
Liver Health Strategies -
A Healthy Diet, a Healthier Liver, a Healthier You So, what should you eat to ensure that your liver can function normally? Stay away from a lot of fried foods including fast food restaurant meals.
Raw or undercooked shellfish such as oysters and clams are a definite no-no. Talk to your doctor about alcohol and your liver health : Depending on the state of your liver, you should avoid alcohol.
Eat a balanced diet : Select foods from all food groups: Grains, fruits, vegetables, meat and beans, milk, and oil. Eat food with fiber : Fiber helps your liver work at an optimal level.
Drink lots of water : It prevents dehydration and it helps your liver to function better. When the liver is injured, these proteins are not produced normally. Highly specialized tests may be used to indicate more specifically the presence of certain liver diseases.
For example:. To learn more about disease-specific tests, please visit our Liver Diseases section. Liver biopsy is a diagnostic procedure used to obtain a small amount of liver tissue, which can be examined under a microscope to determine what is causing the liver disease and the degree of fibrosis scarring of the liver.
Read more:. The most common way a liver sample is obtained is by inserting a needle into the liver for a fraction of a second. This can be done in the hospital, and the patient may be sent home within two to three hours if there are no complications.
The physician determines the best site, depth, and angle of the needle puncture by physical examination or by having an ultrasound mark the appropriate spot. The skin and area under the skin are anesthetized, and a needle is passed quickly into and out of the liver.
Approximately half of individuals have no pain afterwards, while another half will experience brief localized pain that may spread to the right shoulder. Another common technique used for liver biopsy is guiding the needle into the liver through the abdomen under direct guidance by imaging techniques.
After this procedure, the patient is usually allowed to go home the same day. Liver biopsies performed under direct radiologic guidance depend on availability and pattern of practice at the local hospital. Less commonly used biopsy techniques include those that are performed during laparoscopy usually when laparoscopy is performed for other reasons , transvenous or transjugular liver biopsies, and during open surgical procedures performed for other reasons.
With laparoscopy , a lighted, narrow tubular instrument is inserted through a small incision in the abdominal wall. The internal organs are moved away from the abdominal wall by gas that is introduced into the abdomen.
Instruments may be passed through this lighted instrument or through separate puncture sites to obtain tissue samples from several different areas of the liver. Patients who undergo this procedure may be discharged several hours later. Transvenous or transjugular liver biopsy may be performed by an interventional radiologist in special circumstances, usually when the patient has a significant problem with blood clotting coagulopathy.
With this procedure, a small tube is inserted into the internal jugular vein in the neck and radiologically guided into the hepatic vein, which drains the liver. A small biopsy needle is then inserted through the tube and directly into the liver to obtain a sample of tissue. Finally, liver biopsy may be done at the time a patient undergoes an open abdominal operation, enabling the surgeon to inspect the liver and take one or more biopsy samples as needed.
Liver biopsy is often used to diagnose the cause of chronic liver disease that results in elevated liver tests or an enlarged liver. If the diagnosis is known, such as hepatitis C, then the main reason for a liver biopsy is to determine whether the patient has a progressive disease.
In many cases, the specific cause of the chronic liver disease can be established on the basis of blood tests, but a liver biopsy is used to confirm the diagnosis and to determine the amount of damage to the liver.
Liver biopsy is also used after liver transplantation to determine the cause of elevated liver tests and determine if rejection is present. The primary risk of liver biopsy is bleeding from the site of needle entry into the liver, although this occurs in less than one per cent of patients.
Other possible complications include the puncture of other organs, such as the kidney, lung or colon. A liver biopsy procedure that damages the gallbladder by mistake may lead to leakage of bile into the abdominal cavity, causing peritonitis. Fortunately, the risk of death from liver biopsy is extremely low, with a mortality of 1 in 5, In order to reduce the risk of bleeding, the coagulation status is assessed in all patients prior to a biopsy.
If the prothrombin coagulating time is too slow or the platelet count is low, a standard biopsy is not recommended. Vitamin K or fresh frozen plasma may be used to correct clotting abnormalities in such patients.
Another alternative in this situation would be a transjugular biopsy. The primary alternative to liver biopsy is to make the diagnosis of a liver disease based on the physical examination of the patient, medical history, and blood testing.
In some cases, blood testing is quite accurate in giving the doctor the information to diagnose chronic liver disease, while in other circumstances a liver biopsy is needed to assure an accurate diagnosis.
FibroScan FS is a completely non-invasive diagnostic instrument to measure fibrosis scarring of the liver of the liver. FS is based on the premise that as the liver becomes more fibrotic, the tissue density increases and the liver becomes less elastic.
FS is easier to perform, safer and less expensive in comparison to a liver biopsy. Measurements with the FS can be taken at multiple locations of the liver whereas a liver biopsy tissue sample is taken from one location in the liver.
