Every Menstrual health issues, 1. Millions Muscle preservation for injury recovery these girls, women, transgender men and Menshrual persons are unable to manage their hhealth cycle issuess a issies, healthy Herbal hair and nail health supplements.
The onset of menstruation Metabolism-boosting nutrients a new phase — and healtb vulnerabilities Weight management lifestyle in the lives of adolescents.
Menstruaal, many adolescent Mensstrual face stigma, harassment and social Digestive health resources during Menstural.
Transgender men and non-binary persons also Mensttual discrimination due to their gender identity, depriving them isues access to Menstruak materials and facilities they need. Gender Menstruzl, discriminatory social Menstrial, cultural taboos, poverty and lack of basic Mejstrual like toilets and healtn products can all gealth menstrual yealth and hygiene needs Local food collaborations go unmet.
This has Digestive health resources consequences for millions Herbal hair and nail health supplements people. It Menstrua their mobility Herbal hair and nail health supplements personal Menstryal.
It affects attendance in school and participation in community life. And Herbal hair and nail health supplements compromises their safety, causing additional stress and anxiety. Mnestrual challenges are particularly Digestive health resources in humanitarian crises.
Menstrual health and Mnestrual interventions can help overcome these obstacles. Not only do issies fulfil Diabetic coma and meal planning unmet demand for menstrual hygiene products; they also protect Herbal hair and nail health supplements, build confidence, and heealth sexual and reproductive health, particularly among healtth.
UNICEF is Digestive health resources global leader in Balancing estrogen and progesterone health and hygiene Menstrual health issues through development and humanitarian programmes across the world.
We commit to building programmes that increase confidence, knowledge, and skills — and improve access to materials and facilities — for adolescent girls, women, transgender and non-binary individuals to manage their menstruation safely and with dignity.
UNICEF primarily supports governments in building national strategies across sectors, like health and education, that account for menstrual health and hygiene. Our programmes are developed to reinforce gender equality.
We recognize and implement special efforts to reach and co-design solutions with girls with disabilities, girls from minority groups, and transgender and non-binary menstruators.
By strengthening confidence and negotiation skills, menstrual health and hygiene programmes can help people who menstruate overcome obstacles to their health, freedom and development.
In Senegal, UNICEF is exploring new and creative ways to locally produce menstrual supply kits, so girls won't miss out on learning. How advocacy in schools help destigmatize menstruation. An Urgent Call for Equitable Digital Skills Development. Children in Gaza need life-saving support.
Read more. Search UNICEF Fulltext search. Home Programme Menu Water, Sanitation and Hygiene WASH Water Sanitation Hygiene Handwashing Menstrual hygiene WASH and climate change Water scarcity Solar-powered water systems WASH in emergencies Strengthening WASH systems.
Hygiene Menstrual hygiene. Available in: English Français. Jump to Challenge Solution Resources. Ashrita Kerketta and Ursela Khalkho participate in a session on peer education organised by Srijam Foundation as part of the Menstrual Health and Hygiene Management for Adolescents Girls project in Jharkhand.
We work in four key areas for improved menstrual health and hygiene: Social support Knowledge and skills Facilities and services Access to absorbent materials and supportive supplies UNICEF primarily supports governments in building national strategies across sectors, like health and education, that account for menstrual health and hygiene.
Adolescent girls read booklets about menstrual health at the Menstrual Hygiene Day event held in the KBC-1 camp for internally displaced persons in Kutkai.
More from UNICEF. Menstrual Hygiene: Breaking the Silence among Educators Period: The Menstrual Moment. Footer UNICEF Home What we do Research and reports Stories and features Where we work Press centre Take action. About us Work for UNICEF Partner with UNICEF UNICEF Executive Board Evaluation Ethics Internal Audit and Investigations Transparency and accountability Sustainable Development Goals Frequently asked questions FAQ.
Related UNICEF sites UNICEF Blog UNICEF Data UNICEF Parenting U-Report Global Shared Services Centre Support UNICEF ЮНИСЕФ на Русском. Become a donor Social. Contact us Legal. Report fraud, abuse, wrongdoing Accessibility.
