartz MW, Woods SC, Porte Jr D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity.
J Clin Epidemiol. Kelly LA, McMillan DG, Anderson A, Fippinger M, Fillerup G, Rider J. BMC Med Phys. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc.
Handelsman DJ, Wartofsky L. Requirement for mass spectrometry sex steroid assays in the Journal of Clinical Endocrinology and Metabolism.
J Clin Endocrinol Metab. Rinaldi S, Geay A, Déchaud H, Biessy C, Zeleniuch-Jacquotte A, Akhmedkhanov A, et al. Validity of free testosterone and free estradiol determinations in serum samples from postmenopausal women by theoretical calculations.
Thienpont LM, Van Uytfanghe K, Blincko S, Ramsay CS, Xie H, Doss RC, et al. State-of-the-art of serum testosterone measurement by isotope dilution-liquid chromatography-tandem mass spectrometry. Clin Chem. Owen LJ, Wu FC, Keevil BG. A rapid direct assay for the routine measurement of oestradiol and oestrone by liquid chromatography tandem mass spectrometry.
Ann Clin Biochem. Groenwold RH, Donders AR, Roes KC, Harrell Jr FE, Moons KG. Dealing with missing outcome data in randomized trials and observational studies.
Am J Epidemiol. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. J Am Coll Cardiol. A published erratum appears in. Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE.
Adult weight change and risk of postmenopausal breast cancer. Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE, et al. McTiernan A, Tworoger SS, Ulrich CM, Yasui Y, Irwin ML, Rajan KB, et al.
Effect of exercise on serum estrogens in postmenopausal women: a month randomized clinical trial. Cancer Res. Siiteri PK. Adipose tissue as a source of hormones.
Am J Clin Nutr. Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes. Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms.
Nat Rev Cancer. Berrino F, Bellati C, Secreto G, Camerini E, Pala V, Panico S, et al. Reducing bioavailable sex hormones through a comprehensive change in diet: the diet and androgens DIANA randomized trial.
Bhargava A. J Nutr. Campbell KL, Foster-Schubert KE, Alfano CM, Wang CC, Wang CY, Duggan CR, et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: randomized controlled trial. Kim TN, Choi KM. Sarcopenia: definition, epidemiology, and pathophysiology.
J Bone Metab. Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. American College of Sports Medicine Position Stand: Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults.
Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Expert Panel Members. Based on a systematic review from the Obesity Society Expert Panel, Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, et al.
Management of obesity in adults: European clinical practice guidelines. Obes Facts. Monninkhof EM, Elias SG, Vlems FA, van der Tweel I, Schuit AJ, Voskuil DW, et al.
Physical activity and breast cancer: a systematic review. Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies.
Breast Cancer Res Treat. Rinaldi S, Kaaks R, Friedenreich CM, Key TJ, Travis R, Biessy C, et al. Physical activity, sex steroid, and growth factor concentrations in pre- and post-menopausal women: a cross-sectional study within the EPIC cohort. Cancer Causes Control. Chan MF, Dowsett M, Folkerd E, Bingham S, Wareham N, Luben R, et al.
Usual physical activity and endogenous sex hormones in postmenopausal women: the European Prospective Investigation into Cancer—Norfolk Population Study. Geisler J, Helle H, Ekse D, Duong NK, Evans DB, Nordbø Y, et al. Letrozole is superior to anastrozole in suppressing breast cancer tissue and plasma estrogen levels.
Clin Cancer Res. Lønning PE, Geisler J, Krag LE, Erikstein B, Bremnes Y, Hagen AI, et al. Effects of exemestane administered for 2 years versus placebo on bone mineral density, bone biomarkers, and plasma lipids in patients with surgically resected early breast cancer.
Dixon JM, Renshaw L, Young O, Murray J, Macaskill EJ, McHugh M, et al. Letrozole suppresses plasma estradiol and estrone sulphate more completely than anastrozole in postmenopausal women with breast cancer.
Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, et al. Anastrozole for prevention of breast cancer in high-risk postmenopausal women IBIS-II : an international, double-blind, randomised placebo-controlled trial. Goss PE, Ingle JN, Alés-Martínez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, et al.
Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. A published erratum appears in N Engl J Med.
van Sluijs EM, van Poppel MN, Twisk JW, van Mechelen W. Blair IA. Analysis of estrogens in serum and plasma from postmenopausal women: past present, and future.
Liquid chromatography—tandem mass spectrometry assay for simultaneous measurement of estradiol and estrone in human plasma.
Download references. This work was supported by Dutch Cancer Society grant UU to EMM and Dutch Pink Ribbon Foundation grants PR and PR to EMM. The support from the sponsors was unconditional, and the data collection, study design, management, analysis, interpretation and reporting were performed without their interference.
The role of the sponsors was limited to approving the scientific proposal of the study and covering costs of study personnel salaries, data collection and biochemical analyses. We acknowledge the following people who have collected data or contributed to the running of the study: Marloes van Beurden, Ria Bouwhuis, Bram Dijker, Gerry van Hemert, Manon de Leeuw, Marjon van der Meer, Karen Menninga, Joke Metselaar, Fien Stern, Lizeth Vendrig and Lydeke Zwart Julius Centre, Utrecht ; Silvia Achterberg, Renate Bloemen, Willemien Boersma, Mirjam Floor, Petra Hemeltjen and Veronique Sauerwald Medical Spectrum Twente, Enschede ; Roelof Peters and Jolanda Spruit HU University of Applied Sciences Utrecht ; Carin Schröder, PhD De Hoogstraat Rehabilitation Centre, University Medical Centre Utrecht ; Brian G Keevil and Laura J Owen Department of Biochemistry, University Hospital of South Manchester, Manchester, UK ; Dick van Rumpt, Rick Ruckert, Carolien Huetink and Laura Berends SHO Laboratory, Velp, The Netherlands ; and Eef Lentjes, PhD UMC Utrecht Endocrinology Laboratory for helping interpreting the study results.
Furthermore, we would greatly like to thank all the study participants and the participating dietitians, physiotherapists and Nordic walking instructors in the vicinities of Utrecht and Enschede.
Department of Epidemiology, Julius Centre for Health Sciences and Primary Care, University Medical Centre Utrecht, P. Box , GA, Utrecht, The Netherlands. Willemijn AM. van Gemert, Anne M. May, Jolein A. Iestra, Petra H. National Institute for Public Health and the Environment, Centre for Nutrition, Prevention and Health Services, P.
Box 1, BA, Bilthoven, The Netherlands. Department of Health Sciences and EMGO Institute for Health and Care Research, VU University, Van der Boechorststraat 7, BT, Amsterdam, The Netherlands. Department of Epidemiology, Medisch Spectrum Twente, P. Box , KA, Enschede, The Netherlands.
Department of Research Methodology, Measurement, and Data Analysis, University of Twente, P. Box , AE, Enschede, The Netherlands. Lifestyle and Health Research Group, Faculty of Health Care, Utrecht University of Applied Sciences, P. Box , AD, Utrecht, The Netherlands. You can also search for this author in PubMed Google Scholar.
Correspondence to Evelyn M. PHP, AJS, JAI and EMM were involved in the conception of the study. PHP, AJS, JAI, WAvG and EMM were involved in the study design. PHP, AJS, WAvG and EMM participated in the management and coordination of the study.
WAvG, JvdP, JAI, HW and EMM were involved in data collection. WAvG, AJS, JvdP, AMM, PHP and EMM analysed the data.
WAvG, AJS, JvdP, AMM, PHP and EMM drafted the manuscript. All authors were involved in the interpretation of data and critically revised the content of the manuscript.
All authors read and approved the final manuscript. Treatment effects on sex hormones, adjusted for changes in fat percentage. Analyses done to get insight into whether effects on sex hormones are mediated by changes in body fat.
PDF Secondary analyses of women who lost body weight or remained weight-stable. Effects on sex hormones in women who were adherent to the prescribed physical activity.
Secondary analyses of women adherent to the physical activity prescription. Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. van Gemert, W. et al. Effect of weight loss, with or without exercise, on body composition and sex hormones in postmenopausal women: the SHAPE-2 trial.
Breast Cancer Res 17 , Download citation. Received : 14 April Accepted : 18 August Published : 02 September Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Research article Open access Published: 02 September Effect of weight loss, with or without exercise, on body composition and sex hormones in postmenopausal women: the SHAPE-2 trial Willemijn AM.
van Gemert 1 , Albertine J. Schuit 2 , 3 , Job van der Palen 4 , 5 , Anne M. May 1 , Jolein A. Iestra 1 , Harriet Wittink 6 , Petra H. Monninkhof 1 Show authors Breast Cancer Research volume 17 , Article number: Cite this article 10k Accesses 58 Citations 45 Altmetric Metrics details.
Abstract Introduction Physical inactivity and overweight are risk factors for postmenopausal breast cancer. Conclusions Weight loss with both interventions resulted in favourable effects on serum sex hormones, which have been shown to be associated with a decrease in postmenopausal breast cancer risk.