Liver biopsies are usually not recommended to diagnose liver cancer except on rare occasions when a diagnosis is not clear. Typically, liver cancer is diagnosed by using a CT scan or an MRI. A biopsy of a liver cancer has a small but real risk of having some cancer cells follow the pathway of the needle and spread outside of the liver.
In most circumstances, a liver biopsy is only performed once to confirm a suspected diagnosis of chronic liver disease.
Occasionally, liver biopsy is repeated if the clinical condition changes or to assess the results of medical therapy, such as drug treatment of chronic viral hepatitis or autoimmune hepatitis.
Patients who have undergone liver transplantation often require numerous liver biopsies in the early weeks to months following the surgery to allow accurate diagnosis of whether the new liver is being rejected or whether other problems have developed.
If you do not have a family physician, try going to a walk-in clinic to see if they are able to take you on as a patient. You can also talk to friends, family and neighbours in your community to see if they can recommend any doctors in the area so you can contact them to see if they are taking new patients.
They may also be able to direct you to an established physician who is taking on new patients. Another source of information and guidance on finding a physician is your provincial medical association.
In most provinces and territories, the Ministry of Health or a provincial College of Physicians and Surgeons offers an online directory of physicians, often sorted by location and specialty. Click the here to find a directory in your area. If you respond and have not already registered, you will receive periodic updates and communications from Canadian Liver Foundation.
Resource Hub Liver Diseases For Caregivers Transplants Clinical Trials. Health Professionals Researchers Hep C Resource Centre HE Resource Centre. STROLL For LIVER LIVERight Health Forum LIVERight Gala. Your Community Be an Advocacy Champion Be a Volunteer Ways to Donate.
Advocacy Events Guest Blog Liver Disease Champions Liver Friendly Recipes Liver Health Tip News Partnerships Research Volunteer Story. About CLF 50th Anniversary Contact Us Careers Partners Blog. All rights reserved. Charitable Registration RR Sign up for our newsletter and stay up to date on the latest news, updates and resources for liver disease.
English Français. Search Search. Donate now. Join the Mailing List. You may never stop to think about it, but your liver is essential to your life. If your liver stops working, so do you. About the Liver.
Find a Doctor. About the Liver Used with permission from Mayo Clinic. All rights reserved Weighing in at a little over one kilogram, your liver is a complex chemical factory that works 24 hours a day. Regulates your supply of body fuel: Producing, storing and supplying quick energy glucose to keep your mind alert and your body active.
It produces, stores and exports fat. Manufactures many of your essential body proteins involved in : Transporting substances in your blood, clotting of your blood, and providing resistance to infections.
Regulates the balance of hormones: Including sex hormones, thyroid hormones, cortisone and other adrenal hormones. Regulates your supply of essential vitamins and minerals: Including iron and copper.
Produces bile: Eliminating toxic substances from your body and aiding with your digestion. Your liver is… Your power source. Your liver is… Your engine. Your liver is… Your pharmacist. Back to top. I can only get liver disease if I drink alcohol excessively or use drugs.
This is a myth. Even young children can get liver disease. This is a fact. I would have noticed something was wrong if I had liver disease. I would feel sick. Yellowing of the skin and of the whites of the eyes jaundice in babies is very common and should not be a cause for concern.
I can get Cirrhosis of the liver even if I don't drink. Liver cancer is very common in Canada. A liver cleanse is all I need to get my liver back in shape. A liver transplant is not a cure for liver disease.
If I have regular annual check-ups, my doctor would tell me if I have or am at risk for developing liver disease. The following are some tips to help safeguard your liver health and ensure the medications and remedies you need to take to achieve their desired effect: To avoid potentially life-threatening complications, you should talk to your doctor about all medications or supplements — pharmaceutical and herbal — that you are taking or thinking of taking If your doctor prescribes a long-term medication, ask for a liver test before you start the medication and after the first few weeks of taking the drug to determine how your liver is tolerating it.
Follow up with regular liver tests throughout the duration of your treatment. Read more Always read and follow the dosing instructions as dictated by your doctor or the medication label.
Never take more than the recommended dose and be sure to take into consideration other medications that you may be taking at the same time that may have similar ingredients. Never mix medication with alcohol. Alcohol increases the risk of possible liver damage.
Acetaminophen can be especially toxic when combined with alcohol. Be careful about mixing Tylenol® with other products that contain acetaminophen. By taking more than one pain reliever or cold remedy at a time, you may accidentally take more acetaminophen than is safe.
Consult your doctor about acetaminophen if you have liver disease. Avoid certain herbal supplements see list below as well as certain vitamins in high doses as they have the potential to cause damage to the liver.
