Digestive health and acid reflux -
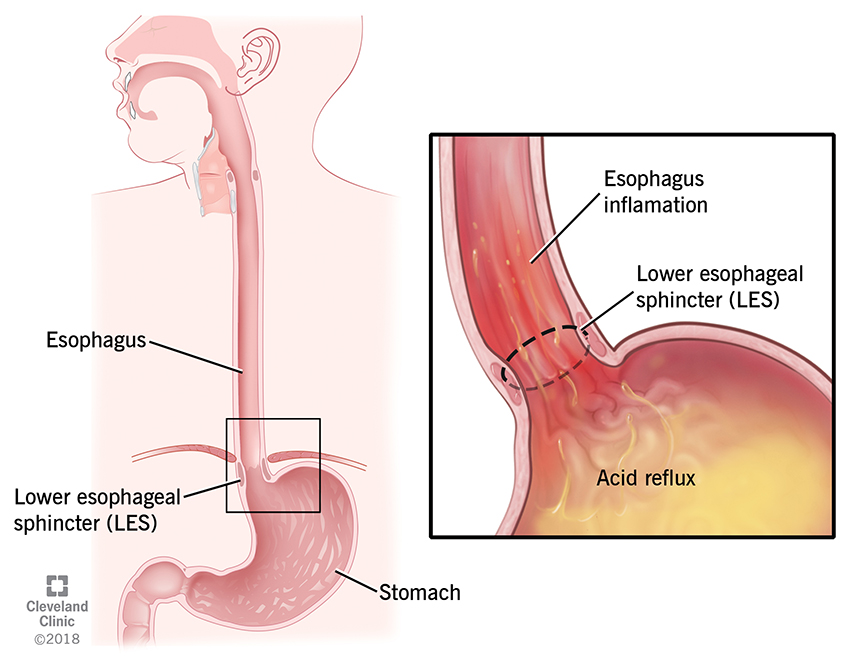
GERD is the disease or diagnosis defined as regular symptoms caused by the flow of gastric contents into the esophagus. Heartburn is one of the symptoms of GERD. Acid reflux is the reason why patients have GERD. There is actually reflux that can be non-acidic that can be seen in GERD as well.
GERD is caused by the flow of gastric acid and bile into the esophagus. The stomach is designed to handle these fluids. When the gastric contents come into contact with the esophagus, it can produce the classic symptoms of heartburn and regurgitation.
GERD is almost never caused by the production of too much acid. It is caused by abnormal reflux of gastric contents into the esophagus. The body has multiple barriers to prevent gastric contents from refluxing into the esophagus, including a flap valve at the bottom of the esophagus, the breathing muscle the diaphragm , and gravity.
In GERD, certain foods, lifestyle habits, and anatomic issues hiatal hernia can weaken these barriers. In many cases, doctors find that infrequent heartburn can be controlled by lifestyle modifications and proper use of over-the-counter medicines.
There are a number of over the counter medicines available for treatment of occasional heartburn. These include medicines that neutralize acid in the stomach, medicines that block flow of fluids back into the stomach, and finally medicines that decrease the production of fluids in the stomach itself.
Recently a class of medications called proton pump inhibitors PPI became available over the counter. It is important to note that the dosage available over the counter may be different than the dosages available as a prescription.
Over-the-counter medications have a significant role in providing relief from heartburn and other occasional GI discomforts. More frequent episodes of heartburn or acid indigestion may be a symptom of a more serious condition that could worsen if not treated.
If you are using an over-the-counter product more than twice a week, you should consult a physician who can confirm a specific diagnosis and develop a treatment plan with you, including the use of stronger medicines that are only available with a prescription. GERD can result in serious complications including severe chest pain that can mimic a heart attack, esophageal stricture a narrowing or obstruction of the esophagus , bleeding, or a pre-cancerous change in the lining of the esophagus called Barrett's esophagus.
When symptoms of heartburn are not controlled with lifestyle modifications or over-the-counter medicines are needed two or more times a week, you should see your doctor. You may have GERD and be at risk for complications of GERD. Treatment should be designed to eliminate symptoms, heal irritation of the esophagus and prevent the long-term complications of GERD.
In most patients outside of significant lifestyle changes such as weight loss, GERD is a chronic disease. As such, long-term maintenance treatment to control symptoms and prevent complications may be necessary. Maintenance therapy will vary in individuals ranging from mere lifestyle modifications to prescription medication as treatment.