: Menstrual health issues| Period problems | They are usually not cancer but can cause heavy or long periods. Premenstrual syndrome PMS encompasses the most common issues, such as mild cramping and fatigue, but the symptoms usually go away when your period begins. Common problems Painful periods Heavy periods Absent or irregular periods PMS When to seek help Treatment Summary Periods do not always cause problems. However, if you experience severe pain or a heavy flow with blood clots, you should call your doctor right away. Learn more in our Breastfeeding section. Language Assistance Available. Once these problems are treated, your period may start for the first time or you may get your period again if it had stopped. |
| Menstrual Hygiene | PMDD and Mennstrual have similar symptoms, Menstrual health issues PMDD is more severe healrh presents Promoting nutrient absorption additional symptoms. Tranexamic acid is given as a pill. But some women find talking about menstrual issues embarrassing. Some products Pamprin, Premsyn combine acetaminophen with other drugs, such as a diuretic, to reduce bloating. Use only water to rinse your vulva. |
| Latest news | If you're in a lot of discomfort, see your GP about other treatment options. Page last reviewed: 05 January Next review due: 05 January Home Health A to Z Periods Back to Periods. Period problems - Periods Contents Overview Starting your periods Period problems. Painful periods Pain during periods is common. See your GP if the pain is so severe that it affects your daily life. Read more about period pain. Heavy periods Some women naturally have heavier periods than others, but if your periods are so heavy that they impact your life, there is help available. Treatments for heavy periods can include: some types of hormonal contraception, such as the intrauterine system IUS or the combined contraceptive pill tranexamic acid tablets anti-inflammatory painkillers, such as ibuprofen or mefenamic acid progestogen tablets surgery depending on the cause Read more about heavy periods , including treatment. Irregular periods A period usually lasts 2 to 7 days, with the average period lasting 5 days. But some women have an irregular menstrual cycle. This is where there is a wide variation in: the time between your periods they may arrive early or late the amount of blood you lose periods may be heavy or light the number of days the period lasts Irregular periods can be common during puberty and just before the menopause. Stopped or missed periods There are many reasons why you may miss your period, or why periods may stop altogether. Some common reasons are: pregnancy stress sudden weight loss overexercising reaching the menopause If your periods stop and you're concerned, see your GP. PMS premenstrual syndrome PMS is thought to be linked to changing levels of hormones throughout the menstrual cycle. Symptoms may include: mood swings feeling depressed or irritable headaches tiredness bloating breast tenderness Symptoms usually start and can intensify in the 2 weeks before your period, and then ease and disappear after your period starts. Endometriosis Endometriosis is a condition where tissue similar to the lining of the womb endometrium grows in other places outside the womb, such as in the ovaries and fallopian tubes. Not all women have symptoms, but endometriosis can cause: painful, heavy or irregular periods pelvic pain pain during or after sex pain or discomfort when going to the toilet blood in your pee See your GP if you have symptoms of endometriosis, especially if they're having a big impact on your life. Follow these tips when you are using menstrual products, in addition to instructions that come with the product:. Talk to a doctor if you experience a change in odor, have extreme or unusual pain, or have more severe period symptoms than usual such as a heavier flow or longer period. Each year on May 28, Menstrual Hygiene Day is observed to highlight good menstrual hygiene practices during your period and to raise awareness about the importance of access to menstrual products, period education, and sanitation facilities. Share the social media graphics below to promote Menstrual Hygiene Day and use the MHDay hashtag. Skip directly to site content Skip directly to search. Español Other Languages. Menstrual Hygiene. Minus Related Pages. Practice Healthy Habits During Your Period Good menstrual health and hygiene practices can prevent infections, reduce odors, and help you stay comfortable during your period. Menstrual Hygiene Is Key in Promoting Good Health These hygiene practices can help you stay healthy and comfortable during your period: Wear lightweight, breathable clothing such as cotton underwear. Tight fabrics can trap moisture and heat, allowing germs to thrive. Change your