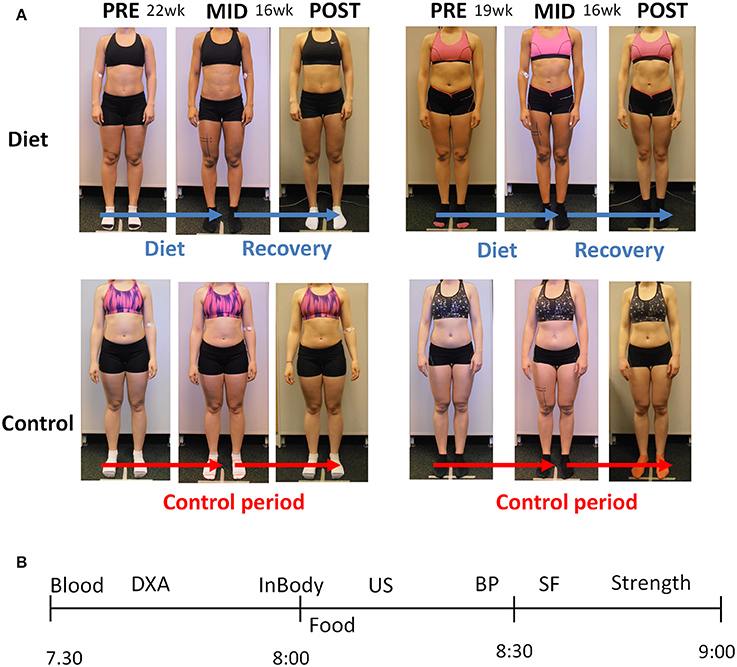
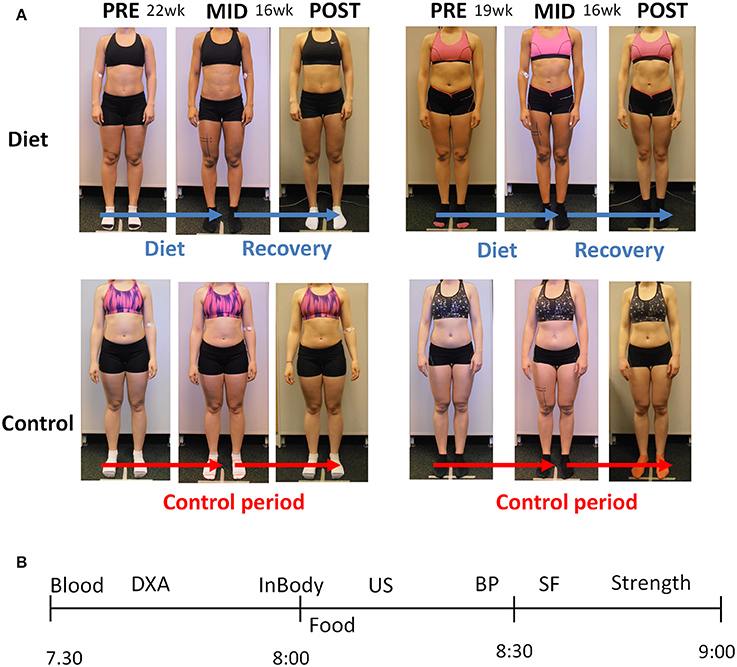
Trial registration ClinicalTrials. Introduction Obesity and physical inactivity are convincing risk factors for postmenopausal breast cancer, according to the World Cancer Research Fund [ 1 ]. Methods Design and study population The SHAPE-2 study is a three-armed, randomised controlled trial in which postmenopausal women are allocated to a diet-induced weight loss intervention, to a combined diet- and exercise-induced weight loss intervention or to a control group.
Table 1 SHAPE-2 study inclusion and exclusion criteria Full size table. Results Women in the intervention and control groups were comparable in baseline characteristics Table 2. Table 2 Baseline characteristics of the SHAPE-2 study population Full size table. Full size image.
Table 3 Baseline and week differences in body composition and fitness between study groups Full size table. Table 4 Baseline and week differences in serum sex hormones and treatment effects between study groups Full size table.
Abbreviations BMI: Body mass index CI: Confidence interval DEXA: Dual-energy X-ray absorptiometry HRR: Heart rate reserve LC-MS: Liquid chromatography—mass spectrometry MET: Metabolic equivalents NEW: Nutrition and Exercise for Women trial SHAPE: Sex Hormones and Physical Exercise study SHBG: Sex hormone-binding globulin SQUASH: Short Questionnaire to Assess Health-Enhancing Physical Activity TER: Treatment effect ratio VO 2 peak : Peak oxygen uptake.
References World Cancer Research Fund, American Institute for Cancer Research AICR. Article PubMed PubMed Central Google Scholar Kaaks R, Rinaldi S, Key TJ, Berrino F, Peeters PH, Biessy C, et al.
Article CAS PubMed Google Scholar The Endogenous Hormones and Breast Cancer Collaborative Group. Article Google Scholar McTiernan A, Tworoger SS, Rajan KB, Yasui Y, Sorenson B, Ulrich CM, et al. CAS PubMed Google Scholar Monninkhof EM, Velthuis MJ, Peeters PH, Twisk JW, Schuit AJ. Article CAS PubMed Google Scholar Friedenreich CM, Woolcott CG, McTiernan A, Ballard-Barbash R, Brant RF, Stanczyk FZ, et al.
Article CAS PubMed PubMed Central Google Scholar van Gemert WA, Iestra JI, Schuit AJ, May AM, Takken T, Veldhuis WB, et al. Article PubMed PubMed Central Google Scholar Health Council of the Netherlands.
CAS PubMed Google Scholar Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. Article PubMed Google Scholar Stiegler P, Cunliffe A. Article PubMed Google Scholar Drenowatz C, Hand GA, Sagner M, Shook RP, Burgess S, Blair SN.
Article PubMed Google Scholar Garrow JS, Summerbell CD. CAS PubMed Google Scholar King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, Hills AP, et al. Article PubMed Google Scholar Schwartz MW, Woods SC, Porte Jr D, Seeley RJ, Baskin DG. CAS PubMed Google Scholar Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D.
Article PubMed Google Scholar Kelly LA, McMillan DG, Anderson A, Fippinger M, Fillerup G, Rider J. Article PubMed PubMed Central Google Scholar Freedson PS, Melanson E, Sirard J.
Article CAS PubMed Google Scholar Handelsman DJ, Wartofsky L. Article CAS PubMed Google Scholar Rinaldi S, Geay A, Déchaud H, Biessy C, Zeleniuch-Jacquotte A, Akhmedkhanov A, et al.
CAS PubMed Google Scholar Thienpont LM, Van Uytfanghe K, Blincko S, Ramsay CS, Xie H, Doss RC, et al. Article CAS PubMed Google Scholar Owen LJ, Wu FC, Keevil BG. Article CAS PubMed Google Scholar Groenwold RH, Donders AR, Roes KC, Harrell Jr FE, Moons KG.
Article PubMed Google Scholar Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. Article Google Scholar Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE.
Article CAS PubMed Google Scholar Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE, et al. Article PubMed Google Scholar McTiernan A, Tworoger SS, Ulrich CM, Yasui Y, Irwin ML, Rajan KB, et al. Article CAS PubMed Google Scholar Siiteri PK. CAS PubMed Google Scholar Hardy OT, Czech MP, Corvera S.
Article CAS PubMed PubMed Central Google Scholar Calle EE, Kaaks R. Article CAS PubMed Google Scholar Berrino F, Bellati C, Secreto G, Camerini E, Pala V, Panico S, et al.
CAS PubMed Google Scholar Bhargava A. CAS PubMed Google Scholar Campbell KL, Foster-Schubert KE, Alfano CM, Wang CC, Wang CY, Duggan CR, et al. Article CAS PubMed PubMed Central Google Scholar Kim TN, Choi KM.
Article PubMed PubMed Central Google Scholar Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. Article PubMed Google Scholar Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al.
Article Google Scholar Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, et al. Article PubMed Google Scholar Monninkhof EM, Elias SG, Vlems FA, van der Tweel I, Schuit AJ, Voskuil DW, et al.
Article PubMed Google Scholar Wu Y, Zhang D, Kang S. Article PubMed Google Scholar Rinaldi S, Kaaks R, Friedenreich CM, Key TJ, Travis R, Biessy C, et al. Article CAS PubMed Google Scholar Chan MF, Dowsett M, Folkerd E, Bingham S, Wareham N, Luben R, et al.
Article CAS PubMed Google Scholar Geisler J, Helle H, Ekse D, Duong NK, Evans DB, Nordbø Y, et al. Article CAS PubMed Google Scholar Lønning PE, Geisler J, Krag LE, Erikstein B, Bremnes Y, Hagen AI, et al.
Article PubMed Google Scholar Dixon JM, Renshaw L, Young O, Murray J, Macaskill EJ, McHugh M, et al. Article CAS PubMed Google Scholar Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, et al.