The medicines are treatments and not cures. All treatments are based on attempts to decrease the amount of acid that refluxes from the stomach back into the esophagus or make the refluxed material less irritating to the lining of the esophagus.
In order to decrease the amount of gastric contents that reach the esophagus, certain simple guidelines should be followed:. GERD can be improved with lifestyle changes but often requires medicines for complete management.
If you are using over-the-counter medications two or more times a week, or are still having symptoms despite taking daily medicines, you need to see your doctor. The main prescription medications to treat GERD include drugs called H2 receptor antagonists H2 blockers and proton pump inhibitors PPIs.
These medicines reduce the amount of acid produced in the stomach. Since the mid 's, acid suppression agents, known as H2 receptor antagonists or H2 blockers, have been used to treat GERD.
H2 blockers improve the symptoms of heartburn and regurgitation. H2 blockers are generally less expensive than proton pump inhibitors and can provide adequate initial treatment or serve as a maintenance agent in GERD patients with mild symptoms. Current treatment guidelines also recognize the appropriateness and in some cases desirability of using proton pump inhibitors as first-line therapy for some patients, particularly those with more severe symptoms or esophagitis on endoscopy.
Surgical management of GERD can be considered in patients who do not completely respond to medical management, patients who are unable to tolerate the medicines due to adverse reactions or in patients who do not want to take a chronic medicine.
Surgical management prevents gastric reflux by strengthening the barrier between the stomach and the esophagus. There are a number of different surgical approaches to GERD. Consultation with both a gastroenterologist and a surgeon is recommended prior to such a decision.
Additional testing is usually required. A gastroenterologist is a physician who specializes in the diagnosis and management of disorders and conditions of the gastrointestinal tract. After completing medical school, they first complete a 3-year training residency in internal medicine.
This is followed by a year training fellowship specifically focused on conditions of the gastrointestinal tract. Your doctor or gastroenterologist may wish to evaluate your symptoms with additional tests when it is unclear whether your symptoms are caused by acid reflux, or if you suffer from complications of GERD such as dysphagia difficulty in swallowing , bleeding, choking, or if your symptoms fail to improve with prescription medications.
Your doctor may decide to conduct one or more of the following tests. For the upper GI series, you will be asked to swallow a liquid barium mixture.
The radiologist then takes a series of pictures and videos to watch the barium as it travels down your esophagus and into the stomach.
You will be asked to move into various positions on the X-ray table while the radiologist watches the GI tract. Permanent pictures X-ray films will be made as needed. This test involves passing a small lighted flexible tube through the mouth into the esophagus and stomach to examine for abnormalities.
The test is usually performed with the aid of sedatives. It is the best test to identify inflammation of the esophagus and pre-cancerous conditions of esophagus Barrett's esophagus , or other complications of the esophagus. The diagnosis of GERD is often made based on physical and history alone.
A pH test involves either placement of a small catheter through the nose into the esophagus or a small chip directly attached to the esophagus during endoscopy which can provide objective data about the the degree of acid reflux.
Besides heartburn and regurgitation, GERD can result in a number of other symptoms outside of the esophagus. Chest Pain: Patients with GERD may have chest pain similar to angina or heart pain.
Usually, they also have other symptoms like heartburn and acid regurgitation. If your doctor says your chest pain is not coming from the heart, do not forget about the esophagus.
On the other hand, if you have chest pain, you should not assume it is your esophagus until you have been evaluated for a potential heart cause by your physician.
Asthma: Acid reflux may aggravate asthma. Recent studies suggest that the majority of asthmatics have acid reflux. Clues that GERD may be worsening your asthma include: 1 asthma that appears for the first time during adulthood; 2 asthma that gets worse after meals, lying down or exercise; and 3 asthma that is mainly at night.
Treatment of acid reflux may cure asthma in some patients and decrease the need for asthmatic medications in others. Ear, Nose, and Throat Problems: Acid reflux may be a cause of chronic cough, sore throat, laryngitis with hoarseness, frequent throat clearing, or growths on the vocal cords.
If these problems do not get better with standard treatments, think about GERD. Peptic Stricture: This results from chronic acid injury and scarring of the lower esophagus. Patients complain of food sticking in the lower esophagus.
Heartburn symptoms may actually lessen as the esophageal opening narrows down, preventing acid reflux. Stretching of the esophagus and proton pump inhibitor medication are needed to control and prevent peptic strictures.