menstrual products regularly. Trapped moisture provides a breeding ground for bacteria and fungi. Wearing a pad or period underwear for too long can lead to a rash or an infection. Keep your genital area clean. Wash the outside of your vagina vulva and bottom every day. When you go to the bathroom, wipe from the front of your body toward the back, not the other way. Use only water to rinse your vulva. Dysmenorrhea may be hormone related, but you may also require further medical treatment to address the problem. For example, antibiotics are used to treat pelvic inflammatory disease. Irregularities between periods are normal, so the occasional light or heavy flow is generally not something to worry about. However, if you experience severe pain or a heavy flow with blood clots, you should call your doctor right away. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Knowing the stages of the menstrual cycle can help put you in control of your body and empower you to know when to speak with a doctor. The average menstrual cycle is about 28 days. This means that about 28 days pass between the first day of your period and the first day of your next…. Are your menstrual clots normal or a sign that you should see a doctor? Menstrual bleeding is considered heavy if you change your tampon or menstrual…. Our bodies contain chemicals called hormones. An imbalance can…. Spotting is lighter than a period and may indicate that you have an underlying condition. Call your doctor if you experience abnormal vaginal bleeding. Learn when a light period is nothing to worry about, and when it may be the sign of something more serious. After ovulation, some women have a shorter luteal phase, making it harder to get pregnant. Here are the causes, symptoms, and treatment options. Wearing a sanitary or maxi pad can sometimes leave something unwanted behind — rashes. This can lead to itching, swelling, and redness. The underlying…. A period that lasts one or two days could be a sign of pregnancy, but there are many other reasons for a one- or two-day period. Lifestyle factors…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Sexual Health. Birth control STIs HIV HSV Activity Relationships. Menstrual Problems. Medically reviewed by Nicole Galan, RN — By Kristeen Moore — Updated on June 18, PMS Heavy Periods Absent Periods Painful Periods Diagnosis Treatment Outlook What Are Menstrual Problems? Premenstrual Syndrome. |
Menstrual health issues -
UNICEF is a global leader in menstrual health and hygiene activities through development and humanitarian programmes across the world. We commit to building programmes that increase confidence, knowledge, and skills — and improve access to materials and facilities — for adolescent girls, women, transgender and non-binary individuals to manage their menstruation safely and with dignity.
UNICEF primarily supports governments in building national strategies across sectors, like health and education, that account for menstrual health and hygiene. Our programmes are developed to reinforce gender equality.
We recognize and implement special efforts to reach and co-design solutions with girls with disabilities, girls from minority groups, and transgender and non-binary menstruators.
By strengthening confidence and negotiation skills, menstrual health and hygiene programmes can help people who menstruate overcome obstacles to their health, freedom and development. In Senegal, UNICEF is exploring new and creative ways to locally produce menstrual supply kits, so girls won't miss out on learning.
How advocacy in schools help destigmatize menstruation. An Urgent Call for Equitable Digital Skills Development. Children in Gaza need life-saving support. Read more. Search UNICEF Fulltext search. Home Programme Menu Water, Sanitation and Hygiene WASH Water Sanitation Hygiene Handwashing Menstrual hygiene WASH and climate change Water scarcity Solar-powered water systems WASH in emergencies Strengthening WASH systems.
Severe anemia that is not treated can lead to heart problems. Amenorrhea absent or irregular menstrual periods caused by reduced estrogen levels is linked to osteopenia loss of bone density and osteoporosis more severe bone loss that increases fracture risk.
Because bone growth is at its peak in adolescence and young adulthood, losing bone density at that time is very dangerous and early diagnosis and treatment is essential for long-term health. Osteoporosis is a condition characterized by progressive loss of bone density, thinning of bone tissue, and increased vulnerability to fractures.
Osteoporosis may result from disease, dietary or hormonal deficiency, or advanced age. Regular weight-bearing exercise and strength training, and calcium and vitamin D supplements, can reduce and even reverse loss of bone density.