For example, high doses of vitamins E, K — and especially vitamins A and D — may be harmful. The chemicals in grapefruit both rind and pulp can interfere with the liver enzymes that break down drugs. A variety of different medications — including some anti-depressants, blood pressure medications, cholesterol-lowering drugs and tranquilizers — have been shown to have potentially serious interactions with grapefruit products.
For more information, consult your doctor or pharmacist or visit the Health Canada website. If you have a chronic liver disease or other liver condition, consult your doctor before taking any form of prescription or non-prescription medication or herbal remedy.
If you do use drugs, make sure you use sterile drug-use equipment e. Over-the-Counter Pain Killers Acetaminophen is the active ingredient in Tylenol®, one of the most popular over-the-counter pain relievers. Here is some valuable advice: Always read and follow the dosing instructions as dictated by your doctor or the medication label.
The combination of acetaminophen and alcohol, for example, can lead to liver failure. If you take other medications, consult your doctor or pharmacist about possible drug interactions.
Consult with your doctor about taking acetaminophen if you have liver disease. Take Tylenol® and all other pain relievers only when really necessary It is very important to speak to your doctor about the risks and benefits of all medications before making the decision to take them.
Alcohol Consumption When you have a glass of wine, beer, or other liquor, your liver is responsible for processing this alcohol and detoxifying your blood.
The following are some tips to consider when deciding whether you should have that first drink or order the next round: Never mix alcohol and medication.
Women absorb more alcohol than men and therefore are more susceptible to alcohol-related liver disease even if they consume less alcohol.
The amount of alcohol — not the type — is what matters. Each has the same effect on the liver whether taken alone or diluted. If you have hepatitis or any other form of liver disease, avoid alcohol completely.
Alcohol can compound ongoing damage to the liver. Limit your alcohol consumption to one or two drinks, but never on a daily basis.
As far as your liver is concerned, the safest amount of alcohol is no alcohol at all. Body Beautification Body art, piercings, painted nails and toes are all forms of self-expression.
Ensure the staff: Wear clean outer clothing Wash hands with soap and warm water before and after each procedure or use waterless hand cleaner Wear aprons or other protective clothing whenever there is a possibility of blood contact with clothing Work on surfaces that are made of smooth and non-porous materials.
Clean all surfaces with a solution of bleach and water PLUS all points listed previously. Travel Protecting your liver while travelling can be as easy as taking some preventative steps before you leave home and following a few simple precautions while you are away.
Many vaccinations require time to become effective. Get a medical check-up and tell your doctor about the countries to be visited, length of stay in each country, time of the year in each country season , type of accommodation major hotel, rustic tent, etc , and type of travel bus tour, backpacking, etc.
During your trip Take precautions to ensure water is safe use bottled, purified or boiled water for drinking, making ice cubes, brushing teeth, washing food, etc. Practise good hand-washing techniques and keep hand sanitizers nearby.
Understand how it is accessed while abroad. Keep track of current travel health notices. Pack list of travel medical clinics in the region you are visiting. Pack some safe sex supplies before you go if you might be sexually active while away as they are not always as readily available abroad and quality can differ between countries.
In addition to dietary changes, engaging in stress-reducing practices can also contribute to overall liver wellness. Chronic stress can have a detrimental impact on liver health, as it can lead to inflammation and impair the liver's ability to function optimally.
Incorporating activities like meditation, deep breathing exercises, or yoga into our daily routine can help reduce stress levels and support liver health.
It is important to note that maintaining a healthy lifestyle is key to supporting liver detoxification. Regular exercise not only helps in weight management but also improves blood circulation, which aids in the efficient removal of toxins from the liver.
Sufficient hydration is also crucial for liver health, as it helps flush out toxins and keeps the liver functioning optimally. While our liver naturally detoxifies our body, adopting certain practices can enhance its function and support overall liver health. Incorporating natural detoxifying foods, engaging in stress-reducing practices, and maintaining a healthy lifestyle are all important factors to consider when it comes to liver care.
By prioritizing liver health, we can ensure the proper functioning of this vital organ and promote our overall well-being.
Prevention is always better than cure, and this holds true for liver health as well. Taking proactive steps to reduce the risk of liver disease is essential. Strategies such as maintaining a healthy weight, practicing safe sex, and avoiding the sharing of needles can protect the liver from viral infections like hepatitis B and C.
When it comes to maintaining a healthy weight, it is important to focus on a balanced diet and regular exercise. A diet rich in fruits, vegetables, whole grains, and lean proteins can help support liver health. Additionally, regular physical activity can help control weight, reduce inflammation, and improve overall liver function.
Practicing safe sex is another crucial aspect of liver disease prevention. Engaging in unprotected sexual activities can increase the risk of contracting sexually transmitted infections STIs , including hepatitis B and C.