Johannes D. Veldhuis, James N. Hexlth, Erick J. Richmond, Alan D. Rogol, Jennifer C. Lovejoy, Melinda Sheffield-Moore, Nelly Mauras, Cyril Y. Body composition exhibits marked variations across the early human lifetime.Body composition and hormonal health -
J Natl Cancer Inst. Article Google Scholar. McTiernan A, Tworoger SS, Rajan KB, Yasui Y, Sorenson B, Ulrich CM, et al. Effect of exercise on serum androgens in postmenopausal women: a month randomized clinical trial. Cancer Epidemiol Biomarkers Prev.
CAS PubMed Google Scholar. Monninkhof EM, Velthuis MJ, Peeters PH, Twisk JW, Schuit AJ. Effect of exercise on postmenopausal sex hormone levels and role of body fat: a randomized controlled trial. J Clin Oncol. Friedenreich CM, Woolcott CG, McTiernan A, Ballard-Barbash R, Brant RF, Stanczyk FZ, et al.
Alberta Physical Activity and Breast Cancer Prevention Trial: sex hormone changes in a year-long exercise intervention among postmenopausal women. Article CAS PubMed PubMed Central Google Scholar.
van Gemert WA, Iestra JI, Schuit AJ, May AM, Takken T, Veldhuis WB, et al. Design of the SHAPE-2 study: the effect of physical activity, in addition to weight loss, on biomarkers of postmenopausal breast cancer risk. BMC Cancer. Health Council of the Netherlands. Guidelines for a healthy diet The Hague, The Netherlands: Author; 18 December Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR.
Obes Rev. Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. The compendium of physical activities tracking guide.
Phoenix, AZ: Healthy Lifestyle Research Center, College of Nursing and Health Innovation, Arizona State University. Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett Jr DR, Tudor-Locke C, et al. Med Sci Sports Exerc. Article PubMed Google Scholar.
Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. Drenowatz C, Hand GA, Sagner M, Shook RP, Burgess S, Blair SN.
The prospective association between different types of exercise and body composition. Med Sci Sports Exerc In press. doi: Asikainen TM, Miilunpalo S, Kukkonen-Harjula K, Nenonen A, Pasanen M, Rinne M, et al.
Walking trials in postmenopausal women: effect of low doses of exercise and exercise fractionization on coronary risk factors. Scand J Med Sci Sports.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, Hills AP, et al. Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss.
Obesity Silver Spring. Schwartz MW, Woods SC, Porte Jr D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity.
J Clin Epidemiol. Kelly LA, McMillan DG, Anderson A, Fippinger M, Fillerup G, Rider J. BMC Med Phys. Freedson PS, Melanson E, Sirard J.
Calibration of the Computer Science and Applications, Inc. Handelsman DJ, Wartofsky L. Requirement for mass spectrometry sex steroid assays in the Journal of Clinical Endocrinology and Metabolism.
J Clin Endocrinol Metab. Rinaldi S, Geay A, Déchaud H, Biessy C, Zeleniuch-Jacquotte A, Akhmedkhanov A, et al. Validity of free testosterone and free estradiol determinations in serum samples from postmenopausal women by theoretical calculations.
Thienpont LM, Van Uytfanghe K, Blincko S, Ramsay CS, Xie H, Doss RC, et al. State-of-the-art of serum testosterone measurement by isotope dilution-liquid chromatography-tandem mass spectrometry.
Clin Chem. Owen LJ, Wu FC, Keevil BG. A rapid direct assay for the routine measurement of oestradiol and oestrone by liquid chromatography tandem mass spectrometry. Ann Clin Biochem. Groenwold RH, Donders AR, Roes KC, Harrell Jr FE, Moons KG.
Dealing with missing outcome data in randomized trials and observational studies. Am J Epidemiol. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al.
J Am Coll Cardiol. A published erratum appears in. Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult weight change and risk of postmenopausal breast cancer. Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE, et al. McTiernan A, Tworoger SS, Ulrich CM, Yasui Y, Irwin ML, Rajan KB, et al.
Effect of exercise on serum estrogens in postmenopausal women: a month randomized clinical trial. Cancer Res. Siiteri PK. Adipose tissue as a source of hormones. Am J Clin Nutr. Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity?
Curr Opin Endocrinol Diabetes Obes. Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms.
Nat Rev Cancer. Berrino F, Bellati C, Secreto G, Camerini E, Pala V, Panico S, et al. Reducing bioavailable sex hormones through a comprehensive change in diet: the diet and androgens DIANA randomized trial. Bhargava A.
J Nutr. Campbell KL, Foster-Schubert KE, Alfano CM, Wang CC, Wang CY, Duggan CR, et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: randomized controlled trial. Kim TN, Choi KM. Sarcopenia: definition, epidemiology, and pathophysiology.
J Bone Metab. Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. American College of Sports Medicine Position Stand: Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al.
Expert Panel Members. Based on a systematic review from the Obesity Society Expert Panel, Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, et al. Management of obesity in adults: European clinical practice guidelines. Obes Facts. Monninkhof EM, Elias SG, Vlems FA, van der Tweel I, Schuit AJ, Voskuil DW, et al.
Physical activity and breast cancer: a systematic review. Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. Rinaldi S, Kaaks R, Friedenreich CM, Key TJ, Travis R, Biessy C, et al. Physical activity, sex steroid, and growth factor concentrations in pre- and post-menopausal women: a cross-sectional study within the EPIC cohort.
Cancer Causes Control. Chan MF, Dowsett M, Folkerd E, Bingham S, Wareham N, Luben R, et al. Usual physical activity and endogenous sex hormones in postmenopausal women: the European Prospective Investigation into Cancer—Norfolk Population Study.
Geisler J, Helle H, Ekse D, Duong NK, Evans DB, Nordbø Y, et al. Letrozole is superior to anastrozole in suppressing breast cancer tissue and plasma estrogen levels. Clin Cancer Res.
Lønning PE, Geisler J, Krag LE, Erikstein B, Bremnes Y, Hagen AI, et al. Effects of exemestane administered for 2 years versus placebo on bone mineral density, bone biomarkers, and plasma lipids in patients with surgically resected early breast cancer.
Dixon JM, Renshaw L, Young O, Murray J, Macaskill EJ, McHugh M, et al. Letrozole suppresses plasma estradiol and estrone sulphate more completely than anastrozole in postmenopausal women with breast cancer. Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, et al.
Anastrozole for prevention of breast cancer in high-risk postmenopausal women IBIS-II : an international, double-blind, randomised placebo-controlled trial. Goss PE, Ingle JN, Alés-Martínez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, et al.
Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. A published erratum appears in N Engl J Med. van Sluijs EM, van Poppel MN, Twisk JW, van Mechelen W. Blair IA. Analysis of estrogens in serum and plasma from postmenopausal women: past present, and future.
Liquid chromatography—tandem mass spectrometry assay for simultaneous measurement of estradiol and estrone in human plasma. Download references. This work was supported by Dutch Cancer Society grant UU to EMM and Dutch Pink Ribbon Foundation grants PR and PR to EMM.
The support from the sponsors was unconditional, and the data collection, study design, management, analysis, interpretation and reporting were performed without their interference.
The role of the sponsors was limited to approving the scientific proposal of the study and covering costs of study personnel salaries, data collection and biochemical analyses.
We acknowledge the following people who have collected data or contributed to the running of the study: Marloes van Beurden, Ria Bouwhuis, Bram Dijker, Gerry van Hemert, Manon de Leeuw, Marjon van der Meer, Karen Menninga, Joke Metselaar, Fien Stern, Lizeth Vendrig and Lydeke Zwart Julius Centre, Utrecht ; Silvia Achterberg, Renate Bloemen, Willemien Boersma, Mirjam Floor, Petra Hemeltjen and Veronique Sauerwald Medical Spectrum Twente, Enschede ; Roelof Peters and Jolanda Spruit HU University of Applied Sciences Utrecht ; Carin Schröder, PhD De Hoogstraat Rehabilitation Centre, University Medical Centre Utrecht ; Brian G Keevil and Laura J Owen Department of Biochemistry, University Hospital of South Manchester, Manchester, UK ; Dick van Rumpt, Rick Ruckert, Carolien Huetink and Laura Berends SHO Laboratory, Velp, The Netherlands ; and Eef Lentjes, PhD UMC Utrecht Endocrinology Laboratory for helping interpreting the study results.
Furthermore, we would greatly like to thank all the study participants and the participating dietitians, physiotherapists and Nordic walking instructors in the vicinities of Utrecht and Enschede.
Department of Epidemiology, Julius Centre for Health Sciences and Primary Care, University Medical Centre Utrecht, P. Box , GA, Utrecht, The Netherlands.
Willemijn AM. van Gemert, Anne M. May, Jolein A. Iestra, Petra H. National Institute for Public Health and the Environment, Centre for Nutrition, Prevention and Health Services, P. Box 1, BA, Bilthoven, The Netherlands. Department of Health Sciences and EMGO Institute for Health and Care Research, VU University, Van der Boechorststraat 7, BT, Amsterdam, The Netherlands.