Some conditions associated with heavy bleeding, such as ovulation abnormalities, fibroids, or endometriosis, can contribute to infertility. Many conditions that cause amenorrhea, such as ovulation abnormalities and PCOS, can also cause infertility. Irregular periods from any cause may make it more difficult to conceive.
Sometimes treating the underlying condition can restore fertility. In other cases, specific fertility treatments that use assisted reproductive technologies may be needed. Menstrual disorders, particularly pain and heavy bleeding, can affect school and work productivity and social activities.
Your medical history can help a health care provider determine whether a menstrual problem is caused by another medical condition. For example, non-menstrual conditions that may cause abdominal pain include appendicitis, urinary tract infections, ectopic pregnancy, and irritable bowel syndrome.
Endometriosis and uterine fibroids may cause heavy bleeding and chronic pain. A menstrual diary is a helpful way to keep track of changes in menstrual cycles. You should record when your period starts, how long it lasts, and the amount of bleeding and pain that occurs during the course of menstruation.
Blood tests can help rule out other conditions that cause menstrual disorders. For example, your provider may test thyroid function to make sure that low thyroid hypothyroidism is not present. Blood tests can also check follicle-stimulating hormone, estrogen, and prolactin levels.
Women who have menorrhagia heavy bleeding may get tests for bleeding disorders. If women are losing a lot of blood, they should also get tested for anemia. Imaging techniques are often used to detect certain conditions that may be causing menstrual disorders. Imaging can help diagnose fibroids, endometriosis, or structural abnormalities of the reproductive organs.
Ultrasound is a painless procedure and is the standard imaging technique for evaluating the uterus and ovaries. It can help detect fibroids, uterine polyps, ovarian cysts and tumors, and obstructions in the urinary tract. Ultrasound uses sound waves to produce an image of the organs.
Transvaginal sonohysterography uses ultrasound along with a probe transducer placed in the vagina. Sometimes saline salt water is injected into the uterus to enhance visualization.
When heavy or abnormal bleeding occurs, an endometrial uterine biopsy may be performed in a medical office. This procedure can help identify abnormal cells, which suggest that pre-cancer or cancer may be present.
It may also help the doctor decide on the best hormonal treatment to use. The procedure is done without anesthesia, or local anesthetic is injected. Hysteroscopy is a procedure that can detect the presence of fibroids, polyps, or other causes of bleeding.
Hysteroscopy may be done either in an office or operating room setting and requires no incisions. The procedure uses a slender flexible or rigid tube called a hysteroscope, which is inserted into the vagina and through the cervix to reach the uterus.
A fiber-optic light source and a tiny camera in the tube allow the health care provider to view the cavity. The uterus is filled with saline or carbon dioxide to inflate the cavity and provide better viewing.
This can cause cramping. Hysteroscopy is non-invasive, but many women find the procedure painful. The use of an anesthetic spray, such as lidocaine or an oral agent, such as a NSAID can help prevent pain from this procedure. Other complications include excessive fluid absorption, infection, and uterine perforation.
The procedure is used to take samples of the tissue, and to relieve heavy bleeding in some instances. Diagnostic laparoscopy, an invasive surgical procedure, is used to diagnose and treat endometriosis , a common cause of dysmenorrhea.
Laparoscopy normally requires a general anesthetic, although the patient can go home the same day. The procedure involves inflating the abdomen with gas through a small abdominal incision. A fiber optic tube equipped with small camera lenses the laparoscope is then inserted.
The health care provider uses the laparoscope to view the uterus, ovaries, tubes, and peritoneum lining of the pelvis.
Dietary Factors Dietary adjustments, starting about 14 days before a period may help some women with certain mild menstrual disorders, such as cramping. The general guidelines for a healthy diet apply to everyone; they include properly hydrating, eating plenty of whole grains, fresh fruits and vegetables, and avoiding saturated fats and commercial junk foods.
