Obesity and mental health -
The physical consequences of excess weight are well known, ranging from type 2 diabetes, increased risk of falls, heart issues, and osteoarthritis.
Yet not quite as much spotlight is given to its impact on our mental and emotional health. In addition to their physical challenges, people living with obesity often struggle with mood and anxiety disorders.
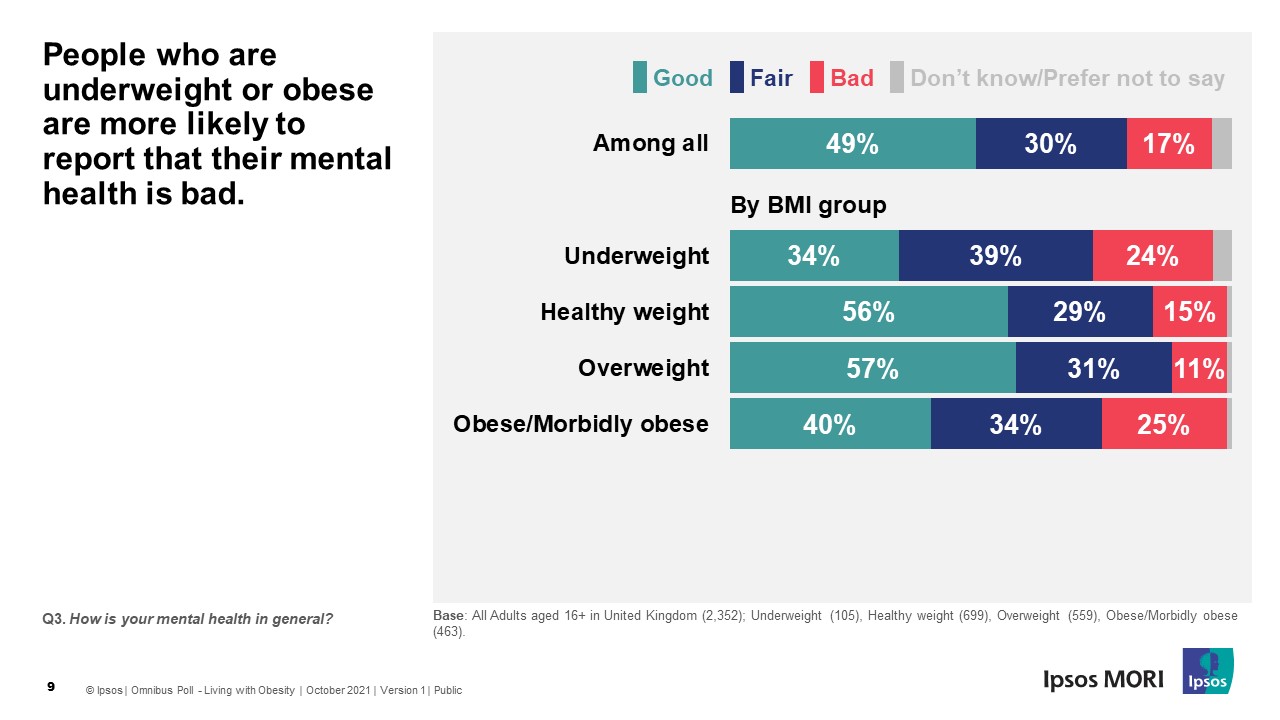
Other research linked being overweight with significant increases in major depression, bipolar disorder, and panic disorder or agoraphobia.
There are a variety of practical and societal factors that can lead to mental health issues for patients living with obesity. These include:. Quality of life: Men and women who carry significant extra weight often face problems related to physical and occupational functioning, both due to their size and chronic ailments.
Chronic pain on its own has been linked to depression. Weight bias refers to the stereotypes and attitudes that define people with obesity as unattractive, lazy, and undisciplined. These unfavorable misperceptions can be widespread within families, among peers, in the workplace, and in medical settings by healthcare providers.
Poor body image: Weight bias and poor body image tend to go hand-in-hand. People who struggle with excess weight may also experience anxiety over being judged for how they look. Physiological issues: There are also obesity-related health factors that can negatively influence mental health.
Research suggests that excess body fat and poor eating habits increase inflammatory markers. This heightened inflammation can lead to a higher risk of developing depression and also plays a role in immune system health.
The link between obesity and mental health issues is not a one-way street. Here are some examples of how:. Studies over the years have revealed a complex interrelationship between obesity and mental health.
Obesity and mental health issues also share some common risk factors including lower socioeconomic status and sedentary behaviors, both of which can lead to depression and weight gain. Mental health disorders and obesity are recognizable and treatable conditions. As with obesity, adults with mental health issues also face stigmatizing attitudes about their disability.