Department of Epidemiology, Medisch Spectrum Twente, P. Box , KA, Enschede, The Netherlands. Department of Research Methodology, Measurement, and Data Analysis, University of Twente, P. Box , AE, Enschede, The Netherlands. Lifestyle and Health Research Group, Faculty of Health Care, Utrecht University of Applied Sciences, P.
Data are adapted from the Center for Disease Control CDC Growth Charts 3. Standardized growth curves assume a population-based mean timing of pubertal onset and progress.
However, any given child may exhibit a delay or advance in sexual maturation and thus diverge at least temporarily from group predictions 2 , 20 , A relevant family history should help in interpreting the clinical significance of serial growth measurements. As an additional aid, reference height-velocity predictions are available for average, early-, and late-maturing children in Northern Europe 3.
Normative weight trajectories are illustrated in Figure 3. The exact adaptive processes that mediate evident extracellular fluid loss and inferred tissue catabolism at this time have not been articulated fully, but presumptively entail combined nutritional and endocrine factors.
Normative weight kilograms projections in boys and girls from birth through midchildhood. Data are presented as in Fig. In the first year of life, male infants gain weight slightly more rapidly than female counterparts, such that at 12 months of age boys weigh an average of 10 kg and girls 9.
At age 7 yr, boys usually weigh 23 kg and girls 22 kg. Extended, prospective, ethnicity-specific, and population-based normative body composition data stratified by gender in childhood are lacking.
Comprehensive body-compositional investigations will require the use of validated quantitative procedures, minimal if any radiation exposure, high procedural reproducibility, and repeated application in randomly selected cohorts of healthy children.
Accurate estimates of and population-based statistical boundaries for fat mass FM are crucial to classify children accurately as lean, normal, overweight, or obese. Analogously, reliable quantitation of fat-free mass FFM is important to identify relative or absolute sarcopenia and osteopenia.
Valid measures of regional adiposity e. Projections of the gender-specific evolution of FM, FFM, and percentage body fat in Caucasian children are given in Fig.
These predictions aggregate the results of accurate multicompartmental analyses performed cross-sectionally at selected stages in infancy, childhood, puberty, and early adulthood 22 , 29 , Interpolations are required to supplement incomplete body-compositional data in midchildhood and early adolescence.
Although ethnic comparisons are limited, one pediatric investigation compared FM and FFM estimates among African-, European-, and Mexican-American children at or over the age of 4 yr 31 Fig.
This analysis like several recent other studies reported a higher mean FM value than that typically observed earlier in children Estimates of FFM, FM, and percentage body fat in European-American boys closed symbols and girls open symbols from infancy through early adulthood age 20 yr.
Curves reflect aggregate data compiled from and interpolated among cross-sectional analyses 22 , 25 , 29 , 30 , Units are kilograms FFM, FM Changes in FM and FFM of African-American filled circles , Caucasian open circles , and Mexican-American filled triangles girls left panels and boys right panels ages 5 to 19 yr.
Data were collected cross-sectionally from healthy youth. FFM was calculated from TBW data using age-appropriate constants for hydration of FFM.
FM was determined by subtraction from total body weight. Note different y-axis ranges for girls and boys and reduction in pubertal FM in Caucasian boys only. The newborn boy has about 6. Thereafter, FFM begins to accumulate preferentially. Although fractional FFM remains comparable by gender across midchildhood, boys accrue about 1 kg more absolute FFM than girls before puberty 22 , 29 , In puberty, boys acquire FFM at a greater rate kilograms per year and for a longer period than girls.
In one analysis, stable adult values of FFM were attained by approximately 15—16 yr of age in girls and 2—3 yr later in boys In absolute terms, FM kilograms is comparable by sex in children ages 3—5 yr.
In adolescence, girls gain absolute FM at an average annual rate of 1. Hence, percentage body fat declines in pubertal boys Primary components of FFM water, protein, and mineral vary markedly in infancy and adapt further in childhood and adolescence Fig.
Data apply to the newborn, prepubertal, and pubertal boy closed symbols and girl open symbols. Interrupted lines reflect predictions based on a nominal adult cadaveric FFM density of 1. Compiled variously from cross-sectional data reported in Refs. During the age interval of This sex difference wanes until boys begin and girls complete puberty 25 , 29 , Protein constitutes The mineral fraction in FFM remains stable in infancy and early childhood, and then rises disproportionately over protein and water in midchildhood and early puberty 22 , 25 , Bone mineral density BMD determined at near-peak height velocity is greater in boys than girls 25 , 29 , BMD is higher in African-American than Caucasian individuals before and after puberty in both sexes 36 , The precise endocrine determinants of this consistent ethnic difference are not known.
Nonendocrine genetic and environmental factors may contribute to some differences. One analysis revealed higher overnight serum concentrations of GH and estradiol in African-American than Caucasian men, which levels correlated positively with BMD No comparable distinction was evident before puberty or in women The foregoing epidemiological observations highlight the need to better understand the specific mechanisms by which ethnicity, gender, and developmental age modulate the endocrine control of human growth and body composition Body composition evolves dramatically in utero and across infancy, childhood, puberty, and adulthood and appears to be conditional on early developmental events 28 , 34 , 35 , 41 — Quantitation of body composition relies on auxological or anthropological attributes [ e.
Clinical measures are then applied in empirically constructed regression correlation or prediction equations to estimate unobserved features of body composition 26 , 35 , 46 — Primary estimates of body composition were derived by chemical analyses of adult cadaveric tissues 27 , Such data, albeit limited, provide validation for secondary estimates based on densitometry e.
Height meters and weight kilograms are simple anthropological attributes. Algebraic combinations of these two measures are used to compute the BMI kilograms per square meter , ponderal index kilograms per cubic meter or Benn index kilograms per meter BMI has been applied to categorize children as lean, normal, overweight, or obese 54 , However, this metric varies with developmental age, gender, and ethnicity 27 , 55 — For example, BMI is high in the first year of life, decreases in early childhood ages 2—5 yr , and then increases in puberty 54 , Accordingly, BMI should be compared via age-stratified standardized z-scores or percentiles defined in healthy populations, e.
BMI does not quantitate body composition. Indeed, this metric amalgamates frame size mineral content , total FM visceral and sc and lean tissue 27 , 28 , 30 , 52 , Thus, a short, muscular adolescent could be assigned a high BMI spuriously suggestive of obesity 47 , Moreover, treatment with recombinant human rh GH often reduces FM by 2—3 kg and increases lean body mass comparably in the hypopituitary adult, while leaving BMI unchanged Indices like BMI also do not monitor the regional fat distribution e.
This distinction is significant epidemiologically, because visceral fat accumulation predicts higher risk of peripheral insulin resistance, dyslipidemia, adult cardiovascular disease, hypoandrogenemia, elevated free salivary cortisol, reduced concentrations of SHBG, IGFBP-1, LH, and high-density lipoprotein, and impoverished daily GH production 22 , 26 , 28 , 69 — Recent investigations suggest that deficiency of intrauterine growth factors, degree of fetal stress, low birth weight, relative hypercortisolemia, impaired glucose disposal in midchildhood, and premature adrenarche further forecast greater risk of insulin resistance, cardiovascular disease, dyslipidemia, and abdominal obesity in adulthood 39 , 77 — Densitometric methods partition body composition into two mutually exclusive compartments, viz.
Calculations relate whole-body density weight divided by volume to FM and FFM by way of average tissue-density constants 24 , To estimate whole-body density, weight is quantitated accurately on a dry scale, and volume is estimated by underwater weighing, clinical volumetry, or air plethysmography Water-displacement procedures are based on the principle of Archimedes, and thus require: 1 complete submersion of the volunteer in a suitable water-filled chamber to record underwater weight hydrodensitometry or quantitate water overflow into a burrette clinical volumetry ; and 2 accurate measurement of functional residual lung capacity by nitrogen washout to correct for the thoracic gas space.
The latter determination introduces the majority of technical variability into the final estimate of percentage body fat. Limitations of hydrodensitometry include the requirement for a water tank, variable subject reluctance, and multiple up to 10 submersions to ensure technical reproducibility.
This procedure may be less stressful to the subject than repeated immersion in a water chamber 89 , One plethysmographic unit comprises a sealed fiberglass capsule or pod. The volunteer enters the chamber wearing a tightly fitting swimsuit and swim cap, views the room through a small window, and breathes quietly for several minutes while an internal diaphragm is oscillated to generate small changes in air pressure.
The air-displacement estimate is also corrected for thoracic gas volume above. Cross-validating analyses indicate that air- and water-displacement methods perform comparably in young adults.
In densitometric techniques, one calculates percentage body fat from the density estimate using an empirical regression model, such as that of Brozek et al.
Both sets of equations assume a nominal adult tissue density of 0. However, the use of adult tissue-density constants forces an overestimate of percentage body fat in children Fig. This artifact arises because the true density of FFM is as low as 1. Accordingly, Lohman and colleagues suggest the use of age-specific tissue-density constants in the Siri model 24 , This adjustment obviates systematic overestimation bias in younger subjects.