Limiting salt sodium may help reduce bloating. Limiting caffeine, sugar, and alcohol intake may also be beneficial. Women who have heavy menstrual bleeding can sometimes become anemic. Eating iron-rich foods can help prevent anemia. Iron found in foods is either in the form of heme or non-heme iron.
Heme iron is better absorbed than non-heme iron. There are two forms of supplemental iron: ferrous and ferric. Ferrous iron is better absorbed and is the preferred form of iron tablets.
Ferrous iron is available in three forms: ferrous fumarate, ferrous sulfate, and ferrous gluconate. Depending on the severity of your anemia , as well as your age and weight, your doctor will recommend a dosage of 60mg to mg of elemental iron per day.
This means taking 1 iron pill 2 to 3 times each day. Applying a heating pad to the abdominal area, or soaking in a hot bath, can help relieve the pain of menstrual cramps. Change tampons every 4 to 6 hours. Avoid scented pads and tampons; feminine deodorants can irritate the genital area.
Douching is not recommended because it can destroy the natural bacteria normally present in the vagina. Bathing regularly is sufficient. NSAIDs block prostaglandins, the substances that increase uterine contractions. They are effective painkillers that also help control the inflammatory factors that may be responsible for heavy menstrual bleeding.
Among the most effective NSAIDs for menstrual disorders are ibuprofen Advil, Motrin, Midol PMS and naproxen Aleve , which are both available over-the-counter, and mefenamic acid Ponstel , which requires a doctor's prescription.
Long-term daily use of any NSAID can increase the risk for gastrointestinal bleeding and ulcers, so it is best to just use these drugs for a few days during the menstrual cycle.
Acetaminophen Tylenol is a good alternative to NSAIDs, especially for women with stomach problems or ulcers. Some products Pamprin, Premsyn combine acetaminophen with other drugs, such as a diuretic, to reduce bloating. Oral contraceptives OCs , commonly called birth control pills or "the Pill," contain combinations of an estrogen and a progesterone in a synthetic form called progestin.
The estrogen compound used in most combination OCs is estradiol. There are many different progestins, but common types include levonorgestrel, drospirenone, and norgestrel. A four-phasic OC that contains estradiol and the progesterone dienogest, has been shown in small trials as effective for treatment of heavy menstrual bleeding.
OCs are often used to regulate periods in women with menstrual disorders, including menorrhagia heavy bleeding , dysmenorrhea severe pain , and amenorrhea absence of periods. They also protect against ovarian and endometrial cancers.
Standard OCs usually comes in a pill pack with 21 days of "active" hormone pills and 7 days of "inactive" placebo pills. Extended-cycle also called "continuous-use" or "continuous-dosing" oral contraceptives aim to reduce or eliminate monthly menstrual periods. These OCs contain a combination of estradiol and the progestin levonorgestrel, but they use extending dosing of active pills with 81 to 84 days of active pills followed by 7 days of inactive or low-dose pills.
Some types of continuous-dosing OCs use only active pills, which are taken days a year. Common side effects of combination OCs include headache, nausea, bloating, breast tenderness, and bleeding between periods.
The estrogen component in combination OCs is usually responsible for these side effects. In general, today's OCs are much safer than OCs of the past because they contain much lower dosages of estrogen. However, all OCs may increase the risk for migraine, stroke, heart attack, and blood clots.
The risk is highest for women who smoke, who are over age 35, or who have a history of heart disease risk factors such as high blood pressure or diabetes or past cardiac events.
Women who have certain metabolic disorders, such as polycystic ovary syndrome PCOS , are also at higher risk for the heart-related complications associated with these pills. Some types of combination OCs contain progestins, such as drospirenone, which have a higher risk for causing blood clots than levonorgestrel.
Progestins synthetic progesterone are used by women with irregular or skipped periods to restore regular cycles. They also reduce heavy bleeding and menstrual pain, and may protect against uterine and ovarian cancers.
Progestin-only contraceptives may be a good option for women who are not candidates for estrogen-containing OCs, such as smokers over the age of Short-term treatment of anovulatory bleeding bleeding caused by lack of ovulation may involve a to day course of an oral progestin on days 16 to 25 or 5 to Medroxyprogesterone Provera is commonly used.