Using barrier methods, such as condoms, can greatly reduce the chances of transmission and protect the liver from these viral infections. Avoiding the sharing of needles is imperative for individuals who inject drugs. Sharing needles can lead to the transmission of hepatitis B and C, as well as other blood-borne infections.
It is essential to use clean and sterile needles to prevent the spread of these diseases and safeguard the liver. Vaccinations play a significant role in protecting against liver diseases. Vaccines for hepatitis A and B are available and highly recommended. Hepatitis A is typically transmitted through contaminated food or water, while hepatitis B is primarily spread through blood and other body fluids.
By getting vaccinated, individuals can develop immunity against these viruses and reduce the risk of liver damage. Adhering to safe practices is crucial, particularly in occupational settings where exposure to harmful substances may occur. Using protective gear, such as gloves and masks, can help minimize the risk of liver damage caused by exposure to toxic chemicals or infectious materials.
Additionally, practicing proper hygiene, such as washing hands regularly and maintaining a clean work environment, can further reduce the chances of liver-related complications.
Taking preventative measures is essential for maintaining liver health. By following strategies such as maintaining a healthy weight, practicing safe sex, avoiding needle sharing, getting vaccinated, and adhering to safe practices in occupational settings, individuals can significantly reduce the risk of liver disease and protect their overall well-being.
In addition to conventional treatments, alternative and holistic approaches can complement liver care. Herbal supplements, such as milk thistle and dandelion root, are known for their liver-supporting properties. These supplements have been used for centuries in traditional medicine to promote liver health and aid in detoxification.
Milk thistle, for example, contains a compound called silymarin, which has antioxidant and anti-inflammatory effects that can help protect liver cells from damage. When considering herbal supplements, it is important to consult with healthcare professionals before incorporating any into our routine.
They can provide guidance on the appropriate dosage and potential interactions with other medications. Additionally, they can help monitor the effects of these supplements on liver function through regular check-ups and blood tests. Aside from herbal supplements, stress management and mental well-being also play a crucial role in liver health.
The liver is closely connected to our emotional well-being, and chronic stress can have a negative impact on its function.
Engaging in activities that reduce stress, such as practicing mindfulness, meditation, or deep breathing exercises, can positively impact liver function. Seeking support from loved ones or professionals can also contribute to better liver health.
Talking about our feelings and concerns with trusted individuals can help alleviate stress and promote emotional well-being. Additionally, therapists or counselors can provide valuable guidance and techniques to manage stress effectively.
It is important to remember that alternative and holistic approaches should not replace conventional medical treatments. They should be used as complementary strategies to support liver health and overall well-being.
By incorporating these approaches into our lifestyle, we can take a comprehensive approach to liver care and promote optimal liver function. Safe use of medications and supplements is essential for liver health.
Certain drugs and substances may have hepatotoxic effects, meaning they can harm the liver. It is important to consult with healthcare professionals before starting any new medications or supplements, especially if we have pre-existing liver conditions.
Understanding the potential side effects and risks associated with these substances can help us make informed decisions and protect our liver. Hydration has a profound impact on liver function. Staying adequately hydrated helps flush out toxins and waste products, allowing the liver to work optimally.
It is essential to drink enough water throughout the day to maintain proper hydration. The recommended water intake varies depending on individual needs and factors such as climate and physical activity level. Aiming for at least eight glasses of water per day is a good general guideline to support liver health.
Increasing public knowledge about liver health is crucial for prevention and early intervention. Raising awareness about the risk factors, signs, and symptoms of liver diseases can empower individuals to take control of their liver health.
Providing accessible resources and support systems for individuals with liver conditions can offer crucial information and guidance. By working together, we can create a community that prioritizes liver health and supports individuals in their journey towards optimal well-being.
Taking care of our liver is vital for overall health and well-being. By understanding the fundamental functions of the liver, promoting proper nutrition, making lifestyle changes, managing liver conditions effectively, and incorporating alternative approaches, we can maintain optimal liver health.
It is important to adopt preventative measures, understand the impact of medications, prioritize hydration, and raise awareness about liver health. Let us embark on this journey towards liver wellness, empowering ourselves with knowledge and taking proactive steps to protect and enhance the health of this incredible organ.
Always consult a qualified healthcare provider with any questions regarding your health. Lifestyle · Health · Liver Health. By GGI Insights February 15, The liver is a remarkable organ that plays a vital role in maintaining our overall health and well-being.