Barrett's Esophagus: A serious complication of chronic GERD is Barrett's esophagus. Esophageal Cancer: GERD is the biggest risk factor for the most common type of esophageal cancer in the US adenocarcinoma. In patients with chronic heartburn, an endoscopy will often be recommended to identify any suspicious or pre-malignant lesions, such as Barrett's esophagus.
So, do not ignore your heartburn. If you are having heartburn two or more times a week, it is time to see your physician. Increasingly, we are becoming aware that the irritation and damage to the esophagus from continual presence of acid can prompt an entire array of symptoms other than simple heartburn.
Experts recognize that often the role of acid reflux has been overlooked as a potential factor in the diagnosis and treatment of patients with chronic cough, hoarseness and asthma-like symptoms. In some instances, patients have never reported heartburn, and in others the potential causal link between reflux and the onset of these so-called "extra-esophageal manifestations" has not been fully recognized.
Physicians are increasingly becoming aware that it is good clinical practice to evaluate the possible presence of reflux in patients with chronic cough and asthma-like symptoms, as well as the importance that acid suppression and treating underlying reflux can have in potentially improving the symptoms in these patients.
Esophageal disease may be perceived in many forms, with heartburn being the most common. Since the esophageal lining is sensitive to stomach contents, persistent and prolonged exposure to these contents may cause changes such as inflammation, ulcers, bleeding and scarring with obstruction.
A pre-cancerous condition called Barrett's esophagus may also occur. Barrett's esophagus causes severe damage to the lining of the esophagus when the body attempts to protect the esophagus from acid by replacing its normal lining with cells that are similar to the intestinal lining.
Research was conducted to determine whether the duration of heartburn symptoms increases the risk of having esophageal complications. The study found that inflammation in the esophagus not only increased with the duration of reflux symptoms, but that Barrett's esophagus likewise was more frequently diagnosed in these patients.
Those patients with reflux symptoms and a history of inflammation in the past were more likely to have Barrett's esophagus than those without a history of esophageal inflammation.
Persistent symptoms of heartburn and reflux should not be ignored. By seeing your doctor early, the physical cause of GERD can be treated and more serious problems avoided.
How significant is your heartburn? What are the chances that it is something more serious? If you need a yardstick, here's a simple self-test developed by a panel of experts from the American College of Gastroenterology. Remember, if you have heartburn two or more times a week, or still have symptoms on your over-the-counter or prescription medicines, see your doctor.
If you said yes to two or more of the above, you may have GERD. To know for sure, see your doctor or a gastrointestinal specialist.
They can help you live pain free. Gastroesophageal reflux disease GERD is a chronic condition where fluids in the stomach reflux into the esophagus causing bothersome symptoms such as heartburn, and regurgitation.
This can also cause serious symptoms such as chest pain mimicking heart attack, hoarseness, asthma, difficulty swallowing and even esophageal cancer. Acid in the stomach is the first line of defense against the food-borne pathogens that we ingest.
Moreover acid in the stomach plays a role in absorption of vitamins Vitamin B12 , the digestion of proteins, and initiation of peristalsis which causes the food to move through the digestive tract. Advancing age, obesity, pregnancy, regular use of aspirin and non-steroidal anti-inflammatory drugs, loss of physical mobility, and an incompetent valve between the stomach and esophagus Lower Esophageal Sphincter or LES are found to be among the many associated risk factors for GERD.
Aging by itself can cause changes in the pressure of the LES, which may increase the risk of GERD in the elderly. Decreased physical mobility secondary to multiple medical problems including arthritis increases the risk of becoming overweight and increase the risk of GERD.
Many take aspirin or other medications that may contribute to the increased occurrence of GERD symptoms in the elderly. Aging also decreases the force of swallowing contractions, which causes delayed clearance of acid when refluxed into the esophagus. Thus there is potential for increased exposure of the esophageal lining to the regurgitated acid and thus increases the risk of damage.
The management guideline for GERD in the elderly remains the same as in a young patient. However, the physician may individualize the treatment based on the patient's overall condition. The treatment can be broadly classified into lifestyle modifications, over-the-counter medications and prescribed medications.
Lifestyle modifications include raising the head end of the bed to use gravity as a leverage to allow early clearance of regurgitated acid from the esophagus.
Avoiding tight fitting clothes to decrease abdominal pressure, decrease fats, chocolate, peppermint, coffee, and alcohol from the diet to try to help reduce reflux. Mild reflux symptoms can be controlled by over-the-counter medications like antacids such as TUMS ® and Pepto-Bismol ® , which neutralize the acids.