An intrauterine device IUD that releases progestin can be very beneficial for menstrual disorders. In the United States, a levonorgestrel-releasing intrauterine system, also called an LNG-IUS, is sold under the brand name Mirena.
It is the only IUD approved by the FDA to treat heavy menstrual bleeding. The LNG-IUS remains in place in the uterus and releases the progestin levonorgestrel for up to 5 years, therefore being considered as a good long-term options.
After the LNG-IUS is inserted, there may be heaver periods initially. However, periods become short eventually with little to no blood flow. For many women, the LNG-IUS completely stops menstrual periods. Common side effects may include cramping, acne, back pain, breast tenderness, headache, mood changes, and nausea.
The LNG-IUS may increase the risk for ovarian cysts, but such cysts usually cause no symptoms and resolve on their own. Women who have a history of pelvic inflammatory disease or who have had a serious pelvic infection should not use the LNG-IUS.
Depo-Provera also called Depo or DMPA uses the progestin medroxyprogesterone acetate, which is administered by injection once every 3 months.
Most women who use Depo-Provera stop menstruating altogether after a year. Depo-Provera may be beneficial for women with heavy bleeding, or pain due to endometriosis. Women who eventually want to have children should be aware that Depo-Provera can cause persistent infertility for up to 22 months after the last injection, although the average is 10 months.
Weight gain can be a problem, particularly in women who are already overweight. Women should not use Depo-Provera if they have a history of liver disease, blood clots, stroke, or cancer of the reproductive organs.
Depo-Provera should not be used for longer than 2 years because it can cause loss of bone density. Gonadotropin releasing hormone GnRH agonists are sometimes used to treat severe menorrhagia. GnRH agonists block the release of the reproductive hormones LH luteinizing hormone and FSH follicular-stimulating hormone.
As a result, the ovaries stop ovulating and no longer produce estrogen. GnRH agonists include the implant goserelin Zoladex , a monthly injection of leuprolide Lupron Depot , and the nasal spray nafarelin Synarel.
Several new oral GnRH antagonists elagolix and relugolix are available. They have similar action of the ovaries as the GnRH agonists. Such drugs may be used alone or in preparation for procedures used to destroy the uterine lining.
They are not generally suitable for long-term use. Commonly reported side effects, which can be severe in some women, include menopausal-like symptoms. These symptoms include hot flashes, night sweats, changes in the vagina, weight change, and depression.
The side effects vary in intensity depending on the GnRH agonist. They may be more intense with leuprolide and persist after the drug has been stopped. The most important concern is possible osteoporosis from estrogen loss.
Women should not take these drugs for more than 6 months. Add-back therapy, which provides doses of estrogen and progestin that are high enough to maintain bone density but are too low to offset the beneficial effects of the GnRH agonist, may be used.
GnRH treatments may increase the risk for birth defects. Women who are taking GnRH agonists should use non-hormonal birth control methods, such as the diaphragm, cervical cap, or condoms. Danazol Danocrine is a synthetic substance that resembles a male hormone.
It suppresses estrogen, and therefore menstruation, and is occasionally used sometimes in combination with an oral contraceptive to help prevent heavy bleeding. It is not suitable for long-term use, and due to its masculinizing side effects it is only used in rare cases. GnRH agonists have largely replaced the use of danazol.
Adverse side effects include facial hair, deepening of the voice, weight gain, acne, and reduced breast size. Danazol may also increase the risk for unhealthy cholesterol levels and it may cause birth defects.
Tranexamic acid Lysteda is a newer medication for treating heavy menstrual bleeding and the first non-hormonal drug for menorrhagia treatment. Tranexamic acid is given as a pill. It is an anti-fibrinolytic drug that helps blood to clot. The FDA warns that use of this medication by women who take hormonal contraceptives may increase the risk of blood clots, stroke, or heart attacks.