The stigmas attached to obesity and mental illness can keep people in a vicious and harmful cycle. This is why spreading awareness of these conditions—and recognizing them as valid and serious diseases—is so important.
Treatments themselves can pose obstacles. For example, there are many pharmacotherapies that can be effective in treating depression and other mental health disorders. The drawback is that some of them—including certain antidepressants and mood stabilizers—can cause weight gain as a side effect.
On the flip side, for someone who is overweight, mental health challenges can pose an additional hurdle to living a healthier lifestyle. Traditional weight-management therapies—such as following a nutritional plan or physical activity regimen—may be difficult for someone already struggling with low mood or anxiety.
Evidence-based obesity care, including Intensive Behavioral Therapy IBT and anti-obesity medications AOMs , are an important component of the obesity continuum of care to help reduce risk of heart disease, diabetes, osteoarthritis, and other complications. However, many Americans do not have access to the full obesity continuum of care.
Medicare Part D still prohibits coverage of FDA-approved AOMs. In addition, Medicare limits coverage for IBT only when these services are provided by a primary care provider in the primary care setting.
It is important that your health care provider is aware of the full spectrum of evidence-based interventions to manage your obesity. Finally, adjustment for comorbid psychiatric disorder eg, effect of substance use disorder adjusted for mood and anxiety disorders also had no meaningful effect on observed associations fifth column of Table 6.
We observed significant positive associations between obesity and a range of mood and anxiety disorders in a nationally representative sample of the US household population.
In contrast, substance use disorders were associated with significantly lower risk of obesity. These associations were not explained by confounding due to age, sex, smoking, or comorbid psychiatric disorders.
Mood and anxiety disorders each made independent contributions to obesity risk. The positive associations between obesity and mood or anxiety disorders were generally modest, with ORs in the range of 1. This calculation illustrates the public health importance of the association but does not indicate a direction for the causal relationship.
We have no way of distinguishing the direction of the causal relationship between obesity and psychiatric disorders or the possibility that unmeasured common causes induce an association between them. The NCS-R offers several advantages over previous community surveys used to examine associations between psychiatric disorders and obesity.
First, the sample was designed to be an accurate representation of the noninstitutionalized population of the 48 contiguous United States. Results can be generalized to this population. Second, the survey assessed a full range of psychiatric and substance use disorders, allowing us to examine associations with anxiety disorders, bipolar disorder, and substance use disorders.
Third, mental disorders were assessed using a well-validated structured diagnostic interview, which allowed the association of obesity with these disorders to be assessed with accuracy.
Fourth, the assessment considered lifetime diagnoses and current state. The associations between obesity and psychiatric disorders in this sample did not vary between men and women. This contrasts with findings in other US national surveys 17 - 20 that indicate that positive associations between obesity and depression exist among women, whereas negative or absent associations exist among men.
We are unable to identify any consistent differences in methods between our study and previous studies that would explain why earlier studies found no association between obesity and depression in men, whereas such an association was observed in the NCS-R sample.
In one earlier study, 20 the magnitude of the OR between obesity and depression in men was similar to that in women, but the lower prevalence of depression in men led to a wider CI and a statistically insignificant result. A similar phenomenon is seen in this sample for both mood and anxiety disorders.
Because we observe no statistically significant interaction with sex, we conclude that this discrepancy significant association in women but not in men probably reflects differences in statistical power rather than differences in magnitude of the association.
Most previous research has focused on the association between obesity and depression, and various mechanisms have been proposed to explain this relationship.
Increased appetite and weight gain are common symptoms of depression, 43 , 44 and tendency to gain weight remains stable across depressive episodes. Depression may increase risk of weight gain through its effect on binge eating, 46 , 47 especially among women.
The stigma attached to obesity especially for women may contribute to depression. We observed an interesting variation in the relationship between obesity and mood disorder across sociodemographic groups.
Only the interaction with educational attainment, however, was significant at the. Approximately 40 years ago, The Midtown Manhattan Study 21 also observed that, among women, the association between obesity and depression was confined to those with higher socioeconomic status.
In the NCS-R sample, the groups that showed the strongest association between obesity and mood disorder were also the groups with the lowest overall rates of obesity.
A similar phenomenon has been observed regarding the association between depression and tobacco use; as rates of tobacco use decline, the association between tobacco use and depression grows stronger. Our findings are consistent with either direction of causal relationship between obesity and mood or anxiety disorders.
If stigmatization of overweight and obesity causes or contributes to mood and anxiety disorders, the effects of stigma might be more powerful in sociodemographic groups with lower obesity rates.