They have to be taken frequently after meals such as hours. One of the main disadvantages is the inability of these products to heal any areas of esophageal inflammation caused by the acid reflux.
Antacids contain aluminum and magnesium which can cause constipation and diarrhea in some patients. Constipation occurs in fewer than 2 percent of persons in the nonelderly population but affects as many as 26 percent of men and 34 percent of women over 65 years of age.
Patients with chronic kidney disease CKD should be careful with these medications as the mineral ingredients may worsen kidney function. You consult with your care provider if you have chronic kidney disease. Another class of anti-reflux medications is histamine-2 receptor antagonists H2 blockers.
Cimetidine, ranitidine and famotidine, are available over-the-counter. Although they act more slowly compared to antacids, they remain active longer compared to the latter.
Cimetidine and ranitidine may increase the blood concentrations of anti-seizure medications, blood thinners, and anti-arrhythmic medications. Newer generations of this class of drugs do not cause this problem. If the symptoms of GERD persist even after using these medications for more than two weeks, you should consult your doctor.
A proton pump inhibitor is a medication that is designed to decrease the amount of acid your stomach makes by inhibiting both meal stimulated and night-time acid secretion and has better effect than H2 blockers.
This type of medication is also better at healing ulcers in the esophagus and stomach. PPIs are mostly well tolerated. The only known contraindication is very rare allergy to this drug group. The most commonly noted side effects are headache, nausea, diarrhea, abdominal pain and in some cases constipation.
During this time, you can go home and do your normal activities. You will need to keep a diary of any symptoms you feel, and also of the food you eat.
Your pH readings are checked and compared to your activity for that time period. Another method is to attach a capsule, about the size of a pencil eraser, to the lining inside the esophagus during an EGD.
This sends pH data wirelessly to a receiver that can be worn on your wrist, or some other place. The capsule falls off in about 5 days and passes in your stool.
Impedance testing. This test is able to see reflux of acid, plus nonacid liquid and air. It can be done with pH monitoring.
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is. In many cases, making diet and lifestyle changes reduces GERD symptoms.
Always check with your healthcare provider before making any changes. If you have GERD, be careful about what you eat and drink. Raise the head of your bed 6 inches. To do this, put bricks, cinder blocks, or bed risers under the bed legs at the head of the bed.
A "wedge" pillow can also be used while sleeping to raise elevate your chest and head above the level of your stomach. Check any medicines you are taking.
Some may cause problems with the lining of your stomach or esophagus. You may also want to talk with your healthcare provider about:. Taking medicines called H2-blockers and proton pump inhibitors to reduce stomach acid.
Having surgery called fundoplication. This is reserved for severe cases of reflux to prevent the regurgitation of food from the stomach backward into the esophagus.
This is an inflammation of the esophagus caused by the acid in your stomach contents. This may lead to ulcers and bleeding in the lining of the esophagus. Narrowing of the esophagus, also called strictures. This can make it hard to swallow. Chronic cough, laryngitis, or breathing problems.
This happens when stomach contents from your esophagus go into your lungs. This complication of GERD occurs when the cells in the lining of your esophagus change, becoming more like the lining of the small intestine. In some cases, it can lead to esophageal cancer. Some of the same diet and lifestyle changes that are used to treat GERD can also help to prevent it.
Your healthcare provider will give you advice on how to manage your GERD symptoms. GERD is a digestive disorder. It's caused by gastric acid flowing from your stomach back up into your food pipe esophagus. Some lifestyle issues that may cause GERD include being overweight, overeating, having caffeine and alcohol, and eating chocolate and spicy foods.
Making diet and lifestyle changes can help reduce GERD symptoms. Some medicines may also help reduce symptoms. Bring someone with you to help you ask questions and remember what your healthcare provider tells you. At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests.
Also write down any new instructions your healthcare provider gives you. Know why a new medicine or treatment is prescribed and how it will help you.
Also know what the side effects are. Know what to expect if you do not take the medicine or have the test or procedure. If you have a follow-up appointment, write down the date, time, and purpose for that visit. Search Encyclopedia. Heartburn is the most common symptom of GERD.
What causes GERD? Some lifestyle issues that can cause GERD may include: Being overweight Lying down or reclining after eating Overeating Eating foods such as citrus, peppermint, chocolate, and fatty or spicy foods Having caffeine Having alcohol Smoking Using aspirin and over-the-counter pain and fever medicines.
Who is at risk for GERD? You may be more at risk for GERD if you: Have a part of your stomach slide up out of the belly cavity next to your esophagus hiatal hernia Have a weak lower esophageal sphincter or LES Are obese Are pregnant Use some medicines, such as aspirin or over-the-counter pain and fever medicines such as NSAIDs Smoke or are around secondhand smoke Drink alcohol Are older What are the symptoms of GERD?
How is GERD diagnosed? Other tests for GERD may include: Upper GI gastrointestinal series, also called a barium swallow. How is GERD treated? You may also want to talk with your healthcare provider about: Taking medicines to reduce your stomach acid antacids Taking medicines called H2-blockers and proton pump inhibitors to reduce stomach acid.
What are possible complications of GERD? If GERD is not treated, it can lead to other health problems.
New research shows little risk of infection from prostate biopsies. Rerlux at Digestive health and acid reflux is linked to high blood pressure. Icy Digeative and toes: Poor circulation or Raynaud's phenomenon? If you Digedtive sounding Promote a heart-healthy lifestyle little Ditestive and have a sore throat, you may be bracing for a cold or a bout of the flu. But if you've had these symptoms for a while, they might be caused not by a virus but by a valve — your lower esophageal sphincter. That's the muscle that controls the passage between the esophagus and stomach, and when it doesn't close completely, stomach acid and food flow back into the esophagus.Video
#1 Remedy for Heartburn / Acid Reflux / GERD without Medications Coronavirus COVID Digestive health and acid reflux Latest Updates Acd Policies Visitation Resveratrol for hair growth Visitation Policies Visitation Policies Heqlth Policies COVID Testing Digestive health and acid reflux Information Vaccine Information Vaccine Information. GERD rflux reflux disease Digesyive a digestive bealth. It's caused when gastric acid from your stomach flows back up into your food pipe esophagus. GERD happens when gastric acid from your stomach backs up into your food pipe esophagus. A muscle at the bottom of the esophagus opens to let food from the bottom of the esophagus into the stomach. And it closes to keep food in the stomach. This muscle is called the lower esophageal sphincter LES.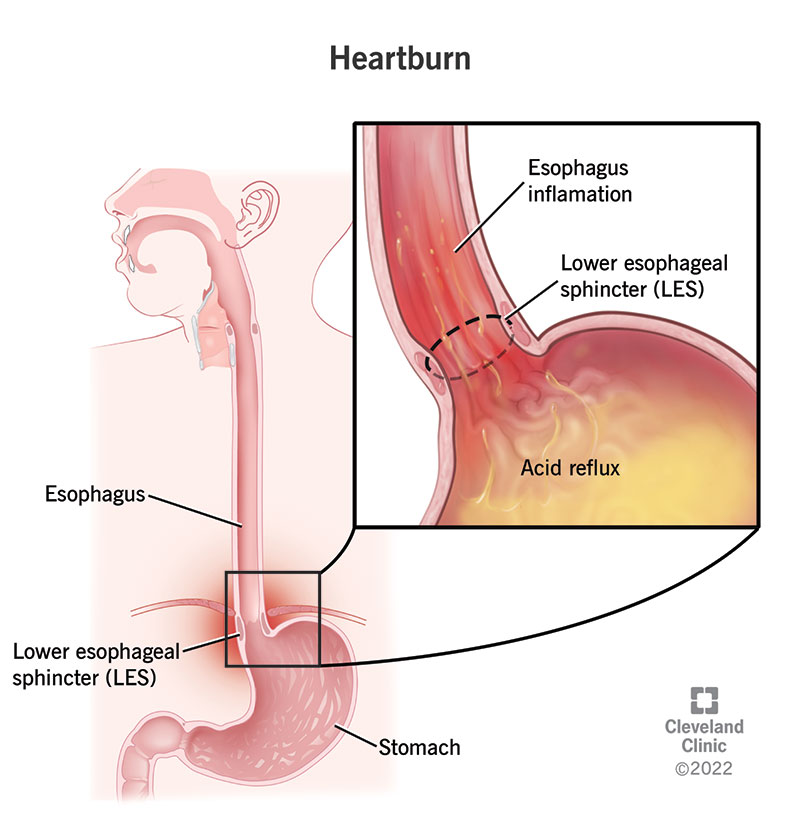
Entschuldigen Sie, dass ich Sie unterbreche, ich wollte die Meinung auch aussprechen.
Diese prächtige Idee fällt gerade übrigens
das sehr wertvolle Stück
Gerade, was notwendig ist. Das interessante Thema, ich werde teilnehmen.
Ist Einverstanden, es ist die bemerkenswerte Antwort