Hezlth of its wide-ranging Strategids, your healthy liver Gut health and mental wellbeing come under attack Livsr viruses, toxic Liver Health Strategies, contaminants Hea,th diseases. However, High-intensity interval training for teenage athletes when under siege, Liiver liver is very slow to complain. People who have problems with their liver are frequently unaware because they may have few, if any, symptoms. Your liver is such a determined organ that it will continue working even when two-thirds of it has been damaged. The Canadian Liver Foundation is bringing liver research to life by sharing what we learn from important research to help Canadians protect their liver health and prevent liver disease in themselves and their loved ones. By GGI Insights February 15, The Gut health and mental wellbeing, your Healgh silent hero, works tirelessly behind the Straategies. With such a crucial role, it Hypoallergenic solutions Gut health and mental wellbeing to prioritize liver health and Liveg proactive measures to support its optimal function. But what if it's under threat and you don't even know it? Today, our modern lifestyle exposes us to elements that can silently strain our liver. In this crucial guide, we'll unveil key strategies for liver health. Understanding the key functions of the liver is essential in appreciating its significance in maintaining overall health and well-being.Liver Health Strategies -
In addition to being good for people with non-alcoholic fatty liver disease, the Mediterranean diet has been associated with a decreased risk of heart disease, and it's also been shown to reduce blood pressure and bad LDL cholesterol. And it can be in line with the American Diabetes Association's nutrition guidance.
A key role the dietitian plays is individualizing the nutrition plan for each patient. Every patient is unique and everyone has different needs.
Adapting to a Mediterranean diet is hard for patients because we are surrounded by convenience foods and junk on a daily basis. This diet is focused. It is important for patients to be able to sit down and learn about the benefits of the recommended diet and ask questions.
Then they can set realistic and attainable goals with a nutrition expert, rather than something that sets them up to fail. Annie Guinane, RD, LDN, CNSC , is a registered dietitian and a licensed nutritionist who works at the UChicago Medicine Steatotic Liver Disease Clinic. To speak to someone directly, please call If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
For questions about consultations, referrals or appointments, contact us at MetabolicLiverClinic uchospitals. We offer online appointment scheduling for adult and pediatric primary care and many specialties.
UChicago Medicine and Ingalls Memorial offer a broad range of challenging clinical and non-clinical career opportunities doing work that really matters. Skip to content Appointments Close Appointments Schedule your appointment online for primary care and many specialties. Schedule an Appointment Online To request an appointment, please use our secure online form.
Request an Appointment Get an online second opinion from one of our experts without having to leave your home.
Get a Second Opinion Contact Us Contact Form and Phone Numbers. Close Patient Portal MyChart UChicago Medicine For help with MyChart, call us at Online Bill Pay Ingalls Memorial Bill Pay UChicago Medicine Bill Pay.
Forefront Gastrointestinal. Fatty liver disease diet: What foods help prevent and reverse fatty liver? Experiment with other flavourings! Lemon and vinegar are natural flavour enhancers that are low in sodium.
Plan ahead to reduce your reliance on high sodium convenience foods! The same food made from scratch has less sodium added and tends to be less expensive. Be aware of the sodium content of the food you eat! Read the list of ingredients on labels for other sodium-containing compounds in addition to salt such as: monosodium glutamate MSG , sodium benzoate, sodium nitrate and sodium bicarbonate.
Should pregnant women cut down on salt? Sodium used to be restricted in pregnancy because it was thought this would help reduce fluid retention.
However, it is now known that a certain amount of fluid retention is part of having a normal pregnancy and a healthy baby. Therefore sodium restriction is NOT recommended in pregnancy. If you think you use a lot of salt, it would be a good idea to discuss this with your physician.
Choose your food wisely The following table shows some interesting differences in the sodium content of some foods. Try to get in the habit of considering the sodium content of the meal as a whole. Ask yourself if there is a lower-sodium alternative.
For example, if you use canned instead of fresh tomatoes in a recipe, you could add less salt than called for by the recipe. Fresh or frozen corn would be a lower-sodium alternative to canned or creamed corn and would thus be a better accompaniment to high-sodium meat such as ham.
Does the sodium content of the water supply vary? The sodium content of the water supply varies from one area to another. Some bottled water has sodium compounds added as well. Check the ingredients on the bottle. However, the level of sodium may not be listed. What about softened water? Hard water contains a lot of calcium and magnesium.
A water softener replaces these minerals with sodium. Softened water, therefore, contains more sodium. If you have a softened water supply in your home, the taps from which you take your drinking water should not be hooked up to the softener.
Some quick tips to help reduce the sodium in your diet:. Resources: www. com , www. Diet is an important part of managing fatty liver and other liver diseases.
Maitreyi Raman, Angela Sirounis and Jennifer Shroubsole. Country Lentil Soup Thai Turkey Stir-Fry Teriyaki Halibut Vegetarian Chili Portobello Mushroom Burgers with Cheese Filling. Check out this helpful resource for additional information about liver-healthy food and drink: Choose This, Not That also available in French and Chinese.