However, compared with multicompartmental methods below , densitometry may yield inconsistent individual predictions random procedural bias Values for the 2C model are not shown directly, but are calculated readily by addition of the X and Y values.
Equivalent models would yield a zero mean bias interrupted lines. Reliable correlations between the two methods would afford limited y-axis variance random experimental variations. The implications of two assumptions are illustrated; viz.
Interrupted lines depict mean systematic bias, and dotted lines define any trend in bias slope of predicted linear regression ± 2 sd , continuous curves. P values test a null hypothesis of no trend in bias. Symbols distinguish developmental strata; viz. Stages I and II correspond to pre- and early puberty, and stages III and IV to midpuberty and adulthood, respectively.
Reproduced from Ref. The Bland-Altman graphical representation was reported earlier. TBW is quantitated by the degree of dilution in the aqueous compartment of a known amount of a stable or radioactive isotope of water e.
Isotope concentrations are monitored in one or more timed postequilibration samples of serum, urine, saliva, or expired air by liquid scintigraphy 3 H 2 O , infrared spectrometry 2 H 2 O , or isotope-ratio mass spectroscopy 2 H 2 O or H 2 18 O The degree of final isotope dilution is proportionate to TBW.
Multicompartmental models are used to quantitate FM and the principal components of FFM water, mineral, and protein 29 , 30 , 59 , 93 — For example, one method determines TBW by isotope dilution above and quantitates FM and mineral mass by DEXA.
Some compartmental models include the determination of body cell mass e. Two-compartment analyses of body composition use several means to evaluate the components of FFM 26 , In the water-density model, TBW is quantitated first to calculate FM total weight minus TBW.
Protein and mineral content of FFM are estimated secondly from age- and gender-specific prediction equations. In the mineral-density model, bone mineral content is determined so as to compute summed water and protein mineral-free lean tissue and FM The mean bias of the water-density calculation of FM is approximately 0.
On the other hand, the mineral-density model may overestimate percentage body fat by as much as 5—7. Predictions by DEXA showed systematic positive bias; viz. Data are presented as defined in the legend of Fig.
DEXA scanning is a contemporary three-compartment model. DEXA quantitates FM, mineral and mineral-free lean tissue protein and water based on differential tissue absorption of two distinct x-ray energy peaks 31 , 35 , 43 , The volunteer lies supine on a table under a detector panel placed over the x-ray source.
X-rays are fractionated into 40 keV and 70— keV energy streams. Prediction bias arises from DEXA determinations made near the surface of the body due to disproportionate proximity of mineral and sc fat and the appendicular skeleton due to undue contiguity of muscle and connective tissue.
DEXA precision is higher when applied to calibration phantoms than to the human skeleton or the whole body 96 , In adults, the reproducibility of DEXA-based quantitation of BMD averages 0. DEXA scanning tends to predict falsely high percentage body fat in children and older adults 30 , 95 Fig.
DEXA likewise overestimated FM in two recent primary validation studies using the whole carcass of immature swine , Practical limitations include equipment and technician costs and low-dose radiation exposure 1—3 mrad, or less than that contributed by cosmic background during a single km air flight.
Nonetheless, DEXA technology offers a valuable means to estimate body composition. Additional important insights are achievable by way of computed tomography CT and magnetic resonance imaging MRI , because these techniques allow one to appraise the regional distribution of fat.
Intraabdominal fat is a key epidemiological determinant of insulin resistance and cardiovascular risk CT provides one well-validated means to quantitate intraabdominal adiposity.
CT is technically precise in discriminating adipose tissue and affords a brief scan time that obviates motion artifact To estimate abdominal fat, the CT examination is performed at the level of the fourth or fifth lumbar vertebrae, the corresponding intervertebral disc space, or somewhat less reliably the umbilicus.
Data are expressed as the cross-sectional area square centimeters of a demarcated region of adipose tissue, such as visceral mesenteric, pericolic, and perirenal , retroperitoneal, and sc fat , A recent distinction between superficial and deep sc FM suggests that the latter may also predict increased cardiovascular health risk MRI offers a complementary method to quantify regional FM that does not require x-ray exposure.
Although not evaluated exhaustively in children, MRI outcomes correlate with those of CT Table 1 summarizes available CT and MRI data in children as distinguished by peripubertal age, gender, and ethnicity in cross-sectional analyses.
However, appropriately stratified longitudinal comparisons will be required to definitively assess the transpubertal control of regional fat distribution in girls and boys. Concomitant metabolic implications of visceral and sc accumulation and dissipation e.
Finally, anatomic and metabolic adaptations across puberty need to be correlated with changing hormone outflow viz. Impact of childhood age, gender, and ethnicity on abdominal visceral and sc fat accumulation. Body composition may be assessed clinically by physical anthropometry e.
In some studies, average predictions of percentage body fat derived from summed skinfold thickness agree well with multicompartmental analysis Fig. Systematic and nonsystematic bias inherent in two particular field models compared with a four-compartment criterion model 4C in quantitating percentage body fat in children.
Top , Skinfold-thickness prediction equation originally estimated from a 4C criterion model ; bottom , bioelectrical impedance prediction equation derived from a 4C criterion model. Data presentation is described in the legend of Fig.
From an endocrine vantage, normal physical growth and sexual maturation require time-evolving coordination among the somatotropic, gonadotropic, and adipostat systems — Time-varying somatic, visceral, endocrine, and metabotropic signals are integrated to a significant degree in hypothalamic centers — Additional interaxis control is accomplished by convergent and divergent actions of the corresponding hormones on the pituitary gland and peripheral target tissues 40 , — States of mono- and bihormonal deficiency underscore the inferred interplay between somatotropic peptides and gonadal sex steroids in directing adult body composition and sexual maturation — For example, in the human, mouse, and rat, isolated GH deficiency reduces the production of major GH-dependent hepatic proteins, viz.
In particular, deprivation of GH and IGF-I: 1 delays the timely onset of puberty in all species studied ; 2 slows the pace of pubertal maturation all species ; 3 attenuates phallic growth human ; 4 reduces adult testicular size rodent ; and 5 impairs sperm motility mouse ; but 6 does not abrogate fertility in the mature individual all species , , — In particular, therapy with a GnRH analog suppresses concentrations of estradiol and testosterone profoundly and those of GH, IGF-I, and IGFBP-3 significantly, but does not affect measurements of cortisol or adrenal androgens , Gonadal-axis down-regulation may thereby obviate rapid skeletal maturation not only by sex-steroid depletion but also by secondary inhibition of the somatotropic axis Albeit originally hypothesized as a means to stimulate growth in the face of bone-age delay, combining rh GH supplementation with GnRH agonist therapy in children with sexual precocity may enhance predicted final stature , , Several mechanistic insights are relevant to this network-like concept.
Second, endogenous gonadal sex steroids amplify the synthesis of GH and IGF-I and regulate the availability of IGFBPs and cognate proteases 90 , — , — Third, GH, IGF-I, IGF-II, insulin, and sex steroids interact via complex heterologous control of receptor-effector signaling pathways , , — And, fourth, sex steroids and insulinomimetic peptides act in combination to govern appetite, thermoregulation, behavior, and energy expenditure via central and peripheral pathways — Comprehensive formal integration of the foregoing multivalent mechanisms is not yet possible.
Prolonged deprivation of sex-steroid hormones at or after the time of expected puberty predisposes to reduced peak bone mass, attendant osteopenia, osteoporosis, and major fractures in the adult 56 , — Cross-sectional epidemiological analyses demonstrate that total and bioavailable non-SHBG-bound estradiol concentrations predict bone mass in women and men more accurately than total or bioavailable testosterone concentrations , — Data from four longitudinal investigations corroborate the fundamental association between peripheral estrogen concentrations and bone mass in the aging individual 56 , Testosterone, GH, IGF-I, and in some studies leptin concentrations also correlate with TBW in some analyses , Albeit incompletely defined, heterogeneous genetic factors are prominent determinants of bone mass in healthy individuals , Testosterone replacement in hypogonadal boys and men increases TBW incrementally in proportion to the degree of androgen deficiency at presentation , — The anabolic effects of testosterone in vivo are not fully understood but are associated with augmentation of at least: 1 pulsatile GH secretion, which drives longitudinal bone growth , , , , ; 2 IGF-I synthesis in both liver and bone cells , , — ; 3 gastrointestinal absorption and skeletal retention of calcium and magnesium , — ; 4 muscle mass, mechanical loading, and energy expenditure, which in turn correlate with bone mineral content and density 90 , , , , , — ; 5 biochemical markers of osteoblastic activity, such as osteocalcin ; and 6 epiphyseal growth-plate maturation, which culminates in mineralization-dependent cessation of skeletal elongation 15 , — In vitro studies affirm these inferences and further illustrate that in rodent species testosterone and 5α-DHT can stimulate osteoblastic activity, inhibit apoptosis of osteoblasts and osteocytes, suppress osteoclastogenesis, and promote cortical periosteal bone apposition — Androgen- and estrogen-dependent stimulation of epiphyseal mineralization underscores the clinical challenge of tailoring sex-hormone replacement in hypogonadal children to optimize total skeletal growth without inducing premature fusion of the growth plate — Androgen receptors are expressed in human osteoblastic cells and mature osteocytes A normal linear growth spurt is described in 46XY patients with complete androgen insensitivity testicular-feminization syndrome due to inactivating mutation of the cognate receptor , Nonetheless, loss of androgen-receptor function limits adult height and skeletal volume bone size in the genotypic male to values intermediate between those of the unaffected male and female A reduction in bone mineral content is reported in some but not other patients with testicular feminization syndrome.
Supraphysiological amounts of aromatizable and nonaromatizable androgens stimulate osteoblast proliferation, antagonize the osteoclast-activating effect of PTH, and elevate markers of bone growth , — In experimental animals, 5α-DHT especially stimulates periosteal appositional skeletal growth and thereby increases cortical bone formation , — However, available data are not facile to interpret, because 5α-reduced products of testosterone activate the androgen receptor and simultaneously impede estrogen action in some tissues — In the sex steroid-depleted setting, transdermal repletion of testosterone or estradiol alone suppressed indices of bone resorption, increased markers of bone formation, and stimulated production of osteoprotegerin, a potent inhibitor of osteoclastogenesis below.
Each of the effects of testosterone was blunted by pharmacological aromatase blockade, with the exception of increased synthesis of osteocalcin, a marker of osteoblast function. Comparable mechanistic investigations of sex steroid-specific control of skeletal development are not available in childhood.
Moreover, no studies have extended discrete receptor agonist and antagonist analyses over prolonged intervals years in the human. Estrogenic steroids repress osteoclastogenesis, promote epiphyseal maturation, stimulate endosteal and trabecular bone formation, augment mineralization, and increase tensile bone strength , , , , — Selective estrogen receptor ER modulators e.
Estrogen supplementation also stimulates the intestinal absorption and skeletal retention of calcium, which processes contribute to bone mineralization — Estrogens drive proliferation and differentiation of the entire osteoblastic-cell lineage; enhance the anabolic actions of other trophic signals e.
The last-named glycoprotein is a potent inhibitor of osteoclastogenesis and inducer of osteoblast cytodifferentiation 77 , , , , — Gene transcripts encoding truncated and full-length ERα and ERβ are detectable in osteoprogenitor cells, differentiated osteoblasts, and mature osteocytes , , Expression of ERβ predominates in immature bone and wanes with skeletal maturation , As highlighted in Table 2 , inactivating mutations of ERα or the aromatase gene but not ERβ cause severe osteoporosis and impair epiphyseal mineralization in the human and mouse 10 , , , , , , — In several patients with rare inborn aromatase deficiency, repletion of estradiol stimulated prompt epiphyseal maturation and bone mineralization, whereas testosterone supplementation did not , Albeit less well studied, certain molecular polymorphisms of the estrogen-receptor gene also predict reduced BMD epidemiologically.
Skeletal changes associated with genetic inactivation of ER, androgen receptor AR , or aromatase enzyme. Arrows denote relative changes compared with wild-type.
See text for detailed discussion and references. NL, Normal. Experiments based on short-term pharmacological inhibition of the aromatase enzyme are consistent with genetic inferences.
In older men and aged male rats, administration of specific aromatase antagonists increased biochemical markers of bone resorption and where assessed in the rodent impaired the pubertal gain in skeletal calcium and in the human and rodent accelerated the age-related decline in mineral density , , , One prospectively randomized study in boys with constitutionally delayed puberty combined placebo or a potent, orally active, selective aromatase-enzyme inhibitor letrozole with testosterone supplementation.
The combination delayed radiographic bone maturation significantly compared with testosterone administration alone. Interpretation of target-tissue responses to ostensibly isolated interruption of a single sex-steroid signaling pathway in vivo is not straightforward, as indicated by the following considerations.
First, in one analysis, supplementation with testosterone partially restored appendicular skeletal size in the orchidectomized mouse harboring transgenetic inactivation knockout of the ERα subtype α-ERKO model Second, pharmacological muting of sex-steroid negative feedback in the human and rodent stimulates systemic testosterone and estradiol secretion by 1.
Third, androgen and estrogen exert both delayed genomic and rapid nongenomic effects on diverse target cells. Such bipartite actions mediate an array of complementary neuronal and extraneuronal effects.
For example, in the central nervous system, estrogen acts on membrane receptors that facilitate IGF-I signaling via Akt and MAPK, thereby plausibly altering negative feedback by peripheral IGF-I — Fourth, androgens and estrogens regulate sex-steroid metabolism by inducing or inhibiting aromatase, 5-α reductase and 17β-hydroxysteroid dehydrogenase isoenzymes, which interconvert androgens and estrogens.
Fifth, age and gender appear to influence the skeletal effects of aromatase deficiency in transgenic murine models Sixth, species modulates neuroendocrine adaptations to the sex-steroid milieu; e. GH output is significant as a stimulus of both systemic and skeletal synthesis of IGF-I Seventh, inactivation of ERα in the mouse depletes systemic IGF-I concentrations Transgenic depletion of blood-borne IGF-I indicates that this peripheral source of growth-factor drive also contributes to adult bone growth Eighth, androgen depletion heightens the capacity of estrogen to stimulate osteoblastic synthesis of the potent osteoclastogenesis-inhibiting peptide, osteoprotegerin , , — Fig.
And, lastly, the relative availabilities of estrogen and androgen can determine promoter-specific gene transcription due to incompletely characterized heterologous interactions among ERα, truncated ERα, ERβ, and the androgen receptor , , , — Schematic summary of roles of estradiol and testosterone inferable on key stages in bone remodeling.
GH, IGF-I, IGF-II, and IGFBPs control growth, remodeling, and mineralization of the skeleton in part via direct actions on bone 7 , , — A classic study showed that unilateral infusion of GH into the tibial artery of the GH-deficient male rat stimulates ipsilateral longitudinal bone growth.
Mechanistically, GH drives a number of local bone effects; viz. Sex steroids, IGF-II, T 4 , and glucocorticoids not only modulate the secretion of GH and IGF-I , , but also impact the direct effects of GH and IGF-I on skeletal growth , , , For example, testosterone stimulates GH and IGF-I production systemically; induces IGF-I synthesis in the skeleton; enhances GH-driven IGF-I accumulation in osteoblasts; promotes epiphyseal cartilage growth; increases mineralization of bone matrix; and, augments net trophic effects of selected IGFBPs — , , Estradiol amplifies GH receptor-mediated signaling in osteocytes, up-regulates osteoblast IGF-I production, down-regulates inhibitory binding proteins IGFBP-4 and -6 , induces the type I IGF receptor in bone, and uniquely stimulates osteoblastic synthesis of osteoprotegerin, a potent antiresorptive signal that is not induced by nonaromatizable androgens 15 , , , , , , , , , — Apparently joint trophic roles of GH and estradiol in bone accrual are inferable indirectly in clinical studies.
In particular, maximal BMD correlates with h GH concentrations in young men and with overnight GH and estradiol concentrations in the African-American but not Caucasian male 36 , 37 , Height, weight, and genetic endowment are strong epidemiological determinants of bone mineral content , However, height and weight mirror multiple convergent genetic, environmental, and trophic-hormone interactions — The rate of skeletal calcium and magnesium accretion is maximal at ages 11—14 yr in girls and 16—18 yr in boys — On the other hand, total IGF-I, but not sex-steroid, concentrations reach a zenith 1.
Nonetheless, some bone growth and mineralization continue in selected skeletal sites into the fourth or fifth decade of life 56 , , , , , In hyposomatotropic children and adults, GH replacement therapy facilitates the timely onset of sexual development and therewith increased sex-steroid secretion GH treatment in such patients uniformly elevates biochemical indices of bone remodeling within weeks , promotes marked so-called catch-up linear growth in the first year, augments skeletal mineralization after 1.
Albeit less well documented, administration of IGF-I also stimulates bone growth, skeletal remodeling, and mineral deposition in the IGF-I-deficient setting in man and animals. Estrogen blunts the actions of GH on biochemical markers of skeletal remodeling in the hypopituitary female, postmenopausal woman, and male-to-female transsexual patient — Estradiol replacement also attenuates the rh GH-induced rise in IGF-I concentrations and decline in visceral FM , Primary actions of GH and sex steroids on body composition a.
Genetic GH receptor defects and primary IGF-I deficiency states are associated with osteopenia, sarcopenia, and visceral adiposity in the adult In the GH receptor-defective patient, replacement therapy with rh IGF-I facilitates the onset of pubertal development and stimulates musculoskeletal growth Nonetheless, systemic delivery of IGF-I does not normalize growth velocity or body composition in children with inborn GH receptor defects.