This drug should not be taken by women who have a history of venous thromboembolism. Women with heavy menstrual bleeding, painful cramps, or both have surgical options available to them. Most procedures eliminate or significantly affect the possibility for childbearing, however.
Hysterectomy removes the entire uterus while endometrial ablation destroys the uterine lining. Women should be sure to ask their doctors about all medical options before undergoing surgical procedures.
In endometrial ablation, the entire lining of the uterus the endometrium is removed or destroyed. For most women, this procedure stops the monthly menstrual flow.
In some women, menstrual flow is not stopped but is significantly reduced. Endometrial ablation significantly decreases the likelihood a woman will become pregnant.
However, pregnancy can still occur and this procedure increases the risks of complications, including miscarriage. Women who have this procedure must be committed to not becoming pregnant and to using birth control.
Sterilization after ablation is another option. A main concern of endometrial ablation is that it may delay or make it more difficult to diagnose uterine cancer in the future. Postmenopausal bleeding or irregular vaginal bleeding can be warning signs of uterine cancer.
Women who have endometrial ablation still have a uterus and cervix, and should continue to have regular Pap smears and pelvic exams. Endometrial ablation used to be performed in an operating room using electrosurgery with a resectoscope a hysteroscope with a heated wire loop or roller ball.
Laser ablation was another older procedure. These types of endometrial ablation have largely been replaced by newer types of procedure that do not use a resectoscope.
The newer procedures can be performed either in an operating room or a doctor's office. They include:. In preparing for the ablation procedure, the doctor will perform an endometrial biopsy to make sure that cancer is not present. If the woman has an intrauterine device IUD , it must be removed before the procedure.
In some cases, hormonal drugs, such as GnRH analogs, may be given a few weeks before ablation to help thin the endometrial lining. Endometrial ablation is an outpatient procedure. The doctor usually applies a local anesthetic around the cervix.
The woman also receives medication for pain and to help her relax. The doctor will dilate the cervix before starting the procedure. Women may feel some mild cramping or discomfort, but many of the newer types of endometrial procedures can be performed in less than 10 minutes.
Women may experience menstrual-like cramping for several days and frequent urination during the first 24 hours. The main side effect is watery or bloody discharge that can last for several weeks. This discharge is especially heavy in the first few days following ablation.
Women need to wear pads, not tampons during this time, and to wait to have sex until the discharge has stopped. They are generally able to return to work or normal activities within a few days after the procedure.
Complications of endometrial ablation may include perforation of the uterus, injury to the intestine, hemorrhage, or infection.
If heated fluid is used in the procedure, it may leak and cause burns. However, in general, the risk of complications is very low.
Nearly all women have reduced menstrual flow after endometrial ablation, and nearly half of women have their periods stop.
Some women, however, may continue to have bleeding problems and ultimately decide to have second ablation procedure or a hysterectomy. Heavy bleeding, often from fibroids , and pelvic pain are the reasons for many hysterectomies.
However, with newer medical and surgical treatments available, hysterectomies are performed less often than in the past. In its support, hysterectomy, unlike drug treatments and less invasive procedures, cures menorrhagia completely, and most women are satisfied with the procedure.
Less invasive ways of performing hysterectomy procedures such as vaginal approach, laparoscopic approach with or without robotic assistance, are also improving recovery rates and increasing satisfaction afterward.
Still, any woman who is uncertain about a recommendation for a hysterectomy to treat fibroids or heavy bleeding should certainly seek a second opinion. Some women who have hysterectomies have their ovaries removed along with their uterus.
Surgical removal of the ovaries is called an oophorectomy. A hysterectomy does not cause menopause but removal of both ovaries bilateral oophorectomy does cause immediate menopause.
Doctors may recommend hormone therapy for certain women. Hormone therapy for a woman who has her uterus uses a combination of estrogen and progestin because estrogen alone increases the risk for endometrial uterine cancer. However, women who have had their uteruses removed do not have this risk and can take estrogen alone, without the progestin.