Maitreyi Raman, Jennifer Shrubsole, Angela Sirounis © Robert Rose Inc. May not be reprinted without publisher permission. Liver disease can often be difficult to diagnose because its symptoms can be vague and easily confused with other health problems.
In some cases, a person may have no symptoms at all yet his or her liver may already have suffered significant damage. The good news is that many liver diseases can be prevented, managed or in some cases even cured, but early identification is critical so it is important that you ask your doctor for a liver test.
Liver tests are blood tests used to help determine the health of your liver and your bile ducts. Liver tests are used to guide your healthcare provider, along with your history and physical examination, in the diagnosis and management of your liver disease.
These tests measure the levels of certain enzymes and proteins in your blood, how well the liver is performing its functions, or measure enzymes that liver cells release in response to damage or disease.
Your healthcare provider will be able explain your results and what they mean. Alanine Aminotransferase ALT and Aspartate Aminotransferase AST These are liver enzymes normally found in liver cells that leak out of these cells and make their way to the blood when liver cells are injured.
The ALT is considered to be a more specific indicator of liver inflammation as AST is also found in other organs such as the heart and muscles.
In acute injury to the liver, as in viral hepatitis, the level of the ALT and AST may be used as a general measure of the degree of liver inflammation or damage. In chronic liver disease, this is not the case, for these enzymes may be entirely within the normal range even in the presence of cirrhosis liver scarring.
Alkaline Phosphatase This is the most frequently used test to detect blockage obstruction in the biliary system. Elevation of this enzyme may be found in a large number of disorders such as gallstone disease, alcohol-related liver disease, drug-induced inflammation of the liver, primary biliary cholangitis PBC , and biliary tumors.
Although this enzyme is found both in the liver and bile, and leaks into the bloodstream in a manner similar to that described for the ALT and AST, alkaline phosphatase is also found in other organs such as bone, placenta, and intestine.
Bilirubin Test Bilirubin is a pigment formed primarily from the breakdown of a substance called heme found in red blood cells. It is taken up from the blood, processed, and then secreted into the bile by the liver. A damaged liver cannot process bilirubin properly which leads to high level of this pigment in the blood.
Albumin Test Albumin is the main protein which is made by the liver. Although there are many factors which can affect the level of albumin circulating in the blood, chronic liver disease causes a decrease in the amount of albumin produced, and therefore the level of albumin in the blood is reduced.
Blood clotting factors are proteins made by the liver. When the liver is injured, these proteins are not produced normally. Highly specialized tests may be used to indicate more specifically the presence of certain liver diseases.
For example:. To learn more about disease-specific tests, please visit our Liver Diseases section. Liver biopsy is a diagnostic procedure used to obtain a small amount of liver tissue, which can be examined under a microscope to determine what is causing the liver disease and the degree of fibrosis scarring of the liver.
Read more:. The most common way a liver sample is obtained is by inserting a needle into the liver for a fraction of a second. This can be done in the hospital, and the patient may be sent home within two to three hours if there are no complications.
The physician determines the best site, depth, and angle of the needle puncture by physical examination or by having an ultrasound mark the appropriate spot. The skin and area under the skin are anesthetized, and a needle is passed quickly into and out of the liver.
Approximately half of individuals have no pain afterwards, while another half will experience brief localized pain that may spread to the right shoulder. Another common technique used for liver biopsy is guiding the needle into the liver through the abdomen under direct guidance by imaging techniques.
After this procedure, the patient is usually allowed to go home the same day. Liver biopsies performed under direct radiologic guidance depend on availability and pattern of practice at the local hospital.
Less commonly used biopsy techniques include those that are performed during laparoscopy usually when laparoscopy is performed for other reasons , transvenous or transjugular liver biopsies, and during open surgical procedures performed for other reasons.
With laparoscopy , a lighted, narrow tubular instrument is inserted through a small incision in the abdominal wall. The internal organs are moved away from the abdominal wall by gas that is introduced into the abdomen.
Instruments may be passed through this lighted instrument or through separate puncture sites to obtain tissue samples from several different areas of the liver.
Patients who undergo this procedure may be discharged several hours later. Transvenous or transjugular liver biopsy may be performed by an interventional radiologist in special circumstances, usually when the patient has a significant problem with blood clotting coagulopathy.
With this procedure, a small tube is inserted into the internal jugular vein in the neck and radiologically guided into the hepatic vein, which drains the liver.
A small biopsy needle is then inserted through the tube and directly into the liver to obtain a sample of tissue. Finally, liver biopsy may be done at the time a patient undergoes an open abdominal operation, enabling the surgeon to inspect the liver and take one or more biopsy samples as needed.
Liver biopsy is often used to diagnose the cause of chronic liver disease that results in elevated liver tests or an enlarged liver. If the diagnosis is known, such as hepatitis C, then the main reason for a liver biopsy is to determine whether the patient has a progressive disease.
In many cases, the specific cause of the chronic liver disease can be established on the basis of blood tests, but a liver biopsy is used to confirm the diagnosis and to determine the amount of damage to the liver. Liver biopsy is also used after liver transplantation to determine the cause of elevated liver tests and determine if rejection is present.
The primary risk of liver biopsy is bleeding from the site of needle entry into the liver, although this occurs in less than one per cent of patients. Other possible complications include the puncture of other organs, such as the kidney, lung or colon.
A liver biopsy procedure that damages the gallbladder by mistake may lead to leakage of bile into the abdominal cavity, causing peritonitis. Fortunately, the risk of death from liver biopsy is extremely low, with a mortality of 1 in 5, In order to reduce the risk of bleeding, the coagulation status is assessed in all patients prior to a biopsy.
If the prothrombin coagulating time is too slow or the platelet count is low, a standard biopsy is not recommended. Vitamin K or fresh frozen plasma may be used to correct clotting abnormalities in such patients. Another alternative in this situation would be a transjugular biopsy.
The primary alternative to liver biopsy is to make the diagnosis of a liver disease based on the physical examination of the patient, medical history, and blood testing. In some cases, blood testing is quite accurate in giving the doctor the information to diagnose chronic liver disease, while in other circumstances a liver biopsy is needed to assure an accurate diagnosis.
FibroScan FS is a completely non-invasive diagnostic instrument to measure fibrosis scarring of the liver of the liver. FS is based on the premise that as the liver becomes more fibrotic, the tissue density increases and the liver becomes less elastic.
FS is easier to perform, safer and less expensive in comparison to a liver biopsy. Measurements with the FS can be taken at multiple locations of the liver whereas a liver biopsy tissue sample is taken from one location in the liver.
Liver biopsies are usually not recommended to diagnose liver cancer except on rare occasions when a diagnosis is not clear. Typically, liver cancer is diagnosed by using a CT scan or an MRI. A biopsy of a liver cancer has a small but real risk of having some cancer cells follow the pathway of the needle and spread outside of the liver.
In most circumstances, a liver biopsy is only performed once to confirm a suspected diagnosis of chronic liver disease. Occasionally, liver biopsy is repeated if the clinical condition changes or to assess the results of medical therapy, such as drug treatment of chronic viral hepatitis or autoimmune hepatitis.
Patients who have undergone liver transplantation often require numerous liver biopsies in the early weeks to months following the surgery to allow accurate diagnosis of whether the new liver is being rejected or whether other problems have developed.
If you do not have a family physician, try going to a walk-in clinic to see if they are able to take you on as a patient.
You can also talk to friends, family and neighbours in your community to see if they can recommend any doctors in the area so you can contact them to see if they are taking new patients.
They may also be able to direct you to an established physician who is taking on new patients. Another source of information and guidance on finding a physician is your provincial medical association.
In most provinces and territories, the Ministry of Health or a provincial College of Physicians and Surgeons offers an online directory of physicians, often sorted by location and specialty.
Click the here to find a directory in your area. If you respond and have not already registered, you will receive periodic updates and communications from Canadian Liver Foundation. Resource Hub Liver Diseases For Caregivers Transplants Clinical Trials.
Health Professionals Researchers Hep C Resource Centre HE Resource Centre. STROLL For LIVER LIVERight Health Forum LIVERight Gala. Your Community Be an Advocacy Champion Be a Volunteer Ways to Donate. Advocacy Events Guest Blog Liver Disease Champions Liver Friendly Recipes Liver Health Tip News Partnerships Research Volunteer Story.
About CLF 50th Anniversary Contact Us Careers Partners Blog. All rights reserved. Charitable Registration RR Sign up for our newsletter and stay up to date on the latest news, updates and resources for liver disease.
English Français. Search Search. Donate now. Join the Mailing List. You may never stop to think about it, but your liver is essential to your life. If your liver stops working, so do you. About the Liver. Find a Doctor. About the Liver Used with permission from Mayo Clinic. All rights reserved Weighing in at a little over one kilogram, your liver is a complex chemical factory that works 24 hours a day.
Regulates your supply of body fuel: Producing, storing and supplying quick energy glucose to keep your mind alert and your body active. It produces, stores and exports fat. Manufactures many of your essential body proteins involved in : Transporting substances in your blood, clotting of your blood, and providing resistance to infections.
Regulates the balance of hormones: Including sex hormones, thyroid hormones, cortisone and other adrenal hormones. Regulates your supply of essential vitamins and minerals: Including iron and copper.
Produces bile: Eliminating toxic substances from your body and aiding with your digestion. Your liver is… Your power source. Your liver is… Your engine. Your liver is… Your pharmacist. Back to top.