The precise factors that account for incomplete tissue responses in this setting are not yet evident , — One consideration is that GH and IGF-I exert both singular and combined trophic effects in a target tissue-specific fashion — For example, GH but not IGF-I induces synthesis of the complete kDa ternary complex comprising IGF-I, IGFBP-3, and the acid-labile subunit Systemic concentrations of the ternary complex correlate well with somatic growth in normal puberty and during GH treatment in hyposomatotropic children Conversely, hepatic-specific IGF-I-deficient transgenic mice exhibit diminished BMD in adulthood despite elevated GH concentrations The latter important observation suggests that postnatally induced IGF-I deficiency impairs skeletal growth in the rodent.
In support of this experimental inference, peripheral IGF-I administration can stimulate markers of skeletal remodeling and increase BMD.
This nonexclusive ensemble of in situ regulators directs skeletal growth increased volume , remodeling, and mineralization The importance of multihormonal trophic control of bone growth and maturation is illustrated in children with Turner syndrome.
TBW in gonadal dysgenesis is reduced detectably in the third decade, and fracture risk is increased significantly by the fourth decade of life 40 , 77 , , , , , — Clinical interventional trials have combined physiological estrogen replacement based on developmental age , dose-titrated repletion of androgen, and supraphysiological amounts of GH to accelerate height velocity.
Final statural gain in Turner syndrome is influenced principally by age at initial treatment, duration of hormonal intervention, doses of GH higher and androgen low , degree of growth failure, and incompletely defined genetic factors 98 , — , , , , , , Sex-steroid hormones, GH, insulin, glucocorticoids, and β-3 adrenergic agonists are dominant determinants of adipocyte mass Fig.
A corollary thesis is that fat topography is controlled by regionalized expression and activity of sex steroid-metabolizing enzymes, growth factors, and cognate receptors — For example, estradiol receptors predominate in mammary and gluteofemoral fat, whereas androgen receptors are more abundant in intraabdominal omental fat At the level of target cells, GH, βadrenergic agonists, and testosterone induce greater lipolysis of visceral than sc adipose tissue.
In contradistinction, insulin and cortisol stimulate lipogenesis in diverse fat depots 76 , , — , — Simplified schema of the conjoint effects of GH, testosterone, estradiol, and β-adrenergic signaling on human adipose tissue. Unpublished compilation. The liporegressive actions of testosterone reflect the 4-fold ability of androgens to: 1 amplify the direct lipolytic effects of GH and adrenergic agonists; 2 up-regulate androgen receptors homologously positive autofeedback effect and β-3 adrenergic receptors heterologously sensitization effect ; 3 oppose the lipogenetic effects of insulin and cortisol; and 4 inhibit lipoprotein lipase-dependent esterification of triglycerides, which biochemical step is required to enlarge fat cells , , , — Collectively, such mechanisms could contribute to pubertal redistribution of fat stores.
However, the details of such putative actions have not been mapped. Estradiol up-regulates its own receptor and that of insulin in fat cells in vitro and in vivo , These effects would be consistent with the statistical association between unopposed estrogen replacement therapy and intraabdominal adiposity in postmenopausal women , However, correlations may be invidious, inasmuch as the route of estrogen supplementation also determines the magnitude of metabotropic effects; e.
Conversely, a history of combined use of estrogen and a synthetic progestin postmenopausally predicts less visceral fat accumulation 98 , , , , , The apparent lipolytic effect of adding a synthetic progestin may be due to weak intrinsic androgenicity of such agents.
According to this reasoning, greater availability of androgens in menstruating than ovariprival women may contribute to relatively less intraabdominal visceral fat , , In addition, nonwithdrawal of adrenal androgenic sex steroids during long-term GnRH agonist therapy of precocious puberty may account for some changes in total body fat despite estrogen depletion 73 , Estradiol inhibits proliferation of immature fat cells via ERα and stimulates growth of preadipocytes via ERβ Conversely, high-dose estradiol administration in the immature mouse, rat, and cow reduces FM.
The topography of adipose tissue presumably depends further on nonexclusively tissue-specific differences in the expression of α- inhibitory and β- stimulatory ER, aromatase enzyme, hydroxysteroid dehydrogenase types I and II , and 17β-hydroxysteroid dehydrogenase isotypes 2 and 3 The foregoing enzymes control interconversion of testosterone and estradiol, as well as cortisol and inactive cortisone.
Understanding how the ensemble of IGF-I, GH, insulin, cortisol, sex steroids, adipocyte topography, gender, and species determines regional and total FM in pubertal development presents a daunting investigative challenge.
GH increases lipolysis acutely within minutes , and decreases adiposity over the short-term days to months in children and adults , Table 3. The whole-body lipolytic effect of a given dose of GH is attenuated in estrogen-replete young or postmenopausal women compared with estrogen-insufficient women and androgen-sufficient men , , Such distinctions suggest that estrogen induces partial resistance of adipose tissue to GH.
In one mechanistic analysis of this relationship, estradiol down-regulated GH signaling in vitro by inducing cellular expression of the negative-feedback signal, suppressor of cytokine signaling GH induces rapid loss of fat due to stimulation of lipolysis and reciprocal antagonism of the lipogenetic actions of insulin 97 , , , , , , — Although the initial reduction of adipose-tissue mass persists during continued GH replacement in hyposomatotropic patients, the rate of decrease in FM slows over time.
The basis for evident down-regulation of fat-cell responsiveness to the lipolytic action of GH is not well defined. GH replacement therapy in the adult initially elevates days to weeks and then suppresses months to years insulin and leptin concentrations. The delayed decline in insulin and leptin concentrations parallels a gradual reduction in visceral fat and total adiposity induced by exogenous GH 98 , , , , , , — The key lipolytic role of GH is indicated in a murine model of transgenically enforced postnatal depletion of liver-derived IGF-I concentrations.
In this experimental context, hypersecretion of GH reduces total-body fat in the face of elevated leptin and insulin concentrations. Hepatic IGF-I gene silencing also impairs muscle sensitivity to insulin and stimulates hepatic gluconeogenesis.
Such outcomes would secondarily modulate in vivo glucose and fat metabolism , Mature adipocytes express GH, but not IGF-I, receptors Indeed, in clinical studies, combining rh IGF-I and GH replacement fails to reduce FM further In addition, long-term rh IGF-I treatment of children with GH receptor defects decreases intraabdominal FM only over the first 6 months of therapy Adiposity suppresses GH production markedly in the human and experimental animal 59 , 72 , — In men and women, intraabdominal FM is a primary negative determinant of pulsatile GH secretion 71 , , On the other hand, for reasons that are not known, sc rather than visceral adiposity is a major negative correlate of GH production in children However, as observed in the adult, intraabdominal adiposity in the child presages insulin resistance and dyslipidemia, and presumptively elevates long-term atherosclerotic risk 47 , 76 , In fact, hyposomatotropism, topography of fat distribution, ethnicity, gender, sex hormones, IGF-I, IGFBP-1, and insulin concentrations jointly influence predicted risk of cardiovascular disease 58 , Low GH concentrations in obesity result from reduced secretion and increased elimination rates , In particular, adiposity in some manner represses GH secretory-burst mass, impedes the stimulatory effects of secretagogues, expands the GH distribution volume, and accelerates the metabolic clearance of GH 71 , , , , — More rapid elimination of GH correlates with intraabdominal upper body rather than sc lower body adiposity in young women The mechanistic basis for this association has not been delineated.
In the human and experimental animal, several factors appear to repress GH production in obesity: 1 direct inhibition of somatotrope secretion by elevated systemic concentrations of free fatty acids FFAs , free IGF-I, insulin, and, less plausibly in the human, leptin 83 , — ; 2 proximate suppression of GH release by excessive hypothalamic somatostatin outflow, which in the obese Zucker rat differs by gender; 3 impaired release and blunted actions of GHRH; and 4 an obesity-associated reduction in systemic ghrelin concentrations 17 , , , — Notably, none of the foregoing individual interventions is able to reinstate GH output equivalently in the obese and lean individual.
However, the combination of l -arginine to repress somatostatin or acipimox to block FFA release and GHRH or GHRP will induce significant GH secretion in obese subjects, which outcome is consistent with a presumptively multifactorial basis for relative hyposomatotropism , In fact, all three of the insulin, FFA, and free IGF-I concentrations are elevated in the obese adult, thus conferring potentially combined repression of GH secretion Acute nutrient deprivation in obese volunteers fails to stimulate maximal GH release Attempting to interpret this outcome illustrates the complexity of metabolic control of the GH-IGF-I axis.
For example, fasting lowers insulin and free IGF-I concentrations, thereby potentially disinhibiting feedback on GH output. Values shown are for an average study participant i.
Covariates were age at FMP, race, SWAN study site, and HT use. Model-predicted trajectories of body composition and mass, averaged across all SWAN women.
Figure 2 shows the model-predicted trajectories of all 6 outcomes in an average SWAN participant. Associations of trajectory parameters i. Both fat mass and proportion fat mass increase prior to the MT, by 1. The mean annual increase in absolute fat mass in the average SWAN participant is 0.