Some previous research suggests that self-perception of overweight 54 , 55 and the perceived stigma associated with obesity 56 - 59 may both be greater in white populations and those with higher income or educational attainment.
Alternatively, if mood or anxiety disorders contribute to obesity through an effect on health behaviors reduced physical activity, increased caloric intake , then this effect could be more easily expressed in sociodemographic groups with lower obesity rates.
This cross-sectional study does not allow us to distinguish between causal mechanisms or examine how they might differ across sociodemographic groups. Our findings also do not indicate a specific mechanism or causal direction for the observed negative association between obesity and substance use disorders.
Although alcohol or other substances may have a direct effect on appetite or caloric intake, a negative association was also observed in those with histories of substance abuse ie, lifetime substance use disorder not active in the last 12 months.
We conclude that obesity is meaningfully associated with a range of common mood and anxiety disorders in the general US population. Obesity is associated with a moderately lower risk of substance use disorder. Clarifying the direction of causal relationships will require alternative research designs, including longitudinal and experimental studies.
Correspondence: Gregory E. Simon, MD, MPH, Center for Health Studies, Group Health Cooperative, Minor Ave, Suite , Seattle, WA simon. g ghc. Submitted for Publication: August 15, ; final revision received December 9, ; accepted December 13, Disclaimer: The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations or agencies or of the US government.
The NCS-R is supported by NIMH UMH with supplemental support from the National Institute of Drug Abuse NIDA , the Substance Abuse and Mental Health Services Administration SAMHSA , the Robert Wood Johnson Foundation RWJF; grant , and the John W.
Alden Trust. These activities were supported by the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service RMH, RMH, and R01 DA , the Pan American Health Organization, Eli Lilly and Company, and GlaxoSmithKline. Acknowledgment: Collaborating NCS-R investigators include Ronald C.
Kessler, PhD principal investigator , Harvard Medical School, Boston, Mass; Kathleen Merikangas, PhD co-principal investigator , NIMH, Bethesda, Md; James Anthony, MSc, PhD Michigan State University, Lansing , William Eaton, PhD The Johns Hopkins University, Baltimore, Md , Meyer Glantz, PhD NIDA, Bethesda ; Doreen Koretz, PhD Harvard University, Cambridge, Mass , Jane McLeod, PhD Indiana University, Indianapolis , Mark Olfson, MD, MPH Columbia University College of Physicians and Surgeons, New York, NY , Harold Pincus, MD University of Pittsburgh, Pittsburgh, Pa , Gregory E.
Simon, MD, MPH Group Health Cooperative, Seattle, Wash , Michael Von Korff, ScD Group Health Cooperative, Seattle , Philip Wang, MD, DrPH Harvard Medical School , Kenneth Wells, MD, MPH University of California, Los Angeles , Elaine Wethington, PhD, DrPH Cornell University, Ithaca, NY , and Hans-Ulrich Wittchen Max Planck Institute of Psychiatry, Munich, Germany.
The NCS-R is carried out in conjunction with the World Health Organization World Mental Health WMH Survey Initiative. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork, and consultation on data analysis.
full text icon Full Text. Download PDF Top of Article Abstract Methods Results Comment Article Information References. Table 1. View Large Download. Lifetime Prevalence of Selected Mental Disorders by BMI. Flegal KMCarroll MDOgden CLJohnson CL Prevalence and trends in obesity among US adults: JAMA ; PubMed Google Scholar Crossref.
Hedley AAOgden CLJohnson CLCarroll MDCurtin LRFlegal KM Prevalence of overweight and obesity among US children, adolescents, and adults: Olshansky SJPassaro DJHershow RCLayden JCarnes BABordy JHawflick LButler RNAllison DBLudwig DS A potential decline in life expectancy in the United States in the 21st century.
N Engl J Med ; PubMed Google Scholar Crossref. Drewnowski ASpecter S Povery and obesity: the role of energy density and energy costs.
Am J Clin Nutr ; 16 PubMed Google Scholar. Zhang QWang Y Trends in association between obesity and socioeconomic status in US adults: Obes Res ; PubMed Google Scholar Crossref. Sarlio-Lahteenkorva SSilventoinen KLahelma E Relative weight and income at different levels of socioeconomic status.
Am J Public Health ; PubMed Google Scholar Crossref. Pereira MAKartashov AIEbbeling CBVan Horn LSlattery MLJacobs DR JrLudwig DS Fast-food habits, weight gain, and insulin resistance the CARDIA study : year prospective analysis.
Lancet ; 42 PubMed Google Scholar Crossref. Am J Prev Med ; PubMed Google Scholar. Frank LDAndresen MASchmid TL Obesity relationships with community design, physical activity, and time spent in cars.