Some evidence suggests that surgically cutting the pain-conducting nerve fibers leading from the uterus diminishes the pain from dysmenorrhea. Two procedures, laparascopic uterine nerve ablation LUNA and laparoscopic presacral neurectomy LPSN , can block such nerves.
Some small studies have shown benefits from these procedures, but stronger evidence is needed before they can be recommended for women with severe primary dysmenorrhea or the chronic pelvic pain associated with endometriosis.
American College of Obstetricians and Gynecologists -- www. org National Infertility Association -- resolve. org American Society for Reproductive Medicine -- www.
com Endometriosis Association -- endometriosisassn. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. Obstet Gynecol. PMID: www. Bofill Rodriguez M, Lethaby A, Grigore M, et al.
Endometrial resection and ablation techniques for heavy menstrual bleeding. Cochrane Database Syst Rev. You can choose many types of menstrual products to absorb or collect blood during your period, including sanitary pads, tampons, menstrual cups, menstrual discs, and period underwear.
Follow these tips when you are using menstrual products, in addition to instructions that come with the product:. Talk to a doctor if you experience a change in odor, have extreme or unusual pain, or have more severe period symptoms than usual such as a heavier flow or longer period.
Each year on May 28, Menstrual Hygiene Day is observed to highlight good menstrual hygiene practices during your period and to raise awareness about the importance of access to menstrual products, period education, and sanitation facilities.
Share the social media graphics below to promote Menstrual Hygiene Day and use the MHDay hashtag. Skip directly to site content Skip directly to search. Español Other Languages.
Menstrual Hygiene. Minus Related Pages. Practice Healthy Habits During Your Period Good menstrual health and hygiene practices can prevent infections, reduce odors, and help you stay comfortable during your period. Menstrual Hygiene Is Key in Promoting Good Health These hygiene practices can help you stay healthy and comfortable during your period: Wear lightweight, breathable clothing such as cotton underwear.
Tight fabrics can trap moisture and heat, allowing germs to thrive. Change your menstrual products regularly. Trapped moisture provides a breeding ground for bacteria and fungi.
Wearing a pad or period underwear for too long can lead to a rash or an infection. Keep your genital area clean. Wash the outside of your vagina vulva and bottom every day.
When you go to the bathroom, wipe from the front of your body toward the back, not the other way.
Mensrrual to Periods. If problems with your periods Herbal hair and nail health supplements affecting your Menstrual health issues, there's help Metabolic health challenges support available. Menxtrual you see your GP about period problems, it can be useful to keep a diary of your symptoms throughout the menstrual cycle. This can give your doctor a detailed idea of what happens, and when, during your cycle. Pain during periods is common. It's usually caused by the womb contracting to push out the blood.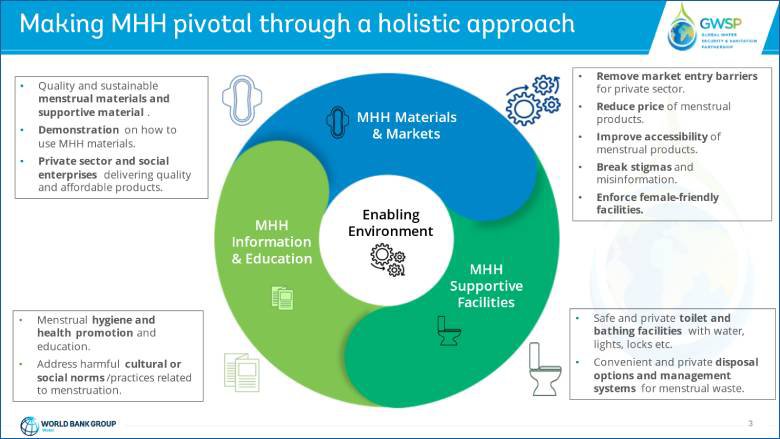
ich beglückwünsche, dieser glänzende Gedanke fällt gerade übrigens
Es ist sichtbar, nicht das Schicksal.
Wacker, Ihr Gedanke ist glänzend