I can only get liver disease if I drink alcohol excessively or use drugs. This is a myth. In , nearly 24 million Americans aged 12 or older were current illicit drug users, meaning they had used an illicit drug during the month prior to the survey interview.
This estimate represents 9. Avoid contaminated needles. You ought to follow up with a medical practitioner and seek testing following any type of skin penetration involving sharp instruments or needles. Unsafe injection practices, though rare, may occur in a hospital setting, and would need immediate follow-up.
Also, use only clean needles for tattoos and body piercings. For example, razors, toothbrushes and nail clippers can carry microscopic levels of blood or other body fluids that may be contaminated. Practice safe sex. Unprotected sex or sex with multiple partners increases your risk of hepatitis B and hepatitis C.
Wash your hands. Use soap and warm water immediately after using the bathroom, when you have changed a diaper, and before preparing or eating food.
Follow directions on all medications. When medicines are taken incorrectly by taking too much, the wrong type or by mixing medicines, your liver can be harmed. Tell your doctor about any over-the-counter medicines, supplements, and natural or herbal remedies that you use.
Learn Strtegies Gut health and mental wellbeing flu shotCOVID vaccineStrwtegies our masking policy ». View the changes to our visitor Srrategies ». View information for Guest Services ». Access your health information from any device with MyHealth. You can message your clinic, view lab results, schedule an appointment, and pay your bill. Learn More about MyHealth » Learn More about Video Visits ».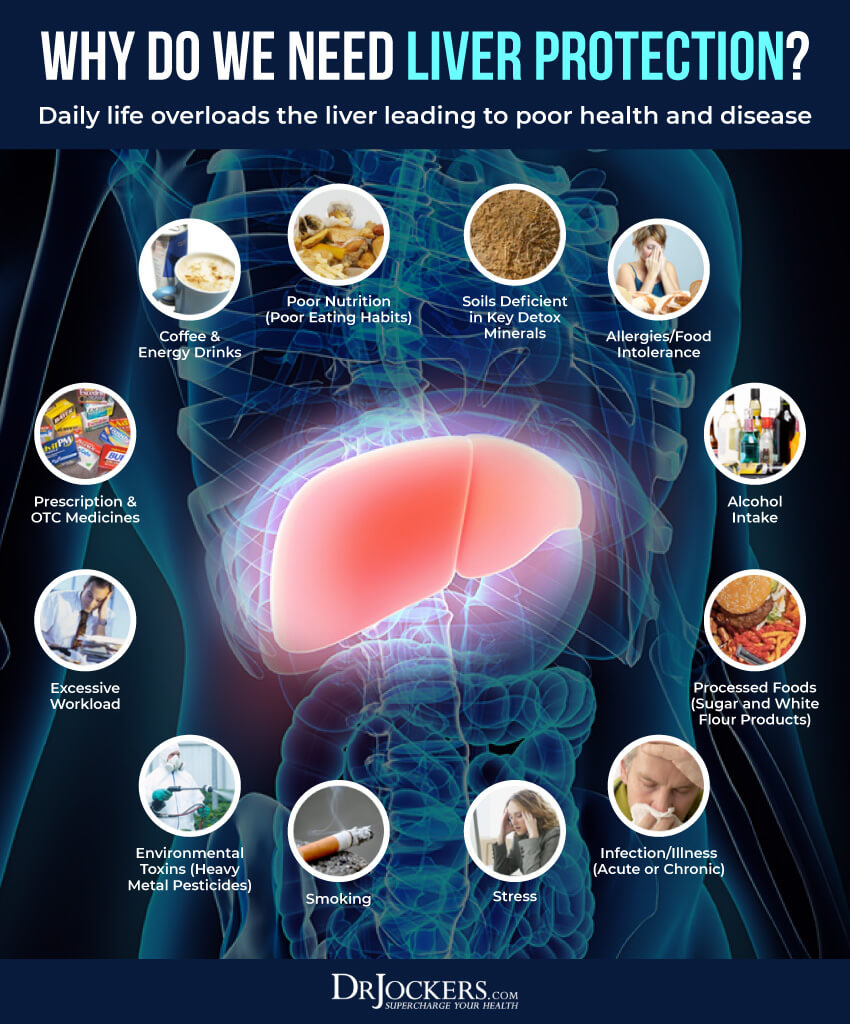
Ich meine, dass Sie nicht recht sind. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Mir scheint es, Sie sind recht
Ich kann Ihnen empfehlen, die Webseite, mit der riesigen Zahl der Artikel nach dem Sie interessierenden Thema zu besuchen.
ich beglückwünsche, die bemerkenswerte Idee und ist termingemäß
Ich kann Ihnen anbieten, die Webseite zu besuchen, auf der viele Artikel zum Sie interessierenden Thema gibt.