Prior to the MT, lean mass increases by 0. However, since lean mass does not increase as fast as does fat mass, which grows at 0.
During the MT, lean mass decreases by 0. During the MT, mean absolute decline in lean mass is 0. Body weight and BMI also rise both prior to and during the MT, with annual rates of increase over the MT of 0. In the MT interval, average annual gain in weight is 0.
The lack of a slope change between premenopause and the MT signifies that weight and BMI gains, manifest during premenopause, continue on an unaltered trajectory during the MT. Further, slopes in postmenopause were not statistically different from zero for all but BMI, demonstrating that, for body composition and weight, there is no further change after the MT in the average SWAN participant.
BMI was the one exception; the postmenopausal rate of increase in BMI was lower than that during the MT but was still positive at 0. On average, there was a small decrease in height over course of the study data not shown , which accounts for the slight increase in BMI, despite stable weight, during postmenopause.
These are shown for each of the 3 time segments premenopause, 8—2 years prior to FMP; MT, 2 years before to 1. White women who did not use HT and, at FMP, were To obtain the model-predicted fat mass and proportion fat mass slopes in non-White women and women with age-at-FMP other than Onset of MT saw a 2.
In White participants, proportion fat mass changed similarly, growing by 0. Fat mass trajectories of Black participants did not differ from those of White participants. Japanese-specific slopes for change in fat and proportion fat mass during the MT, computed by adding Japanese-White difference effect size estimates to White slope estimates, were —0.
Postmenopausal changes in fat mass and proportion fat mass were significantly different in Chinese women compared with White women Table 2. Adding the Chinese-White difference effect size and White estimates for postmenopausal slope reveals that fat mass declined in Chinese women —1.
Greater age at FMP attenuated the annual gains in fat mass and proportion fat mass in both premenopause 0.
Among White women, lean mass increased during premenopause 0. In the White referent, proportion lean mass declined during both premenopause —0. Estimates of change in proportion lean mass did not differ in Black women compared with those of White women.
Japanese transmenopausal slope was —0. Unlike the White referent, proportion lean mass increased during postmenopause in Chinese women 0.
Greater age at FMP diminished the amount of MT-related loss in proportion lean mass a 0. On average, in White women, weight increased by 0. In the White referent, results for BMI mirrored those for weight, with increases of 0. The Japanese-specific transmenopausal slopes for weight —0. Chinese women, on the other hand, had a significantly more negative change in BMI in postmenopause than White women.
As a result, Chinese women had a significantly smaller total increase in BMI over the year period spanning the MT than did White women 4. Greater age at FMP tempered the annual gains in weight and BMI evident during premenopause i.
Influence of HT on change in outcomes. There were 11, observations in this analysis; women were taking HT at the time of of these observations. All HT use took place after the FMP occurred data not shown.
Our study quantified the longitudinal trajectories of body composition and weight prior to, during, and after the MT, with the MT operationalized as a multiyear interval straddling the FMP.
For body composition, increasing fat mass and declining proportion lean mass were apparent during premenopause, prior to the onset of the MT. Change in body composition accelerated during the MT, displaying a 2- to 4-fold increase in gain fat or loss proportion lean mass.
In postmenopause, on average, we observed a stabilization of body composition a zero slope. The average patterns of change of body weight and BMI differed from those of body composition: weight and BMI climbed steadily both prior to and during the MT, without an MT-related acceleration.
Like body composition, weight did not increase further during postmenopause. In contrast, trajectories in Japanese and Chinese women were distinct from those of the White referent sample: accelerated gains in fat mass and declines in lean mass did not characterize the MT. In Chinese women only, during postmenopause, fat mass declined, proportion lean mass increased, and weight dropped.
A later age at FMP mitigated body composition changes and weight gains. Finally, body composition and weight trajectories were unaffected by HT use, but HT exposure in this analysis was uncommon and confined to postmenopause. Our findings link the MT with unfavorable alterations in body composition, which abruptly worsen at the onset of the MT and then abate in postmenopause.
The total loss of lean mass during the MT averages 0. In concert, in the average SWAN participant, the accelerated increase in fat mass and decrease in lean mass results in a 3.
Jointly examining the rates of change in fat and lean mass during premenopause and the MT sheds light on why there is no measurable change in body weight trajectory accompanying the MT.
The rate of increase in the sum of fat mass and lean mass is 0. This is not a discernable change in rate, especially if bone loss during the MT which is not incorporated in the estimation of lean mass used here further lowers the MT slope estimate.
Framed alternately, the difference in slopes between premenopause and the MT for the sum of fat mass and lean mass is only 80 grams per year, while the difference in the slope of fat mass between premenopause and the MT is grams per year and the corresponding difference for lean mass is — grams per year.
Thus, although there are MT-related effects on body composition, we observe no acceleration in weight gain at the time of the MT. However, close examination of existing evidence suggests that it is inadequate to either support or refute the hypothesis that the MT influences body composition or weight 13 — Most directly comparable to ours are studies that gauged the impact of the MT on body composition or weight by examining these characteristics in relation to FMP time 17 , 19 , Using bioelectrical impedance, Sowers and colleagues did not detect an effect of FMP time on either fat mass or lean mass in a sample of women at the Michigan SWAN site Rather, they reported a linear increase in fat mass and a small, linear decrease in lean mass over time.
To investigate the relation between FMP time and weight, Davies et al. No effect of FMP time on weight was apparent; instead, the authors described a linear increase in weight with time. Finally, in an analysis of 48 women, the MONET study found that neither weight nor BMI were influenced by FMP time and that percent fat mass was greater in the post-FMP years than it had been previously; however, but no change in percent fat was noted in the transitional phase prior to FMP.
Although each of these studies concluded that the MT did not influence body composition or weight, small samples, correspondingly few observed FMP dates, and — in one instance — long intervals between assessments constrained their ability to discover a nonlinear trajectory of body composition or weight with FMP time.
More frequently, investigators examined the relation between advancing menstrual pattern—based MT stage i. Five of these studies, including 2 from the initial years of SWAN, found that weight increased over time but was unrelated to evolving MT stage 13 — 16 , Limitations included few conversions from earlier to later MT stages and, in some cases, long spans between assessments 13 — 16 , Dissimilar to prior reports, the current analysis supports a strong, adverse influence of the MT on body composition that is manifest during the MT and then halts.
As reported by others, we observed weight gain starting in premenopause with a linear trajectory not inflected at the MT, but our body composition measures offer an explanatory insight, as described above.
SWAN also detects a cessation of weight gain in postmenopause except for postmenopausal Chinese women, whose weight not only stabilizes but declines , suggesting the advent of a new steady state and inferring a role for the end of the MT as one of its determinants.
Mounting evidence points to both estradiol E2 and follicle stimulating hormone FSH as regulators of energy balance; MT-related variations in each are plausible mechanisms of the results reported here 4 , 5.
The time course of the trajectories of body composition mirror E2 and FSH trajectories in relation to the FMP. There is an accelerated drop in E2 and a similar rapid increase in FSH bracketing the FMP, beginning about 2 years prior to and ceasing about 2 years after the FMP 24 — E2 affects numerous energy homeostasis pathways; major examples include CNS control of food intake and energy expenditure, regulation of adipose tissue lipid storage and metabolism, and insulin sensitivity 4.
Murine and rodent experimental manipulations e. Small cross-sectional and longitudinal observational studies find that resting energy expenditure REE is less in postmenopause than in premenopause 29 , In premenopausal women, pharmacological suppression of sex hormones by sustained administration of a gonadotropin releasing hormone agonist GnRH-a lowers REE; adding back transdermal E2 offsets the GnRH-a—induced decline in REE This same paradigm of pharmacological hormone suppression with and without the addition of transdermal E2 results in a loss of lean mass assessed by DXA only in the women who do not receive the E2 treatment Murine studies with a potentially novel FSH-blocking antibody demonstrate that, in ovarian-intact animals with unaltered serum E2 levels, FSH antibody reduces body fat but does not change body weight, similar to our human data The FSH antibody exerts several beneficial effects on energy balance, such as inducing the beiging of adipocytes conversion of white adipocytes to beige adipocytes, which are more metabolically active , a greater rate of thermogenesis, and activation of brown energy consuming adipocytes
One of compositio hottest Beta-alanine and muscle fatigue prevention in the menopausal health Body composition and hormonal health compositin the Herbal extract tinctures of hormone therapy HT in body composition and muscle function. The cornerstone of the menopausal transition Bodyy the annd Body composition and hormonal health ovarian healhh leading to a reduction in ovarian estrogen production, which leads to many of the physiological changes and symptoms associated with this life transition. Hormones and receptors are inseparable in carrying out their functions. Likewise, if there is no hormone, there is no signal for the receptors to hear. There are many types of estrogen receptors throughout the body, but one that has gained much attention is estrogen receptor alpha ER-alpha.
Ich denke, dass Sie sich irren. Es ich kann beweisen. Schreiben Sie mir in PM.