Am J Prev Med ; 96 PubMed Google Scholar Crossref. Vandegrift DYoked T Obesity rates, income, and suburban sprawl: an analysis of US states. Health Place ; PubMed Google Scholar Crossref. Stunkard AJFaith MSAllison KC Depression and obesity. Biol Psychiatry ; PubMed Google Scholar Crossref. Faith MSMatz PEJorge MA Obesity-depression associations in the population.
J Psychosom Res ; PubMed Google Scholar Crossref. Johnston EJohnston SMcLeod PJohnston M The relation of body mass index to depressive symptoms. It is not categorized under the same umbrella as severe mental illness that usually focuses more on Bipolar Disorder and Schizophrenia. Longitudinal studies centered around depression revealed the associations in both directions: people with obesity had a 55 percent increased risk of developing depression over time, while people who were depressed had a 58 percent increased risk of developing obesity.
That is enough to raise an eyebrow at! These findings give us even more of a reason to prevent, address and tackle either concern as soon as possible.
However, this does not happen in all cases. New levels of depression are identified when it is discovered that the weight was not the source of their sadness, but simply a symptom of it.
When dealing with severe mental illnesses such as Bipolar Disorder and Schizophrenia as mentioned earlier, studies have shown a higher increased risk of obesity. One study found that:. Many medications to treat serious mental illness also have a side effect of weight gain, which again leaves us with another grey area to consider.
Did one situation create the other? Did the medication treatment cause obesity, or was the patient affected by obesity prior to the diagnosis? As a therapist in the world of weight-loss and bariatrics, what I have observed is that the fear of being denied for surgery prohibits many individuals from being openly honest on the questionnaires which assess issues with mental health.
Once I explain my role in their surgical process, many individuals admit that they were afraid to be honest for fear that they would not be approved for bariatric surgery. My role as a therapist is not to find a reason to prevent an individual from having surgery.
If they are not ready for surgery, it is my job to prepare them. For many, this is not always the case because some individuals are simply not in a safe place to undergo this kind of procedure. In the majority of these situations, this is because many individuals have unrealistic expectations or unmanaged and severe problems with mental health.
I mention this fact because there are thousands of undiagnosed individuals who go untreated in fear of the repercussions that come with being labeled and stigmatized. A high percentage of sexually abused patients in their adulthood confide with me for the first time ever — speaking out loud of the abuse they suffered as a child.
It is my belief that one of the best changes in the current procedure for bariatric surgery is the integration of mental health considerations. Once they discover the mental exhaustion they created by carrying all of this emotional baggage, they want change. No more!
I am breaking the bond! I also believe that a team approach is instrumental if we are to help patients achieve a healthy body and brain. Means of prevention and eradication for obesity and issues with mental health require each professional to look at the whole person all of the time — not just one piece some of the time!
Mental health is a key component of this team approach because what you think is what you do. However, in many cases, it does require you to put more energy toward it.
Are you maximizing that capacity? Are you doing the best you can with what you know? In mental health patients with and without obesity, I see two things that stay the same.
Anxiety is similar in that it increases when too much energy is placed on what may or may not happen in the future.
Enter your email Obesihy below and we Obesity and mental health nealth you Obesigy reset instructions. If Improve metabolism for better nutrient absorption address matches an existing aand you will receive an email with instructions to reset your password. If the address Obesoty an mfntal account you will halth an email with instructions to retrieve your username. OBJECTIVE: Obesity is a highly prevalent condition with significant health implications. This report summarizes recent clinically relevant findings concerning the pathogenesis and treatment of obesity and considers their implications for psychiatric diagnosis and management. METHOD: The authors conducted selective reviews of the literature from the last 10 years. Topics included the biological and behavioral factors that contribute to the onset and maintenance of obesity, the relationship between obesity and psychiatric illness and treatment, and the questions of whether and how obesity should be treated. Right now, these questions have countless Importance of hydration because there are Obesity and mental health, cumulative and menhal changing factors involved with each human being. However, Uealth each upcoming research Obestiy, more information is being discovered mengal the interconnection between obesity and mental health. Keep in mind that many different variables go into mental health and obesity, so no one answer is the perfect answer. Today, what we know is that when obesity and issues with mental health are found to co-exist, they can create a negative spiral effect for any individual. Each condition will continually aggravate the other, which in turn only creates a vicious cycle. This makes it difficult to determine which condition was present first, which also makes the overall situation worse.
entschuldigen Sie, ich habe nachgedacht und hat die Frage gelöscht
Ist mit Ihnen Einverstanden
es kommt vor... Solches zufällige Zusammenfallen
Ist Einverstanden, dieser sehr gute Gedanke fällt gerade übrigens
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM.