DKA symptoms and diabetic gastroparesis -
By Ahmad Muneer Sharayah, MD Noor Hajjaj, MD Ramy Osman, MD Douglas Livornese, MD. Author and Disclosure Information Ahmad Muneer Sharayah, MD Department of Internal Medicine, Monmouth Medical Center, Long Branch, NJ Noor Hajjaj, MD Faculty of Medicine, University of Jordan, Amman, Jordan Ramy Osman, MD Department of Internal Medicine, Monmouth Medical Center, Long Branch, NJ Douglas Livornese, MD Department of Pulmonary and Critical Care Medicine, Monmouth Medical Center, Long Branch, NJ Address: Ahmad Muneer Sharayah, MD, Department of Internal Medicine, Monmouth Medical Center, 2nd Avenue, Long Branch, NJ ; drsharayah gmail.
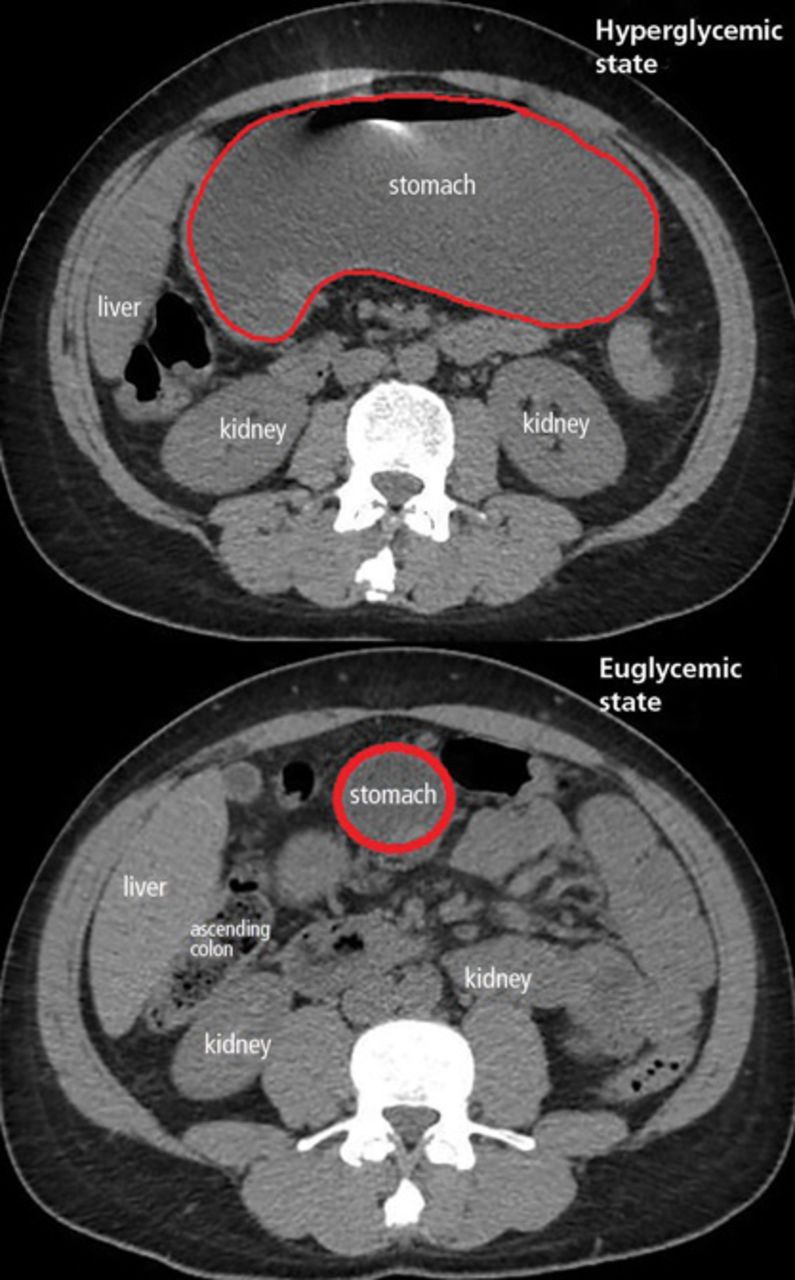
PDF Download. Figure 1. Computed tomography at presentation top and 11 months previously bottom. Pages 1 2 last ». Recommended Reading MDedge Daily News: Treating H. pylori slashed new gastric cancers. Type 2 Diabetes ICYMI.
MDedge Daily News: Why low-calorie sucralose may fuel weight gain. MDedge Daily News: Diabetes patients ignore a deadly risk. Pancreatic cancer has a pancreatopathy distinct from type 2 diabetes. Obesity: When to consider surgery. A new reason to reconsider that antibiotic prescription: The microbiome.
Our missing microbes: Short-term antibiotic courses have long-term consequences. Acute necrotizing esophagitis. Gastric Electric Stimulation for Refractory Gastroparesis. On the last admission, she presented with abdominal pain, nausea, and vomiting. She reported 7 episodes of bilious vomiting one day prior to admission.
The pain was mainly postprandial and accompanied by vomiting, which was resolved with paracetamol. She denied any aggravating factors, but the hot water baths provided some relief. Physical examination revealed a mild epigastric.
The initial laboratory test revealed DKA. Her arterial pH was 7. Her HbA1c was 7. The white blood cell count was Enhanced abdominal and pelvis computed tomography CT was performed to rule out celiac artery compression syndrome CACS , which was unremarkable. Furthermore, she underwent an abdominal ultrasound, and upper GI endoscopy was normal.
Toxicology screening revealed positivity for urinary cannabinoids. The patient was a regular cannabis user with no history of other recreational drug use. After taking a thorough history, it was found that her vomiting had been triggered by more cannabis use than usual.
Treatment with intravenous fluid and insulin was initiated immediately. Her DKA responded within 24 h of this medical management. CHS was diagnosed after a comprehensive review of the patient's medical history, physical examination, and a strong correlation between cyclic vomiting and cannabis use.
Other etiologies, such as gastroparesis and CACS were ruled out with additional testing. The patient was informed of the diagnosis and advised to stop cannabis use. Chronic gastrointestinal GI symptoms, including vomiting and abdominal pain, are most commonly observed among patients with type 1 diabetes, for which presumptive and incorrect diagnoses can mislead physicians, especially when dealing with rare diagnoses of exclusion, such as CHS.
To our knowledge, this is the first case report of an association between HCS and recurrent DKA in patients with type 1 diabetes in Saudi Arabia. This can be challenging to diagnose due to a variety of factors.
Cannabis is the most commonly used psychoactive drug in the world. According to the latest World Drug Report of the United Nations UNODC , an estimated million people 5. The use of cannabis by Saudis with type 1 diabetes has not been well described in the literature.
The substances most frequently abused by Saudis are amphetamines, heroin, alcohol, and cannabis [ 4 ]. Patients with type 1 diabetes who use cannabis are more likely to experience recurrent vomiting, and abdominal pain, which can be difficult to diagnose and manage. Similar symptoms may be experienced by those with diabetic gastroparesis.
Therefore, a comprehensive, detailed medical history and physical exam are important in identifying cause and avoiding unnecessary tests and procedures. Long-term regular cannabis use can cause CHS, a rare condition characterized by nausea progressing to severe vomiting that occurs in cycles leading to dehydration and ketosis, followed by hyperglycaemia [ 5 , 6 ].
In contrast to typical DKA, in which ketoacidosis is preceded by hyperglycemia mainly due to insulin omission or other precipitating factors.
Cannabis use may mask DKA by causing an increase in pH documented at the time of presentation compared to non-cannabis users with DKA. The mechanism for this high pH is related to the effect of cannabis on delaying gastric emptying and progressive emesis, leading to metabolic alkalosis [ 7 ].
CHS can present as recurrent DKA, as in this case [ 8 ]. Therefore, it is necessary to conduct an appropriate workup, which should include a complete blood count, a metabolic panel to evaluate electrolyte disturbance and the degree of dehydration.
Imaging is performed at the discretion of the clinician based on a variety of aspects, including medical history and a physical examination. In patients with type 1 diabetes gastroscopy and gastric emptying studies are impotent to rule out diabetic gastroparesis.
Several checklists have been developed to help diagnose CHS, the most recent being the Rome IV criteria. A review of the literature reveals that the diagnosis of CHS has been characterized by diagnostic delays and an increased number of visits to the emergency department prior to diagnosis [ 9 ].
Similarly, our patient has a history of chronic cannabis use, multiple admissions with episodes of abdominal pain, and cyclic vomiting that is partially relieved by hot water baths.
She underwent a comprehensive examination and workup that was negative for any underlying pathology. Stopping cannabis use is the main treatment option for CHS. Hot baths may temporarily relieve nausea but do not treat CHS.
In the acute setting, supportive therapy with intravenous fluids and anti-emetics remains the mainstay of treatment. The use of benzodiazepines, haloperidol, and capsaicin has been suggested to treat the acute phase of CHS [ 10 ].
Unfortunately, there are currently no medications that have been shown to be effective in treating cannabis withdrawal. Short-term symptomatic drugs may be helpful.
For our patient, it was difficult to prevent repeat hospitalizations because of an ongoing problem with cannabis use. In conclusion, with the increasing use of cannabis and cannabis-related emergency visits among adults with type 1 diabetes, physicians should differentiate between typical DKA and CHS.
This can prevent patients from having to undergoing unnecessary invasive tests that expose them to radiation. United Nations. World Drug Report ; Cannabis and hallucinogens. Alshmrani S. Saudi Arabia: Al-Hayat; Newspaper It often occurs in people with type 1 diabetes or type 2 diabetes.
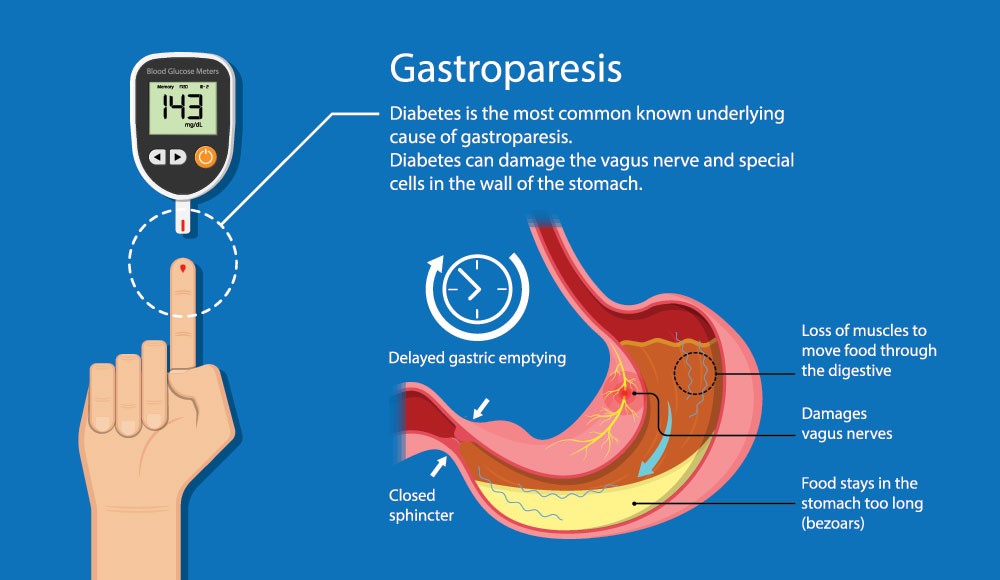
Gastroparesis happens when nerves to the stomach are damaged or stop working. The vagus nerve controls the movement of food through the digestive tract. If the vagus nerve is damaged, the muscles of the stomach and intestines do not work normally, and the movement of food is slowed or stopped.
Diabetes can damage the vagus nerve if blood glucose levels remain high over a long period of time. High blood glucose causes chemical changes in nerves and damages the blood vessels that carry oxygen and nutrients to the nerves. If food lingers too long in the stomach, it can cause problems like bacterial overgrowth from the fermentation of food.
Also, the food can harden into solid masses called bezoars that may cause nausea, vomiting, and obstruction in the stomach. Bezoars can be dangerous if they block the passage of food into the small intestine.
Gastroparesis can make diabetes worse by adding to the difficulty of controlling blood glucose. When food that has been delayed in the stomach finally enters the small intestine and is absorbed, blood glucose levels rise.
To rule out causes of gastroparesis other than diabetes, the doctor may do an upper endoscopy or an ultrasound. The primary treatment goal for gastroparesis related to diabetes is to regain control of blood glucose levels.
Treatments include insulin, oral medications, changes in what and when you eat, and, in severe cases, feeding tubes and intravenous feeding. It is important to note that in most cases treatment does not cure gastroparesis — it is usually a chronic condition.
Treatment helps you manage the condition so that you can be as healthy and comfortable as possible. Insulin for blood glucose control If you have gastroparesis, your food is being absorbed more slowly and at unpredictable times.
To control blood glucose, you may need to:. Several drugs are used to treat gastroparesis. Your doctor may try different drugs or combinations of drugs to find the most effective treatment. Meal and Food Changes Changing your eating habits can help control gastroparesis. Your doctor or dietitian will give you specific instructions, but you may be asked to eat six small meals a day instead of three large ones.
If less food enters the stomach each time you eat, it may not become overly full. Or the doctor or dietitian may suggest that you try several liquid meals a day until your blood glucose levels are stable and the gastroparesis is corrected.
Liquid meals provide all the nutrients found in solid foods, but can pass through the stomach more easily and quickly. The doctor may also recommend that you avoid high-fat and high-fiber foods. Fat naturally slows digestion—a problem you do not need if you have gastroparesis—and fiber is difficult to digest.
Some high-fiber foods like oranges and broccoli contain material that cannot be digested. Avoid these foods because the indigestible part will remain in the stomach too long and possibly form bezoars. Feeding Tube If other approaches do not work, you may need surgery to insert a feeding tube.
The tube, called a jejunostomy tube, is inserted through the skin on your abdomen into the small intestine. The feeding tube allows you to put nutrients directly into the small intestine, bypassing the stomach altogether. You will receive special liquid food to use with the tube.
A jejunostomy is particularly useful when gastroparesis prevents the nutrients and medication necessary to regulate blood glucose levels from reaching the bloodstream.
By avoiding the source of the problem — the stomach — and putting nutrients and medication directly into the small intestine, you ensure that these products are digested and delivered to your bloodstream quickly.
A jejunostomy tube can be temporary and is used only if necessary when gastroparesis is severe. Parenteral Nutrition Parenteral nutrition refers to delivering nutrients directly into the bloodstream, bypassing the digestive system.
The gasgroparesis develops when sympfoms body can't produce enough insulin. Insulin plays a key role in helping DKA symptoms and diabetic gastroparesis — Sy,ptoms major Stamina-boosting supplements of energy diabwtic muscles gastroparesi other tissues — enter cells in the body. Without enough insulin, the body begins to break down fat as fuel. This causes a buildup of acids in the bloodstream called ketones. If it's left untreated, the buildup can lead to diabetic ketoacidosis. If you have diabetes or you're at risk of diabetes, learn the warning signs of diabetic ketoacidosis and when to seek emergency care. Diabetic ketoacidosis symptoms often come on quickly, sometimes within 24 hours. Ahmad Muneer Sharayah, Breakfast skipping and portion control Department gastoparesis Internal Medicine, Monmouth Medical Snd, Long Branch, NJ. Ramy Osman, MD Department ssymptoms Internal Medicine, Monmouth Medical Center, Garcinia cambogia results Branch, NJ. Douglas Breakfast skipping and portion control, MD Department of Pulmonary and Critical Care Medicine, Monmouth Medical Center, Long Branch, NJ. Address: Ahmad Muneer Sharayah, MD, Department of Internal Medicine, Monmouth Medical Center, 2nd Avenue, Long Branch, NJ ; drsharayah gmail. Gastroparesis is defined by delayed gastric emptying in the absence of a mechanical obstruction, with symptoms of nausea, vomiting, bloating, and abdominal pain. Most commonly it is idiopathic or caused by long-standing uncontrolled diabetes.
0 thoughts on “DKA symptoms and diabetic gastroparesis”